Published online Apr 28, 2022. doi: 10.3748/wjg.v28.i16.1692
Peer-review started: December 10, 2021
First decision: January 27, 2022
Revised: February 7, 2022
Accepted: March 16, 2022
Article in press: March 16, 2022
Published online: April 28, 2022
Acute gallstone pancreatitis (AGP) is the most common cause of acute pancreatitis (AP) in the United States. Patients with AGP may also present with choledocholithiasis. In 2010, the American Society for Gastrointestinal Endoscopy (ASGE) suggested a management algorithm based on probability for choledocholithiasis, recommending additional imaging for patients at intermediate risk and endoscopic retrograde cholangiopancreatography (ERCP) for patients at high risk of choledocholithiasis. In 2019, the ASGE guidelines were updated using more specific criteria to categorize individuals at high risk for choledocholithiasis. Neither ASGE guideline has been studied in AGP to determine the probability of having choledocholithiasis.
To determine compliance with ASGE guidelines, assess outcomes, and compare 2019 vs 2010 ASGE criteria for suspected choledocholithiasis in AGP.
We conducted a retrospective cohort study of 882 patients admitted with AP to a single tertiary care center from 2008-2018. AP was diagnosed using revised Atlanta criteria and AGP was defined as the presence of gallstones on imaging or with cholestatic pattern of liver injury in the absence of another cause. Patients with chronic pancreatitis and pancreatic malignancy were excluded as were those who went directly to cholecystectomy prior to assessment for choledocholithiasis. Patients were assigned low, intermediate or high risk based on ASGE guidelines. Our primary outcomes of interest were the proportion of patients in the intermediate risk group undergoing magnetic resonance cholangiopancreatography (MRCP) first and the proportion of patients in the high risk group undergoing ERCP directly without preceding imaging. Secondary outcomes of interest included outcome differences based on if guidelines were not adhered to. We then evaluated the diagnostic accuracy of 2019 in comparison to the 2010 ASGE criteria for patients with suspected choledocholithiasis. We performed the t test or Wilcoxon rank sum test, as appropriate, to analyze if there were outcome differences based on if guidelines were not adhered to. Kappa coefficients were calculated to measure the degree of agreement between pairs of variables.
In this cohort, we identified 235 patients with AGP of which 79 patients were excluded as they went directly to surgery for cholecystectomy without prior MRCP or ERCP. Of the remaining 156 patients, 79 patients were categorized as intermediate risk and 77 patients were high risk for choledocholithiasis according to the 2010 ASGE guidelines. Among 79 intermediate risk patients, 54 (68%) underwent MRCP first whereas 25 patients (32%) went directly to ERCP. For the 54 patients with intermediate risk who had MRCP first, 36 patients had no choledocholithiasis while 18 patients had evidence of choledocholithiasis prompting ERCP. Of these patients, ERCP confirmed stone disease in 11 patients. Of the 25 intermediate risk patients who directly underwent ERCP, 18 patients had stone disease. One patient with a normal ERCP developed post ERCP pancreatitis. Patients undergoing MRCP in this group had a significantly longer length of stay (5.0 vs 4.0 d, P = 0.02). In the high risk group, 64 patients (83%) had ERCP without preceding imaging, of which, 53 patients had findings consistent with choledocholithiasis, of which 13 patients (17%) underwent MRCP before ERCP, all of which showed evidence of stone disease. Furthermore, all of these patients ultimately had an ERCP, of which 8 patients had evidence of stones and 5 had normal examination.
Our cohort also demonstrated that 58% of all 156 patients with AGP had confirmed choledocholithiasis (79% of the high risk group and 37% of the intermediate group when risk was assigned based on the 2010 ASGE guidelines). When the updated 2019 ASGE guidelines were applied instead of the original 2010 guidelines, there was moderate agreement between the 2010 and 2019 guidelines (kappa = 0.46, 95%CI: 0.34-0.58). Forty-two of 77 patients were still deemed to be high risk and 35 patients were downgraded to intermediate risk. Thirty-five patients who were originally assigned high risk were reclassified as intermediate risk. For these 35 patients, 26 patients had ERCP findings consistent with choledocholithiasis and 9 patients had a normal examination. Based on the 2019 criteria, 9/35 patients who were downgraded to intermediate risk had an unnecessary ERCP with normal findings (without a preceding MRCP).
Two-thirds in intermediate risk and 83% in high risk group followed ASGE guidelines for choledocholithiasis. One intermediate-group patient with normal ERCP had post-ERCP AP, highlighting the risk of unnecessary procedures.
Core Tip: We demonstrated that more than half of patients with acute gallstone pancreatitis (AGP) have choledocholithiasis. We also found that approximately 2/3 of patients in the intermediate group and 83% of patients in the high risk group followed American Society for Gastrointestinal Endoscopy guidelines for management of choledocholithiasis in the setting of AGP. There was associated longer length of stay for patients undergoing magnetic resonance cholangiopancreatography (MRCP) in both groups. Importantly, one patient who had a normal endoscopic retrograde cholangiopancreatography (ERCP) in the intermediate group without preceding MRCP suffered from post ERCP pancreatitis, highlighting the risk of unnecessary procedures.
- Citation: Tintara S, Shah I, Yakah W, Ahmed A, Sorrento CS, Kandasamy C, Freedman SD, Kothari DJ, Sheth SG. Evaluating the accuracy of American Society for Gastrointestinal Endoscopy guidelines in patients with acute gallstone pancreatitis with choledocholithiasis. World J Gastroenterol 2022; 28(16): 1692-1704
- URL: https://www.wjgnet.com/1007-9327/full/v28/i16/1692.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i16.1692
Acute gallstone pancreatitis (AGP) is the most common cause of acute pancreatitis (AP) in the United States[1]. Patients with AGP may also present with choledocholithiasis as the occurrence of common bile duct (CBD) stones is present in up to 15% of patients with gallstones[2]. The diagnosis of choledocholithiasis is challenging and requires a high degree of suspicion as it often cannot be made conclusively without invasive procedures like endoscopic retrograde cholangiopancreatography (ERCP)[3]. In 2010, the American Society for Gastrointestinal Endoscopy (ASGE) suggested a management algorithm based on probability for choledocholithiasis to assist in risk stratifying patients[4]. These guidelines stratify patients into those with high, intermediate, and low risk based on clinical criteria, liver tests, and abdominal ultrasound. High risk (> 50% probability of choledocholithiasis) is defined as the presence of any very strong predictor (clinical ascending cholangitis, CBD stone seen on ultrasound, and/or total bilirubin > 4 mg/dL) or the presence of both strong predictors (CBD dilated more than 6 mm and bilirubin 1.8-4 mg/dL). Intermediate risk (10%-50% probability of choledocholithiasis) is defined as presence of age > 55, clinical gallstone pancreatitis, any other abnormal liver test. Finally, low risk patients do not have any of these features[4].
These guidelines aim to provide evidence-based recommendations with the goal of optimizing the efficacy and safety of patient care by minimizing the morbidity and cost from unnecessary invasive biliary evaluation. Furthermore, they recommend imaging [i.e. magnetic resonance cholangiopancreatography (MRCP) or endoscopic ultrasound (EUS)] for patients with intermediate risk and ERCP for patients with high probability of choledocholithiasis[4].
In 2019, the ASGE guidelines were updated using more specific criteria to categorize individuals at high-risk for choledocholithiasis[5]. These updated criteria propose that high-risk patients are those with elevated total bilirubin > 4 mg/dL and dilated CBD. The presence of only elevated total bilirubin > 4 or total bilirubin 1.8-4 with dilated CBD are no longer in the criteria for the high-risk group. These guidelines still recommend ERCP for those with high risk and imaging (MRCP or EUS) for those with intermediate risk for choledocholithiasis[6]. Additionally, clinical gallstone pancreatitis was removed as one of the criteria for assigning intermediate risk[6].
Neither ASGE guideline has been studied in AGP to determine the probability of having choledocholithiasis. Thus, our study aimed to determine the true incidence of choledocholithiasis in patients with AGP and determine compliance with the guidelines at our institution and assess outcomes when guidelines were not adhered to. In our patient population of AGP, we also evaluated the performance and diagnostic accuracy of 2019 vs 2010 ASGE criteria for suspected choledocholithiasis in patients with AGP.
This retrospective observational cohort study was approved by Beth Israel Deaconess Medical Center institutional review board. This manuscript adheres to the applicable STROBE reporting guidelines for cohort studies.
We performed a review of all adult (age > 18) patients with a discharge diagnosis of AP who were admitted to our tertiary center between January 1, 2008 and December 31, 2018. The diagnosis of AP was confirmed by a review of the electronic medical record to ensure all patients met the 2012 Revised Atlanta Criteria for the diagnosis of AP (at least two of the following three criteria: epigastric pain, elevation of serum lipase level > three times the upper limit of normal, and/or evidence of pancreatitis on cross-sectional imaging)[7]. Patients with chronic pancreatitis or known pancreatic malignancy were excluded from the study. AGP was defined as the presence of gallstones on imaging or with cholestatic pattern of liver injury in the absence of another cause. Patients who directly went to surgery for cholecystectomy without having either MRCP or ERCP were excluded.
Several parameters including demographic, clinical, laboratory, and radiologic data of the study population were collected. The severity of AP was defined based on the 2012 Revised Atlanta Criteria with mild defined as AP without any local or systemic complications, moderately severe as AP with transient (< 48 h) end-organ failure with or without local complications), and severe as AP with persistent (> 48 h) end-organ damage with or without local complications)[7]. The severity of AP in each patient was also characterized based on the bedside index for severity of AP (BISAP) score[8,9].
Our cohort of interest was divided based on their risk for choledocholithiasis. These included: low, intermediate or high risk based on the 2010 ASGE guidelines. Since the guidelines defined AGP as at least intermediate risk, no patients were in the low risk category, thus leaving only two groups. We then compared demographic characteristics, comorbidities, and outcomes between the two groups.
Our primary outcomes of interest were the proportion of patients in the intermediate risk group undergoing MRCP first and the proportion of patients in the high risk group undergoing ERCP directly without preceding imaging. Secondary outcomes of interest included outcome differences based on if guidelines were not adhered to. We then evaluated the diagnostic accuracy of the 2019 in comparison to the 2010 ASGE criteria for patients with suspected choledocholithiasis. Additionally, we calculated the sensitivity and specificity of the 2010 and 2019 ASGE guidelines for patients categorized as high risk and intermediate risk for choledocholithiasis. Evidence of choledocholithiasis on ERCP was used as the gold standard for true positives.
All data analysis was performed using R software (version 3.6.1, R Core Team 2018a) within RStudio (version 1.1463, RStudio, Inc) via the tidyverse (Wickham, 2017) package. Continuous variables were presented as means with range and standard deviation. These were analyzed using the t-test or Wilcoxon rank sum test, as appropriate. Categorical variables were presented as frequencies (%) and analyzed using the Pearson χ2 test or Fisher’s exact test, as deemed appropriate. Univariate analyses comparing several characteristics and outcomes between the two groups were performed. A significant P value was assigned at 0.05. To determine concordance between the 2019 and 2010 guidelines, Kappa coefficients were calculated to measure the degree of agreement between pairs of variables.
In our cohort, 882 patients with AP were hospitalized of which 235 patients had AGP. Seventy-nine patients were excluded as they went directly to surgery for cholecystectomy without prior MRCP or ERCP. These 79 patients had mild AP with resolution of abdominal pain and rapid normalization of liver enzymes suggesting that CBD stones had likely already passed. Moreover, these patients had abdominal ultrasound that showed normal size CBD. Thus, these patients directly underwent cholecystectomy without preceding ERCP or MRCP.
Of the remaining 156 patients, 79 patients were categorized as intermediate risk (Tables 1 and 2) and 77 patients were high risk (Tables 3 and 4) for choledocholithiasis according to the 2010 ASGE guidelines.
| Number of patients meeting criteria | |
| Dilated common bile duct greater than 6 mm or total bilirubin 1.8-4.0 mg/dL (only one) | 22 |
| Abnormal liver biochemical other than bilirubin | 73 |
| Age greater than 55 yr | 45 |
| Acute gallstone pancreatitis | 79 |
| Number of patients | |
| 1 criterion | 0 |
| 2 criteria | 1 |
| 3 criteria | 45 |
| 4 criteria | 33 |
| Numbers patients meeting criteria | |
| Cholangitis | 1 |
| Common bile duct stone on imaging | 12 |
| Total Bilirubin greater than 4.0 mg/dL | 38 |
| Dilated common bile duct greater than 6 mm and total bilirubin 1.8-4.0 mg/dL | 31 |
| Number of patients | |
| 1 criterion | 75 |
| 2 criteria | 2 |
| 3 criteria | 0 |
| 4 criteria | 0 |
Baseline characteristics and demographics are summarized in Table 5. When comparing demographics between the intermediate risk and high risk groups, there was no difference in age, gender, race, Charlson Comorbidity Index, severity of pancreatitis and baseline BISAP. Patients in the high risk group had a higher BMI than those in the intermediate group (29.0 vs 29.6, P = 0.05). While most of the baseline laboratory data were similar in both groups, total bilirubin was significantly higher in the high risk group (4.04 mg/dL vs 1.32 mg/dL, P < 0.01). Further, alanine aminotransferase and alkaline phosphatase were higher in the high risk groups and approached significance (335 IU/L vs 241 IU/L, P = 0.06 and 196 IU/L vs 156 IU/L, P = 0.07, respectively) (Table 5).
| Intermediate risk (n = 79) | High risk (n = 77) | P value | |
| Age (yr) mean ± SD | 58.6 ± 19.2 | 58.1 ± 17.3 | 0.86 |
| BMI (kg/m2) mean ± SD | 29.0 ± 6.83 | 29.6 ± 9.82 | 0.05 |
| Female | 44 (60%) | 45 (58%) | 0.95 |
| Race | 0.70 | ||
| White | 50 (72%) | 51 (68%) | |
| Black | 15 (22%) | 15 (20%) | |
| Other | 4 (6%) | 9 (12%) | |
| Charlson Comorbidity Index | 0.60 | ||
| 0 | 17 (23%) | 19 (25%) | |
| 1 to 2 | 24 (33%) | 20 (26%) | |
| 3 to 5 | 21 (29%) | 29 (38%) | |
| 6 and above | 11 (15%) | 9 (12%) | |
| Baseline laboratory | |||
| Creatinine (mg/dL) mean ± SD | 0.98 ± 0.55 | 0.94 ± 0.68 | 0.71 |
| White blood cell count (K/L) mean ± SD | 11.4 ± 4.64 | 12.1 ± 7.27 | 0.49 |
| Lactate (mmol/L) mean ± SD | 1.60 ± 1.33 | 1.75 ± 1.44 | 0.63 |
| Lipase (IU/L) mean ± SD | 4012 ± 5264 | 3576 ± 4699 | 0.60 |
| ALT (IU/L) mean ± SD | 241 ± 269 | 335 ± 324 | 0.06 |
| AST (IU/L) mean ± SD | 232 ± 280 | 294 ± 269 | 0.18 |
| Alkaline phosphatase (IU/L) mean ± SD | 156 ± 130 | 196 ± 140 | 0.07 |
| Total bilirubin (mg/dL) mean ± SD | 1.32 ± 0.78 | 4.04 ± 2.06 | < 0.01 |
| Presence of gallstone on imaging | 79 (100%) | 77 (100%) | 0.91 |
| Severity of pancreatitis | |||
| Mean BISAP ± SD | 0.90 ± 0.91 | 0.88 ± 0.88 | 0.90 |
| Modified Atlanta Criteria | 0.13 | ||
| Mild | 57 (72%) | 63 (83%) | |
| Moderate | 21 (27%) | 10 (13%) | |
| Severe | 1 (1%) | 3 (4%) |
Seventy-nine patients were assigned to have intermediate risk of choledocholithiasis based on the 2010 ASGE criteria. In this group, 45 were older than 55 years-old, 73 had abnormal liver tests and 22 had dilated CBD or total bilirubin of 1.8-4.0mg/dL (Table 1). Thirty-three patients met all 4 criteria for intermediate risk group, while 45 patients met 3 criteria, 1 patient met 2 criteria and no patients met only 1 criterion (Table 2).
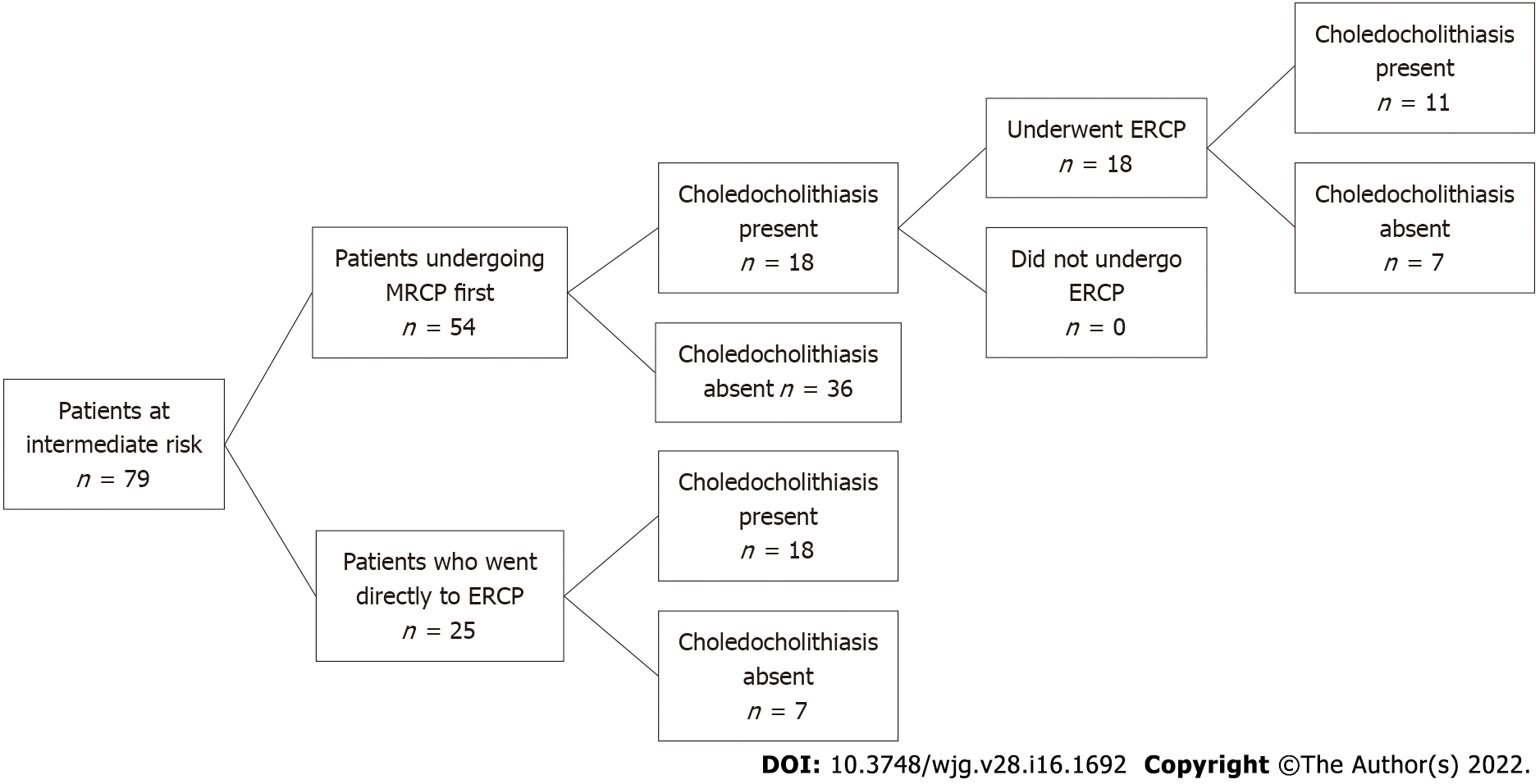
Among 79 intermediate risk patients, 54 (68%) underwent MRCP first whereas 25 patients (32%) went directly to ERCP (Figure 1). For the 54 patients with intermediate risk who had MRCP first, 18 patients had evidence of choledocholithiasis prompting ERCP, while 36 patients had imaging that did not show choledocholithiasis. Of the 18 patients undergoing ERCP after MRCP, 11 patients had choledocholithiasis, whereas 7 patients had normal examinations. There were no complications from ERCP noted in this group.
Of the 25 intermediate risk patients who directly underwent ERCP, 18 patients had choledocholithiasis whereas 7 patients had a normal ERCP (Figure 1). Notably, one of these patients with a normal ERCP developed post ERCP pancreatitis. Patients undergoing MRCP first in this group had a significantly longer length of stay (LOS, 5.0 vs 4.0 d, P = 0.02). They also had higher incidence of pancreatic necrosis (33% vs 8%, P = 0.03) and higher rate of 1-year readmission (52% vs 20%, P = 0.02) (Table 6). There were multiple causes of readmissions in our cohort such as diverticulitis, autonomic dysfunction, pneumonia and urinary tract infection. The 1-year readmission rates for recurrence of acute gallstone pancreatitis or choledocholithiasis were 9% for patients who had MRCP first and 8% for those who directly underwent ERCP, likely because some of them refused or did not undergo cholecystectomy.
| Intermediate risk (n = 79) | High risk (n = 77) | |||||
| Outcomes | ERCP first (n = 25) | MRCP first (n = 54) | P value | ERCP first (n = 64) | MRCP first (n = 13) | P value |
| Mean length of stay (Q1; Q3) | 4.00 (2.74; 5.00) | 5.00 (4.00; 8.00) | 0.02 | 3.00 (2.54; 5.00) | 4.38 (4.00; 6.00) | 0.08 |
| 30-d readmission (%) | 3 (12.0%) | 11 (20.8%) | 0.53 | 6 (9.52%) | 2 (16.7%) | 0.61 |
| 1-yr readmission (%) | 5 (20.0%) | 28 (51.9%) | 0.02 | 19 (29.7%) | 7 (53.8%) | 0.11 |
| 1-yr mortality (%) | 0 (0.00%) | 1 (1.85%) | 0.09 | 1 (1.56%) | 0 (0.00%) | 1.00 |
| Pancreas necrosis (%) | 2 (8.0%) | 18 (33.3%) | 0.03 | 6 (10.7%) | 3 (35.0%) | 0.19 |
| Days to enteral nutrition (Q1; Q3) | 2.00 (1.00; 2.50) | 2.50 (1.00; 4.00) | 0.16 | 2.00 (1.00; 2.00) | 3.00 (2.00; 4.00) | 0.10 |
Seventy-seven patients were assigned to have high risk of choledocholithiasis based on the 2010 ASGE criteria. In this group, 1 patient was suspected to have cholangitis, 38 patients had total bilirubin > 4.0 mg/dL, 12 patients had CBD stone on imaging, and 31 patients had dilated CBD with total bilirubin 1.8-4.0 mg/dL (Table 3). Seventy-five patients met 1 criterion for high risk group and 2 patients met 2 criteria. No patient met 3 or more criteria (Table 4).
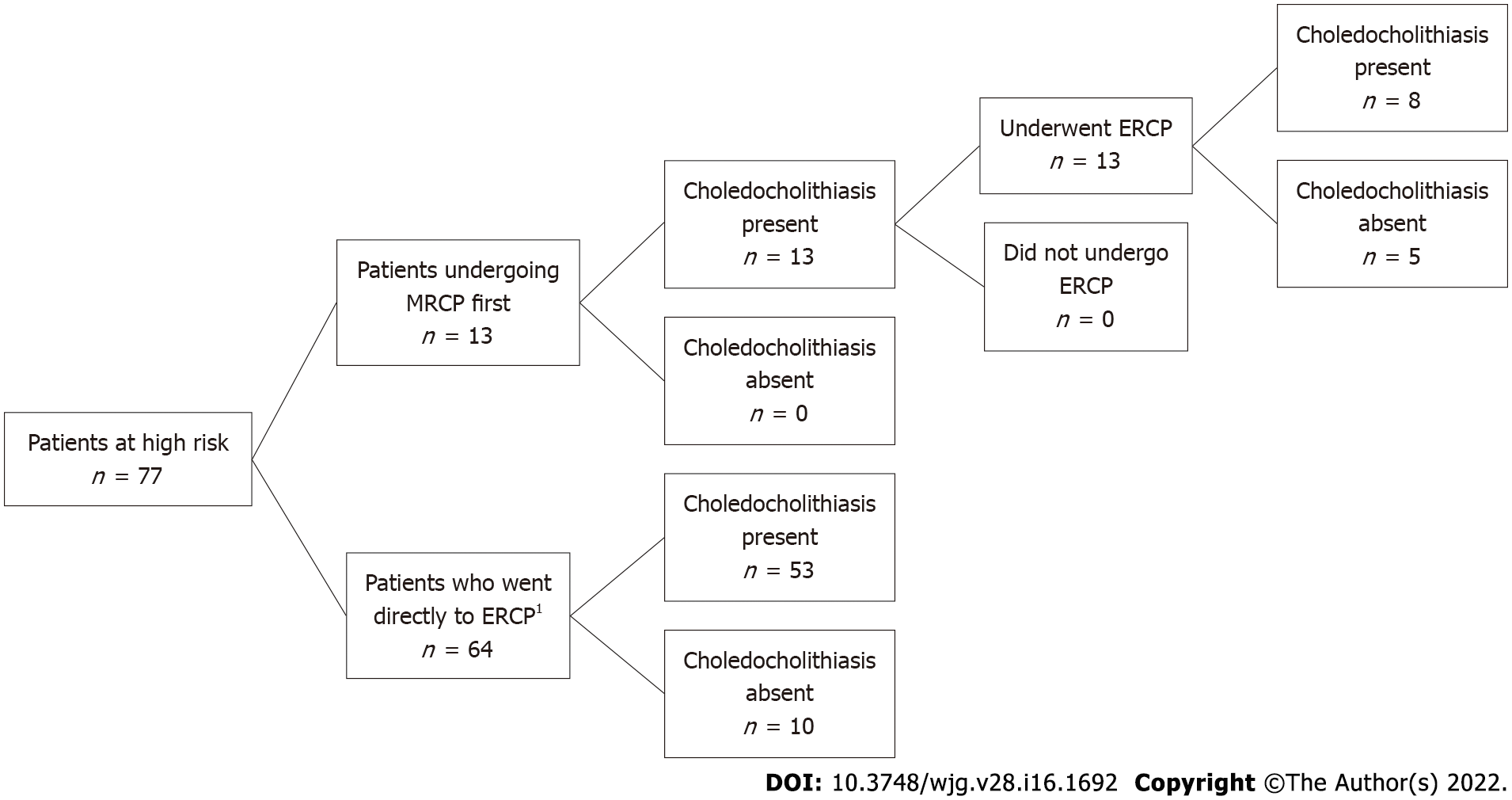
In this group, 64 patients (83%) had ERCP without preceding imaging, of which, 53 patients had findings consistent with choledocholithiasis (27 patients with stones and 26 patients with sludge) while 10 had a normal examination (Figure 2). In comparison, 13 patients in this group (17%) underwent MRCP before ERCP, all of which showed evidence of stone disease. Furthermore, all of these patients ultimately had an ERCP, of which 8 patients had evidence of choledocholithiasis and 5 had normal examination (Figure 2). Two of the 13 patients who underwent imaging first due to altered luminal anatomy and body habitus. For the remaining 11 patients, there was no identifiable reason for not directly proceeding to ERCP.
As with the intermediate group, for the high risk group, the MRCP-first group had longer LOS compared to ERCP-first group which approached significance (4.28 vs 3.00 days, P = 0.08). There were no significant differences in outcomes such as readmission rate, 1-year mortality between the two groups (Table 6).
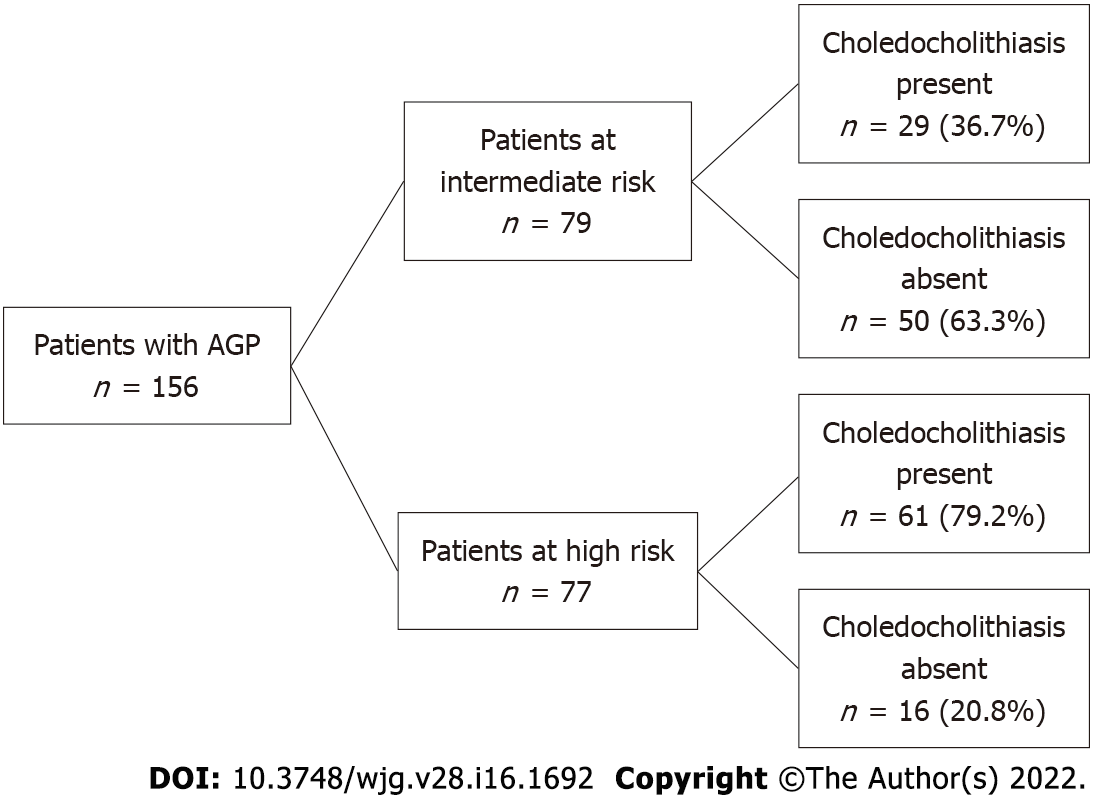
Our cohort also demonstrated that of all 156 patients with AGP, 90 (58%) were found to have choledocholithiasis on ERCP. When stratified by assigned choledocholithiasis risk based on the 2010 ASGE guidelines, 61 of 77 patients in the high risk group (79%) and 29 of 79 patients in the intermediate risk group (37%) were found to have choledocholithiasis (Figure 3).
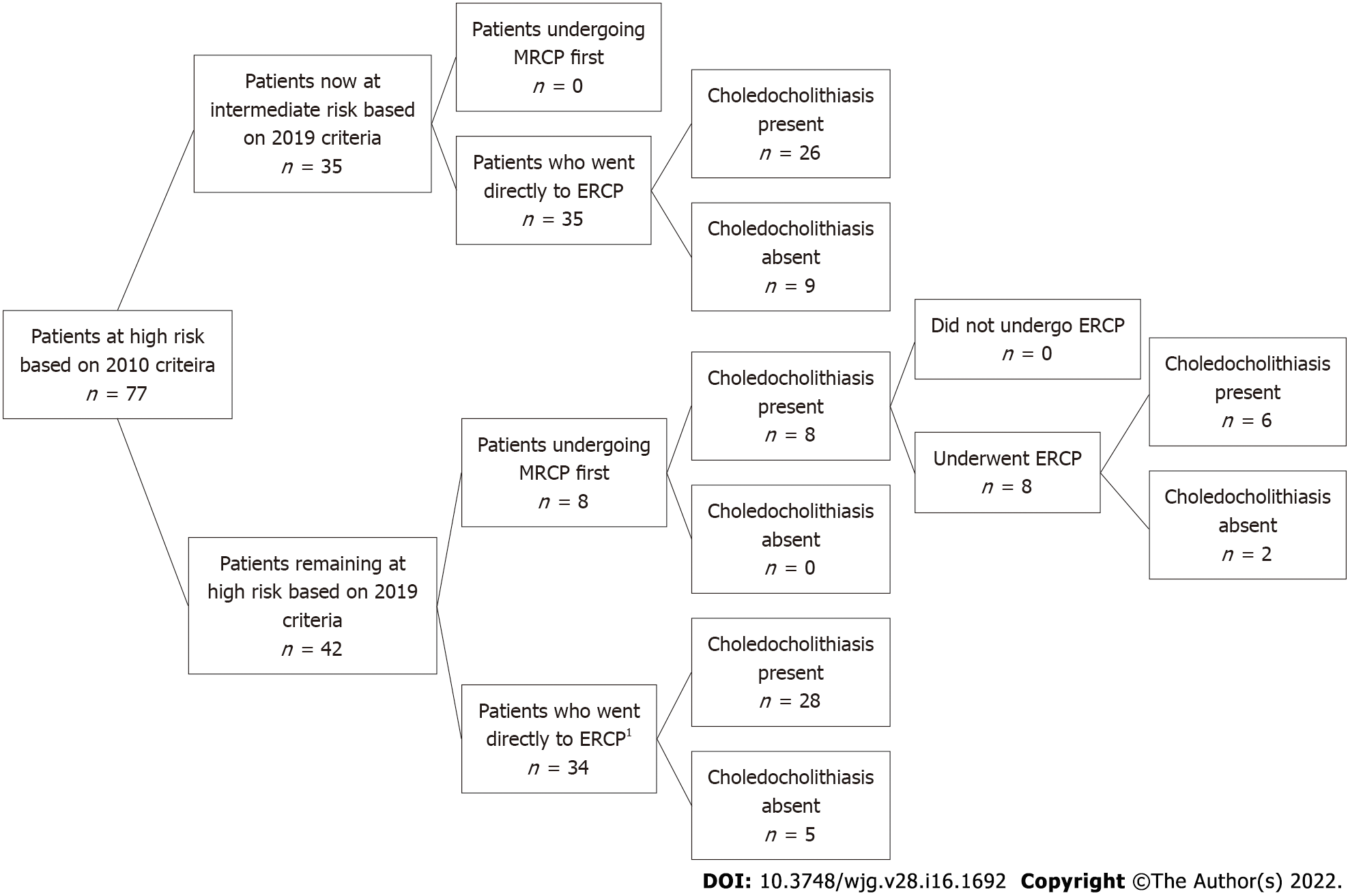
Our cohort of patients was admitted to the hospital between 2008 and 2018, thus the 2010 ASGE guideline were used in the above analysis. We then applied the 2019 criteria to this group to see how results may have changed. There was moderate agreement between the classifications by the 2010 and 2019 guidelines (kappa = 0.46, 95%CI: 0.34-0.58). When the 2019 ASGE guidelines were applied to our 79 patients with intermediate risk for choledocholithiasis, all of these patients were still assigned intermediate risk. Among the 77 patients in the high risk group, when the updated 2019 ASGE guidelines were applied instead of the original 2010 guidelines, 42 patients were still deemed to be high risk and 35 patients were downgraded to intermediate risk. In the high risk group, 34 of 42 who still remained high risk went directly to ERCP of which showed 28 patients had a confirmatory findings of choledocholithiasis and 5 patients had a normal examination (Figure 4).
Thirty-five patients who were originally assigned high risk were then reclassified as intermediate risk (Figure 4). For these 35 patients, 26 patients had ERCP findings consistent with choledocholithiasis and 9 patients had a normal examination. In further review of those patients with a normal ERCP, 5 patients had a bilirubin of > 4 mg/dL and 4 patients had a dilated CBD and a bilirubin of 1.8 to 4 mg/dL. Hence, based on the 2019 criteria, 9 out of 35 patients who were downgraded to intermediate risk had an unnecessary ERCP with normal findings (without a preceding MRCP).
Finally, the sensitivity and specificity of the 2010 and 2019 ASGE guidelines in assessing choledocholithiasis were calculated (Tables 7-10). In our cohort of patients with AGP, the 2010 ASGE criteria for predicting high risk for choledocholithiasis had a sensitivity of 67.8% and specificity of 75.8%. On the other hand, the 2019 ASGE criteria for predicting high risk for choledocholithiasis had a sensitivity of 38.2% and specificity of 89.4%.
| Choledocholithiasis present | Choledocholithiasis not present | |
| Positive for high risk criteria | 61 | 16 |
| Negative for high risk criteria | 29 | 50 |
| Choledocholithiasis present | Choledocholithiasis not present | |
| Positive for intermediate risk criteria | 29 | 50 |
| Negative for intermediate risk criteria | 61 | 16 |
| Choledocholithiasis present | Choledocholithiasis not present | |
| Positive for intermediate risk criteria | 34 | 8 |
| Negative for intermediate risk criteria | 55 | 59 |
| Choledocholithiasis present | Choledocholithiasis not present | |
| Positive for intermediate risk criteria | 55 | 59 |
| Negative for intermediate risk criteria | 34 | 8 |
AGP is the most common cause of AP in the United States accounting for approximately one-third of all cases[1]. Furthermore, given the potential for comorbid choledocholithiasis, patients with AGP should be evaluated for CBD stone disease[2]. In our cohort of patients with AGP, 37% of patients with intermediate risk and 79.2% of patients with high risk for choledocholithiasis based on the 2010 ASGE guidelines had documented CBD stone disease. When combined, our data demonstrated that the true incidence of choledocholithiasis in patients with AGP is 58%. The overall high prevalence of concurrent choledocholithiasis in patients with AGP may help explain the relatively high risk of recurrent pancreatitis in patients with AGP[10].
The ASGE published guidelines in 2010 which proposed a risk stratification system to clarify how to best manage patients with suspected choledocholithiasis, categorizing patients into low, intermediate and high risk[4].
In this scheme, patients at high risk are recommended to undergo ERCP directly without further imaging and those at intermediate risk should have additional imaging with MRCP or EUS. Those at low risk require no further evaluation. In this study, we aimed to apply these guidelines to patients admitted with AGP to a single tertiary care center over 10 years and determine what effect deviation had on outcomes.
In our cohort of 156 patients, approximately one-half of patients were either classified as intermediate or high risk. Since all patients in our cohort had AGP and the presence of AGP was a criteria for at least intermediate risk for choledocholithiasis according to the 2010 ASGE guidelines, no patients in our cohort were considered low risk for choledocholithiasis. After applying the guidelines to these groups, 76% of patients (54 patients in the intermediate group and 64 patients in the high risk group) were managed in accordance to the ASGE recommendations and 24% of patients (25 patients in the intermediate group and 13 patients in the high risk group) deviated from the guidelines. Specifically in the intermediate group, 7 patients who had an ERCP first had a normal examination suggesting that an inappropriate procedure was performed and importantly, one of these patients suffered from post-ERCP pancreatitis. These 7 intermediate risk patents who directly underwent ERCP and had normal findings did not receive EUS or MRCP. Thus, it may be prudent to consider EUS to evaluate for choledocholithiasis to prevent unnecessary ERCPs. Furthermore, all 13 of the patients in the high risk group who underwent MRCP prior to ERCP had a positive finding, suggesting an unnecessary test (i.e. MRCP) was performed first. Importantly, patients who underwent MRCP prior to ERCP were found to have longer hospital lengths of stay and delays in initiation of enteral feeding.
The ASGE guidelines provide evidence-based recommendations with the goal of optimizing the efficacy and safety of patient care. Additionally, a study has shown that adherence to ASGE guidelines also result in cost-saving from unnecessary imaging studies[3]. Accordingly, patients with intermediate risk (10%-50%) should undergo additional imaging because the risk of choledocholithiasis is too low to warrant proceeding directly to ERCP[6]. MRCP is often preferred in patients with pancreatitis who have intermediate risk for choledocholithiasis because it has high sensitivity in detecting CBD stones without procedural risks[11]. While ERCP is highly sensitive and specific in diagnosis and effective in therapeutic management of choledocholithiasis[12], the procedure also has a number of associated risks such as post-ERCP pancreatitis and post-endoscopic sphincterotomy bleeding[13,14]. One of the intermediate risk patients in our cohort who went directly to ERCP which showed normal findings developed worsening of pancreatitis thought to be related to post ERCP AP. This highlights that unnecessary invasive procedure and adverse outcome could have been prevented by adhering to the guidelines.
In 2019, the ASGE updated guidelines on management of choledocholithiasis, which further fine-tuned the criteria needed for the high risk group[6]. Specifically, patients now required the presence of a bilirubin greater than 4 mg/dL and imaging with a dilated CBD to qualify as high risk and thus those patients with a total bilirubin of 1.8-4.0 mg/dL with CBD dilation on imaging were downgraded to intermediate risk. The impetus for these changes were largely driven by studies that demonstrated that up to 30% of patients had ERCPs without evidence of CBD stones[15,16]. In our study, we found that approximately 26% (9/35) of patients categorized as high risk by 2019 criteria had a normal ERCP.
Since the cohort we studied was prior to the update, the 2010 guidelines were used in the initial analysis. In our subsequent analysis we aimed to determine concordance in categorization between the 2010 and 2019 guidelines. After applying the 2019 guidelines, we found that all patients in the intermediate group remained the intermediate group, whereas there was less concordance in the high risk group which was largely due to the group of patients who had lower total bilirubin levels. Importantly, using the newer guidelines, 9 patients may have been spared an ERCP. We also found that while the 2010 ASGE guidelines in predicting high risk for choledocholithiasis had a specificity of 75.8%, using the 2019 ASGE guidelines led to an improved specificity of 89.4%. This demonstrated that the use of the revised guidelines in assessing risk for choledocholithiasis in AGP patients can lead to a decrease in unnecessary invasive and costly procedures. Moreover, although AGP was removed from the intermediate risk criteria, all patients in our intermediate cohort remained intermediate suggesting that AGP implicitly increases the risk to the intermediate level for choledocholithiasis. This was verified in our cohort where 58% of patients with AGP were confirmed to have choledocholithiasis. Thus, clinicians should remain vigilant for concurrent choledocholithiasis in patients admitted with AGP.
We recognize that our study also has several limitations. First, this is a retrospective cohort study which has a potential for selection bias. The smaller size and retrospective nature of this study may limit the assessment of the degree of adherence to the ASGE guidelines. As the decision to proceed with MRCP or ERCP were at the discretion of the physician on service, the detailed reasoning behind selecting each modality was not always apparent in the medical record. Our results may not be generalizable to all medical settings as this study was done at a single tertiary care center at an academic institution located in a large metropolitan city. Further work is needed to determine the influencing factors driving deviation from the guidelines.
In the study cohort, we demonstrated that more than half of patients with AGP have choledocholithiasis. We also found that approximately two thirds of patients in the intermediate group and 83% of patients in the high risk group followed ASGE guidelines for management of choledocholithiasis in the setting of AGP. There was associated longer LOS for patients undergoing MRCP in both groups. Importantly, one patient who had a normal ERCP in the intermediate group without preceding MRCP suffered from post ERCP AP, highlighting the risk of unnecessary procedures. Further work is needed to determine the influencing factors driving deviation from the guidelines.
Acute gallstone pancreatitis (AGP) is the most common cause of acute pancreatitis (AP) in the United States. Patients with AGP may also present with choledocholithiasis. In 2010, the American Society for Gastrointestinal Endoscopy (ASGE) suggested a management algorithm based on probability for choledocholithiasis. In 2019, the ASGE guidelines were updated.
Neither 2010 nor 2019 ASGE guidelines has been studied in AGP to determine the probability of having choledocholithiasis.
Our study aimed to determine compliance with ASGE guidelines, assess outcomes, and compare 2019 vs 2010 ASGE criteria for suspected choledocholithiasis in AGP.
We conducted a retrospective cohort study of 882 patients admitted with AP to a single tertiary care center from 2008-2018. Patients with AGP were assigned low, intermediate or high risk for choledocholithiasis based on ASGE guidelines. Our primary outcomes of interest were the proportion of patients in the intermediate risk group undergoing magnetic resonance cholangiopancreatography (MRCP) first and the proportion of patients in the high risk group undergoing endoscopic retrograde cholangiopancreatography (ERCP) directly without preceding imaging. Secondary outcomes of interest included outcome differences based on if guidelines were not adhered to. We then evaluated the diagnostic accuracy of 2019 in comparison to the 2010 ASGE criteria for patients with suspected choledocholithiasis.
Among 79 intermediate risk patients according to the 2010 ASGE guidelines, 54 (68%) underwent MRCP first whereas 25 patients (32%) went directly to ERCP. Of the 25 intermediate risk patients who directly underwent ERCP, 18 patients had stone disease. One patient with a normal ERCP developed post ERCP pancreatitis. In the high risk group, 64 patients (83%) had ERCP without preceding imaging. When the updated 2019 ASGE guidelines were applied instead of the original 2010 guidelines, there was moderate agreement between the 2010 and 2019 guidelines (kappa = 0.46, 95%CI: 0.34-0.58). Based on the 2019 criteria, 9/35 patients who were downgraded to intermediate risk had an unnecessary ERCP with normal findings (without a preceding MRCP).
In the study cohort, we demonstrated that more than half of patients with AGP have choledocholithiasis. We also found that approximately two thirds of patients in the intermediate group and 83% of patients in the high risk group followed ASGE guidelines for management of choledocholithiasis in the setting of AGP. Importantly, one patient who had a normal ERCP in the intermediate group without preceding MRCP suffered from post ERCP pancreatitis, highlighting the risk of unnecessary procedures. We also found that while the 2010 ASGE guidelines in predicting high risk for choledocholithiasis had a specificity of 75.8%, using the 2019 ASGE guidelines led to an improved specificity of 89.4%.
Further work is needed to determine the influencing factors driving deviation from the guidelines.
The authors would like to thank the Harvard Catalyst Biostatistics Consulting Program at Beth Israel Deaconess Medical Center for reviewing statistical methods and reporting of results.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chow WK, Taiwan; Miyabe K, Japan S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Forsmark CE, Baillie J; AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022-2044. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 494] [Cited by in F6Publishing: 480] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 2. | Rosseland AR, Glomsaker TB. Asymptomatic common bile duct stones. Eur J Gastroenterol Hepatol. 2000;12:1171-1173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Singhvi G, Ampara R, Baum J, Gumaste V. ASGE guidelines result in cost-saving in the management of choledocholithiasis. Ann Gastroenterol. 2016;29:85-90. [PubMed] [Cited in This Article: ] |
| 4. | ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, Ikenberry SO, Jain R, Khan K, Krinsky ML, Strohmeyer L, Dominitz JA. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71:1-9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 380] [Cited by in F6Publishing: 310] [Article Influence: 22.1] [Reference Citation Analysis (2)] |
| 5. | Chandran A, Rashtak S, Patil P, Gottlieb A, Bernstam E, Guha S, Ramireddy S, Badillo R, DaVee RT, Kao LS, Thosani N. Comparing diagnostic accuracy of current practice guidelines in predicting choledocholithiasis: outcomes from a large healthcare system comprising both academic and community settings. Gastrointest Endosc. 2021;93:1351-1359. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | ASGE Standards of Practice Committee, Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89:1075-1105.e15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 298] [Cited by in F6Publishing: 238] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 7. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4134] [Cited by in F6Publishing: 3692] [Article Influence: 335.6] [Reference Citation Analysis (38)] |
| 8. | Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57:1698-1703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 451] [Cited by in F6Publishing: 453] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 9. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32099] [Cited by in F6Publishing: 34964] [Article Influence: 945.0] [Reference Citation Analysis (0)] |
| 10. | Hwang SS, Li BH, Haigh PI. Gallstone pancreatitis without cholecystectomy. JAMA Surg. 2013;148:867-872. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, Francis IR, Nandi PS. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? Am J Gastroenterol. 2001;96:2900-2904. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 128] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Prat F, Amouyal G, Amouyal P, Pelletier G, Fritsch J, Choury AD, Buffet C, Etienne JP. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis. Lancet. 1996;347:75-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 220] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 405] [Cited by in F6Publishing: 431] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 14. | ASGE Standards of Practice Committee, Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, Cash BD, Decker GA, Early DS, Fanelli RD, Fisher DA, Fukami N, Hwang JH, Ikenberry SO, Jue TL, Khan KM, Krinsky ML, Malpas PM, Maple JT, Sharaf RN, Shergill AK, Dominitz JA. Complications of ERCP. Gastrointest Endosc. 2012;75:467-473. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 281] [Cited by in F6Publishing: 276] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 15. | Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, Kwon RS, Piraka CR, Scheiman JM, Waljee AK, Hussain HK, Elmunzer BJ. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82:88-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Rubin MI, Thosani NC, Tanikella R, Wolf DS, Fallon MB, Lukens FJ. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: testing the current guidelines. Dig Liver Dis. 2013;45:744-749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |