Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.12844
Peer-review started: August 19, 2022
First decision: September 30, 2022
Revised: October 10, 2022
Accepted: November 30, 2022
Article in press: November 30, 2022
Published online: December 16, 2022
The variability of vascular anatomy of the pancreas underlines the difficulty of its transplantation. Research regarding the consistency of anatomical variations shows splenic arterial dominance in most cases. This can significantly improve transplantation success. A systematic literature review was performed according to the quality standards described in the AMSTAR measurement tool and the PRISMA guidelines. We valuated existing literature regarding the vascularization and blood perfusion patterns of the pancreas in terms of dominance and variability. The collected data was independently analyzed by two researchers. Variance of vascular anatomy was seen to be underreported in literature, though significant findings have been included and discussed in this study, providing valuable insight into the dynamics of pancreatic perfusion and feasibility of transplantation on several different supplying arteries. The splenic artery (SA) has a high percentage of consistency in all found studies (over 90%). High frequency of anastomoses between arterial pools supplying the pancreas can mediate sufficient blood supply through a dominant vessel, such as the SA, which is present in most cases. Pancreatic transplantation with isolated SA blood supply can provide sufficient arterial perfusion of the pancreas for stable transplant viability due to high anatomical consistency of the SA and vast communications with other arterial systems.
Core Tip: We summarize existing findings on the variant anatomy of pancreatic blood supply to justify, from an anatomical point of view, the possibility of pancreatic transplantation with isolated splenic artery blood supply (ISABS). The blood supply of the pancreas is characterized the absence of a single large source arterial inflow, and an intimate communication with arteries of the surrounding organs. The practical significance of anatomical features of blood supply of cephalocervical and corporocaudal segments of the pancreas and well-described numerous arterial collaterals and anastomoses of these areas are the basis for establishing collateral circulation in cases of reduced blood flow through one or more arteries or in case of pancreatic transplantation with ISABS.
- Citation: Dmitriev I, Oganesyan M, Popova A, Orlov E, Sinelnikov M, Zharikov Y. Anatomical basis for pancreas transplantation via isolated splenic artery perfusion: A literature review. World J Clin Cases 2022; 10(35): 12844-12853
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/12844.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.12844
Pancreatic transplantation is the “gold standard” in surgical treatment of patients with type 1 diabetes mellitus, allowing for restoration of stable euglycemia with underlying insulin independence[1]. Russia has reported over 4.5 million patients with diabetes mellitus[2]. Gruessner et al[3] reported that from 2001 to 2016, the annual number of pancreatic transplantations according to the International Pancreas Transplant Registry/United Network of Organ Sharing registry ranged from 860-1200. Forty-one pancreas transplantations were performed in Russia between 2015 and 2018[4]. The need for pancreatic transplantation does not correspond to the number of transplantations performed, due to critical deficit of donor organs. Furthermore, due to strict selection criteria for potential donors, 30% of pancreatic grafts obtained during multi-organ harvesting are recognised as unsuitable for transplantation[5]. While it a first choice for a pancreatic graft is a transplant with a preliminary standard arterial reconstruction using a Y-shaped prosthesis, in some cases different vascular pedicles may be used. We summarise existing findings on the variant anatomy of pancreatic blood supply to justify, from an anatomical point of view, the possibility of pancreatic transplantation with isolated splenic artery blood supply (ISABS).
A thorough literature search for information regarding the variable anatomy of pancreatic arterial supply the Google Scholar, EMedicine, and PubMed databases was performed. The references of found articles were reviewed and a citation search was conducted. The review was performed according to the quality standards described in the AMSTAR measurement tool and the PRISMA checklist. The PICO model formed the basis of the search strategy. Two co-authors independently selected, evaluated, and extracted data. Keywords of the strategy of the search were the following: pancreas, arterial supply, blood supply, pancreatic anatomy, vascular anatomy, common arteries of pancreas. The criteria for inclusion were limited to the presence of experimental or clinical findings on the consistency of pancreatic blood supply via variable arterial systems. Exclusion of articles was performed due to lack of information about arterial vessels of the pancreas, insufficient data regarding the consistency of arterial anatomy, lack of comparative analysis and qualitative measurement. Due to the nature of the study (literature review), ethical approval was waived.
A total of 793 information sources were studied, of which only 24 studies were used to form a hypothesis. The results can be categorized into three groups: embryological aspects of pancreatic blood supply variability; anatomical findings on consistency of pancreatic blood supply; substantiation of isolated splenic artery (SA) for pancreatic transplantation.
The main stages of pancreatic development during embryogenesis define the peculiarities of arterial blood supply to its segments (Figure 1). The pancreas develops from two endodermal rudiments (foregut diverticulum): the dorsal (splenic) and ventral (hepatic).
The dorsal rudiment of the pancreas, with its duct, develops at 4 wk in the mesentery of the duodenum (mesoduodenum), with blood supply from branches of the SA. The ventral rudiment of the pancreas develops by 4.5-5 wk (along with rudiments of the liver, gallbladder, and associated ducts from the liver diverticulum) with blood supply from branches of the common hepatic artery (CHA). Following the turn of the duodenum to the right, the ventral rudiment moves to the back and becomes adjacent to the dorsal rudiment. Then they are conjoined within 6 wk, and their ducts are anastomosed.
Formation of the pancreas from two embryonic rudiments and its structural features as a gland with mixed secretion explain the peculiarity of blood supply to the organ via branches of various arterial systems[6-8]. Taking into account the embryotic development of the pancreas, an adult pancreas can be divided into two segments: the ventral (posteroinferior part of the head, and most of the uncinate process), and dorsal (anterosuperior part of the head, apex of the uncinate process, body, and tail) segments[9].
From the anatomical-surgical point of view[10,11], the pancreas is divided into two segments: right (cephalocervical) and left (corporocaudal), separated by a poorly vascularised area. They are then divided into 5 anatomical parts: head, neck (isthmus), uncinate process, body, and tail. The vascular anatomy of the pancreas remains unstandardized, despite a rich history of published findings[12-14]. Existing data on the blood supply of the pancreas are ambiguous, which is explained by different variants of vessel distribution in the pancreas during embryogenesis as well as by the retention or reduction of primary arterial pancreatic vessels, individual features of topographic anatomy, age, constitution and different pancreatic pathology.
Bertelli et al[12,15,16] showed that the arterial blood supply to the pancreas stems from three main sources: the gastroduodenal artery (GDA), SA, and superior mesenteric artery (SMA). These vessels form a network of anastomoses, trunks, and arches (arcades), both on the surface of the gland and within the parenchyma.
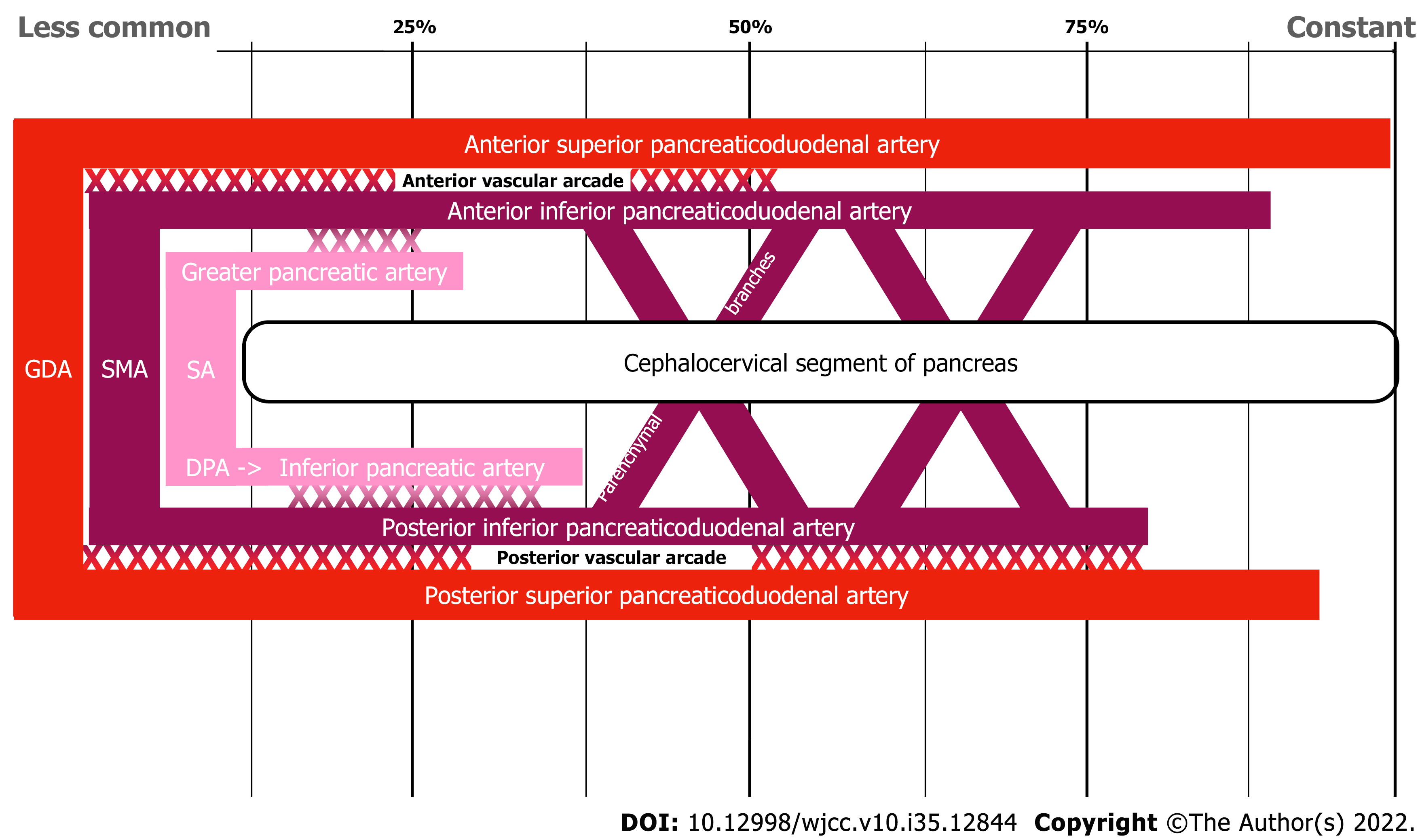
According to the International Anatomical Terminology, the arteries of the pancreas are as follows: anterior and posterior superior pancreaticoduodenal arteries, inferior pancreaticoduodenal artery with anterior and posterior branches, and pancreatic branches of the SA [dorsal pancreatic artery (DPA), greater pancreatic artery (GPA), artery to the tail of the pancreas, prepancreatic artery, transverse, or inferior pancreatic artery (TPA, or IPA)].
Blood supply to the head of the pancreas comes from branches originating from the GDA and SMA. The GDA gives off a branch—the superior pancreaticoduodenal artery (SPDA), which divides into the anterior SPDA (ASPDA) and the posterior SPDA (PSPDA). The SMA continues as the inferior pancreaticoduodenal artery (IPDA), from which anterior (AIPDA) and posterior (PIPDA) branches originate. Inferior pancreaticoduodenal vessels are much more variable in origin and topography than superior pancreaticoduodenal vessels. In this region, the anterior and posterior pancreaticoduodenal arcades serve as origins for smaller branches involved in the formation of secondary parenchymal arcades[14].
Akstilovich et al[17] investigated the anatomy of arteries of the head of the pancreas in 55 human organ complexes with dissection, polychrome arterial injection of gelatin-based die solutions, X-ray angiography, morphometry, and multispiral computer tomography. The main arteries of the head of the pancreas are the ASPDA, PSPDA AIPDA, and the PIPDA. Additional arteries involved in the blood supply to the head of the pancreas are the IPA and GPA. An additional source of blood supply to the pancreatoduodenal region is the DPA, the right branch of which forms an anastomosis with the anterior pancreaticoduodenal arterial arc in the form of IPA (Figure 2, Table 1).
| Source of blood supply | Consistency (%) | ||
| Akstilovich etal[17]
| Macchi etal[18] | ||
| Cephalocervical segment | |||
| Gastroduodenal artery | Anterior superior pancreaticoduodenal artery | 100 | 92.6 |
| Posterior superior pancreatoduodenal artery | 92.7 | 100 | |
| Superior mesenteric artery | Anterior inferior pancreaticoduodenal artery | 98.2 | 73.1 |
| Posterior inferior pancreaticoduodenal artery | 87.3 | 86.4 | |
| Splenic artery | Greater pancreatic artery | 14.5 | - |
| Inferior pancreatic artery | 21.8 | - | |
Macchi еt al[18] described the blood supply of the cephalocervical segment of the pancreas based on injection of acrylic resins to obtain vascular moulds and 30 computed tomography angiography (CTA) image sets. According to their data, the PSPDA is visualised in 100% of cases, ASPDA in 92.6%, anterior branch of IPDA in 73.1%, and posterior branch of IPDA in 86.4% of cases (Table 1).
Branches of the SPDA and IPDA form the anterior and posterior arterial arcades with variable anastomoses between them[12]. Pronin et al[19] showed that a greater number of branches originate from the posterior vascular arc than from the anterior one. According to Bertelli et al[20], the anterior pancreatic arterial arcade may be absent in 50% of cases and the posterior in just 20% of cases.
The number of arteries involved in the formation of two arterial arcades, in the head of the pancreas can significantly differ[6,13,21,22]. Authors Macchi et al[18] reported that the number of arteries involved in the formation of the superior arcade varies from two to six, and for the inferior arcade—from two to four. Szuák et al[23] also determined the frequency of variants of pancreaticoduodenal arterial arcades by injection of a resin mixture into the vessels of human organ complexes (n = 50) of the abdominal cavity using the corrosion method. CT imaging and three-dimensional reconstruction showed that two arcades were found in 58%, three arcades in 30%, one arcade in 6%, four arcades in 2%, and five arcades in 4% of cases, with the anterior arc being dominant in 52% of the cases.
The blood supply of the corporocaudal segment of the pancreas is characterized by considerable variability (Figure 3)[16,24-26]. The SA is considered to be the dominant source of blood supply to the body and tail of the pancreas. The DPA most often originates from the SA, but can be a branch of the CHA, SMA, or coeliac trunk[16,18,19,27-29].
Akstilovich et al[30] identified the dominant vessel as the SA (in 87.3% of cases), coeliac trunk (in 3.6% of cases), and CHA (in 9.1% of cases) as main arteries of the body and tail of the pancreas, based on dissection and angiograms of the pancreas. The authors noted that the “classic” version of blood supply to the body and tail of the pancreas is via: the DPA and GPA. In 84.1% of all cases the DPA originates from the SA, in 11.4% of cases, from CHA and in 4.5%, from coeliac trunk.
Tarasov et al[31] revealed that in 76% of cases, vascularisation of the corporocaudal segment of the pancreas is carried out only by branches of SA, in 15% of cases by branches of the CHA, in 6% of cases by branches of SA and SMA, and in 3% of cases by branches of SA together with gastric arteries. In 15% of cases, the final pancreatic branch going to the tail of the gland originated from one of the terminal branches of the SA rather than the main arterial trunk.
Wu et al[32], performed, found that the body and tail of the pancreas were supplied by the DPA in 50% of cases; DPA and GPA in 21.6% of cases; by solely GPA in 15.7% of cases; by TPA in 10.8% of cases. The DPA originates from the proximal segment of SA in 46.6% of cases, from CHA in 23.3%, and from SMA in 19.2% of cases. GPA originates mainly from the middle segment of the SA in 94.7% of cases. TPA originates from IPDA in 54.5% and from GDA in 36.4% of cases.
According to studies by Pronin et al[19] in 2016, the DPA originates from the proximal segment of the SA in 91.1% of cases, less often from the coeliac trunk, CHA, and SMA. According to the area of blood supply and anastomoses, IPA and DPA are interchangeable. Neither artery was found in the same investigated complex.
Covantev et al[33] using gross dissection (50 cases) and the corrosion cast method (22 cases), distinguished three main types of vascularisation of the distal segment of the pancreas: type 1, only short branches of SA (36% of cases on the macroscopical dissection specimen and 36.4% of cases on corrosion cast specimens); type 2, long and short SA branches (40% of cases on the specimen and 45.5% in case of corrosion cast specimens); and type 3, only long branches of SA (24% and 18%, respectively). The corrosion cast method identified the absence of arteries in the tail in 18.2% cases, one artery in 27.27% cases, two arteries in 45.46% cases, and three arteries in 9.09% cases. The authors noted that DPA was present in 76% of cases; GPA in 46% of cases, and the pancreas was supplied by both DPA and GPA only in 26% of cases.
Woodburne and Olsen[14] showed that the GPA originated from the GDA in 37.5% of cases and from ASPDA in 14.5% of cases. The artery moves along the anterior surface of the head of the pancreas, then along the lower edge of the neck, and in the area of the body comes anastomoses with pancreatic branches from the SA. In 62.5% of cases, both the GPA and DPA are observed, which anastomose among themselves. The authors describe the IPA along the inferior margin of the pancreas as the left branch of the DPA present in most cases (84%). The GPA enters the parenchyma of the pancreas from the SA between the middle and left third and is observed in 64.7% of cases. The artery to the tail of the pancreas reaches the tail originating mainly from the SA or the left gastro-omental artery and is observed in 78.7% of cases.
According to Kulchitsky et al[34], the GPA can be observed in the absence of the DPA and IPA in 14% of cases. It originates from the GDA or IPA and moves along the anterior surface of the head and neck of the pancreas (as the right branch of the DPA or IPA), then, in the body of the pancreas (as the left branch of the DPA or IPA) goes towards the tail, connecting with arterial anastomoses from branches of the SA.
Kopchak et al[35] reported that DPA, IPA, and GPA are interchangeable according to the blood supply area and branches. Kulenović and Sarač-Hadžihalilović[25] described arteries with an abundant anastomotic network, originating from SA and travelling to the body and tail of the pancreas, with a pronounced GPA, DPA, or IPA and an artery to the tail of the pancreas to form arcades of different shapes and sizes. As in many previous studies, the authors confirmed that the arteries of the body of the pancreas anastomose with the arteries of its head. In all cases, anastomoses are formed through the DPA between the arteries of the head and tail of the pancreas. The body and tail of the pancreas, on the whole, are supplied by the SA, through one to five collateral branches. According to their data, the SA and vein form one vascular axis sufficient to supply the corporocaudal segment of the pancreas during transplantation.
Okahara et al[36] performed 226 selective abdominal angiographies (SAA) and scans in selective CT angiography (CTA). As a result, they divided the body of the pancreas, depending on the vascular supply, into the superior and inferior parts supplied by the DPA and GPA, and the tail of the pancreas into the superior and inferior sections supplied by TPA and GPA, and the terminal caudal segment supplied with caudal pancreatic arteries.
The presence of a superior horizontal pancreatic artery in combination with IPA provides blood supply to the distal part of the pancreas[29]. Mosca et al[37] using SAA on 1000 angiograms, visualised the superior horizontal pancreatic artery as a variant of the GPA in 25.93% of cases. The artery gives origin to the descending branches that anastomose with the IPA.
Baranski et al[38] believed that the DPA provides basic blood supply to the pancreatic tail and plays an important role in the vascularization of pancreatic grafts. In rare cases, when the DPA originates from the CHA or coeliac trunk, instead of a splenic origin, it can be easily missed by surgeons, which can lead to unintentional impairment of the blood supply of the tail of the pancreas, and pose harm to the pancreatic graft after reperfusion.
Macchi еt al[18] described the blood supply of the corporocaudal segment of the pancreas based on the injection of acrylic resins to obtain vascular casts and using the results of the analysis of 30 CTA. In CTA transverse (inferior) pancreatic artery (TPA, or IPA), the only artery travelling from the cephalocervical segment to the corporocaudal segment is detected in 76.9% of cases; suprapancreatic SA is observed in 66.7% and intrapancreatic SA with the winding course in 33.3%; DPA is observed in 86.4% of cases; GPA in 73.1%; and arteries of the body of the pancreas and artery to the tail of pancreas in 96.2% of cases.
Most transplant centres perform pancreatic transplantation using Y-graft arterial reconstruction to restore the pancreas graft blood supply via the SMA and SA. In cases where it is not applicable due to variant arterial anatomy, surgeons utilise any graft suitable for transplantation. Troppmann et al[39] were the first who mentioned in their article the possibility of pancreatic allograft survival following partial Y-graft thrombosis due to dual blood supply (SMA, SA).
Hagspiel et al[40] described a patient with occlusion of the SMA of the pancreas graft and preserved patency of the SA. They were the first who radiologically documented with MR angiography that patency of only one pancreatic graft artery as sufficient to supply adequate perfusion to the entire pancreatic graft.
Margreiter et al[41] analysed graft function in recipients experiencing a thrombotic occlusion of one branch of the Y-graft and found that the occurrence of anastomoses between the SA and SMA, but particularly to the pancreaticoduodenal arcade, was observed in all specimens. In view of the functional importance of such anastomoses in pancreatic surgery, the authors proposed the term “splenocephalic anastomoses”, which can be considered as ways of collateral circulation in addition to the two pancreatic arcades. During the anatomical study using angiography, excellent perfusion of the pancreaticoduodenal arcade via intraparenchymal anastomoses was shown in all cases after isolated injection of even low volumes of contrast medium into the SA. Even after occlusion of the SMA, sufficient global perfusion of the pancreatic graft was provided by the SA through retrograde perfusion of the pancreaticoduodenal arcade, thus bringing into question the need for a Y-graft at all.
Matsumoto et al[42] described a case of a functioning pancreatic graft with occlusive thrombosis of the splenic and superior mesenteric arteries after simultaneous pancreas-kidney transplantation. In that case, pancreas graft perfusion was maintained via the I-graft in the head of the pancreas and the transverse pancreatic artery in the body and tail of the pancreas with SA and SMA thrombosis.
The problem of the critical deficit of donor organs and pancreatic graft utilisation when Y-graft reconstruction is not applicable was resolved by the idea of performing pancreatic transplantation with ISABS. Pinchuk et al[43] conducted an anatomical study of the viability of pancreatic transplantation with ISABS and introduced this method to clinical practice. They performed an anatomical study using a transplant model with ISABS. The SA contrast-enhanced X-ray examination showed the presence of a sufficiently developed system of collaterals between its system and the SMA system, which enabled adequate perfusion to be achieved in all parts of the transplant. 3D computed tomography reconstruction with contrast enhancement and CT perfusion enabled them to prove the sufficient blood supply of PG’s parenchyma in the study group and uniform blood supply of the transplant through the collateral system between the splenic and superior mesenteric arteries[43].
Adequate and sufficient perfusion of all segments of the graft with ISABS is justified and possible due to the development of collateral systems between the SA and SMA. The most frequent anastomoses of these systems are provided by the DPA and IPA (TPA). DPA provides basic blood supply to the tail of the pancreas together with SA[18,38,44]. Variants of DPA origin affect arterial vascularisation of the pancreas, the number of collaterals, and anastomoses with other arterial vessels of different organ segments[45,46]. The presence of a superior horizontal pancreatic artery in combination with IPA provides blood supply to the distal part of the pancreas[29]. Thus, DPA, which in most cases originates from the SA, is divided into two branches travelling in opposite directions: one branch, like Kirk’s anastomosis, travels to the ASPDA, that is, to the anterior pancreatic arcade, and the other branch travels to the body and tail of the pancreas[16,33,35,38,47-49]. As a result, an anastomotic arc is formed, which travels along with the head, neck, and body of the pancreas. The TPA, when originated from GDA or its branches, runs along the inferior surface of the body and tail of the pancreas, anastomoses with the branches of the DPA or GPA[48]. The arteries of the tail of the pancreas form anastomoses between the branches of the DPA and GPA. Arterio-arterial intracorporeal anastomoses with caudal arteries have been previously described[16,18,29,30,50,51]. Anterior and posterior anastomotic arcades in 86.3% of cases are connected by communicant arteries, which are referred to as the middle pancreatic arterial arcade[12,49].
At the time of preparation of this article, there was one published description of the single-centre experience of pancreatic transplantation with ISABS[43]. The method was proposed to use organs that were previously recognised as unsuitable and were utilised for disposal[43].
The blood supply of the pancreas is characterized the absence of a single large source arterial inflow, and an intimate communication with arteries of the surrounding organs. The arterial blood comes from the CHA, SMA, and SA, and the topography of the pancreatic arteries is characterised by the presence of anastomoses between them.
In the head of the pancreas, the anterior and posterior pancreaticoduodenal arcades are formed between the ASPDA and PSPDA and the anterior and posterior branches of the IPDA, respectively. The number of such arcades can vary from two to six. Moreover, the anterior and posterior arteries are connected by communicant arteries.
Despite the fact that the pancreas is divided into cephalocervical and corporocaudal segments, based on the type of blood supply, it is difficult to consider the pancreas as a classic segmental organ. Of particular importance are anastomoses that combine arterial systems of the right cephalocervical and left corporocaudal segments. The system of blood vessels that branches off from the GDA and SMA, supplying the head of the pancreas, is involved in the blood supply of the body and tail of the pancreas by anastomoses with DPA, GPA, or IPA. According to many authors, anastomoses formed by the right branch of the DPA and ASPDA (branch of GDA), the so-called “Kirk’s anastomosis”, are often found.
In rare cases, the pancreas does not have a large number of anastomoses between branches[33]. Although the vessels of the body and tail of the pancreas are often anastomosed with the vessels of its head, some authors claim that in 42.1% of cases, the tail has an autonomous blood supply[52]. This should also be taken into account when considering the transplantation of the pancreas with ISABS.
The topography of the arteries of the pancreas is characterised by significant variability, which should be considered in case of surgical interventions. The practical significance of anatomical features of blood supply of cephalocervical and corporocaudal segments of the pancreas and well-described numerous arterial collaterals and anastomoses of these areas are the basis for establishing collateral circulation in cases of reduced blood flow through one or more arteries or in case of pancreatic transplantation with ISABS.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anatomy and morphology
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Aseni P, Italy; Wang P, China S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Press M. The nature of the problem: why do we need pancreatic transplantation? In: Hakim NS and others (eds). Pancreas, Islet and Stem Cell Transplantation for Diabetes, 2 edn (Oxford, 2010; online edn, Oxford Academic, 1 May 2013). [DOI] [Cited in This Article: ] |
| 2. | Dedov II, Shestakova MV, Vikulova OK, Zheleznyakova AV, Isakov MА. Diabetes mellitus in Russian Federation: prevalence, morbidity, mortality, parameters of glycaemic control and structure of glucose lowering therapy according to the Federal Diabetes Register, status 2017. Diabetes mellitus. 2018;21:144-159. [Cited in This Article: ] |
| 3. | Gruessner AC, Gruessner RWG. Pancreas Transplantation for Patients with Type 1 and Type 2 Diabetes Mellitus in the United States: A Registry Report. Gastroenterol Clin North Am. 2018;47:417-441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 4. | Gautier SV, Khomyakov SM. Organ donation and transplantation in the Russian Federation in 2018. 11th report of the Registry of the Russian Transplant Society. Russian Journal of Transplantology and Artificial Organs. 2019;21:7-32. [DOI] [Cited in This Article: ] |
| 5. | Adamson D, Holzner ML, Wadhera V, Shapiro R. Reconstruction of a Pancreatic Allograft With Variant Arterial Anatomy for Transplantation. Transplant Direct 2019; 5: e425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Skandalakis LJ, Rowe JS Jr, Gray SW, Skandalakis JE. Surgical embryology and anatomy of the pancreas. Surg Clin North Am. 1993;73:661-697. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Suda K, Mizuguchi K, Hoshino A. Differences of the ventral and dorsal anlagen of pancreas after fusion. Acta Pathol Jpn. 1981;31:583-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Takada T, Yasuda H, Uchiyama K, Hasegawa H, Iwagaki T, Yamakawa Y. A proposed new pancreatic classification system according to segments: Operative procedure for a medial pancreatic segmentectomy. J Hep BilPancr Surg. 1994;1:322-325. [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Suda K, Nobukawa B, Takase M, Hayashi T. Pancreatic segmentation on an embryological and anatomical basis. J Hepatobiliary Pancreat Surg. 2006;13:146-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Bertelli E, Di Gregorio F, Bertelli L, Civeli L, Mosca S. The arterial blood supply of the pancreas: a review. II. The posterior superior pancreaticoduodenal artery. An anatomical and radiological study. Surg Radiol Anat. 1996;18:1-9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 72] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Snopok Iu, Matevossian É. [Organ-preserving and segmental resections of the head of the pancreas: anatomic substantiation and surgical technique]. Vestn Khir Im I I Grek. 2014;173:100-105. [PubMed] [Cited in This Article: ] |
| 12. | Bertelli E, Di Gregorio F, Bertelli L, Mosca S. The arterial blood supply of the pancreas: a review. I. The superior pancreaticoduodenal and the anterior superior pancreaticoduodenal arteries. An anatomical and radiological study. Surg Radiol Anat. 1995;17:97-106, 1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 49] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Woodburne RT, Olsen LL. The arteries of the pancreas. Anat Rec. 1951;111:255-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Bertelli E, Di Gregorio F, Bertelli L, Civeli L, Mosca S. The arterial blood supply of the pancreas: a review. III. The inferior pancreaticoduodenal artery. An anatomical review and a radiological study. Surg Radiol Anat. 1996;18:67-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Bertelli E, Di Gregorio F, Mosca S, Bastianini A. The arterial blood supply of the pancreas: a review. V. The dorsal pancreatic artery. An anatomic review and a radiologic study. Surg Radiol Anat. 1998;20:445-452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Akstilovich ICh. Arteries of the head of the human pancreas. Bulletin of the Vitebsk State Medical University. 2009;8:13-20. [Cited in This Article: ] |
| 18. | Macchi V, Picardi EEE, Porzionato A, Morra A, Bardini R, Loukas M, Tubbs RS, De Caro R. Anatomo-radiological patterns of pancreatic vascularization, with surgical implications: Clinical and anatomical study. Clin Anat. 2017;30:614-624. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Pronin NA, Tarasenko SV, Pavlov AV, Suchkov I. Operative Treatment of Chronic Pancreatitis with Regard to Anatomical Features of Arterial Network in the Pancreatic Head. Novosti Khirurgii. 2016;24:348-354. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Bertelli E, Di Gregorio F, Bertelli L, Orazioli D, Bastianini A. The arterial blood supply of the pancreas: a review. IV. The anterior inferior and posterior pancreaticoduodenal aa., and minor sources of blood supply for the head of the pancreas. An anatomical review and radiologic study. Surg Radiol Anat. 1997;19:203-212. [PubMed] [Cited in This Article: ] |
| 21. | Chong M, Freeny PC, Schmiedl UP. Pancreatic arterial anatomy: depiction with dual-phase helical CT. Radiology. 1998;208:537-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Hong KC, Freeny PC. Pancreaticoduodenal arcades and dorsal pancreatic artery: comparison of CT angiography with three-dimensional volume rendering, maximum intensity projection, and shaded-surface display. AJR Am J Roentgenol. 1999;172:925-931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Szuák A, Németh K, Korom C, Gáti E, Karlinger K, Harsányi L, Nemeskéri Á. Pancreaticoduodenal arterial arcades: Their dominance and variations-their potential clinical relevance. Clin Anat. 2018;31:544-550. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Fontaine C, Francke JP, Ribet M, Libersa C. [Arterial vascularization of the tail of the pancreas]. Bull Assoc Anat (Nancy). 1981;65:93-100. [PubMed] [Cited in This Article: ] |
| 25. | Kulenović A, Sarac-Hadzihalilović A. Blood vessels distribution in body and tail of pancreas- a comparative study of age related variation. Bosn J Basic Med Sci. 2010;10:89-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Martin R, GOUPPIE G. Étude des variations des branches du tronc artériel pancréatico-duodéno-jéjunal. Presse Med. 1960;68:1266-1266. [Cited in This Article: ] |
| 27. | Ibukuro K. Vascular anatomy of the pancreas and clinical applications. Int J Gastrointest Cancer. 2001;30:87-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Murakami G, Hirata K, Takamuro T, Mukaiya M, Hata F, Kitagawa S. Vascular anatomy of the pancreaticoduodenal region: A review. J Hepatobiliary Pancreat Surg. 1999;6:55-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 47] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Ross B, Fox M. Blood supply of the distal part of the human pancreas: a study with segmental pancreatic transplantation in view. Transplantation. 1981;31:134-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Akstilovich ICh, Zhuk IG, Kiselevsky YuM. Variant anatomy of the arteries of the body and tail of the human pancreas. Journal of the Grodno State Medical University. 2010;2:35-38. [Cited in This Article: ] |
| 31. | Tarasov AN. Questions at issue of the resection and pancreas transplantation in aspect of blood supply features. Sibirskij medicinskij zhurnal. 2010;25:90-93. [Cited in This Article: ] |
| 32. | Wu ZX, Yang XZ, Cai JQ, Liao LM, Yang L, Lin YN, Tan JM. Digital subtraction angiography and computed tomography angiography of predominant artery feeding pancreatic body and tail. Diabetes Technol Ther. 2011;13:537-541. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Covantev S, Mazuruc N, Belic O. The Arterial Supply of the Distal Part of the Pancreas. Surg Res Pract. 2019;2019:5804047. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Kulchitsky K, Bobrik I. Blood supply to the human digestive tract. Kiev: Zdorov'ya 1970: 42. [Cited in This Article: ] |
| 35. | Kopchak V, Usenko A, Kopchak K, Zelenskiy A. Khirurgicheskaya anatomiya podzheludochnoy zhelezy. Kiev: Ascania, 2011: 23-43. [Cited in This Article: ] |
| 36. | Okahara M, Mori H, Kiyosue H, Yamada Y, Sagara Y, Matsumoto S. Arterial supply to the pancreas; variations and cross-sectional anatomy. Abdom Imaging. 2010;35:134-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 37. | Mosca S, Di Gregorio F, Regoli M, Bertelli E. The superior horizontal pancreatic artery of Popova: a review and an anatomoradiological study of an important morphological variant of the pancreatica magna artery. Surg Radiol Anat. 2014;36:1043-1049. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 38. | Baranski AG, Lam HD, Braat AE, Schaapherder AF. The dorsal pancreatic artery in pancreas procurement and transplantation: anatomical considerations and potential implications. Clin Transplant. 2016;30:1360-1364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Troppmann C, Gruessner AC, Benedetti E, Papalois BE, Dunn DL, Najarian JS, Sutherland DE, Gruessner RW. Vascular graft thrombosis after pancreatic transplantation: univariate and multivariate operative and nonoperative risk factor analysis. J Am Coll Surg. 1996;182:285-316. [PubMed] [Cited in This Article: ] |
| 40. | Hagspiel KD, Nandalur K, Burkholder B, Angle JF, Brayman KL, Spinosa DJ, Matsumoto AH, Veldhuis OL, Sanfey H, Sawyer RG, Pruett TL, Leung DA. Contrast-enhanced MR angiography after pancreas transplantation: normal appearance and vascular complications. AJR Am J Roentgenol. 2005;184:465-473. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Margreiter C, Mark W, Wiedemann D, Sucher R, Öllinger R, Bösmüller C, Freund M, Maier HT, Greiner A, Fritsch H, Pratschke J, Margreiter R, Aigner F. Pancreatic graft survival despite partial vascular graft thrombosis due to splenocephalic anastomoses. Am J Transplant. 2010;10:846-851. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Matsumoto I, Shinzeki M, Asari S, Goto T, Shirakawa S, Ajiki T, Fukumoto T, Ku Y. Functioning pancreas graft with thromboses of splenic and superior mesenteric arteries after simultaneous pancreas-kidney transplantation: a case report. Transplant Proc. 2014;46:989-991. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Pinchuk AV, Dmitriev IV, Anisimov YA, Storozhev RV, Balkarov AG, Kondrashkin AS, Khodilina IV, Muslimov RS. Pancreas transplantation with isolated splenic artery blood supply - Single center experience. Asian J Surg. 2020;43:315-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 44. | Hong SD, Nam DH, Seol HJ, Choi NY, Kim HY, Chung SK, Dhong HJ. Endoscopic binostril versus transnasal transseptal microscopic pituitary surgery: Sinonasal quality of life and olfactory function. Am J Rhinol Allergy. 2015;29:221-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 45. | Pandey SK, Bhattacharya S, Mishra RN, Shukla VK. Anatomical variations of the splenic artery and its clinical implications. Clin Anat. 2004;17:497-502. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Yi N, Yi S, Wang H, Ogawa Y, Ohta T, Ozaki N, Itoh M. Anterior Inferior Pancreaticoduodenal Artery Running Between the Dorsal and Ventral Pancreas: Morphological and Embryological Viewpoint. The Open Anatomy Journal. 2010;2:79-85. [Cited in This Article: ] |
| 47. | Ebeneizer D, Jiji P, Vadgaonkar R, Prabhu LV, Tonse M, Venunadan A. Kirk’s arcade: a case report. Int J Anat Variat. 2009;2:78-79. [Cited in This Article: ] |
| 48. | Kimura W, Hirai I, Yamaguchi H, Wakiguchi S, Murakami G, Kimura Y. Surgical anatomy of arteries running transversely in the pancreas, with special reference to the superior transverse pancreatic artery. Hepatogastroenterology. 2004;51:973-979. [PubMed] [Cited in This Article: ] |
| 49. | Yamaguchi H, Wakiguchi S, Murakami G, Hata F, Hirata K, Shimada K, Kitamura S. Blood supply to the duodenal papilla and the communicating artery between the anterior and posterior pancreaticoduodenal arterial arcades. J Hepatobiliary Pancreat Surg. 2001;8:238-244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 50. | Donatini B. A systematic study of the vascularisation of the pancreas. Surg Radiol Anat. 1990;12:173-180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 32] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 51. | Stingl J, Borůvka V, Brestáková M, Ruzbarský V, Vanék I. Vascularization of the body and tail of the pancreas. Folia Morphol (Praha). 1985;33:338-343. [PubMed] [Cited in This Article: ] |
| 52. | Fiedor P, Kaminski P, Rowinski W, Nowak M. Variability of the arterial system of the human pancreas. Clin Anat. 1993;6:213-216. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |