Published online Jul 7, 2013. doi: 10.3748/wjg.v19.i25.4083
Revised: February 26, 2013
Accepted: March 8, 2013
Published online: July 7, 2013
Underdiagnosis of drug-induced fever leads to extensive investigation and prolongation of hospitalization, and may lead to multiple unnecessary invasive procedures and a wrong diagnosis. Azathioprine is a widely used immunosuppressive drug. We report a case of a 53-year-old female patient diagnosed with autoimmune hepatitis treated with azathioprine, who presented to the emergency room with a 6-wk history of fever and chills without other associated symptoms. Since the patient’s fever was of unknown origin, she was hospitalized. All treatment was stopped and an extensive workup to explore the source of fever and chills was performed. Results of chest X-ray, viral, urine, and blood cultures, autoimmune serology, transthoracic and transesophageal echocardiography, and abdominal ultrasound revealed no source of infection. A rechallenge test of azathioprine was performed and the fever and chills returned within a few hours. Azathioprine was established as the definite cause following rechallenge. Fever as an adverse drug reaction is often unrecognized. Azathioprine has been reported to cause drug-induced fever in patients with inflammatory bowel disease, rheumatoid arthritis, and sarcoidosis. To the best of our knowledge there have been no previous reports documenting azathioprine-induced fever in patients with autoimmune hepatitis. The occurrence of fever following the readministration of azathioprine suggests the diagnosis of drug-induced fever, particularly after the exclusion of other causes. A careful rechallenge is recommended to confirm the diagnosis.
Core tip: Azathioprine is widely used in inflammatory disease such as rheumatoid arthritis, inflammatory bowel disease and post solid organ transplant such as kidney transplantation. Azathioprine is an immune modulator drug that can expose patients to various infections and clinical fever. Azathioprine needs to be remembered as a potential fever provoker in the differential diagnosis of fever origin.
- Citation: Khoury T, Ollech JE, Chen S, Mizrahi M, Shalit M. Azathioprine-induced fever in autoimmune hepatitis. World J Gastroenterol 2013; 19(25): 4083-4086
- URL: https://www.wjgnet.com/1007-9327/full/v19/i25/4083.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i25.4083
Drug reaction is an underestimated cause of fever. Drug-induced fever may be defined as a disorder characterized by the appearance of elevated body temperature 7-10 d following the administration of a specific medication, with resolution of the fever upon discontinuation of the suspected agent. Less often, the fever can appear after a long period of treatment. Drug-induced fever is estimated to account for about 10% of elevated body temperature evaluations[1,2] and fever as the sole symptom of a drug’s side effect has been reported in about 3%-5%[3].
The diagnosis of drug-induced fever is usually challenging, especially in medically complicated patients with multiple treatment regimens. There are no clear guidelines for the diagnosis, which is usually made by exclusion of the responsible drug. Underdiagnosis of drug-induced fever may lead to extensive investigations, unnecessary antibiotic treatment, and prolonged hospitalization[4].
Azathioprine-induced fever is a relatively rare disorder. It has been reported in only a few patients with inflammatory bowel disease, rheumatoid arthritis, and sarcoidosis[5-7]. In several other reported cases, it was associated with accompanying manifestations such as pruritus and cutaneous rash[8,9].
We report the case of a patient with autoimmune hepatitis who developed fever and chills induced by azathioprine. Rechallenge confirmed the diagnosis. To the best of our knowledge, this is the first described case of azathioprine-induced fever in autoimmune hepatitis.
A 53-year-old female of Arab descent was diagnosed in 2009 with autoimmune hepatitis by liver biopsy, which showed moderate inflammatory activity with infiltrating plasma cells suggestive of autoimmune hepatitis. Serological tests for anti-nuclear antibody (ANA), anti-double-stranded antibodies, and anti-parietal antibodies were positive, and serum immunoglobulins IgM 329 mg/dL (normal range 65-280 mg/dL), IgA 786 mg/dL (90-450 mg/dL), IgG 3120 mg/dL (800-1700 mg/dL) were elevated (Table 1). The patient had been treated with budesonide until 6 wk before admission, when azathioprine 100 mg/d was added to the treatment regimen.
| Clinical feature | Score | Patient |
| Female gender | +2 | +2 |
| ALP:AST ratio | +2 | |
| < 1.5 | +2 | |
| 1.5-3.0 | 0 | |
| > 3.0 | -2 | |
| Serum globulin or IgG above normal | +2 | |
| > 2.0 | +3 | |
| 1.5-2.0 | +2 | |
| 1.0-1.5 | +1 | |
| < 1.0 | 0 | |
| ANA, SMA, LKM1 | +3 | |
| > 1:80 | +3 | |
| 1:80 | +2 | |
| 1:40 | +1 | |
| < 1:40 | 0 | |
| Illicit drug use history | +1 | |
| Positive | -4 | |
| Negative | +1 | |
| Average alcohol intake daily | +2 | |
| < 25 g/d | +2 | |
| > 60 g/d | -2 | |
| Histologic findings | Lymphoplasmacytic infiltrate | |
| Interface hepatitis | +3 | +1 |
| Lymphoplasmacytic infiltrate | +1 | |
| Rosette formation | +1 | |
| None of the above | -5 | |
| Biliary changes | -3 | |
| Other changes | +2 | |
| Other autoimmune disease | +2 | No other autoimmune disease |
| AMA positivity | -4 | AMA negative |
| Hepatitis viral markers | +3 | |
| Positive | -3 | |
| Negative | +3 | |
| Aggregate score without treatment | Overall 16 points | |
| Definite AIH | > 15 | |
| Probable AIH | 10-15 |
Her medical history was notable for valvular heart disease, paroxysmal atrial fibrillation, hypertension, hypothyroidism, diabetes mellitus, and microcytic anemia. Her medications included warfarin 22.5 mg once daily, metformin 850 mg 3 times daily, omeprazole 20 mg once daily, losartan 80 mg twice daily, insulin detemir 20 units once daily, insulin aspart 10 units 3 times daily, metoprolol 25 mg twice daily, spironolactone 100 mg once daily, aspirin 100 mg daily, furosemide 40 mg once daily, azathioprine 50 mg once daily, and thyroxine 50 mg once daily. She presented to the emergency room due to fever and chills of several weeks duration, without other associated symptoms. On admission, the patient was stable; blood pressure was 155/69 mmHg, pulse rate 62 beats/min, and temperature 38.4 °C. Her physical examination was unremarkable except for small skin erosion with surrounding erythema in her anterior abdominal wall. Blood tests showed a white blood cell count of 7.700 per cubic millimeter (4-10 thousand per cubic millimeter) with 90% neutrophils (40%-70%), 5.5% lymphocytes (15%-41%) and 3.5% monocytes (1%-7%). Hemoglobin was 9.3 g (12-16 g). Results of blood chemistry, including electrolytes and kidney function, were normal except for mild elevation of liver function tests. Urinalysis showed a few leukocytes but otherwise was normal. Nasal viral cultures were negative. C-reactive protein and erythrocyte sedimentation rate were normal. Computed tomography was performed to exclude an intra-abdominal cause of fever and revealed a small area of subcutaneous inflammation adjacent to the skin erosion. Chest X-ray showed no changes suggestive of infection.
The patient was admitted to the Department of Internal Medicine with an initial diagnosis of fever, most likely secondary to the localized skin infection in the abdominal wall. Azathioprine was withheld and the patient was treated with antibiotics. Within several hours the fever subsided and the patient remained afebrile throughout 5 d of hospitalization.
Following recovery and resolution of the cellulitis, the patient was discharged and azathioprine was re-administered. Within a few hours, fever and chills recurred and the patient was re-admitted to the hospital. An extensive work-up for fever of unknown origin was done including blood and urine cultures and nasal viral cultures, which were all negative. Serological tests for human immunodeficiency virus, hepatitis viruses, brucella, Q fever and toxoplasma were negative. Autoimmune serology showed ANA 2 of 4, anti-parietal cell antibodies 4 of 4; anti-smooth muscle, anti-mitochondrial and immunoglobulins were negative. In addition, ultrasonography of the abdomen revealed no evidence of ascites or infection. Transthoracic and transesophageal echocardiography did not show vegetation or abscess. Purified protein derivative test was negative. Again azathioprine was withheld and the fever resolved within a few hours.
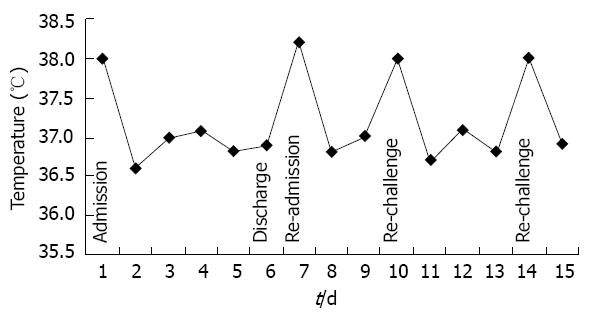
With the patient’s informed consent, a rechallenge with one tablet of 50 mg azathioprine was performed twice under observation. Chills appeared within 3 h and there was a gradual increase in temperature up to 38 °C within 7 h. Fever and chills resolved completely within 6 h after discontinuation of azathioprine.
Drug-induced fever is an underdiagnosed condition, particularly in patients treated with a large number of medications. It is described as a febrile response that coincides temporally with the administration of a drug and disappears after discontinuation of the offending agent. It is usually suspected when no other cause for fever can be explained, leaving drug fever as the diagnosis of exclusion.
Several mechanisms have been implied in the pathogenesis of drug-induced fever, most importantly hypersensitivity reaction involving the formation of antigen-antibody complexes. Common agents associated with hypersensitivity type reaction include penicillins, cephalosporins, phenytoin, methyldopa, procainamide, and antitubercular agents[2,3,10]. Other mechanisms include idiosyncratic reactions, drug effects on the thermoregulatory center, reactions to drug administration, and the extension of drug pharmacological effects as seen in patients who developed cell lysis and release of variable pyrogenic substances following chemotherapy treatment[1,11-13].
Azathioprine suppresses the immune system by inhibiting the activity of T cell lymphocytes. It is a prodrug which, following oral ingestion, is metabolized into active mercaptopurine, a purine synthesis inhibitor that impedes DNA synthesis and inhibits cell proliferation[14]. Azathioprine is known to cause multiple adverse effects, including fever, gastrointestinal symptoms, nervous system symptoms, bone marrow suppression, hepatic symptoms, myalgia, and arthralgia. Discontinuation of azathioprine is seen in about 10%-15% of patients due to side effects[5].
Several cases of azathioprine-induced fever in association with other symptoms have been reported; fever and chills were the only reported symptoms when azathioprine was administered to patients with sarcoidosis and inflammatory bowel disease, and after kidney transplantation[5,7,15,16].
In an observational study, three of 25 patients with RA developed symptoms of fever, chills, skin rash, hepatotoxicity, nausea, and diarrhea 2 wk after starting treatment with azathioprine. One patient developed only fever and chills. Rechallenge was performed in two patients with the appearance of more severe reactions[6]. In these patients, the febrile reaction appeared several days up to several weeks after beginning treatment with azathioprine. In our case the fever appeared within a few hours after restarting the offending agents. Thus the lag period between the initiation of the offending agent and the appearance of fever is highly variable.
In our patient, the sequence of events and the lack of objective evidence of infection are both highly suggestive of azathioprine-induced fever. In addition, previous reports of azathioprine causing drug fever in other disease states support the likelihood of a similar event in this patient[5-7]. With the patient’s permission, two rechallenge tests were done in which 50 mg azathioprine was administered. Fever of 38 °C was measured about 7 h after administration, without other associated symptoms or objective findings on blood analysis, and without recurrence of the fever upon discontinuation of azathioprine (Figure 1). Thus, fever and chills in our case are the only manifestations of azathioprine and were likely caused by the administration of azathioprine.
In conclusion, drug reaction is an underestimated cause of fever. Clinicians should be aware of the fact that an immunomodulatory drug such as azathioprine, commonly used to treat various autoimmune conditions and to suppress the inflammatory response, can cause fever and chills. It is thus essential to withdraw a suspected medication and perform a rechallenge when fever fails to regress in patients already treated with antibiotics.
We thank Miss Roemi Lilach and Miss Shifra Fraifeld for technical and editorial assistance.
P- Reviewers Neuberger J, Tanaka A S- Editor Song XX L- Editor O’Neill M E- Editor Li JY
| 1. | Johnson DH, Cunha BA. Drug fever. Infect Dis Clin North Am. 1996;10:85-91. [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 87] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 2. | Tabor PA. Drug-induced fever. Drug Intell Clin Pharm. 1986;20:413-420. [PubMed] [Cited in This Article: ] |
| 3. | Roush MK, Nelson KM. Understanding drug-induced febrile reactions. Am Pharm. 1993;NS33:39-42. [PubMed] [Cited in This Article: ] |
| 4. | Mackowiak PA, LeMaistre CF. Drug fever: a critical appraisal of conventional concepts. An analysis of 51 episodes in two Dallas hospitals and 97 episodes reported in the English literature. Ann Intern Med. 1987;106:728-733. [PubMed] [Cited in This Article: ] |
| 5. | Smak Gregoor PJ, van Saase JL, Weimar W, Kramer P. Fever and rigors as sole symptoms of azathioprine hypersensitivity. Neth J Med. 1995;47:288-290. [PubMed] [Cited in This Article: ] |
| 6. | Jeurissen ME, Boerbooms AM, van de Putte LB, Kruijsen MW. Azathioprine induced fever, chills, rash, and hepatotoxicity in rheumatoid arthritis. Ann Rheum Dis. 1990;49:25-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | McBane S, Rojas C. Azathioprine-induced fever in sarcoidosis. Ann Pharmacother. 2011;45:e19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Bidinger JJ, Sky K, Battafarano DF, Henning JS. The cutaneous and systemic manifestations of azathioprine hypersensitivity syndrome. J Am Acad Dermatol. 2011;65:184-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Yiasemides E, Thom G. Azathioprine hypersensitivity presenting as a neutrophilic dermatosis in a man with ulcerative colitis. Australas J Dermatol. 2009;50:48-51. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Bayard PJ, Berger TG, Jacobson MA. Drug hypersensitivity reactions and human immunodeficiency virus disease. J Acquir Immune Defic Syndr. 1992;5:1237-1257. [PubMed] [Cited in This Article: ] |
| 11. | Beutler B, Munford RS. Tumor necrosis factor and the Jarisch-Herxheimer reaction. N Engl J Med. 1996;335:347-348. [PubMed] [Cited in This Article: ] |
| 12. | Hanson MA. Drug fever. Remember to consider it in diagnosis. Postgrad Med. 1991;89:167-170, 173. [PubMed] [Cited in This Article: ] |
| 13. | Saper CB, Breder CD. The neurologic basis of fever. N Engl J Med. 1994;330:1880-1886. [PubMed] [Cited in This Article: ] |
| 14. | Corbett M, Schlup M. Azathioprine hypersensitivity mimicking underlying inflammatory bowel disease. Intern Med J. 2001;31:366-367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 15. | Garey KW, Streetman DS, Rainish MC. Azathioprine hypersensitivity reaction in a patient with ulcerative colitis. Ann Pharmacother. 1998;32:425-428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Dhaliwal HK, Anderson R, Thornhill EL, Schneider S, McFarlane E, Gleeson D, Lennard L. Clinical significance of azathioprine metabolites for the maintenance of remission in autoimmune hepatitis. Hepatology. 2012;56:1401-1408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |