Published online Mar 18, 2023. doi: 10.5312/wjo.v14.i3.103
Peer-review started: July 13, 2022
First decision: August 22, 2022
Revised: September 1, 2022
Accepted: February 21, 2023
Article in press: February 21, 2023
Published online: March 18, 2023
Since the 1990s, new insights in wrist arthroscopy have led to the introduction of numerous treatment methods. Consequently, therapeutic procedures are no longer limited to resection as more specialized repair and functional reconstruc
Core Tip: Several novel procedures with specific surgical indications have been developed over the past 15 years. More difficult and precise procedures can now be performed with fewer complications as both techniques and instrumentation improve. Debridement and resection are no longer the only therapeutic treatment available. Functional reconstruction treatments involving the repair of tissue defects and augmentation of important structures with graft material as well as more particular anatomical structure fixing procedures have been performed with established clinical benefit. This article covers current arthroscopic techniques used in clinical practice in Indonesia, some of which represent cutting-edge breakthroughs in therapeutic arthroscopy.
- Citation: Satria O, Hadinoto SA, Fathurrahman I. Advances in wrist arthroscopic surgery in Indonesia. World J Orthop 2023; 14(3): 103-112
- URL: https://www.wjgnet.com/2218-5836/full/v14/i3/103.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i3.103
The constant development of numerous treatment methods since the 1990s has triggered significant advancements in wrist arthroscopy. Due to the simultaneous development of tailored instruments adapted for small joints, most techniques used in large joint arthroscopy are either transferred or inspired from already established methods. The increase of popularity in therapeutic arthroscopy has increased the usage and role of arthroscopy in the treatment of wrist disorders including acute and elective settings. Wrist arthroscopy has become a new standard for evaluation and treatment in specific clinical disorders, such as chronic ulnar wrist pain. Similarly, in an increasing variety of clinical illnesses, such as scaphoid fractures, carpal nonunion, ganglion, and triangular fibro cartilage complex (TFCC) lesions, novel therapeutic strategies are challenging traditional surgical treatment methods, thinking, and long-term outcomes. Consequently, wrist arthroscopy could eventually reach the same level of popularity as other arthroscopy surgery.
Several novel procedures with specific surgical indications have been developed over the past 15 years. More difficult and precise procedures can now be performed with fewer complications as both techniques and instrumentation improve. Debridement and resection are no longer the only therapeutic treatment available. Functional reconstruction treatments involving the repair of tissue defects and augmentation of important structures with graft material as well as more particular anatomical structure fixing procedures have been performed with established clinical benefit. This article covered current arthroscopic techniques used in clinical practice in Indonesia on a regular basis, some of which represent cutting-edge breakthroughs in therapeutic arthroscopy.
This method is used when the accumulated debris in the joint contributes either directly or indirectly to the manifestation of symptoms. Degenerative arthritis, gout, central TFCC tear[1], Kinbock disease[2], and partial interosseous ligament tear[3] are all examples. In the partial excision of a central TFCC tear, several devices such as suction punches, motorized shavers, arthroscopic knives, and more recently radiofrequency devices can all be used. In the absence of carpal dissociation, debridement can provide clinical alleviation in partial intraosseous ligament rupture[4]. If the ulnar variance of the wrist is neutral or minus[5,6], clinical improvement should be expected after partial excision of a central TFCC rupture. Wafer procedure[7], or formal ulnar shortening[8] is frequently needed for definitive treatment in patients with ulnar positive (Figure 1A and B).
Rheumatoid arthritis and other systemic diseases affecting the wrist joint are the best candidates for this operation. Arthroscopic synovectomy can reduce surgical trauma while allowing simple access to different wrist compartments. The first series of arthroscopic synovectomy on 18 wrists of 16 patients was reported by Adolfsson and Nylander[9] in 1997, and the results showed a significant improvement in pain intensity and range of motion in all patients. At a mean follow-up of 7.9 years, Lee et al[10] revealed the long-term results of arthroscopic synovectomy in 49 subjects with 56 wrists. The mean Mayo wrist score increased from 48 to 76; the mean of wrist pain calculated using visual analogue score reduced from 6.3 to 1.7. Synovitis was successfully managed in 42 wrists (75%) but recurred in the remaining 14 wrists at the final follow-up[10] (Figure 1C).
Ganglionectomy is better described as marsupialization of the ganglion because the ganglion cyst is not anatomically removed. This method is based on the idea of eliminating the “check valve” effect by producing a capsular defect at the stalk section of the ganglion cyst, where it communicates with the wrist joint, allowing the ganglion to drain, diminish, and resolve spontaneously. The approach for the usual dorsal wrist ganglion originating proximal to the scapholunate joint was first published by Osterman[11] in 1995; 6R was the viewing portal. To resect a 1-cm defect in the dorsal capsule, a full-radius resector can be introduced via the 3-4 portal. The goal of this process is to induce a flood of mucinous fluid drain into the joint, which allow the ganglion to entirely vanish outwardly. All 18 cases in the Osterman series had full resection and no recurrence (Figure 1D and E).
In 2 cases of significant post-traumatic capsular fibrosis and stiff wrist[12], Verhellen and Bain[12] used combined volar and dorsal portals to accomplish arthroscopic release. Except for the ulno-carpal ligament complex and the volar radio-ulnar ligament, all volar capsular ligaments were entirely separated with a shaver, RF probe, or arthroscopic knife and then gently manipulated under anesthesia (Figure 1F).
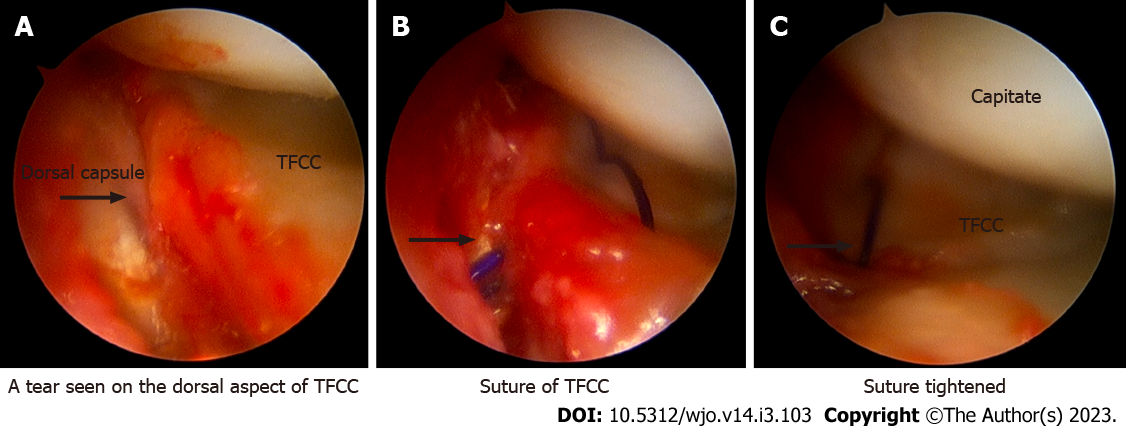
The TFCC is prone to damage because it is subjected to significant axial loading and shear stresses[13,14]. Palmer[15] demonstrated and classified tears concerning the TFCC in 1989. This laid the foundation for current ulnar-sided wrist pain diagnosis and treatment. Thiru et al[16] and Bednar et al[17] found that the outside 10%-40% of the articular disc was highly perfused, implying that these wounded areas could heal if they were repaired. Consequently, there has been a lot of effort directed to preserve and repair peripheral TFCC lesions. In 1991, Hermansdorfer and Kleinman[18] reported that open TFCC repair produced good results, with 8 of 11 patients able to go back to regular activities. Using open repairs, Cooney et al[19] reported 26 good to excellent results in 33 operated wrists. With the introduction of wrist arthroscopy, surgeons have been able to duplicate, if not exceed, the results of open repairs[20-24]. The majority of research focused on palmar 1B tear healing, with types 1C and 1D tears reported less frequently. The inside-out and outside-in approaches to arthroscopic repair have been advocated. Simple hypodermic needles[25], epidural Tuohy needles, meniscal needles, and zone-specific repair kits[26] were among the instruments used.
In terms of clinical outcomes, the open group had a higher rate of postoperative superficial ulnar nerve discomfort and reoperation. There has been no recent study comparing the outcomes of various arthroscopic repair procedures. To promote healing and induce fibrovascular in growth, it is critical to debride the rim of the torn ligament down to healthy vascular tissue in all TFCC mending procedures. To ensure healing, the torn peripheral rim of the TFCC is positioned against the fovea or the capsular tissue (Figure 2).
The optimum surgical reconstruction for painful distal radioulnar joint (DRUJ) instability induced by TFCC disruption has been a source of debate until recently. The dorsal and palmar of radio-ulnar marginal ligaments, which are linked during various stages of prono-supination, are now recognized as the most important stabilizers of the DRUJ. During forearm rotational movement, damage to one or both of these ligaments resulted in pain and instability. Adams et al[27] and Adams[28] conducted a thorough biomechanical analysis and advocated anatomical repair of the distal radio-ulnar ligaments as the optimal treatment option for this complex problem. The authors found good results from open reconstruction with graft from palmaris longus tendon in 12 patients with post-traumatic DRUJ instability with 1-4 years of follow-up evaluation[28].
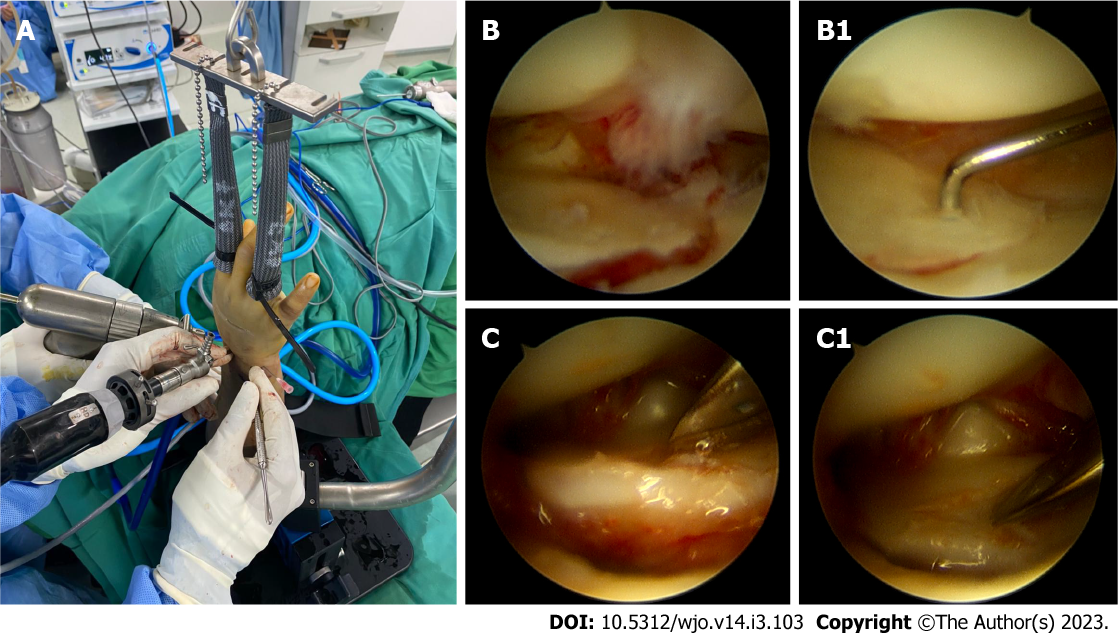
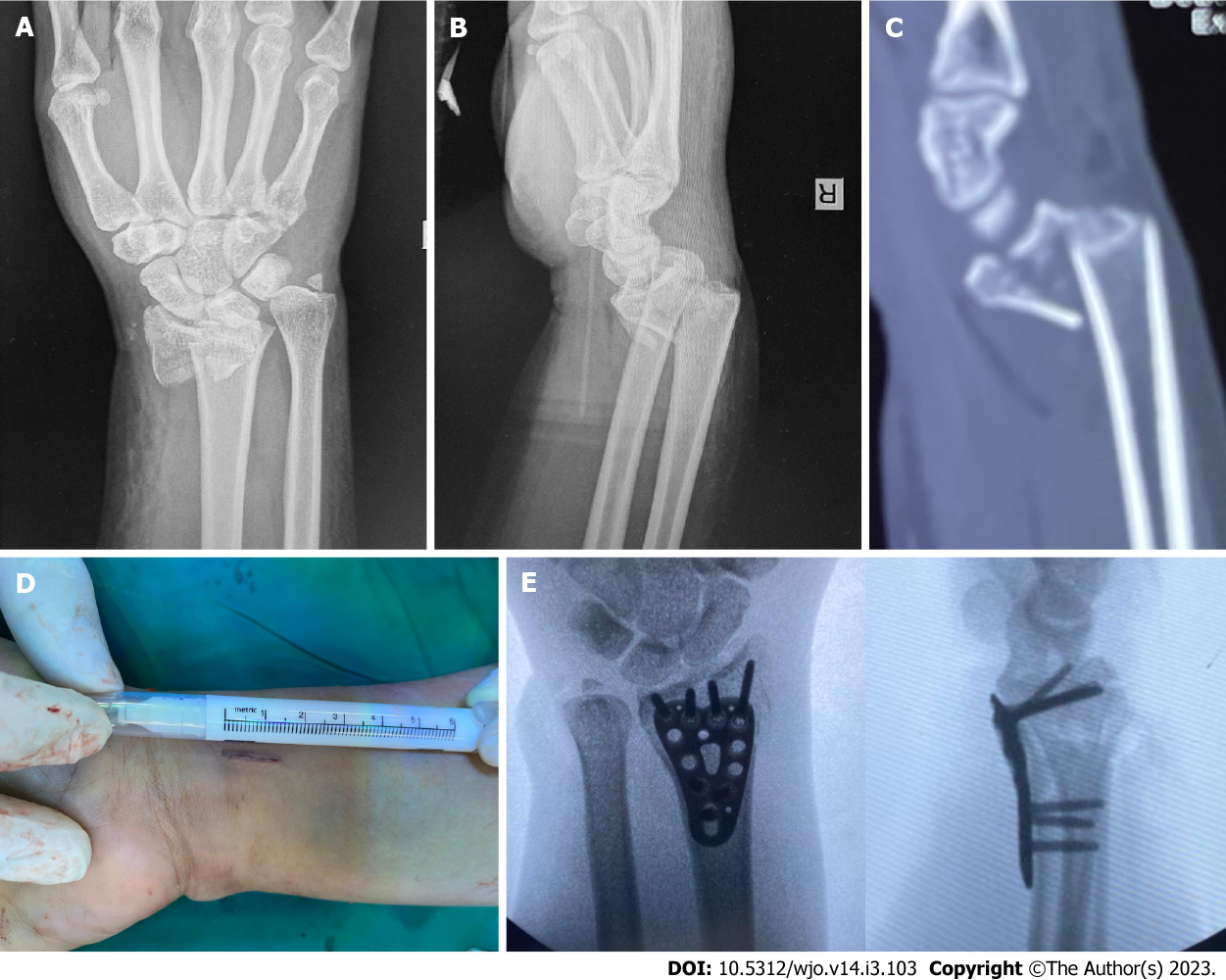
For proper reduction and fixing, arthroscopic-assisted reduction and internal fixation is still necessary. Furthermore, arthroscopy can be used to treat related soft tissue injuries in the same setting, with success rates ranging from 40%-75% in distal radius fracture and up to 50% in scaphoid fracture. Intra-articular fracture with comminution and displacement is the best indication for arthroscopic intervention in distal radius fractures, and the target of articular reduction is within 2 mm of step or gap[29]. Percutaneous access to and assessment of depressed intra-articular fragments is notoriously difficult. In terms of measuring joint surface reduction, arthroscopy has been proven to be superior to intraoperative fluoroscopy and plain radiograph[30]. When compared to the conventional reduction method with fluoroscopy alone, patients that underwent arthroscopically-assisted reduction of intra-articular distal radius fractures had better clinical outcomes, improved radiologic variable regarding displacement and angulation, and greater range of motion[31,32].
Through arthroscopic portals, the misplaced fragments can be attacked, elevated, and reduced using a fine bone or a probe under direct visualization. When volar plating is being considered, both dorsal and volar ports can be utilized. While the articular reduction is monitored and regulated arthroscopically, the fragments can also be elevated with an osteotome or a bone spike injected through the metaphyseal region. Subchondral screws or pins are used to repair the decreased fracture. Dry arthroscopy has grown in favor in recent years, especially for fracture reduction and fixation because it allows for easier fracture manipulation and reduces the possibility of fluid extravasation, which can lead to compartment syndrome[33]. Arthroscopy can also detect and treat unnoticed soft tissue and cartilage injuries.
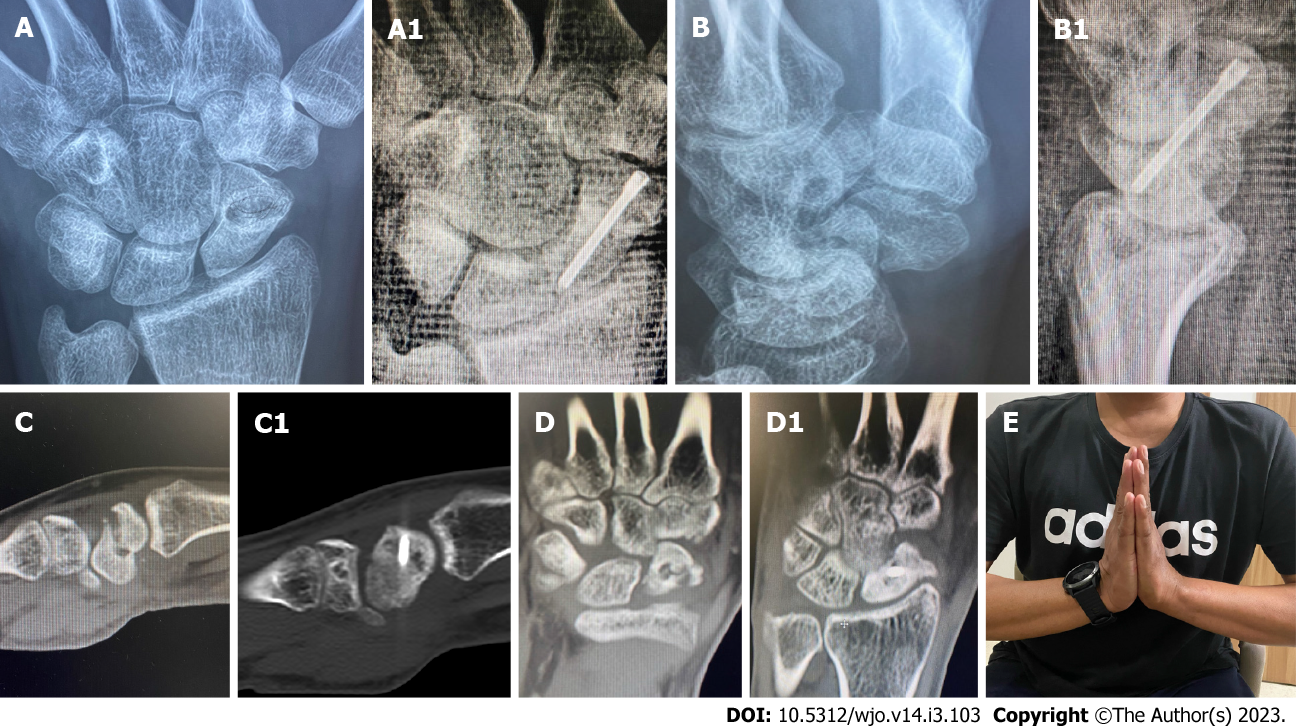
In the treatment of acute scaphoid fractures, percutaneous screw fixation is gaining popularity. The majority of series had a high rate of union and a positive functional outcome. Arthroscopy can become a useful adjuvant to a minimally invasive method for treating tricky cases, such as misplaced fractures, fracture comminution, and delayed presentation, and can often eliminate the need for open reduction. It causes minimum vascular and soft tissue disruption, promoting fracture union. In most cases, including proximal third fractures, we undertake reduction and percutaneous fixation using the volar route. In many series, the volar approach not only has a higher union rate and lower complication rate but also provides safer and easier screw entry, maintains and corrects fracture deformity in the extended wrist, does not disrupt the load bearing proximal scaphoid cartilage, has minimum hardware issues, and gives no harm to the tendons and dorsal wrist structures, which have been expressed in dorsal approach surgeries[34] (Figures 3 and 4).
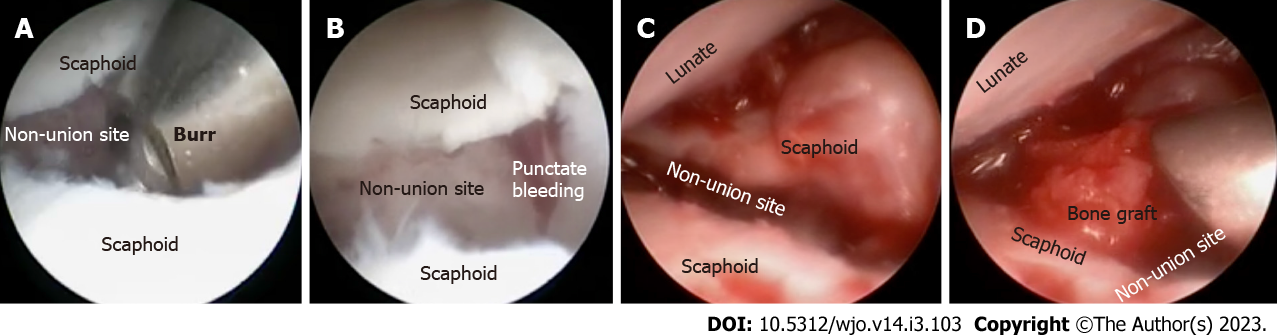
The complete intra-articular position of scaphoid nonunion favor an arthroscopic approach for diagnostic and therapeutic interventions while preserving as much blood supply and ligamentous architecture as possible, which favors union and functional restoration.
Between 2019 and 2021, we used arthroscopic bone grafting to treat osseous abnormalities in 6 cases of scaphoid nonunion. In all situations, we obtained union within 4 mo on average. Minimal disruption to complex ligamentous structures, maximum preservation of carpal bone vascularity, holistic assessment of wrist joint allowed prior to surgical intervention, minimum scar and pain, unnecessary tourniquet, stitch-less surgery, and faster healing process were all potential benefits of this approach (Figures 5-7).
Radial styloidectomy for post-traumatic arthritis secondary to scaphoid nonunion and rheumatoid or carpal instability, as well as the Wafer operation for ulnar impaction syndrome, are two of the most common indications for osseous resection plasty. The advantage of arthroscopic radial styloidectomy is that it allows for improved vision and conserves the radio-scapho-capitate ligament that acts as a crucial stabilizing structure of the wrist.
Furthermore, the Wafer method is a well-established therapy for the ulnar impaction syndrome. A completely perforated TFCC is required for an arthroscopic operation, which is usually only possible for degenerative TFCC tears of Palmer stage 2C or higher. In cases of distal radius malunion, osteotomy may also be used for reconstruction. A challenging intra-articular distal radius malunion can be restored using osteotomy assisted by arthroscopy in conjunction with a three-dimensional-printed surgical guide (Figure 8).
When surgeons began debating whether meniscal surgery of the knee could be done arthroscopically 40 years ago, the phrase “open meniscectomy” was likely only used in the dictionary. If the result can be shown to be equivalent or superior to open surgery, then minimally invasive arthroscopic surgery would be the optimum and preferred therapy. Because it has only been in development since 1986, wrist arthroscopy will still benefit from improvements. In fact, we learned from the literature that most traditional open wrist surgery has been attempted arthroscopically with varying degrees of success over the last 15 years. While diagnostic arthroscopy has established itself as the gold standard, most novel therapeutic studies had small numbers of clinical subjects and insufficient controlled randomized prospective study methods and lacked long-term evaluation. Well-designed clinical trials confirm the therapeutic significance in diverse wrist ailments. Wrist arthroscopy as an office diagnostic technique may become a reality in the future, with a considerably broader clinical applicability. Future advancements will most likely be restricted only by surgeons’ imaginations and skill. Nonetheless, further controlled randomized prospective studies are needed to determine the genuine efficacy of each arthroscopy treatment approach in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: AlSuwayeh FM, Saudi Arabia; Saracco M, Italy S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | Osterman AL. Arthroscopic debridement of triangular fibrocartilage complex tears. Arthroscopy. 1990;6:120-124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 174] [Cited by in F6Publishing: 139] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Watanabe K, Nakamura R, Imaeda T. Arthroscopic assessment of Kienböck’s disease. Arthroscopy. 1995;11:257-262. [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg Am. 1996;21:412-417. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 108] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am. 1997;22:344-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 151] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Husby T, Haugstvedt JR. Long-term results after arthroscopic resection of lesions of the triangular fibrocartilage complex. Scand J Plast Reconstr Surg Hand Surg. 2001;35:79-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Westkaemper JG, Mitsionis G, Giannakopoulos PN, Sotereanos DG. Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy. 1998;14:479-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 85] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Wnorowski DC, Palmer AK, Werner FW, Fortino MD. Anatomic and biomechanical analysis of the arthroscopic wafer procedure. Arthroscopy. 1992;8:204-212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 67] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Hulsizer D, Weiss AP, Akelman E. Ulna-shortening osteotomy after failed arthroscopic debridement of the triangular fibrocartilage complex. J Hand Surg Am. 1997;22:694-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 98] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Adolfsson L, Frisén M. Arthroscopic synovectomy of the rheumatoid wrist. A 3.8 year follow-up. J Hand Surg Br. 1997;22:711-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 43] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Lee HI, Lee KH, Koh KH, Park MJ. Long-term results of arthroscopic wrist synovectomy in rheumatoid arthritis. J Hand Surg Am. 2014;39:1295-1300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Osterman AL, Raphael J. Arthroscopic resection of dorsal ganglion of the wrist. Hand Clin. 1995;11:7-12. [PubMed] [Cited in This Article: ] |
| 12. | Verhellen R, Bain GI. Arthroscopic capsular release for contracture of the wrist: a new technique. Arthroscopy. 2000;16:106-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Palmer AK, Werner FW, Glisson RR, Murphy DJ. Partial excision of the triangular fibrocartilage complex. J Hand Surg Am. 1988;13:391-394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 87] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Adams BD, Holley KA. Strains in the articular disk of the triangular fibrocartilage complex: a biomechanical study. J Hand Surg Am. 1993;18:919-925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 71] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594-606. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 848] [Cited by in F6Publishing: 642] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 16. | Thiru RG, Ferlic DC, Clayton ML, McClure DC. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg Am. 1986;11:258-263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 148] [Cited by in F6Publishing: 115] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg Am. 1991;16:1101-1105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 162] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am. 1991;16:340-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 219] [Cited by in F6Publishing: 176] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. J Hand Surg Am. 1994;19:143-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 224] [Cited by in F6Publishing: 191] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 20. | Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy. 1996;12:588-597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 81] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Corso SJ, Savoie FH, Geissler WB, Whipple TL, Jiminez W, Jenkins N. Arthroscopic repair of peripheral avulsions of the triangular fibrocartilage complex of the wrist: a multicenter study. Arthroscopy. 1997;13:78-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 169] [Cited by in F6Publishing: 166] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg Am. 1997;22:57-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 133] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 23. | Haugstvedt JR, Husby T. Results of repair of peripheral tears in the triangular fibrocartilage complex using an arthroscopic suture technique. Scand J Plast Reconstr Surg Hand Surg. 1999;33:439-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Shih JT, Lee HM, Tan CM. Early isolated triangular fibrocartilage complex tears: management by arthroscopic repair. J Trauma. 2002;53:922-927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 53] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Mahajan RH, Kim SJ, Song DH, Kang YH, Park KY. Arthroscopic repair of the triangular fibrocartilage complex using a hypodermic needle: a technical note. J Orthop Surg (Hong Kong). 2009;17:231-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | de Araujo W, Poehling GG, Kuzma GR. New Tuohy needle technique for triangular fibrocartilage complex repair: preliminary studies. Arthroscopy. 1996;12:699-703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Adams BD, Samani JE, Holley KA. Triangular fibrocartilage injury: a laboratory model. J Hand Surg Am. 1996;21:189-193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Adams BD. Anatomic Reconstruction of the Distal Radioulnar Ligaments for DRUJ Instability. Tech Hand Up Extrem Surg. 2000;4:154-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-659. [PubMed] [Cited in This Article: ] |
| 30. | Edwards CC 2nd, Haraszti CJ, McGillivary GR, Gutow AP. Intra-articular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am. 2001;26:1036-1041. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Ruch DS, Vallee J, Poehling GG, Smith BP, Kuzma GR. Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy. 2004;20:225-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 32. | Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999;81:1093-1110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 117] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 33. | del Piñal F. Dry arthroscopy and its applications. Hand Clin. 2011;27:335-345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Bushnell BD, McWilliams AD, Messer TM. Complications in dorsal percutaneous cannulated screw fixation of nondisplaced scaphoid waist fractures. J Hand Surg Am. 2007;32:827-833. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |