Published online Jun 18, 2023. doi: 10.5312/wjo.v14.i6.436
Peer-review started: December 28, 2022
First decision: March 24, 2023
Revised: April 14, 2023
Accepted: May 15, 2023
Article in press: May 15, 2023
Published online: June 18, 2023
Fusion of the first metatarsophalangeal (MTP1) joint is a common surgery perfor
To assess outcomes of our surgical technique including non-union rates, accuracy and aims of correction.
Between September 2011 and November 2020 a total 72 of MTP1 fusions were performed using a low profile, pre-contoured dorsal locking plate and a plantar compression screw. Union and revision rates were analyzed with a minimum clinical and radiological follow up of at least 3 mo (range 3-18 mo). The following parameters were evaluated on pre- and postoperative conventional radiographs: Intermetatarsal angle, Hallux-valgus angle, dorsal extension of the proximal phalanx (P1) in relation to the floor and the angle between the Metatarsal 1 and the P1 (MT1-P1 angle). Descriptive statistical analysis was performed. Pearson analysis was used to assess for correlations between radiographic parameters and achievement of fusion.
An overall union rate of 98.6% (71/72) was achieved. Two out of 72 patients did not primarily fuse with one patient suffering from a non-union, whilst the other demonstrating a radiological delayed union without clinical symptoms, with eventually complete fusion after 18 mo. There was no correlation between the measured radiographic parameters and the achievement of fusion. We believe the reason for the non-union was mainly attributed to the patient’s incompliance without wearing the therapeutic shoe leading to a fracture of the P1. Furthermore, we didn`t find any correlation between fusion and the degree of correction.
With our surgical technique, high union rates (98%) can be achieved using a compression screw and a dorsal variable-angle locking plate to treat degenerative diseases of the MTP1.
Core Tip: The most important findings in this study are that metatarsophalangeal joint fusion using a compressions screw and a dorsal plate can achieve union rates close to 100% even in patients that are diabetic or smoke. Furthermore, we didn't find any correlation between the degree of correction and risk of nonunion.
- Citation: von Deimling C, Tondelli T, Brunner S, Andronic O, Graf AD. Achieving high union rates after first metatarsophalangeal joint arthrodesis: Radiographic outcomes and technical pitfalls. World J Orthop 2023; 14(6): 436-442
- URL: https://www.wjgnet.com/2218-5836/full/v14/i6/436.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i6.436
Arthrodesis of the metatarsophalangeal (MTP1) joint is a common surgery performed to correct hallux rigidus, hallux rigidus et valgus and other painful degenerative diseases of the MTP1. Furthermore, it is a salvage procedure for failed hallux valgus surgery. High patient satisfaction and union rates have been reported in the literature with union rates ranging from 77% to 100%[1-4]. Nevertheless, nonunion of the arthrodesis has been purported as a common complication with unsatisfying results often leading to revision surgery[5,6].
A wide range of fixation methods has been published showing that biomechanically the most stable construct is a combination of a compression screw and a dorsal locking plate[2,7,8]. Commonly a dorsal plate fixation is used as it offers superior strength and sagittal plane rigidity allowing for immediate weight bearing[9,10]. In our own institution we have been using the combination of a compression screw with a dorsal locking plate for more than 10 years. The technique is similar to the technique published by Kumar et al[11] with slight variations.
The given literature about radiologic outcomes after arthrodesis of the first ray is limited. Therefore, the aim of this study was to retrospectively assess our own patient collective regarding non-union rate, degree of correction, complications, look for independent risk factors of failure and describe our own surgical technique using a compression screw and a dorsal plate while giving some insightful tips on how to avoid classical pitfalls.
This retrospective study was approved by the ethics commission board of northwest- and central-Switzerland and was conducted entirely at the authors institution: BASEC Nr 2021-00837. Patients recruited have provided written informed consent.
Out of the institution’s database every MTP1 arthrodesis that was executed between September 2011 and November 2020 was identified. The consecutive cohort consisted of 9 male patients and 62 female patients with 34 left and 38 right feet. The average age was (70 years, range 32-90). All patients underwent fusion of the MTP1 by using a compression screw and a low-profile dorsal locking plate. An anatomical, variable-angle dorsal locking plate 2.4/2.7 mm (DePuy-Synthes, Johnson&Johnson) was used. Pre and postoperatively weight bearing radiographs (anterior-posterior, oblique and lateral) were obtained. All Patients with a minimum follow-up of 3 mo and a complete radiographic data set as mentioned above were included in the study.
A single surgeon (SB) performed all surgeries. A classical medial approach is used to expose the medial capsule. A longitudinal incision is used to divide the capsule. After opening the capsule, the capsule is partially released from the metatarsal head. Afterwards the joint is dislocated and a 1.6 mm Kirschner wire is inserted centrally into the first metatarsal head. Now spherical reamers are used to prepare a convex first metatarsal head and a concentric concave proximal phalanx (P1). Afterwards 1 mL demineralized bone matrix is applied (Osteosparx, SeaSpine Carlsbad, CA 92008) into the arthrodesis gap. Now the correct position of the arthrodesis is adjusted under fluoroscopy. The sagittal position is verified using a flat tray simulating a weight-bearing situation. Once the correct position is set, the joint is temporarily fixated with a Kirschner wire inserted from medial to lateral and proximal to distal direction already defining the position of the compression crew. Now the clinical and radiologic position of the arthrodesis is checked again. The reduction is secured with a 4.3 mm cannulated screw (Qwix, Integra) inserted over the wire. Afterwards any dorsal prominences are removed allowing for a good fit of the arthrodesis plate. The plate can be provisionally fixed using olive-Kirschner wires. After assuring the correct position of the plate standard variable-angle locking screws are used. Now, the implant position and length of the screws is checked again, and the correct position of the arthrodesis is verified under fluoroscopy. Subsequently, the wound is closed in layers with non-absorbable suture material for the skin. A sterile wound dressing and a flat operative shoe are applied.
Postoperatively, full weight bearing is allowed with wearing the flat operative shoe day and night for 6 wk[12,13]. At six weeks regular shoes were permitted. Clinical-radiological follow-up takes place after 6 wk and 3 mo.
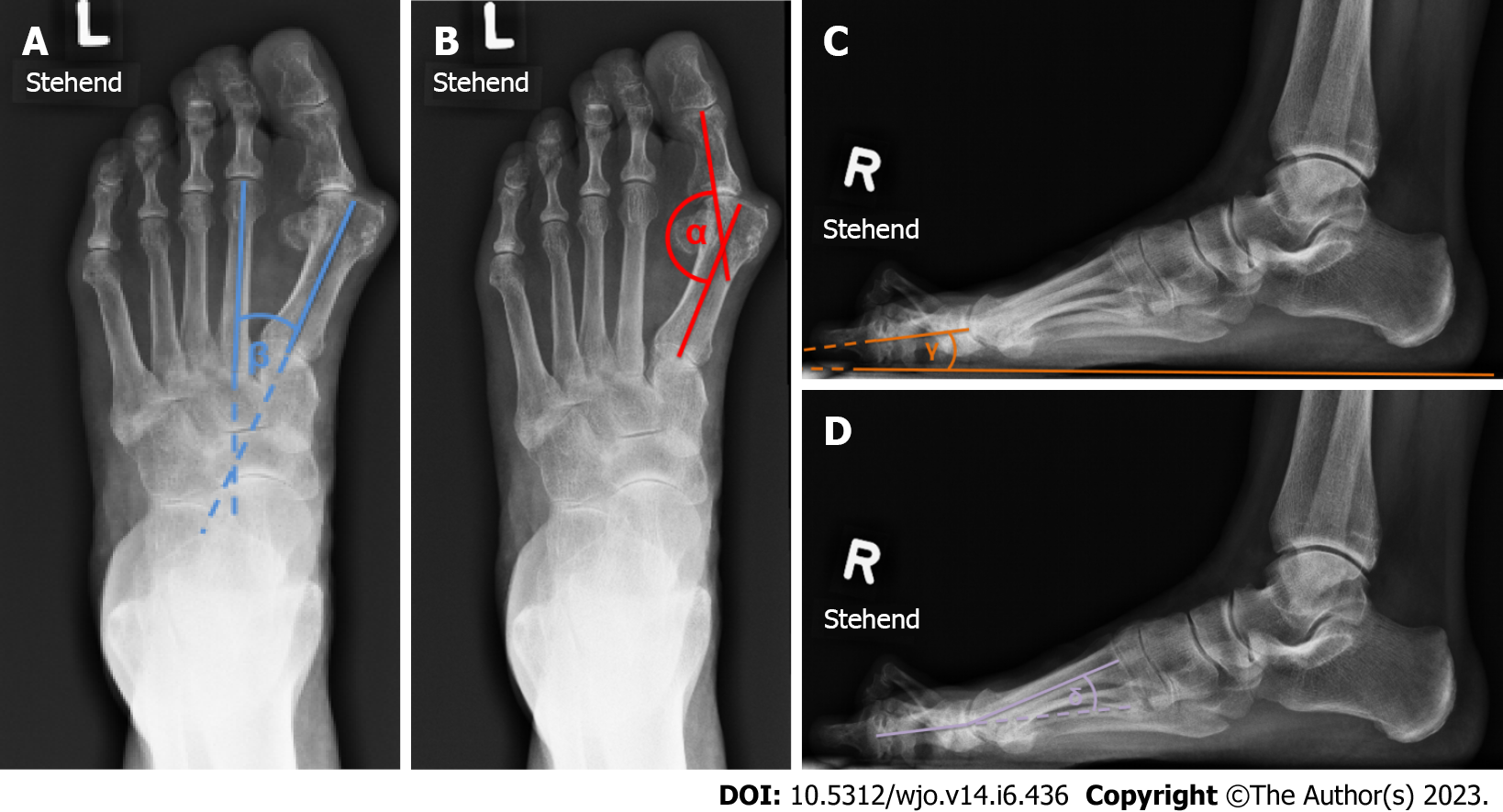
The following parameters were evaluated on pre- and postoperative conventional radiographs which are widely used and accepted as the standard of care and decision making[14]: Intermetatarsal angle (IMA), Hallux-valgus angle (HVA), dorsal extension of the P1 in relation to the floor and the angle between the Metatarsal 1 and the P1 (MT1-P1 angle) as shown in Figure 1. Measurements were always taken from recordings of the last available follow-up. All conventional radiographs were recorded during weight bearing. Imaging was analyzed in a blinded manner by two independent orthopedic surgeons on the picture archiving and communication system (PACS) using PACS measurement tools. Fusion was defined as patients being pain free at 3 mo and by vanishing of the gap within the arthrodesis in at least three cortices.
IMA: The IMA was measured using the long axis of the first and second Metatarsal. An angle of less than 9° was viewed as normal[15].
HVA: The HVA was assessed by using the long axis of the first Metatarsal in relation to the P1. A value of less than 15 was deemed physiologic[16].
Dorsal extension of P1 in relation to the floor: The Angle between the long axis of the P1 in relation to the floor was measured on lateral radiograph to assess the position of the arthrodesis.
Angle between the first MT1 and the P1 angle: The position of the P1 in relation to the MT1 was measured on a lateral standing weight bearing radiograph.
Descriptive analysis of patient characteristics and outcome parameters was performed. For continuous variables the mean and range are reported. Frequencies and percentages were used for dichotomous variables. Union rates are reported as frequencies and exact pearson-clopper 95% confidence intervals (CI) were calculated. The subgroup analyses of diabetics and smokers was done in a descriptive fashion due to the low number of observations. Statistical analyses were computed using Stata/IC 15.1 software (StataCorp LP, College Station, TX, United States).
Of 71 patients with 72 feet were included in the study with a minimum follow up of three months. There were 9 male and 62 female patients with an average age of 70.1 years (range 32-90). The body mass index averaged 26.5 kg/m2 (range 17-38). Further patient characteristics are displayed in Table 1. Out of these, 71 patients showed a fused arthrodesis (98.6%) at the latest follow-up with one patient suffering from malunion. One patient finally fused after 18 mo showing a delayed union while being asymptomatic throughout the whole period. One patient did not stick to the postop rehab protocol due to a rapidly increasing dementia leading to a P1 fracture. In consideration of the patient's underlying disease and freedom from symptoms, revision surgery was not performed. In one case the locking mechanism of the locking screws failed leading to relapse in valgus and pronation of the first toe which eventually fused in that position. In total three patients developed a symptomatic adjacent joint degeneration over time (15-37 mo). In one case the first tarsometatarsal joint (TMT I) and in two cases the interphalangeal (IP) joint was affected all requiring a TMT or IP joint arthrodesis over time. The preoperative HVA was in average 25.2 (range 14-64) with a correction down to 12 in average (range 2-27) while the preoperative IMA was 13.48 (range 4.5-24) with a postoperative correction to 9.2 in average (range 3.5-15). The preoperative MT1-P1 angle was 8.7 (range -28.05 to 55) with postoperative values of in average 16.89 (-4.05 to 34.5) which was already shown. All radiographic parameters are in detail displayed in Table 2. All patients with diabetes and smoking fused without showing signs of delayed healing or wound healing disorders. Only one patient developed a postoperative wound infection, which ultimately required a skin graft. Preoperatively the patient had a duplex ultrasound which did not show diminished perfusion. During the wound healing disorder another angiography was performed which showed a long-distance stenosis of the superficial femoral artery and the popliteal artery which was treated by balloon dilatation. Another wound healing disorder appeared that was successfully treated with oral antibiotics
| Classification | |
| Age, years (Avg, range) | 70.1 (range 32-90) |
| Gender | 9 males; 62 females |
| BMI, kg/m2 (Avg, range) | 26.5 (range 17-38) |
| Surgical side | 38 right; 34 lefts |
| Follow-up, months (Avg, range) | 3 (60-108) |
| Previous surgeries | 4 |
| Diabetes Mellitus | 8 |
| Smoker (Avg PY, range) | 13 (28, range 20-40) |
| Rheumatic disease | 12 |
| Immunosuppression | 6 |
| Preoperative (Avg, range) | Postoperative (Avg, range) | |
| Hallux-Valgus-angle | 25.21 (14-64) | 12 (2-27) |
| Intermetatarsal-angle | 13.48 (3.5-15) | 9.2 (3.5-15) |
| P1-floor | 3.33 (-38.05-18.55) | 1.23 (-15.35-18.9) |
| MT1-P1 | 8.37 (-28.05-55) | 16.89 (-4.05-34.5) |
Arthrodesis of the MTP1 is a highly successful surgery to treat degenerative diseases of the MTP1. It has already been shown that using a construct of a compression screw and dorsal locking plate offers biomechanically the most stable construct[10]. In our own cohort, union rate was 98.6% (CI: 90.3-99.6) with one nonunion and one delayed union which we counted as a union as it finally fused. One malunion appeared due to failure of the locking mechanism. This patient had a known osteoporosis and suffered over the course of time of insufficiency fractures of the ipsilateral second and third metatarsal as a sign of lowered bone density. The clear nonunion was most likely attributed to a rapidly progre
The MT1-P1 angle was used to assess the sagittal position of the first ray. In our opinion this needs to be done intraoperatively using a flat tray as mentioned above and recommended by Drittenbass et al[20] simulating a weight-bearing situation as the MT1-P1 is strongly influenced by the position of the first metatarsal which differs in flatfoot, cavo-varus or other foot deformities reflected by the wide postoperative range and has to be taken into account intraoperatively[20]. Accordingly, we observed a wide range of the MT1-P1 angle in our own cohort with an average value of 16.89 (-4.05 to 34.5). This has already been published long ago deeming an average value of 12 degrees (range 0-32) as physiologic[22,23].
Strengths of the present study are more certainly that a SB performed all surgeries, and the same implant and fixation technique were used in all cases. Limitations of this study include the short period of follow up and the lack of clinical scores to correlate radiological and clinical outcome. Future studies should particularly correlate radiological data with clinical scores to confirm their clinical relevance and superiority.
We were able to show that with our surgical technique, high union rates (98%) can be achieved using a compression screw and a dorsal variable-angle locking plate to treat degenerative diseases of the MTP1 even in diabetic and smoking patients.
Fusion of the first metatarsophalangeal joint (MTP1) is a common surgery performed to correct hallux rigidus, hallux rigidus et valgus and other painful degenerative diseases of the MTP1. High patient satisfaction and union rates have been reported in the literature with union rates ranging from 77% to 100%. In our own cohort we were also able to show high fusion rates.
Analyze our own cohort regarding union rate and radiologic outcome.
The main objective of this study as to asses our own patient collective regarding fusion rate and radiologic outcome including degree of correction.
Out of the institution’s database every MTP1 arthrodesis that was executed between September 2011 and November 2020 was identified. The consecutive cohort consisted of 9 male patients and 62 female patients with 34 left and 38 right feet. Patients were followed and pre and postoperatively weight bearing radiographs (anterior-posterior, oblique and lateral) were analyzed for fusion rate and various radiologic parameters.
Of 71 patients showed a fused arthrodesis (98.6%) at the latest follow-up with one patient suffering from malunion. One patient finally fused after 18 months showing a delayed union while being asymptomatic throughout the whole period. The preoperative Hallux-valgus angle was in average 25.2 (range 14-64) with a correction down to 12 in average (range 2-27) while the preoperative intermetatarsal angle was 13.48 (range 4.5-24) with a postoperative correction to 9.2 in average (range 3.5-15). The preoperative MT1-P1 angle was 8.7 (range -28.05 to 55) with postoperative values of in average 16.89 (-4.05 to 34.5) which was already shown.
We were able to show that with our surgical technique, high union rates (98%) can be achieved using a compression screw and a dorsal variable-angle locking plate to treat degenerative diseases of the MTP1 even in diabetic and smoking patients.
Future studies should particularly correlate radiological data with clinical scores to confirm their clinical relevance and superiority.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Switzerland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mahmoud MZ, Saudi Arabia; Ravenell RA, United States S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | DeSandis B, Pino A, Levine DS, Roberts M, Deland J, O'Malley M, Elliott A. Functional Outcomes Following First Metatarsophalangeal Arthrodesis. Foot Ankle Int. 2016;37:715-721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Buranosky DJ, Taylor DT, Sage RA, Sartori M, Patwardhan A, Phelan M, Lam AT. First metatarsophalangeal joint arthrodesis: quantitative mechanical testing of six-hole dorsal plate versus crossed screw fixation in cadaveric specimens. J Foot Ankle Surg. 2001;40:208-213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 57] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Raikin SM, Ahmad J, Pour AE, Abidi N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg Am. 2007;89:1979-1985. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Womack JW, Ishikawa SN. First metatarsophalangeal arthrodesis. Foot Ankle Clin. 2009;14:43-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Beeson P. The surgical treatment of hallux limitus/rigidus: a critical review of the literature. The Foot. 2004;14:6-22. [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Coughlin MJ. Arthrodesis of the first metatarsophalangeal joint with mini-fragment plate fixation. Orthopedics. 1990;13:1037-1044. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 158] [Cited by in F6Publishing: 131] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Curtis MJ, Myerson M, Jinnah RH, Cox QG, Alexander I. Arthrodesis of the first metatarsophalangeal joint: a biomechanical study of internal fixation techniques. Foot Ankle. 1993;14:395-399. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 94] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Molloy S, Burkhart BG, Jasper LE, Solan MC, Campbell JT, Belkoff SM. Biomechanical comparison of two fixation methods for first metatarsophalangeal joint arthrodesis. Foot Ankle Int. 2003;24:169-171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int. 2006;27:869-876. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 169] [Cited by in F6Publishing: 140] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2003;24:332-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 123] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Kumar S, Pradhan R, Rosenfeld PF. First metatarsophalangeal arthrodesis using a dorsal plate and a compression screw. Foot Ankle Int. 2010;31:797-801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Crowell A, Van JC, Meyr AJ. Early Weight-Bearing After Arthrodesis of the First Metatarsal-Phalangeal Joint: A Systematic Review of the Incidence of Non-Union. J Foot Ankle Surg. 2018;57:1200-1203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Abben KW, Sorensen MD, Waverly BJ. Immediate Weightbearing After First Metatarsophalangeal Joint Arthrodesis With Screw and Locking Plate Fixation: A Short-Term Review. J Foot Ankle Surg. 2018;57:771-775. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Heineman N, Liu G, Pacicco T, Dessouky R, Wukich DK, Chhabra A. Clinical and imaging assessment and treatment of hallux valgus. Acta Radiol. 2020;61:56-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Doty JF, Harris WT. Hallux Valgus Deformity and Treatment: A Three-Dimensional Approach. Foot Ankle Clin. 2018;23:271-280. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Fitzgerald JA. A review of long-term results of arthrodesis of the first metatarso-phalangeal joint. J Bone Joint Surg Br. 1969;51:488-493. [PubMed] [Cited in This Article: ] |
| 17. | Roukis TS. Nonunion after arthrodesis of the first metatarsal-phalangeal joint: a systematic review. J Foot Ankle Surg. 2011;50:710-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Weber C, Yao D, Schwarze M, Andersson K, Andric V, Kinkelin M, Claassen L, Stukenborg-Colsman C, Waizy H. Risk Analysis of Nonunion After First Metatarsophalangeal Joint Arthrodesis. Foot Ankle Spec. 2021;14:120-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Leaseburg JT, DeOrio JK, Shapiro SA. Radiographic correlation of hallux MP fusion position and plate angle. Foot Ankle Int. 2009;30:873-876. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Drittenbass L, Kutaish H, Chin L, Stern R, Assal M. Why and How Often Is Revision Surgery Necessary after First Metatarsophalangeal Joint Arthrodeses? A Cohort of 120 Consecutive Cases. Open J Orthop. 2021;11:221-232. [DOI] [Cited in This Article: ] |
| 21. | McKean RM, Bergin PF, Watson G, Mehta SK, Tarquinio TA. Radiographic Evaluation of Intermetatarsal Angle Correction Following First MTP Joint Arthrodesis for Severe Hallux Valgus. Foot Ankle Int. 2016;37:1183-1186. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Joseph J. Range of movement of the great toe in men. J Bone Joint Surg Br. 1954;36-B:450-457. [DOI] [Cited in This Article: ] |
| 23. | Sarrafian S, Kelikian A. Sarrafian’s Anatomy of the Foot and Ankle. Sarrafian’s Anatomy of the Foot and Ankle, 3rd ed Philadelphia, PA: Lippincott Williams & Wilkins; 2011. [Cited in This Article: ] |