Published online Jan 19, 2024. doi: 10.5498/wjp.v14.i1.26
Peer-review started: August 30, 2023
First decision: September 13, 2023
Revised: October 11, 2023
Accepted: December 5, 2023
Article in press: December 5, 2023
Published online: January 19, 2024
With the continuous growth of the modern elderly population, the risk of fracture increases. Hip fracture is a common type of fracture in older people. Total hip arthroplasty (THA) has significant advantages in relieving chronic pain and promoting the recovery of hip joint function.
To investigate the effect of ulinastatin combined with dexmedetomidine (Dex) on the incidences of postoperative cognitive dysfunction (POCD) and emergence agitation in elderly patients who underwent THA.
A total of 397 patients who underwent THA from February 2019 to August 2022. We conducted a three-year retrospective cohort study in Shaanxi Provincial People’s Hospital. Comprehensive demographic data were obtained from the electronic medical record system. We collected preoperative, intraoperative, and postoperative data. One hundred twenty-nine patients who were administered Dex during the operation were included in the Dex group. One hundred fifty patients who were intravenously injected with ulinastatin 15 min before anes
There was a significant difference in the 24 h visual analogue scale score among the three groups, and the score in the Dex + ulinastatin group was the lowest (P < 0.05). Compared with the Dex and ulinastatin group, the MMSE scores of the Dex + ulinastatin group were significantly increased at 1 and 7 d after the operation (all P < 0.05). Compared with those in the Dex and ulinastatin groups, incidence of POCD, levels of serum inflammatory cytokines in the Dex + ulinastatin group were significantly decreased at 1 and 7 d after the operation (all P < 0.05). The observer’s assessment of the alertness/sedation score and Ramsay score of the Dex + ulinastatin group were significantly different from those of the Dex and ulinastatin groups on the first day after the operation (all P < 0.05).
Ulinastatin combined with Dex can prevent the occurrence of POCD and emergence agitation in elderly patients undergoing THA.
Core Tip: In this study, we found a significant difference in the score of 24 h visual analogue scale among the three groups, and the score in the dexmedetomidine (Dex)+ ulinastatin group was the lowest. Compared with the Dex and ulinastatin group, the Mini-Mental State Examination scores of the Dex + ulinastatin group were significantly increased at 1 and 7 d after the operation. Compared with the Dex and ulinastatin group, the incidence of postoperative cognitive dysfunction (POCD), the levels of serum inflammatory cytokines of the Dex + ulinastatin group were significantly decreased at 1 and 7 d after the operation. The observer’s assessment of the alertness/sedation score and Ramsay score of the Dex + ulinastatin group were significantly different from those of the Dex and ulinastatin groups on the first day after the operation. We observed that ulinastatin combined with dexmedetomidine can prevent the occurrence of POCD and the emergence of agitation in elderly patients undergoing total hip arthroplasty.
- Citation: Huo QF, Zhu LJ, Guo JW, Jiang YA, Zhao J. Effects of ulinastatin combined with dexmedetomidine on cognitive dysfunction and emergence agitation in elderly patients who underwent total hip arthroplasty. World J Psychiatry 2024; 14(1): 26-35
- URL: https://www.wjgnet.com/2220-3206/full/v14/i1/26.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i1.26
Older adults are prone to fall because of their slow response and unstable gait. With the continuous growth of the elderly population, the risk of fracture has increased. Hip fracture is a common type of fracture in older people[1]. Traditional conservative treatment is prone to delay healing and cause muscle atrophy, joint stiffness, and other problems, seriously affecting the quality of life of elderly patients[2]. With the improvement of modern surgical technology, an increasing number of elderly patients with fractures choose surgical treatment[3]. Total hip arthroplasty (THA) has significant advantages in relieving chronic pain and promoting the recovery of hip joint function[4]. However, most elderly patients have chronic diseases, and their tolerance to surgery is poor, so they are prone to various complications in the perioperative period, such as postoperative delirium, cognitive dysfunction, and pressure sores[5]. The occurrence of post
Dexmedetomidine (Dex) is a specific α2 adrenoceptor agonist that is effective for surgical analgesia and sedation[6]. Dex can effectively relief postoperative pain and reduce the stress reaction in elderly patients undergoing medullary joint replacement[7]. Emerging evidence suggests that intraoperative application of Dex can reduce the risk of postoperative delirium and cognitive dysfunction[8]. Remarkably, it has been shown recently that Dex can protect the nervous system by reducing surgical stress and inflammatory responses[9]. Ulinastatin is a trypsin inhibitor that can effectively inhibit the decomposition of many enzymes and the release of inflammatory factors[10]. As reported previously, ulinastatin reduced neuronal apoptosis by inhibiting inflammatory factors such as interleukin (IL)-6 and C-reactive protein (CRP), thus relieving postoperative cognitive impairment and reducing the incidence of postoperative cognitive dysfunction (POCD)[11]. However, it is unclear whether the combination of ulinastatin and Dex can further reduce the incidence of POCD in elderly patients undergoing THA. Therefore, the aim of the current study is to evaluate the effect of ulinastatin combined with Dex on the incidences of POCD and emergence agitation. We also investigated the observer’s assessment of alertness/sedation (OAA/S) scale scores of the elderly patients undergoing THA.
We conducted a three-year (February 2019 to August 2022) retrospective cohort study in Shaanxi Provincial People’s Hospital. Comprehensive demographic data were obtained from the electronic medical record system. The Ethics Committee of the Shaanxi Provincial People’s Hospital permitted this study, which was carried out according to the Declaration of Helsinki. We retrospectively reviewed the medical records of patients who underwent unilateral THA.
The inclusion criteria in this retrospective study were as follows: (1) Patients undergoing THA under general anesthesia in our hospital; (2) Patients aged 65 to 80 years old; (3) Patients with an American Society of Anesthesiologists (ASA) class I-III; and (4) Patients with a body mass index (BMI) 18-25kg/m2. We excluded: (1) Patients with delirium or those diagnosed with dementia, depression, schizophrenia or epilepsy, Parkinson’s disease, hypertension, coronary heart disease, diabetes, severe liver and kidney dysfunction, or hearing impairment in the past; and (2) Patients with severe hepatorenal dysfunction, severe malnutrition, blood coagulation disorders, and immune system diseases.
Preoperative information of qualified patients, including sex, age, BMI, ASA classification, mental disease, and cognitive damage, was obtained from the medical records. Intraoperative statistics were collected from anesthesia records, including anesthesia and surgery method, operation time, intraoperative data, blood loss volume, urine volume, and Dex and ulinastatin dosage. Record the heart rate (HR) and mean arterial pressure (MAP) of three groups of patients before anesthesia, 10 min of anesthesia, and 60 min of anesthesia. Postoperative data, including visual analogue scale (VAS) scores[12] at 24 h after the operation, Ramsay scores, Mini-Mental State Examination (MMSE) scores, OAA/S scale scores, serum CRP and IL-6, were collected. The Ramsay score is 1-6 points, with 1 point indicating restlessness; 2 points: Clear and able to follow commands; 3 points: Sleepy, able to follow instructions; 4 points: Shallow sleep state, able to awaken; 5 points: Call response is slow; 6 points: Deep sleep state, no response; the higher the score, the better the sedative effect. The MMSE score[13] included 10 points for orientation, 9 points for language and spatial structure, 5 points for attention and calculation, 3 points for recognition memory, and 3 points for memory, for a total of 30 points. Those with a score 2 points lower than those before anesthesia were considered to have cognitive impairment. The VAS score was evaluated by a visual analog scale, with a total score of 10. The higher the score, the more severe the pain. The OAA/S sedation score[14] is divided into five levels: Level 1: The patient is unconscious and does not respond to gentle tapping on the body but responds to noxious stimuli. Level 2: The patient’s level of consciousness is vague but consciousness is not wholly lost, and there is no response when the name is called loudly; Level 3: The level of consciousness is vague but consciousness is not wholly lost, and there is a response to tapping the body; Level 4: The patient’s level of consciousness is vague, and there is a response when calling the name; Level 5: The patient is conscious and can respond to the questions asked by the nursing staff.
By examining the patients’ electronic medical records, 576 elderly patients who underwent THA in our hospital from February 2019 to August 2022 were selected. Among them, 129 patients who were administered Dex 0.3 μg/kg/h during the operation were included in the Dex group. One hundred fifty patients who were intravenously injected with 5000 U/kg ulinastatin 15 min before anesthesia were included in the ulinastatin group. During the operation, one hundred eighteen patients who were administered 5000 U/kg ulinastatin (15 min before anesthesia) combined with Dex 0.3 μg/kg/h were included in the Dex + ulinastatin group. Data were evaluated by SPSS 22.0 (IBM Corporation). The categorical data are indicated as n (%), and continuous variables are indicated as the mean ± SD. Continuous variables were compared with one-way ANOVA or the Mann-Whitney U test. Categorical variables were compared with Fisher’s exact test. P < 0.05 was considered statistically significant.
The original investigation of our hospital’s electronic medical system showed that 576 patients underwent THA from February 2019 to August 2022. Fifty-eight patients who were either under age 65 years or over 80 years were disqualified. After excluding 63 patients complicated with severe chronic physical diseases and 58 patients with incomplete data, 397 patients were eligible for this study. A flowchart describing the selection of patients included in this retrospective study is shown in Figure 1.
The Dex cohort (129 cases) consisted of patients who received Dex during the operation. The ulinastatin cohort (150 cases) consisted of patients who received ulinastatin 15 min before anesthesia. In the Dex + ulinastatin group, 118 patients received Dex (during the operation) combined with ulinastatin (15 min before anesthesia). The descriptive statistics between the three cohorts were not statistically significant (all P > 0.05, Table 1).
| Dex group (n = 129) | Ulinastatin group (n = 150) | Dex + ulinastatin group (n = 118) | F/χ2 | P value | |
| Sex, n | 1.240 | 0.092 | |||
| Male | 62 | 74 | 53 | ||
| Female | 67 | 76 | 65 | ||
| Age (yr), mean ± SD | 71.72 ± 2.45 | 71.23 ± 4.91 | 72.25 ± 2.65 | 1.217 | 0.301 |
| Weight (kg), mean ± SD | 59.12 ± 6.90 | 61.21 ± 7.13 | 59.23 ± 6.18 | 0.680 | 0.509 |
| BMI, mean ± SD | 24.80 ± 4.69 | 24.72 ± 5.04 | 24.90 ± 4.82 | 1.207 | 0.304 |
| Intraoperative hypotension, n | 8 | 7 | 9 | 2.447 | 0.099 |
| Marital status, n | 0.669 | 0.095 | |||
| Single | 10 | 7 | 6 | ||
| Married | 119 | 143 | 112 | ||
| ASA classification (level III) | 5 | 6 | 4 | 0.519 | 0.082 |
Table 2 shows no significant difference in operation duration, intraoperative blood loss volume, operation time, preoperative MMSE scores, infusion volume, total blood loss volume, or urine volume among the three groups (all P > 0.05). There were significant differences in VAS scores at 24 h after the operation among the three groups, and the score in the Dex + ulinastatin group was the lowest (P < 0.05).
| Dex group (n = 129) | Ulinastatin group (n = 150) | Dex + ulinastatin group (n = 118) | F value | P value | |
| Intraoperative blood loss (mL) | 33.12 ± 3.75 | 34.27 ± 3.81 | 32.73 ± 3.85 | 2.297 | 0.107 |
| Operation duration (min) | 206.45 ± 36.32 | 201.65 ± 40.03 | 199.85 ± 40.38 | 0.690 | 0.082 |
| Preoperative MMSE score | 28.70 ± 0.82 | 28.84 ± 0.92 | 28.52 ± 0.84 | 0.379 | 0.686 |
| VAS score 24 h after the operation | 3.25 ± 0.37 | 3.30 ± 0.52 | 3.13 ± 0.25 | 3.878 | 0.024 |
| Time of anesthesia (min) | 217.18 ± 42.79 | 220.51 ± 38.94 | 223.35 ± 41.67 | 1.550 | 0.980 |
| Infusion volume (mL) | 1558.72 ± 170.56 | 1489.54 ± 187.46 | 1580.67 ± 191.88 | 0.673 | 0.058 |
| Urine volume (mL) | 174.87 ± 42.57 | 165.38 ± 56.16 | 168.48 ± 58.16 | 1.097 | 0.779 |
Compared with those of the Dex and ulinastatin groups, the MMSE scores of the Dex + ulinastatin group were significantly increased at 1 and 7 d after the operation (all P < 0.05, Table 3 and Figure 2A).
Compared with that in the Dex and ulinastatin groups, the incidence of POCD in the Dex + ulinastatin group significantly decreased at 1 and 7 d after the operation (all P < 0.05, Table 4 and Figure 2B).
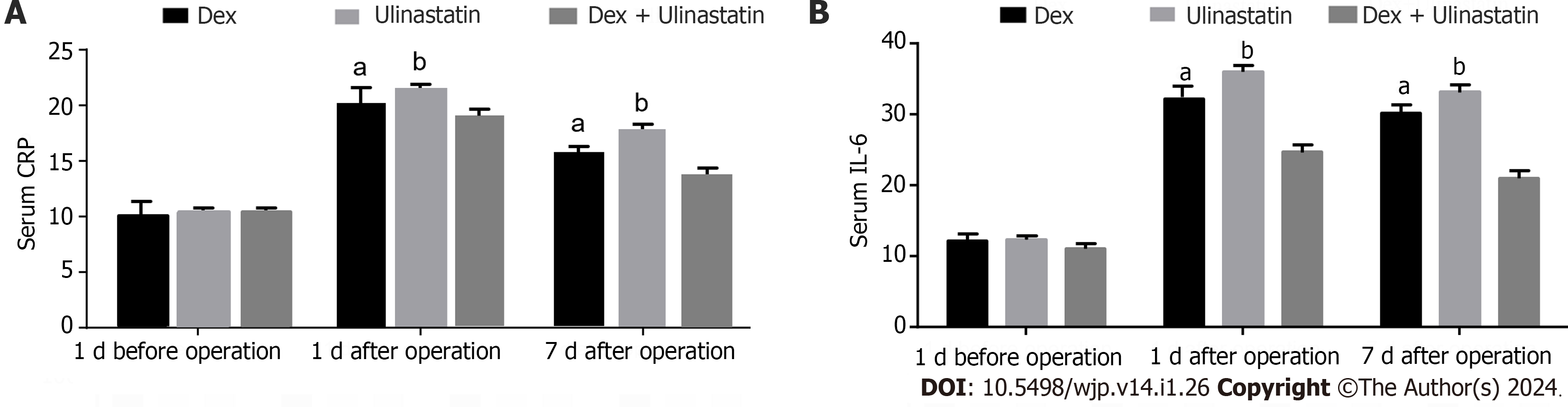
Compared with those in the Dex and ulinastatin groups, the levels of serum inflammatory cytokines (CRP and IL-6) in the Dex + ulinastatin group were significantly decreased at 1 and 7 d after the operation (all P < 0.05, Figure 3).
As shown in Table 5, OAA/S sedation score and Ramsay score of the Dex + ulinastatin group were significantly different from those of the Dex and ulinastatin groups on the first day after the operation (all P < 0.05).
| Dex group (n = 129) | Ulinastatin group (n = 150) | Dex + ulinastatin group (n = 118) | F value | P value | |
| OAA/S sedation score | 3.60 ± 0.61 | 3.51 ± 0.60 | 2.21 ± 0.40 | 9.501 | < 0.001 |
| Ramsay score | 1.98 ± 0.23 | 2.02 ± 0.33 | 3.21 ± 1.02 | 15.698 | < 0.001 |
Compared with those of the Dex and ulinastatin groups, HR and MAP of the Dex + ulinastatin group significantly reduced on the 10 minutes of anesthesia and 60 min of anesthesia (all P < 0.05, Table 6).
| Item | Dex group (n = 129) | Ulinastatin group (n = 150) | Dex + ulinastatin group (n = 118) | F value | P value | |
| HR (times/min) | T0 | 78.02 ± 3.28 | 78.66 ± 3.49 | 78.51 ± 3.64 | 1.140 | 0.323 |
| T1 | 84.32 ± 5.47 | 85.74 ± 5.48 | 81.07 ± 5.55 | 7.084 | 0.001 | |
| T2 | 85.16 ± 5.39 | 86.63 ± 5.73 | 80.39 ± 5.85 | 18.882 | < 0.001 | |
| MAP (mmHg) | T0 | 91.72 ± 8.74 | 92.04 ± 8.38 | 91.69 ± 8.77 | 0.033 | 0.965 |
| T1 | 96.31 ± 7.05 | 97.72 ± 7.37 | 92.11 ± 6.38 | 7.417 | 0.001 | |
| T2 | 95.87 ± 7.85 | 96.48 ± 7.69 | 91.05 ± 7.94 | 8.289 | < 0.001 | |
THA is a standard approach for the surgical treatment of hip paralysis that mainly involves replacement of the damaged hip joint with an artificial hip[15]. The efficacy and safety of THA have improved in recent years. However, patients still have a particular risk of postoperative complications, mainly due to various stress reactions caused by bleeding intraoperatively, performing the operation, and making the surgical incision[16]. Postoperative pain is a common complication after hip arthroplasty, and pain can cause symptoms such as increased HR and high blood pressure[17]. Effective analgesic measures should be taken to prevent various complications caused by postoperative stress reactions[18].
Dex is an α2 receptor agonist with a high affinity for α2 receptors and is often used in sedation therapy in the intensive care unit and surgery. The drug’s half-life is 6 min after intravenous injection, excreted in urine after extensive metabolism, and the clearance half-life is two hours[19]. Because the drug is injected through the kidney, patients with impaired renal function may have more adverse reactions[20]. Therefore, patients with hepatic and renal dysfunction were excluded from this study. Ulinastatin is isolated in and excreted through human urine, and widely used because of its broad spectrum of enzyme inhibition[21]. Previous studies have shown that ulinastatin can inhibit the organic inflammatory response and improve learning and memory dysfunction by reducing the apoptosis of nerve cells, which is beneficial in reducing the incidence of postoperative cognitive impairment in elderly patients[22]. Combining two drugs with the same effect has a synergistic effect. However, the effect of the combination of Dex and ulinastatin on elderly patients undergoing THA remains unknown. Therefore, this retrospective cohort study investigated the effect of Dex combined with ulinastatin on the incidences of POCD and emergence agitation in elderly patients who underwent THA.
As reported previously, ulinastatin has an excellent anti-inflammatory response, reduces the level of inflammatory mediators, relieves postoperative pain, and reduces the postoperative stress response. The clearance rate of the drug in elderly patients is slower than that in young patients, and because the kidney does not metabolize the drug, it can be used even if it the patient has impaired renal function[23]. In this study, we observed that the combination of ulinastatin and Dex could effectively reduce the stress response and improve the quality of life of patients after the operation. The VAS scores of the Dex + ulinastatin group were lower than those of the ulinastatin or Dex group at 24 h after the operation, indicating that the analgesic scheme of ulinastatin combined with Dex could effectively relieve postoperative pain symptoms in elderly patients who underwent total joint replacement. The Ramsay score and OAA/S sedation score mainly reflects the sedation of patients after the operation[24]. In this study, OAA/S sedation score and Ramsay score of the Dex + ulinastatin group were significantly different from those of the Dex and ulinastatin groups on the first day after the operation, meanwhile, compared with those of the Dex and ulinastatin groups, HR and MAP of the Dex + ulinastatin group significantly reduced on the 10 min of anesthesia and 60 min of anesthesia, indicating that preemptive analgesia with ulinastatin combined with Dex could effectively reduce the postoperative stress response and improve the sedation effect.
Previous studies have shown that systemic inflammatory response syndrome caused by surgical trauma, postoperative pain, body stress, and the release of different types of cytokines play an essential role in the development of perioperative neurocognitive impairment[25]. The body’s immune system can be activated by surgical trauma, leading to a robust inflammatory response[26]. Therefore, the levels of inflammatory factors in surgical patients’ central nervous system and peripheral tissues increase. At the same time, surgery can lead to enhanced production of proinflammatory cytokines, such as plasma IL-6 and IL-1β, and the degree of increase is related to the decline in cognitive function[27]. Changes in cerebral oxygenation during THA may cause different degrees of nerve injury and induce POCD[28]. Therefore, how to reduce the incidence of POCD in elderly patients undergoing THA and improve their quality of life in their later years is particularly important. Our results found that compared with those of the Dex and ulinastatin groups, the MMSE scores of the Dex + ulinastatin group were significantly increased at 1 and 7 d after the operation, suggesting that preinjection of Dex and ulinastatin might play a significant role in preventing POCD and that the combined infusion is more helpful in preventing the occurrence of early POCD. A prophylactic combination of Dex and ulinastatin during knee arthroplasty in older adults is beneficial in reducing the incidence of POCD. The possible mechanism is that Dex inhibits excessive stress responses, such as inhibiting the concentration of plasma cortisol and reducing the damage of catecholamines to brain nerves. At the same time, ulinastatin protects the brain by inhibiting the release of proinflammatory cytokines (IL-6 and CRP).
This study also has some limitations. At present, multiscale combined evaluation is recommended for the diagnosis of POCD. This study used the MMSE scale to evaluate cognitive function, and some postoperative patients with cognitive impairment may not have been identified. Therefore, whether there are other mechanisms by which Dex combined with ulinastatin reduces the incidence of POCD in elderly patients undergoing THA should be further studied.
In summary, ulinastatin combined with Dex can reduce the incidence of POCD in elderly patients undergoing THA, and the mechanism may be related to the reduction in plasma levels of CRP and IL-6. In addition, we also observed that applying ulinastatin combined with Dex can reduce postoperative pain and improve the postoperative stress response in elderly patients undergoing THA.
Most elderly patients are prone to various complications in the perioperative period, such as postoperative delirium and cognitive dysfunction. Cognitive dysfunction seriously affects the postoperative rehabilitation of patients, prolongs hospital stay, increases the incidence of postoperative complications and mortality, in addition to a serious decline in personal quality of life, but also increases the burden of the family and society. Many researchers believe that advanced age and “major surgery” are important risk factors for cognitive dysfunction in patients undergoing non-cardiac surgery. Therefore, cognitive dysfunction is an important issue in the medical field at present, and the study of the occurrence factors, pathogenesis, effective prevention, and treatment of cognitive dysfunction is an important topic in the field of anesthesiology.
It is unclear whether the combination of ulinastatin and dexmedetomidine (Dex) can further reduce the incidence of postoperative cognitive dysfunction (POCD) in elderly patients undergoing total hip arthroplasty (THA). Therefore, the current study aims to evaluate the effect of ulinastatin combined with Dex on POCD and emergence agitation. Therefore, solving these problems could effectively improve the postoperative stress response and improve the sedation effect for elderly patients undergoing THA. This is the first study to explore the effect of ulinastatin combined with Dex on POCD and emergence agitation in elderly patients undergoing THA.
In view of the high incidence of POCD in elderly orthopedic patients, this study will compare the effects of different anesthetic methods on the early cognitive function of elderly patients after THA, and explore the related factors, to provide some guidance for the anesthetic mode and anesthetic management of clinical orthopedic surgery in the future. The purpose of this study is to provide clinical basis for the selection of anesthesia in elderly patients undergoing hip arthroplasty.
In this study, we collected the postoperative data, including visual analogue scale (VAS) scores at 24 h after operation, postoperative stress response indicators [Mini-Mental State Examination (MMSE) scores, hemodynamic indexes, observer’s assessment of alertness/sedation (OAA/S) scale and Ramsay score], inflammatory cytokines [C-reactive protein (CRP) and interleukin (IL)-6]. A total of 129 patients administrated with Dex 0.3 μg/kg/h during the operation were included in the Dex group. One hundred fifty patients who were intravenously injected 5000 U/kg of ulinastatin 15 min before anesthesia were included in the ulinastatin group. One hundred eighteen patients who were administrated with 5000 U/kg of ulinastatin (15 min before anesthesia) combined with Dex 0.3 μg/kg/h during the operation were included in the Dex + ulinastatin group.
The findings of this study demonstrated that ulinastatin combined with Dex could reduce the incidence of POCD in elderly patients undergoing THA, and the mechanism might be associated with the lessening of plasma levels of CRP and IL-6. Moreover, the combination of ulinastatin and Dex can reduce postoperative pain and postoperative stress response in elderly patients undergoing THA. Our results validated that the combination therapy can effectively improve the cognitive function of nervous system after operation and improved the quality of life for patients.
This is the first study explored the efficacy of ulinastatin combined with Dex on POCD and emergence agitation in elderly patients undergoing THA. We collected the postoperative data, including VAS scores at 24 h after operation, postoperative stress response indicators (MMSE scores, hemodynamic indexes, OAA/S scale, CRP, and IL-6). The results of this study not only demonstrate that combination therapy can reduce postoperative cognitive impairment, but also find that the mechanism may be related to the reduction of plasma levels of CRP and IL-6.
In future research, we will focus on the specific mechanisms related to the combined therapy through in vitro and in vivo experiments.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Trzeciak P, Poland; Yirci R, Turkey S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | Meinberg E, Ward D, Herring M, Miclau T. Hospital-based Hip fracture programs: Clinical need and effectiveness. Injury. 2020;51 Suppl 2:S2-S4. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Pech-Ciau BA, Lima-Martínez EA, Espinosa-Cruz GA, Pacho-Aguilar CR, Huchim-Lara O, Alejos-Gómez RA. [Hip fracture in the elderly: epidemiology and costs of care]. Acta Ortop Mex. 2021;35:341-347. [PubMed] [Cited in This Article: ] |
| 3. | Alexiou KI, Roushias A, Varitimidis SE, Malizos KN. Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging. 2018;13:143-150. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Scott CEH, Clement ND, Davis ET, Haddad FS. Modern total hip arthroplasty: peak of perfection or room for improvement? Bone Joint J. 2022;104-B:189-192. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Stibolt RD Jr, Patel HA, Huntley SR, Lehtonen EJ, Shah AB, Naranje SM. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: A systematic review of characteristics, outcomes, and complications. Chin J Traumatol. 2018;21:176-181. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Wen G, Xin N. Dexmetomidine promotes the activity of breast cancer cells through miR-199a/HIF-1α axis. Transl Cancer Res. 2021;10:4817-4828. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Li X, Li X, Wang R, Hua T, Li G. Application of dexmetomidine in gynecological laparoscopic surgery and its effect on S-100 β protein and cognitive function in patients. Minerva Med. 2022;113:599-601. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Deiner S, Luo X, Lin HM, Sessler DI, Saager L, Sieber FE, Lee HB, Sano M; and the Dexlirium Writing Group, Jankowski C, Bergese SD, Candiotti K, Flaherty JH, Arora H, Shander A, Rock P. Intraoperative Infusion of Dexmedetomidine for Prevention of Postoperative Delirium and Cognitive Dysfunction in Elderly Patients Undergoing Major Elective Noncardiac Surgery: A Randomized Clinical Trial. JAMA Surg. 2017;152:e171505. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Muñoz-Leyva F, Jack JM, Bhatia A, Chin KJ, Gandhi R, Perlas A, Jin R, Chan V. No Benefits of Adding Dexmedetomidine, Ketamine, Dexamethasone, and Nerve Blocks to an Established Multimodal Analgesic Regimen after Total Knee Arthroplasty. Anesthesiology. 2022;137:459-470. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Lv B, Jiang XM, Wang DW, Chen J, Han DF, Liu XL. Protective Effects and Mechanisms of Action of Ulinastatin against Cerebral Ischemia-Reperfusion Injury. Curr Pharm Des. 2020;26:3332-3340. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Zhang YH, Guo XH, Zhang QM, Yan GT, Wang TL. Serum CRP and urinary trypsin inhibitor implicate postoperative cognitive dysfunction especially in elderly patients. Int J Neurosci. 2015;125:501-506. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Han Y, Wang M, Shen J, Zhang Z, Zhao M, Huang J, Chen Y, Chen Z, Hu Y, Wang Y. Differential efficacy of methylcobalamin and alpha-lipoic acid treatment on symptoms of diabetic peripheral neuropathy. Minerva Endocrinol. 2018;43:11-18. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Lauretani F, Ticinesi A, Gionti L, Prati B, Nouvenne A, Tana C, Meschi T, Maggio M. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exp Res. 2019;31:1435-1442. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Lim TW, Choi YH, Kim JY, Choi JB, Lee SK, Youn EJ, Lee JS. Efficacy of the bispectral index and Observer's Assessment of Alertness/Sedation Scale in monitoring sedation during spinal anesthesia: A randomized clinical trial. J Int Med Res. 2020;48:300060519893165. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Flevas DA, Tsantes AG, Mavrogenis AF. Direct Anterior Approach Total Hip Arthroplasty Revisited. JBJS Rev. 2020;8:e0144. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Moerenhout K, Derome P, Laflamme GY, Leduc S, Gaspard HS, Benoit B. Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Can J Surg. 2020;63:E412-E417. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Goh GS, Parvizi J. Nerve Injuries Following Total Hip Arthroplasty: The Influence of Surgical Approach. Orthop Clin North Am. 2022;53:129-137. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Urish KL, Giori NJ, Lemons JE, Mihalko WM, Hallab N. Trunnion Corrosion in Total Hip Arthroplasty-Basic Concepts. Orthop Clin North Am. 2019;50:281-288. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Persson NDÅ, Uusalo P, Nedergaard M, Lohela TJ, Lilius TO. Could dexmedetomidine be repurposed as a glymphatic enhancer? Trends Pharmacol Sci. 2022;43:1030-1040. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Eizaga Rebollar R, García Palacios MV, Fernández Riobó MC, Torres Morera LM. Dexmedetomidine and perioperative analgesia in children. Rev Esp Anestesiol Reanim (Engl Ed). 2022;69:487-492. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Wei X, Zhu X, Jiang L, Long M, Du Y. Recent research progress on the role of ulinastatin in chronic kidney disease. Nephrology (Carlton). 2021;26:708-714. [PubMed] [DOI] [Cited in This Article: ] |
| 22. | Chen L, Jin S, Yang M, Gui C, Yuan Y, Dong G, Zeng W, Zeng J, Hu G, Qiao L, Wang J, Xi Y, Sun J, Wang N, Wang M, Xing L, Yang Y, Teng Y, Hou J, Bi Q, Cai H, Zhang G, Hong Y, Zhang Z. Integrated Single Cell and Bulk RNA-Seq Analysis Revealed Immunomodulatory Effects of Ulinastatin in Sepsis: A Multicenter Cohort Study. Front Immunol. 2022;13:882774. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Hong Y, Meng S, Wang S, Liu T, Liu J. Ulinastatin Alleviates Repetitive Ketamine Exposure-Evoked Cognitive Impairment in Adolescent Mice. Neural Plast. 2022;2022:6168284. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Sieber F, Neufeld K, Oh ES, Gottschalk A, Wang NY. Effect of baseline cognitive impairment on association between predicted propofol effect site concentration and Bispectral index or sedation score. BMC Anesthesiol. 2020;20:129. [PubMed] [DOI] [Cited in This Article: ] |
| 25. | Liao YL, Zhou XY, Ji MH, Qiu LC, Chen XH, Gong CS, Lin Y, Guo YH, Yang JJ. S100A9 Upregulation Contributes to Learning and Memory Impairments by Promoting Microglia M1 Polarization in Sepsis Survivor Mice. Inflammation. 2021;44:307-320. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | Bortolotti P, Faure E, Kipnis E. Inflammasomes in Tissue Damages and Immune Disorders After Trauma. Front Immunol. 2018;9:1900. [PubMed] [DOI] [Cited in This Article: ] |
| 27. | Wang J, Zhou Y, Li K, Li X, Guo M, Peng M. A Noradrenergic Lesion Attenuates Surgery-Induced Cognitive Impairment in Rats by Suppressing Neuroinflammation. Front Mol Neurosci. 2021;14:752838. [PubMed] [DOI] [Cited in This Article: ] |
| 28. | Lin R, Zhang F, Xue Q, Yu B. Accuracy of regional cerebral oxygen saturation in predicting postoperative cognitive dysfunction after total hip arthroplasty: regional cerebral oxygen saturation predicts POCD. J Arthroplasty. 2013;28:494-497. [PubMed] [DOI] [Cited in This Article: ] |