Published online Apr 6, 2024. doi: 10.12998/wjcc.v12.i10.1785
Peer-review started: October 28, 2023
First decision: January 17, 2024
Revised: January 30, 2024
Accepted: March 13, 2024
Article in press: March 13, 2024
Published online: April 6, 2024
Jaffe-Campanacci syndrome (JCS) is a very rare syndrome. The treatment of JCS is more conservative, and most authors recommend that no surgery should be done in asymptomatic patients. The conventional concept holds that the natural course of non-ossifying fibromas (NOFs) grows with the development of bones, and the osteolytic region gradually stops expanding and self-healing through bone ossifying around the lesion and ossification within the lesion. But in this case, the bone lesions were potentially biologically aggressive, which led to severe limb deformities and pain.
We present the case of a 5-year-old girl with JCS presenting with not only NOF sand café-au-lait macules, but also showed features not mentioned before, severe limb pain, and at last resulted in amputation. She was admitted to our hospital after presenting with claudication and mild pain over her right thigh, which worsened when stretching or being touched. Skin examination revealed multiple café-au-lait macules on the neck, arm, axilla, and torso, including the nipples and perineum. Radiographs revealed multiple lytic lesions in the proximal part of the right humerus, distal part of the right clavicle, proximal and distal parts of the right femur, and proximal parts of the right tibia and fibula. Curettage and biopsy were performed on the distal part of the right femur. At the age of 7, the girl was re-admitted to our hospital for a pathological fracture in the middle in the right femur and underwent Intralesional excision, internal fixation, bone grafting, and spica casting. At the age of 10, the girl came to our hospital again for severe pain of the right leg. Amputation from the middle level of the right femur was performed. We present the case of a 5-year-old girl with JCS presenting with not only NOFs and café-au-lait macules, but also showed features not mentioned before, severe limb pain, and at last resulted in amputation. She was admitted to our hospital after presenting with claudication and mild pain over her right thigh, which worsened when stretching or being touched. Skin examination revealed multiple café-au-lait macules on the neck, arm, armpit, and torso, including the nipples and perineum. Radiographs revealed multiple lytic lesions in the proximal part of the right humerus, distal part of the right clavicle, proximal and distal parts of the right femur, and proximal parts of the right tibia and fibula. Curettage and biopsy were performed on the distal part of the right femur. At the age of 7, the girl was re-admitted to our hospital for a pathological fracture in the middle in the right femur and underwent Intralesional excision, internal fixation, bone grafting, and spica casting. At the age of 10, the girl came to our hospital again for severe pain of the right leg. Amputation from the middle level of the right femur was performed.
In our opinion, education on preventing pathological fractures and explaining the consequent serious con
Core Tip: Jaffe-Campanacci syndrome (JCS) is exceedingly rare. In this case, a 10-year-old girl with JCS presented with not only non-ossifying fibromas and café-au-lait macules, but also showed features not mentioned before, severe limb pain, and at last resulted in amputation. This case is a big failure with a tragic ending and has revelatory educational value to all orthopaedic surgeons. We aim to share our failures in treatment and remind other doctors that not every JSC grows with bone development and can be self-healing. We highly recommend education on preventing pathological fractures and explaining the consequent serious consequences to the parents is a matter of prime significance. At the same time, prophylactic treatment (restricted exercise, support, or surgery) is also considerable for JSC.
- Citation: Jiang J, Liu M. Jaffe-Campanacci syndrome resulted in amputation: A case report. World J Clin Cases 2024; 12(10): 1785-1792
- URL: https://www.wjgnet.com/2307-8960/full/v12/i10/1785.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i10.1785
Jaffe-Campanacci syndrome (JCS) is a very rare syndrome that was first described by Jaffe in 1959[1]. In 1983, Campa
A 10-year-old Chinese girl was admitted to our hospital for severe pain accompanied by shortening and deformity of the right leg.
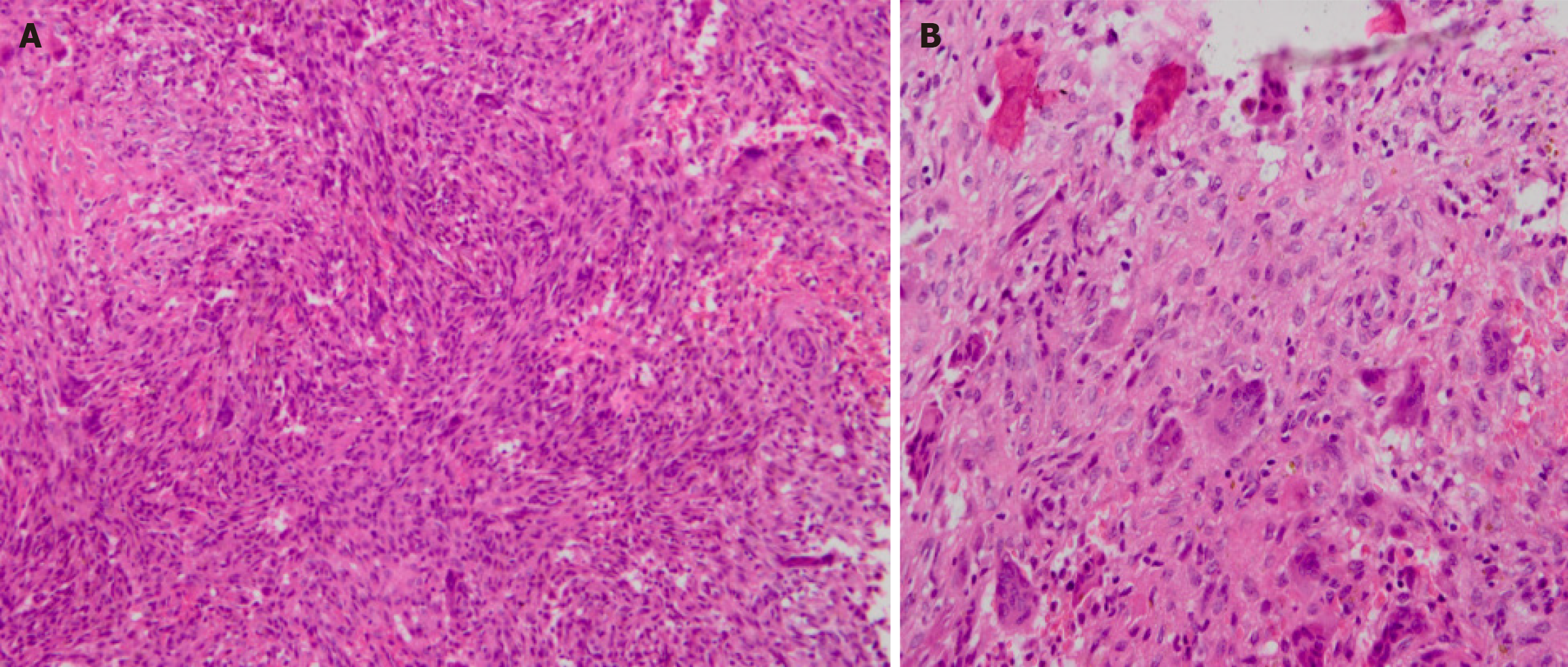
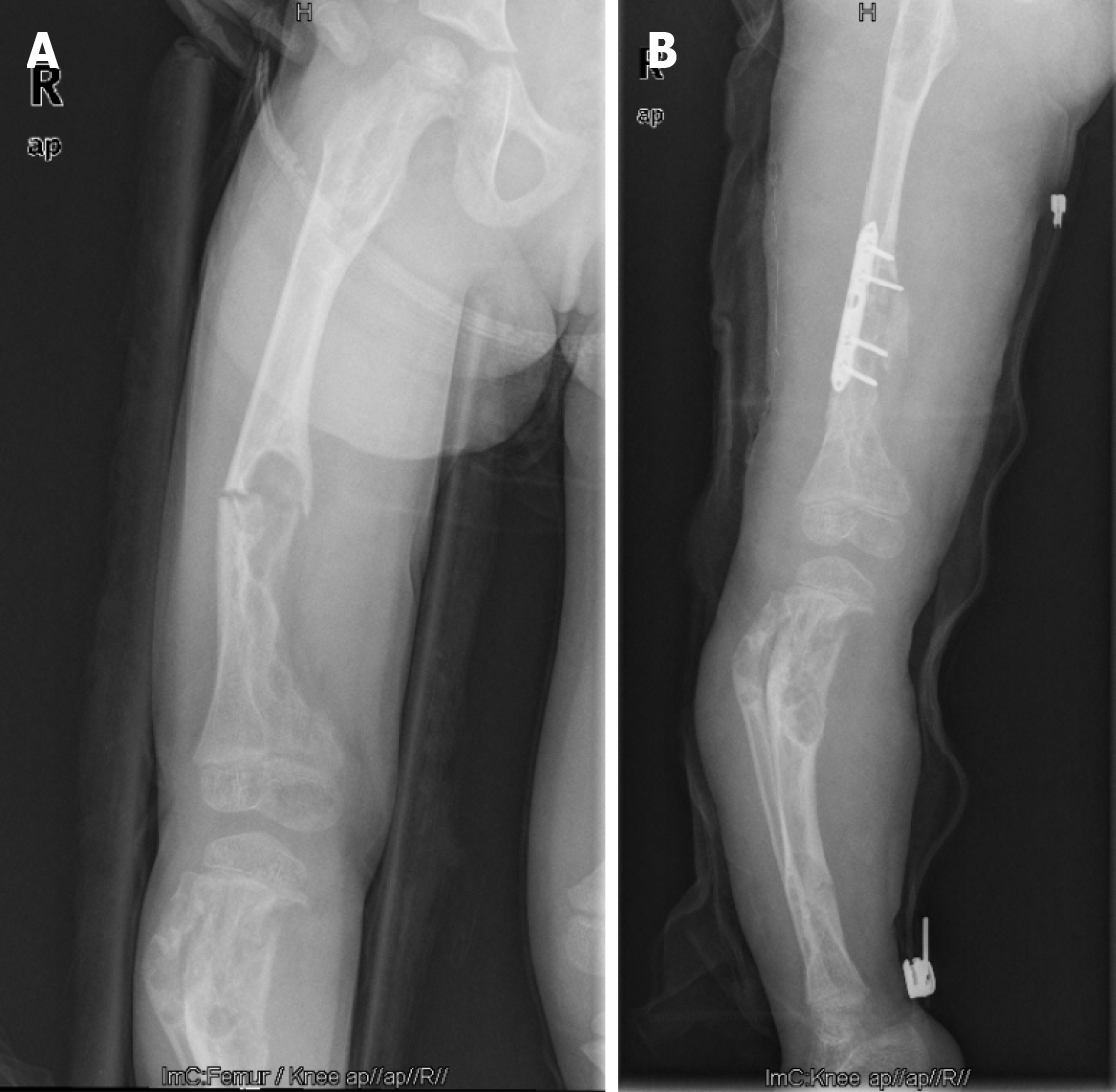
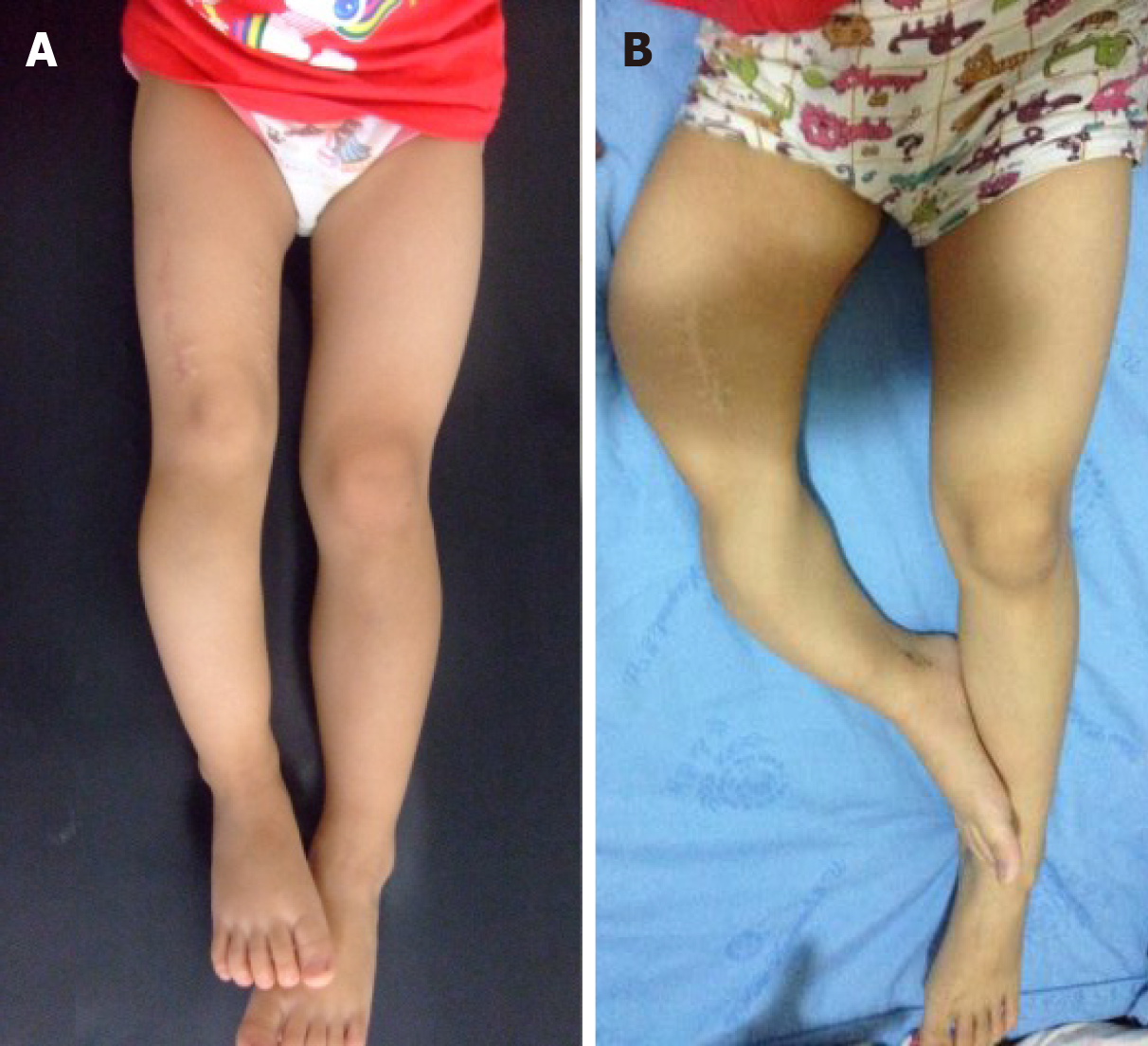
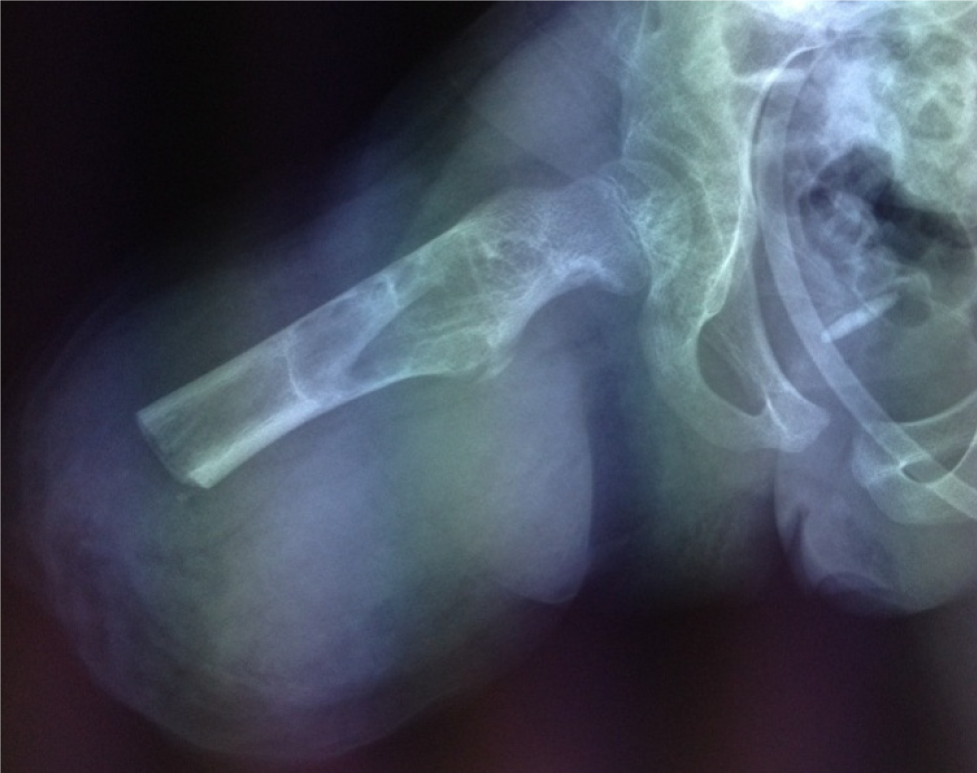
Five years ago, the patient (5-year-old) came to our hospital after presenting with claudication and mild pain over her right thigh, which worsened when stretching or being touched. Radiographs revealed multiple lytic lesions in the proximal part of the right humerus, distal part of the right clavicle, proximal and distal parts of the right femur, and proximal parts of the right tibia and fibula (Figure 1). Curettage and biopsy were performed on the distal part of the right femur. Histopathological examination showed spindle-shaped fibroblastic and collagenous stromal tissue, characteristic of the NOF (Figure 2), then the diagnosis of JCS was made. Conservative therapy was applied with suggestions of observation, reduction of mobility, and follow-up. Three years ago, at the age of 7, the patient was re-admitted to our hospital for a pathological fracture in the middle of the right femur. Intralesional excision, internal fixation, bone grafting, and spica casting were performed (Figure 3). During the operation, brown granulomas-like tissues were found in the cortex and marrow of the femur and were extending into the metaphysis of the distal femur. The plaster was removed one month after surgery and the patient began to walk three months postoperatively.
Family history did not reveal any familial disease, neurofibromatosis, or bone lesions.
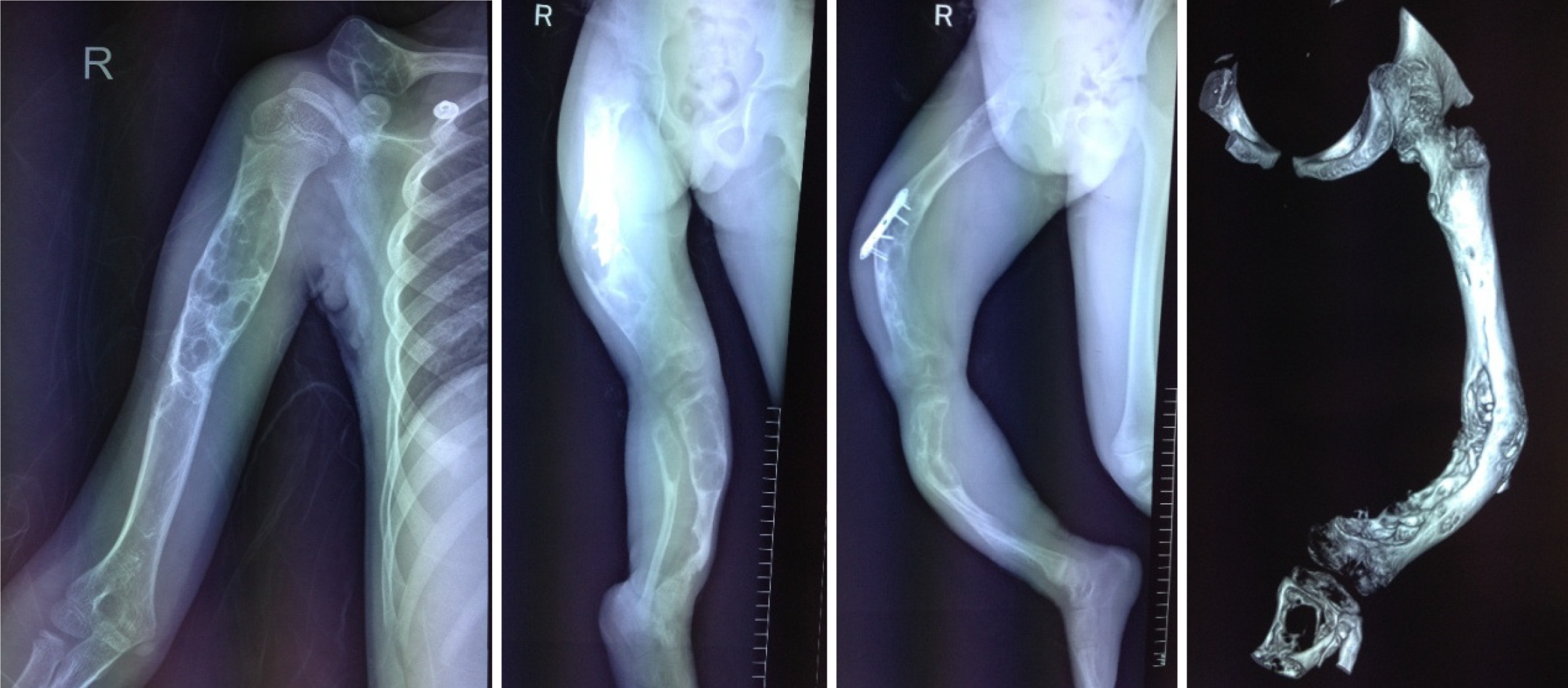
The right leg was 20 cm shorter than the left leg, with a severe curved deformity of the thigh and crus (Figure 4). During palpation, there was severe pain from the middle part of the right thigh to the upper part of the calf. The right knee joint remained in a flexed position and could not be extended or flexed. The muscles of the right lower limb were atrophied. Skin examination revealed multiple café-au-lait macules on the neck, arm, armpit, and torso, including the nipples and perineum. The patient showed no pain or itching associated with the macules. The area of the lesions covered the neck, arm, armpit, and torso including the nipple and the perineum, and had a “Coast of Maine” shape with ragged, irregular outlines. Brown granular nodules eres noted in the middle of the lesions (Figure 5).
Laboratory testing revealed no abnormal findings. The whole exome gene test found tuberous sclerosis complex (TSC) 1 (exon7) on the chr9:135797354 had a missense mutation [NM_000368.4: c.515T>C (p. Val172Ala)] in peripheral blood.
The lytic lesions of the right femur, tibia, and fibula were larger than before, both femur and tibia were severely curved. The whole tibia was affected by the lesion with a large cortical defect in the lower part of the tibia (Figure 6).
Considering the results of imaging and histopathological examination we arrived at a final diagnosis of JSC.
Amputation from the middle level of the right femur was performed (Figure 7).
The wound on the right thigh healed well 2-month after surgery with no pain reoccurring, and the girl started rehabilitation. During the following 3-year follow-up, the area of the lesions did not expand with no pain or itching. She could walk and run well with the help of artificial limb.
Presently, most scholars describe JCS as an ill-defined syndrome associated with NOFs, skin manifestations (café-au-lait macules), and extraskeletal anomalies, which include mental retardation, hypogonadism, cryptorchidism, ocular anomalies, or cardiovascular malformations some. It is still controversial whether JCS is a special type of type 1 neu
In all 22 cases have been reported in English literature, most patients were under the age of 18 and males were more than females (13 males, 9 females) (Supplementary Table 1). Three previous cases have been reported in East Asia, and, thus, the present case is the fourth[9-11]. It is interesting to find that the bone lesions and café-au-lait macules of this and another case from East Asia were unilateral—especially the abdominal café-au-lait macules which were bounded by the midline on the right and did not cross to the other side (Figure 5). The café-au-lait macules were in the shape of the “coast of Maine”, rather than the “coast of California”. In this case, brown granular nodules occurred in the middle of the café-au-lait macules, which was different from those described in the previous literature of JCS. The lesion feature of NF1 commonly presents as a painless skin-colored or violaceous papule, nodule, or subcutaneous mass, which is also different from this case. These features are distinct from those reported in Caucasian patients. Localized skin lesion histopathological examination was suggested, but the parents refused to do any more surgeries but the leg.
Most JCS patients are asymptomatic, the most typical extraskeletal anomalies are café-au-lait macules, some patients have axillar freckling, i.e., clusters of freckle-like light brown macules with a diameter of 1 mm to 3 mm located in the armpits or other parts of the trunk. Another unusual manifestation was limb pain. The child felt mild pain after activity, which worsened gradually and extended from the thigh to the crus. The right leg became shorter and shorter with femoral and tibial flexion deformity, which seriously affected mobility and daily life. Serious pain was not reported in previous cases, the reason and mechanism are still uncertain. But it seems to be caused by the bone lesions, for the pain in the right thigh had greatly relieved after the intralesional excision surgery and became more serious as the bone lesions deteriorated. During the treatment, an arachnoid cyst was found in the occipital area of the head, which was not men
No consensus has been reached for the treatment for JSC. In most cases, JSC patients were treated conservatively, for the simple reason as Campanacii et al[2] found, the natural course of NOFs grows with bone development, the osteolytic region gradually stops expanding, and there will be self-healing through bone ossification around the lesion and ossification within the lesion[2]. The reason why this case is characterized by pain, and it became more and more serious with the progress of the bone lesions is uncertain. However, the lesions in this case were potentially biologically aggressive, consistent with the case described by Blau et al[12].
If pathological the fracture occurs, curettage, grafting, and internal fixation would be necessary. Colby and Saul[7] supposed this could be because large polyostotic area lesions cause weight-bearing bones (e.g., proximal femur, proximal tibia) to become thin and brittle. When pathological fractures occur, operation is necessary[7]. As differentiation of JSC from other osteolytic lesions is sometimes difficult, some authors also recommend a two-stage operation[6]. Biopsy surgery should be performed first and then Definitive surgery followed. Of all the 22 cases of JSC reported in the English literature, 59.1% (13/22) had pathological fractures, which is much higher than the incidence of NOFs pathological fractures. The girl in the present case is the first report of amputation in JCS. There are various reasons for amputation. Firstly, the progressive aggravation of the lesions leads to severe limb deformities. After curettage, grafting, and internal fixation with a conventional plate, the lesions of the right femur and tibia were enlarged with a large defect in the lower part of the tibia, and the tibia was bent and deformed with severe shortening. As the progression of the disease, there was no way to regain either alignment or length of the leg. Secondly, the pain in the right leg is from beginning to end. When the girl had performed Intralesional excision, internal fixation, and bone grafting surgery, the pain was relieved for half a year, but then became more and more serious and gradually extended to the right crus. Before amputation, the girl had to ease the pain by drugs every day.
There are limited reports about the long-term prognosis. The short-term prognosis of JCS with conservative treatment is good except high incidence of pathological fractures. Patients with pathological fractures gradually healed after surgery, and mobility was largely unaffected. Although there have been no reports of limb malformations in JCS, limb malformation caused by NOFs has been reported[13]. Proper intervention (restricted exercise, support, or surgery) may reduce the rate of long-term disability[7]. Given the present case, we highly recommend preventive measures for patients (especially overweight patients) with simultaneous femoral and tibial lesions who have a high risk of limb deformity. Given the close relationship between JSC and NF1, some researchers have suggested that patients diagnosed with NF1 should undergo bone examination to exclude NOFs or even JCS to prevent secondary pathological fractures[4]. However, the skin lesions of this case are different from those in other cases of JSC. Meanwhile, both the bone lesions and the pain were continuously deteriorating, leading to a poor prognosis. All these suggested the lesions in this case were potentially aggressive.
Our case showed features of JCS not mentioned before. The bone lesions and café-au-lait macules of this case were unilateral—especially the abdominal café-au-lait macules which were bounded by the midline on the right and never crossed to the other side. Another unusual manifestation was severe limb pain. Both the bone lesions and the pain were continuously deteriorating, leading to a poor prognosis. All these suggested the lesions in this case were potentially aggressive. In our opinion, education on preventing pathological fractures and explaining the consequent serious consequences to the parents is a matter of prime significance. At the same time, prophylactic treatment (restricted exercise, support, or surgery) is also considerable for JSC.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Katanec T, Croatia S-Editor: Che XX L-Editor: A P-Editor: Zhao S
| 1. | Jaffe HL. Tumors and tumorous conditions of the bones and joints. J Med Educ. 1959;34:72. [DOI] [Cited in This Article: ] |
| 2. | Campanacci M, Laus M, Boriani S. Multiple non-ossifying fibromata with extraskeletal anomalies: a new syndrome? J Bone Joint Surg Br. 1983;65:627-632. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Mirra JM, Gold RH, Rand F. Disseminated nonossifying fibromas in association with café-au-lait spots (Jaffe-Campanacci syndrome). Clin Orthop Relat Res. 1982;192-205. [PubMed] [Cited in This Article: ] |
| 4. | Cherix S, Bildé Y, Becce F, Letovanec I, Rüdiger HA. Multiple non-ossifying fibromas as a cause of pathological femoral fracture in Jaffe-Campanacci syndrome. BMC Musculoskelet Disord. 2014;15:218. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Hau MA, Fox EJ, Cates JM, Brigman BE, Mankin HJ. Jaffe-Campanacci syndrome. A case report and review of the literature. J Bone Joint Surg Am. 2002;84:634-638. [PubMed] [Cited in This Article: ] |
| 6. | Sonar M, Isik M, Ekmekci AY, Solmaz OA. Pathological fractures on both lower limbs with Jaffe-Campanacci's syndrome. BMJ Case Rep. 2012;2012. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Colby RS, Saul RA. Is Jaffe-Campanacci syndrome just a manifestation of neurofibromatosis type 1? Am J Med Genet A. 2003;123A:60-63. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Stewart DR, Brems H, Gomes AG, Ruppert SL, Callens T, Williams J, Claes K, Bober MB, Hachen R, Kaban LB, Li H, Lin A, McDonald M, Melancon S, Ortenberg J, Radtke HB, Samson I, Saul RA, Shen J, Siqveland E, Toler TL, van Maarle M, Wallace M, Williams M, Legius E, Messiaen L. Jaffe-Campanacci syndrome, revisited: detailed clinical and molecular analyses determine whether patients have neurofibromatosis type 1, coincidental manifestations, or a distinct disorder. Genet Med. 2014;16:448-459. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Yang C, Gong Y, Li C, Gu G, Liu J, Qi X. Jaffe-Campanacci Syndrome: A Case Report and Review of Literature. JBJS Case Connect. 2012;2:e10. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Choi EM, Jung N, Shim YJ, Choi HJ, Kim JS, Kim HS, Song KS, Lee HJ, Kim SP. Short stature and growth hormone deficiency in a girl with encephalocraniocutaneous lipomatosis and Jaffe-Campanacci syndrome: a case report. Ann Pediatr Endocrinol Metab. 2016;21:240-244. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Han Y, Wang H. Intracranial arterial dolichoectasia and skull damage in a girl with Jaffe-Campanacci syndrome: a case report. Childs Nerv Syst. 2019;35:1051-1054. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Blau RA, Zwick DL, Westphal RA. Multiple non-ossifying fibromas. A case report. J Bone Joint Surg Am. 1988;70:299-304. [PubMed] [Cited in This Article: ] |
| 13. | Tsuchiya H, Morsy AF, Matsubara H, Watanabe K, Abdel-Wanis ME, Tomita K. Treatment of benign bone tumours using external fixation. J Bone Joint Surg Br. 2007;89:1077-1083. [PubMed] [DOI] [Cited in This Article: ] |