Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8170
Peer-review started: August 28, 2023
First decision: October 24, 2023
Revised: October 26, 2023
Accepted: November 28, 2023
Article in press: November 28, 2023
Published online: December 6, 2023
Venous adventitial cystic disease (VACD) is a rare disease characterized by cysts, filled with a gelatinous mucous substance similar to joint fluid, in the adventitia of blood vessels adjacent to the joints. It is often misdiagnosed as deep vein thro
A 69-year-old woman visited our hospital with a complaint of swelling in the right lower extremity. The patient was diagnosed with DVT and prescribed apixaban at an outpatient clinic. After 3 wk, the patient was hospitalized again because of sudden swelling in the right lower extremity. We diagnosed VACD and performed surgery for cyst removal as well as patch angioplasty and thrombectomy of the right common femoral vein. The patient received anticoagulants for 6 mo and has been doing well without recurrence for 1 year postoperatively.
Recurrent VACD requires complete removal of the connections to the joint cavity to prevent recurrence.
Core Tip: Venous adventitious cystic disease is a rare condition characterized by the occurrence of cysts filled with a gelatinous substance similar to synovial fluid in the outer layer of blood vessels adjacent to joints. It can be misdiagnosed as deep vein thrombosis, femoral varices, venous tumors, or lymphadenopathy. To prevent recurrence, it is important to completely remove the connections to the joint cavity.
- Citation: Bae M, Huh U, Lee CW, Kim JW. Venous adventitial cystic disease is a very rare disease that can cause deep vein thrombosis: A case report. World J Clin Cases 2023; 11(34): 8170-8175
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8170.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8170
Venous adventitial cystic disease (ACD) (VACD) is a rare malformation characterized by the accumulation of mucinous materials in cysts in the vascular adventitia[1]. According to an extensive literature review, only 53 cases have been reported to date[2]. Cysts usually occur in blood vessels around the major joints, and patients complain of severe swelling, tenderness, and pain[3].
We describe the case of a patient who was first diagnosed with deep vein thrombosis (DVT) and later diagnosed with VACD due to symptom recurrence during treatment. Recovery was achieved through surgical treatment.
Right leg swelling.
A 69-year-old woman visited our hospital complaining of swelling in the right lower extremity. The patient was diagnosed with DVT at a local hospital, and thrombolysis was performed. Venography was performed after throm
The patient had a history of hypertension.
She had no relevant personal or family history.
The physical examination revealed no noteworthy abnormalities.
Her D-dimer levels were elevated to 80 μg/mL (normal range 0-0.5 μg/mL). Other laboratory parameters were within the normal ranges.
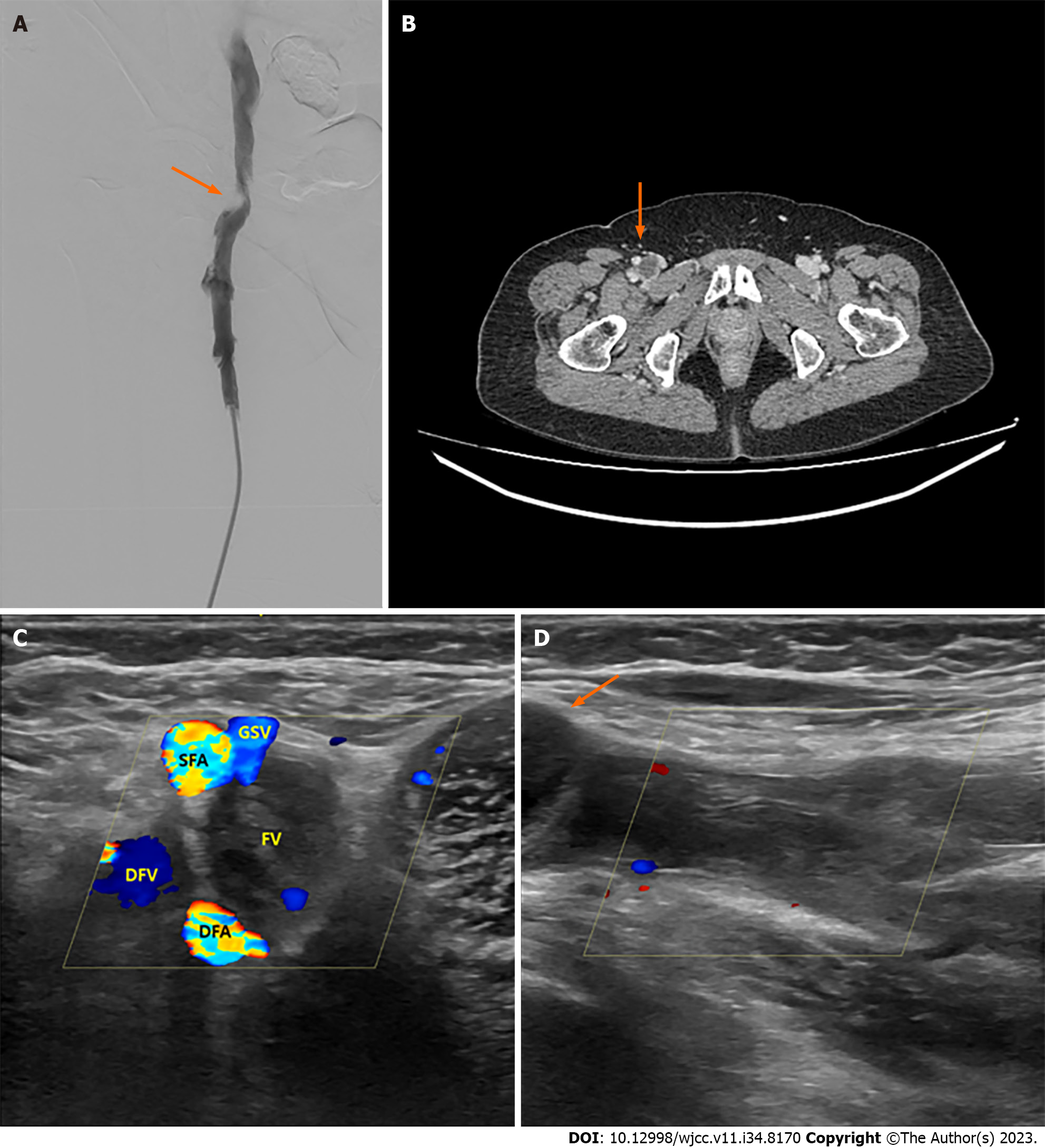
Venography revealed a mass-like lesion (scimitar sign) located outside of and pressing on the right CFV (Figure 1A). A cystic mass was observed in the right CFV (Figure 1B). On ultrasonography, we did not observe flow to the right femoral artery (FV) because the cystic mass had blocked the right CFV (Figure 1C and D).
The patient was diagnosed with VACD and surgery was planned. After surgery, histological examination confirmed VACD. A cystic wall composed of fibrous tissue with increased proteoglycan levels and few elastic fibers was observed.
The patient underwent surgery under general anesthesia. A longitudinal incision was made in the right groin. The distal external iliac vein above the branch of the great saphenous vein (GSV) was dissected into the GSV, proximal FV, and proximal deep femoral vein. In particular, to eliminate communication with the synovial fluid, the bottom wall of the vein was completely dissected and communication was removed (Figure 2). After venotomy, the cyst and the vein wall in the cystic area were removed. The right leg was squeezed to remove any remaining thrombus. The right posterior tibial vein was punctured, and a guidewire was moved to the CFV to facilitate thrombectomy, using a Fogarty catheter to remove as much of the remaining thrombus as possible. Patch angioplasty using the GSV was considered, but venous flow through the GSV was superior on preoperative ultrasound. Therefore, the vein was reconstructed using an Edwards bovine pericardial patch (Edwards Lifesciences Corp., Irvine, CA, United States).
The venous flow was restored, and the swelling of the right leg was completely recovered before discharge. Intravenous heparinization was performed for 7 d, after which the patient was switched to direct oral anticoagulants (apixaban). The inferior vena cava filter was removed on postoperative day 11, and the patient was discharged on postoperative day 12.
Apixaban was discontinued because DVT was no longer observed on computed tomography venography performed 6 mo after surgery. The patient is currently under follow-up as an outpatient and has been without recurrence for 1 year after surgery.
The present case report sheds light on the rare and often misdiagnosed entity of VACD. VACD is a rare condition, accounting for only 0.1% of all vascular diseases[4]; however, it is challenging to diagnose and manage due to its nonspecific clinical manifestations and resemblance to other vascular anomalies.
VACD is a benign vascular anomaly characterized by the formation of cystic structures within the adventitial layer of the veins. The presentation of this condition varies widely, ranging from asymptomatic incidental findings on imaging to cases with symptoms, such as pain, swelling, or compression of adjacent structures. Enlarged cysts can exert localized focal pressure on target vessels, leading to claudication or obstruction of venous outflow and limb swelling[3]. The rarity of this disease often leads to misdiagnosis or delayed diagnosis of DVT, femoral aneurysms, venous tumors, or lymphadenopathy, highlighting the need for clinical suspicion[5]. Over a period of 50 years (1963-2016), according to an extensive literature review on 45 cases of VACD, it was found that the femoral vein was the most common location of VACD lesions (56%), followed by the external iliac vein (24%), extra-saphenous vein (13%), and the popliteal vein (7%)[1]. The average age of patients participating in this study was 47 years, with 50% being male.
The pathogenesis of ACD is attributed to adventitial cystic degeneration caused by repetitive trauma, de novo adventitial degeneration caused by systemic processes, and resting residual mesenchymal cells[6]. The articular (synovial fluid) theory of the development of ACD has been proposed[2,7,8]. In particular, this theory about the cause of arterial ACD is predominant in the literature[8,9]. As the etiology of VACD is unclear and may differ from that of arterial ACD, adjacent structures must be thoroughly investigated during surgery to rule out events that are unlikely to be part of the underlying etiology of the disease.
Diagnostic imaging plays a pivotal role in confirming the presence of VACD and differentiating it from other vascular lesions. Ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) are commonly performed. VACD can be suspected upon careful examination of the duplex ultrasound; however, both CT angiography and MRI are usually needed to confirm the diagnosis and rule out other coincidental pathologies[10]. A venogram may reveal crescentic compression (the “scimitar sign”) on the target vein, with distal venous distension[11,12]. Intravascular ultrasound has also been used to delineate lesions and estimate the degree of compression[13]. The increased sensitivity of CT and MRI in the venous phase has improved their use for making an accurate diagnosis, without the need for further invasive tools[3]. The characteristic features include well-defined cystic structures adjacent to the veins, which often show fluid–fluid levels on imaging.
In ACD, cysts tend to recur even after treatment[14]. Minimally invasive management of adventitial cysts by image-guided needle aspiration has been reported, but the recurrence rate is high because secondary cyst drainage is incomplete due to the high viscosity of the mucinous material in the cyst, and mucus-secreting mesenchymal cells remain in place[6,11]. Endovascular treatment is also ineffective because it does not address the underlying cause of compression, and it can be problematic for cross-articular lines of stents and thrombosis of low-flow veins[15]. Therefore, physicians must use surgical intervention as the treatment of choice. If the patient's vein is intact and the lumen has no damage, transluminal or transadventitial evacuation of the cyst is performed prior to cyst wall excision. As the recurrence rate is 20%, surgeons must carefully perform thorough wall resection. If the wall is not properly excised, mesenchymal cells of the bursa may remain in the adventitia and secrete sufficient mucus leading to recurrence[1]. Vein resection with graft placement in either the great or small saphenous veins has a recurrence rate of 14.3%. However, this method should only be used when the vein being treated is damaged or when the surgeon is unable to visualize and operate on the vessel adequately[16].
VACD can be misdiagnosed as DVT, femoral varices, venous tumors, or lymphadenopathy. To prevent its recurrence, it is crucial to remove the connections to the joint cavity completely.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ren WR, China S-Editor: Lin C L-Editor: Filipodia P-Editor: Yu HG
| 1. | Bascone C, Iqbal M, Narh-Martey P, Szuchmacher M, Cicchillo M, Krishnasastry KV. Venous Adventitial Cystic Disease: A Review of 45 Cases Treated Since 1963. Int J Vasc Med. 2016;2016:5287697. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Desy NM, Spinner RJ. The etiology and management of cystic adventitial disease. J Vasc Surg. 2014;60:235-245, 245.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Mousa AY, Alhalbouni S, Abu-Halimah S, Gill G, Sadek B, Nanjundappa A, Hass SM, Aburahma AF. Cystic adventitial disease of the common femoral vein: a case report and review of the literature. Vasc Endovascular Surg. 2013;47:569-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Ann JH, Kim JH, Byun SS, Kang JM, Kim HS, Choi HY. Percutaneous Ethanol Sclerotherapy for Recurrent Adventitial Cystic Disease of External Iliac Vein after Surgical Treatment: A Case Report. J Korean Soc Radiol. 2015;73:384-388. [DOI] [Cited in This Article: ] |
| 5. | Min SK, Han A, Min S, Park YJ. Inconsistent Use of Terminology and Different Treatment Outcomes of Venous Adventitial Cystic Disease: A Proposal for Reporting Standards. Vasc Specialist Int. 2020;36:57-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Lun Y, Zhang J, Jiang H, Xu D, Sun J, Wang S, Xin S. Treatment Options for Venous Cystic Adventitial Disease: A Case Report and Literature Review. Ann Vasc Surg. 2020;64:413.e1-413.e4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Dix FP, McDonald M, Obomighie J, Chalmers N, Thompson D, Benbow EW, Smyth JV. Cystic adventitial disease of the femoral vein presenting as deep vein thrombosis: a case report and review of the literature. J Vasc Surg. 2006;44:871-874. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Admetller-Castiglione X, Dı´az-Torrens J, Pa~nella-Agustı´ F, Rodríguez-Espinosa N, García-Vidal R, Mellado-Joan M, Martin-Paredero V. Quiste adventicial de arteria poplítea y su relación con la articulación de la rodilla. Histología y resonancia magnéticaAdventitial cyst of the popliteal artery and its relation to the knee joint. histology and magnetic resonance imaging. Angiología. 2005;57:243-246. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Paravastu SC, Regi JM, Turner DR, Gaines PA. A contemporary review of cystic adventitial disease. Vasc Endovascular Surg. 2012;46:5-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Wiwanitkit V. Cystic adventitial disease and high spatial resolution magnetic resonance imaging. Ann Vasc Surg. 2012;26:443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Wick MC, Tauscher T, Rieger M. Claudication due to cystic adventitial degeneration: a classical differential diagnosis of atherosclerotic peripheral artery disease. Circulation. 2012;125:1926-1927. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Hong JS, Lee KB, Kim DK, Kim DI. Cystic adventitial disease of the popliteal artery: report of a case. Surg Today. 2007;37:719-722. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Vos LD, Tielbeek AV, Vroegindeweij D, van den Bosch HC, Buth J. Cystic adventitial disease of the popliteal artery demonstrated with intravascular US. J Vasc Interv Radiol. 1996;7:583-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Seo JY, Chung DJ, Kim JH. Adventitial cystic disease of the femoral vein: a case report with the CT venography. Korean J Radiol. 2009;10:89-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Johnson JM, Kiankhooy A, Bertges DJ, Morris CS. Percutaneous image-guided aspiration and sclerosis of adventitial cystic disease of the femoral vein. Cardiovasc Intervent Radiol. 2009;32:812-816. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Sugimoto T, Yamamoto K, Tanaka S, Saitou N, Kikuchi C, Motohashi S, Kasuya S. Adventitial cystic disease of the femoral vein: report of a case. Surg Today. 2004;34:286-288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |