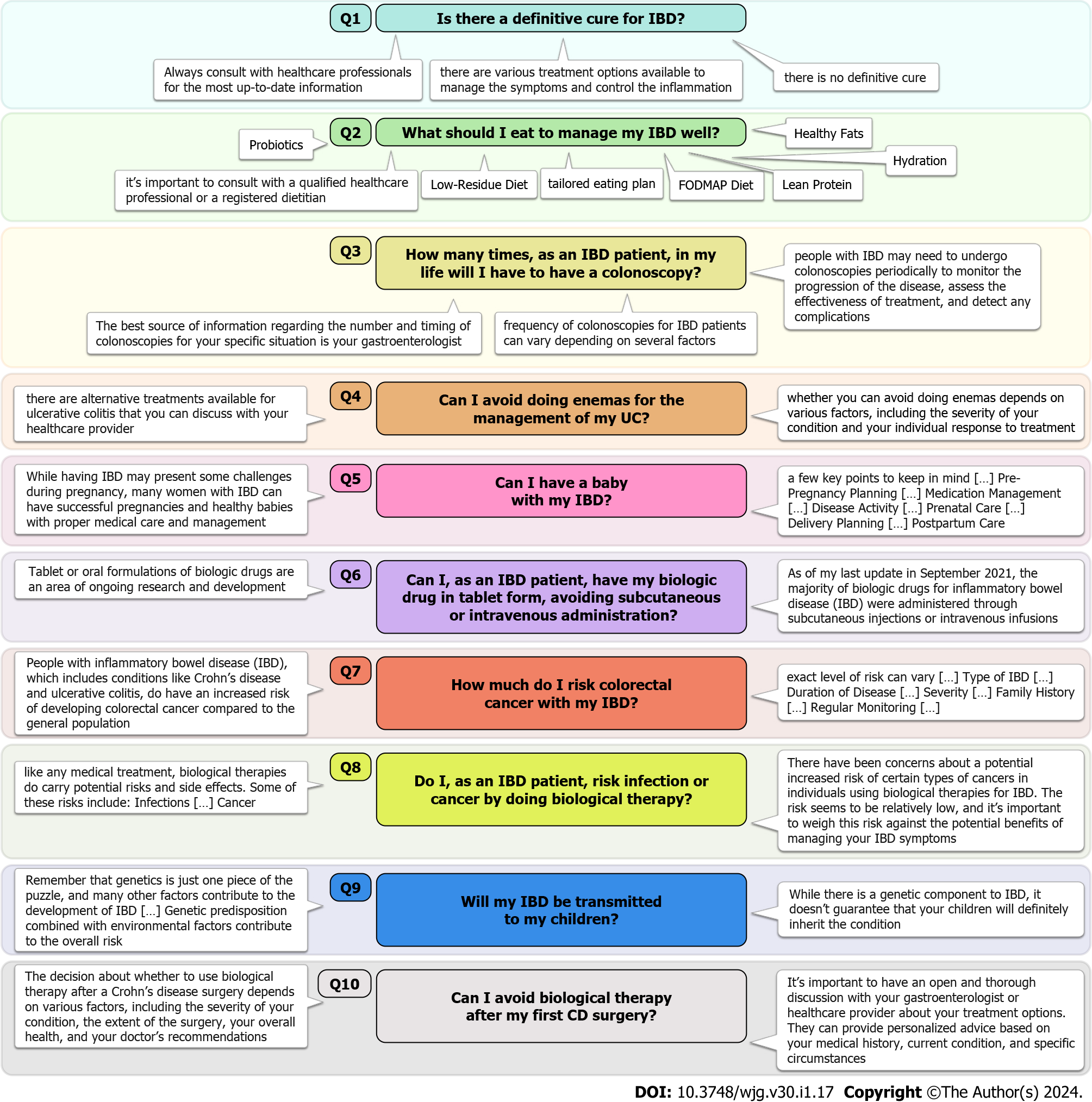
| Q1 | As of my last knowledge update in September 2021, there is no definitive cure for IBD, which is a group of chronic inflammatory conditions that primarily affect the digestive tract. The two main types of IBD are CD and UC. While there is no cure, there are various treatment options available to manage the symptoms and control the inflammation associated with IBD. These treatments include medications, lifestyle changes, dietary modifications, and in some cases, surgical interventions. The goal of treatment is to induce and maintain remission, improve quality of life, and prevent complications. It’s important to note that research and medical advancements are ongoing, so I recommend consulting with a healthcare professional or checking more recent sources for the latest information on IBD treatment options and potential developments | As of my last knowledge update in September 2021, there is still no definitive cure for IBD. IBD is a complex and chronic condition that includes conditions like CD and UC, which involve inflammation of the digestive tract. While there have been significant advancements in understanding and treating IBD, no treatment or intervention has been proven to completely eliminate the underlying causes of the disease. Current treatments aim to manage symptoms, reduce inflammation, and promote remission, but they do not offer a guaranteed cure. It’s important to stay updated with the latest medical research and consult with healthcare professionals for the most accurate and current information on IBD treatments and potential breakthroughs | As of my last update in September 2021, there is still no definitive cure for IBD, which includes conditions like CD and UC. IBD is a complex and chronic condition characterized by inflammation of the digestive tract. While there have been significant advancements in understanding and managing IBD, a true cure that eliminates the underlying causes of the disease has not been discovered. Current treatments focus on managing symptoms, reducing inflammation, and achieving periods of remission, but they do not provide a permanent cure. Research and medical advancements are ongoing, so it’s important to stay informed about the latest developments in IBD treatments. Always consult with healthcare professionals for the most up-to-date information and advice regarding IBD management and potential breakthroughs |
| Q2 | I am not a doctor, but I can offer some general dietary guidelines that are commonly recommended for managing IBD. It’s important to consult with a qualified healthcare professional or a registered dietitian who specializes in IBD for personalized advice tailored to your specific condition and needs. Here are some general tips: (1) Low-residue diet: This involves consuming foods that are easy to digest and produce less waste. It may include well-cooked and peeled fruits and vegetables, refined grains, lean protein sources, and well-cooked eggs; (2) FODMAP diet: This diet reduces intake of certain types of carbohydrates that can be poorly absorbed in the small intestine, leading to symptoms in some individuals. It may be helpful for managing symptoms such as gas, bloating, and diarrhea; (3) Anti-inflammatory foods: Incorporate foods rich in anti-inflammatory properties, such as fatty fish (like salmon and mackerel), walnuts, flaxseeds, chia seeds, turmeric, ginger, and leafy greens; (4) Lean protein: Choose lean sources of protein, such as skinless poultry, fish, eggs, tofu, and tempeh. Protein is important for tissue repair and immune function; (5) Good fats: Consume healthy fats from sources like olive oil, avocados, nuts, and seeds. These fats can help reduce inflammation; (6) Hydration: Drink plenty of fluids to stay hydrated, as diarrhea and other symptoms can lead to dehydration. Water, herbal teas, and clear broths are good options; (7) Avoid trigger foods: Identify and avoid foods that trigger your symptoms. Common triggers vary from person to person but may include dairy products, spicy foods, caffeine, and alcohol; (8) Small, frequent meals: Eating smaller, more frequent meals throughout the day can help ease the digestive process and prevent overwhelming your system; (9) Probiotics: Some people with IBD find that probiotics can help regulate gut flora and improve symptoms. Consult your healthcare provider before adding probiotics to your routine; (10) Monitor fiber intake: While fiber is generally beneficial for digestion, too much insoluble fiber can worsen symptoms for some individuals. Gradually introduce soluble fiber sources like oats, bananas, and cooked vegetables; (11) Dairy alternatives: If you’re lactose intolerant or sensitive to dairy, consider trying lactose-free or plant-based dairy alternatives like almond milk, coconut milk, or lactose-free yogurt; and (12) Supplements: Some people with IBD may need supplements to address nutrient deficiencies. Consult your healthcare provider before taking any supplements. Remember, what works for one person may not work for another. Keep a food diary to track your symptoms and identify patterns, and work closely with a healthcare professional to develop a personalized dietary plan that suits your specific condition and needs | Managing IBD requires a personalized approach that considers your specific symptoms, triggers, and nutritional needs. While I can’t provide medical advice, I can offer some general dietary tips that may help you manage your condition better. However, it’s crucial to work closely with a healthcare professional or registered dietitian who specializes in IBD to develop a tailored eating plan. Here are some dietary principles to consider: (1) Low-residue diet: This diet focuses on consuming foods that are easily digestible and produce minimal waste. It may include well-cooked fruits and vegetables, refined grains, lean proteins, and limited high-fiber foods; (2) FODMAP diet: Some individuals with IBD find relief by following a low-FODMAP diet, which limits certain types of carbohydrates that can trigger digestive symptoms; (3) Anti-inflammatory foods: Include foods rich in anti-inflammatory properties, such as fatty fish (salmon, mackerel), walnuts, flaxseeds, turmeric, ginger, and leafy greens; (4) Lean protein: Opt for lean sources of protein like skinless poultry, fish, eggs, tofu, and tempeh. Protein is essential for healing and immune function; (5) Healthy fats: Incorporate healthy fats from sources like olive oil, avocados, nuts, and seeds. These fats can help reduce inflammation; (6) Hydration: Stay well-hydrated to prevent dehydration, which can worsen symptoms. Water, herbal teas, and clear broths are good choices; (7) Individual triggers: Identify and avoid specific trigger foods that exacerbate your symptoms. These triggers can vary widely from person to person; (8) Small, frequent meals: Eating smaller meals throughout the day can ease digestion and prevent overwhelming your digestive system; (9) Probiotics: Some individuals with IBD find that probiotics help balance gut bacteria and improve symptoms. Consult your healthcare provider before using probiotics; (10) Monitor fiber intake: Gradually introduce soluble fiber sources like oats, bananas, and cooked vegetables. Monitor your tolerance and adjust accordingly; (11) Dairy alternatives: If you’re lactose intolerant or sensitive to dairy, consider lactose-free or plant-based alternatives like almond milk or coconut yogurt; (12) Supplements: Nutrient deficiencies are common in IBD. Discuss with your healthcare provider whether you need supplements to address any deficiencies; (13) Listen to your body: Pay attention to how your body responds to different foods. Keep a food diary to track symptoms and identify patterns; (14) Avoid rapid changes: Make dietary changes gradually to give your body time to adapt and monitor how each change affects you; and (15) Collaborate with professionals: Work closely with a healthcare provider and a registered dietitian who specializes in IBD to create a personalized eating plan that meets your nutritional needs and helps manage your symptoms. Remember that IBD is a complex condition, and what works for one person might not work for another. It’s important to develop an individualized approach that considers your unique situation and preferences | Managing IBD through diet can be complex and highly individualized, as the condition varies from person to person. It’s important to work closely with a healthcare provider or a registered dietitian who specializes in IBD to create a personalized eating plan tailored to your specific needs and symptoms. That being said, here are some general dietary guidelines that you might find helpful: (1) Low-residue diet: This type of diet focuses on consuming foods that are easy to digest and produce minimal waste. It may include well-cooked vegetables, lean protein sources, refined grains, and tender fruits; (2) FODMAP diet: Some individuals with IBD may benefit from a low-FODMAP diet, which limits certain types of carbohydrates that can trigger digestive symptoms. It’s important to work with a healthcare professional to properly implement this diet; (3) Anti-inflammatory foods: Incorporate foods with anti-inflammatory properties, such as fatty fish (salmon, mackerel), nuts, seeds, turmeric, ginger, and leafy greens; (4) Lean protein: Choose lean sources of protein like skinless poultry, fish, eggs, tofu, and tempeh. Protein is essential for healing and immune function; (5) Healthy fats: Include healthy fats from sources like olive oil, avocados, nuts, and seeds. These fats can help reduce inflammation; (6) Hydration: Drink plenty of fluids to prevent dehydration, which can worsen symptoms. Water, herbal teas, and clear broths are good options; (7) Individual triggers: Identify and avoid foods that trigger your symptoms. Common triggers include dairy products, spicy foods, caffeine, and alcohol; (8) Small, frequent meals: Eating smaller meals throughout the day can help ease digestion and prevent overwhelming your digestive system; (9) Probiotics: Some individuals with IBD find that probiotics help balance gut bacteria and improve symptoms. Consult your healthcare provider before using probiotics; (10) Monitor fiber intake: Gradually introduce soluble fiber sources like oats, bananas, and well-cooked vegetables. Monitor how fiber affects your symptoms and adjust as needed; (11) Dairy alternatives: If you’re lactose intolerant or sensitive to dairy, consider lactose-free or plant-based alternatives like almond milk or coconut yogurt; (12) Supplements: Nutrient deficiencies are common in IBD. Work with your healthcare provider to determine if you need supplements to address any deficiencies; (13) Listen to your body: Pay attention to how your body responds to different foods. Keep a food diary to track symptoms and identify patterns; and (14) Collaborate with professionals: Your healthcare provider and a registered dietitian experienced in IBD can help you create a personalized eating plan that considers your individual needs and goals. Remember, managing IBD involves ongoing experimentation to find what works best for you. It’s not uncommon for dietary needs to change over time, so staying in close communication with your healthcare team is crucial |
| Q3 | I am not a doctor, but I can provide you with some general information about colonoscopies for IBD. The frequency of colonoscopies for IBD patients can vary depending on several factors, including the type of IBD (CD or UC), the severity of the condition, your response to treatment, and your doctor’s recommendations. In general, people with IBD may need to undergo colonoscopies periodically to monitor the progression of the disease, assess the effectiveness of treatment, and detect any complications. Early detection and management of inflammation are important to prevent further damage to the digestive tract. It’s best to discuss the recommended frequency of colonoscopies with your gastroenterologist, as they can provide personalized guidance based on your specific condition and medical history. They will take into account factors such as your symptoms, disease activity, and overall health to determine the appropriate timing and frequency of colonoscopies for you | The number of colonoscopies a person with IBD may need during their lifetime can vary widely based on individual factors. These factors include the type of IBD (CD or UC), the severity of the disease, how well the disease responds to treatment, and the presence of any complications. Generally, individuals with IBD may have colonoscopies at various points in their lives: (1) Diagnosis: Colonoscopy is often used to diagnose IBD. If you are newly diagnosed, you might have had at least one colonoscopy for diagnostic purposes; (2) Monitoring disease activity: Depending on the severity and type of IBD, your doctor may recommend regular colonoscopies to monitor disease activity and assess the effectiveness of treatment. This could range from once a year to every few years; (3) Flares or symptoms: During periods of disease flares or if new symptoms develop, your doctor might recommend a colonoscopy to assess the current state of your digestive tract; (4) Surveillance: In some cases, individuals with long-standing UC may need regular colonoscopies to monitor for the development of dysplasia (abnormal cell changes that can lead to cancer). This is less common in CD; (5) Preventive measures: If you have a family history of colorectal cancer or other risk factors, your doctor might recommend more frequent colonoscopies as a preventive measure; and (6) Post-surgery: After certain surgeries for IBD, follow-up colonoscopies might be performed to assess healing and the overall condition of the intestine. It’s important to note that medical recommendations can change over time as new research and guidelines emerge. Your healthcare provider will create a personalized plan based on your specific circumstances and the most up-to-date medical knowledge. Regular communication with your gastroenterologist is crucial to determining the appropriate frequency of colonoscopies for your situation | The number of colonoscopies you’ll need as an individual with IBD can vary greatly depending on multiple factors. These factors include the type of IBD (CD or UC), the severity of your condition, your response to treatment, your overall health, and any complications that may arise. It’s important to understand that there is no fixed number of colonoscopies that applies to all IBD patients. The frequency and necessity of colonoscopies will be determined by your healthcare provider based on your specific situation. Here are some general guidelines: (1) Diagnosis: You will likely have at least one colonoscopy for diagnostic purposes when your IBD is first diagnosed; (2) Disease monitoring: Depending on the severity of your IBD and how well it responds to treatment, your doctor may recommend periodic colonoscopies to monitor disease activity and assess the condition of your intestines. This could range from once every year or two to less frequently; (3) Flares or symptoms: If you experience a flare-up of symptoms or new symptoms emerge, your doctor might recommend a colonoscopy to evaluate the extent of inflammation and identify any issues; (4) Long-term management: If your IBD is well controlled, the frequency of colonoscopies might decrease over time. However, your doctor will still periodically assess whether colonoscopies are necessary; (5) Complications or surgery: If you experience complications related to IBD or if you undergo surgery, you may need additional colonoscopies to monitor healing and overall intestinal health; and (6) Individualized care: Your doctor will create an individualized care plan that takes into account your specific medical history, disease progression, and treatment response. This plan will determine the frequency of colonoscopies you’ll need throughout your life. The best source of information regarding the number and timing of colonoscopies for your specific situation is your gastroenterologist. They will guide you based on the latest medical guidelines and your personal health profile. Regular communication with your healthcare provider is crucial to managing your IBD effectively and making informed decisions about your medical care |
| Q4 | I am not a doctor, but I can offer you some general information. The management of UC typically involves a combination of medications, lifestyle changes, and sometimes medical procedures. Enemas may be recommended by a healthcare professional as part of the treatment plan, but whether you can avoid doing enemas depends on various factors, including the severity of your condition and your individual response to treatment. It’s important to discuss your concerns and preferences with your healthcare provider | Whether you can avoid using enemas for the management of your UC depends on several factors, including the severity of your condition, your response to other treatments, and your doctor’s recommendations. Enemas are one of the treatment options used to deliver medications directly to the inflamed areas of the colon in order to reduce inflammation and manage symptoms. However, there are alternative treatments available for UC that you can discuss with your healthcare provider. These may include: (1) Oral medications: Depending on the severity of your condition, your doctor may prescribe oral medications such as aminosalicylates, corticosteroids, immunomodulators, or biologics. These medications can help reduce inflammation and manage symptoms without the need for enemas; (2) Suppositories: If you are uncomfortable with enemas, your doctor might recommend using rectal suppositories as an alternative. These medications work similarly to enemas but are inserted into the rectum; (3) Lifestyle modifications: Making certain changes to your diet and lifestyle can also help manage UC symptoms. This includes avoiding trigger foods, staying hydrated, managing stress, and getting regular exercise; and (4) Surgery: In more severe cases of UC that do not respond well to other treatments, surgery may be considered. Surgery can involve removing the affected portion of the colon and may offer long-term relief from symptoms. It’s important to have an open and honest discussion with your healthcare provider about your preferences, concerns, and treatment options. They can help tailor a treatment plan that aligns with your needs and goals while effectively managing your UC symptoms. Remember that self-management decisions should be made in consultation with your healthcare team, as they have the expertise to guide you toward the best treatment approach for your individual case | Yes, in some cases, it might be possible to avoid using enemas for the management of UC, depending on the severity of your condition, your response to other treatments, and your doctor’s recommendations. Enemas are one way to deliver medications directly to the inflamed areas of the colon, but there are alternative treatments available that might be suitable for you. It’s important to work closely with your healthcare provider to determine the best treatment plan for your specific situation. Here are some alternatives to enemas for managing UC: (1) Oral medications: Your doctor might prescribe oral medications such as aminosalicylates, corticosteroids, immunomodulators, or biologics to reduce inflammation and manage symptoms; (2) Rectal suppositories: If you’re uncomfortable with enemas, your doctor might recommend using rectal suppositories. These medications are inserted into the rectum and can be effective in treating inflammation in the lower part of the colon; (3) Lifestyle modifications: Making dietary and lifestyle changes can help manage UC symptoms. Avoiding trigger foods, staying hydrated, managing stress, and getting regular exercise can contribute to symptom relief; (4) Topical creams or foams: Some topical creams or foams containing corticosteroids can be used to treat inflammation in the rectum and lower colon; (5) Biologic injections: Biologic medications can be administered through injections or infusions, and they target specific parts of the immune system to reduce inflammation; and (6) Surgery: In severe cases where other treatments are not effective, surgery might be considered to remove the affected part of the colon. This can offer long-term relief from symptoms, but it’s typically considered when other options have been exhausted. Ultimately, the decision to avoid enemas and explore alternative treatments should be made in consultation with your healthcare provider. They will take into account your medical history, the severity of your condition, and your preferences to help you create a treatment plan that is both effective and manageable for you |
| Q5 | IBD refers to a group of chronic inflammatory conditions that affect the gastrointestinal tract. The two main types of IBD are CD and UC. These conditions can cause symptoms such as abdominal pain, diarrhea, fatigue, and weight loss. If you have IBD and are considering having a baby, it’s important to consult with your healthcare provider, such as a gastroenterologist and an obstetrician/gynecologist. While having IBD may present some challenges during pregnancy, many women with IBD can have successful pregnancies and healthy babies with proper medical care and management. Here are a few points to consider and discuss with your healthcare provider: (1) Pre-pregnancy planning: It’s a good idea to discuss your plans to conceive with your healthcare provider before getting pregnant. They can help you optimize your IBD management and make any necessary adjustments to your treatment plan to ensure your health is stable before conception; (2) Medication management: Many medications used to treat IBD have been studied for their safety during pregnancy. Your doctor will work with you to find the right balance between managing your disease and minimizing potential risks to the baby. In some cases, adjustments to medications might be needed during pregnancy; (3) Disease activity: Ideally, it’s best to conceive when your IBD is in remission or under good control. Active inflammation could potentially affect both your health and the health of the baby; (4) Nutrition and lifestyle: Maintaining a healthy lifestyle and nutrition plan can be crucial for managing IBD during pregnancy. Your doctor or a registered dietitian can provide guidance on foods that may help manage your symptoms; (5) Monitoring and follow-up: Regular prenatal care and monitoring are essential. Your healthcare team will monitor your IBD symptoms and adjust your treatment plan as needed throughout your pregnancy; and (6) Delivery and postpartum: The mode of delivery (vaginal or cesarean) may be influenced by your IBD status and any complications. Postpartum care should also be carefully managed to ensure your IBD remains well-controlled. Remember, every individual’s situation is unique, and the impact of IBD on pregnancy can vary. By working closely with your healthcare team and following their guidance, you can make informed decisions to promote a healthy pregnancy and successful outcomes for both you and your baby | Yes, many individuals with IBD can have successful pregnancies and healthy babies with proper medical care and management. However, it’s important to approach pregnancy with careful planning and consultation with your healthcare providers, including a gastroenterologist and an obstetrician/gynecologist. Here are a few key points to keep in mind: (1) Pre-pregnancy planning: Before trying to conceive, it’s advisable to consult with your healthcare team. They can assess your overall health, the status of your IBD, and your current treatment plan. This will allow them to make any necessary adjustments to ensure you’re in the best possible condition for pregnancy; (2) Medication management: Your healthcare provider will review your medications to ensure they are safe for pregnancy. In some cases, modifications to your treatment plan might be necessary to balance managing your IBD symptoms while minimizing potential risks to the baby; (3) Disease activity: If possible, it’s generally recommended to conceive when your IBD is in remission or well-controlled. Active inflammation could potentially affect your health and the health of the baby; (4) Prenatal care: Regular prenatal care is crucial for monitoring both your IBD and the progress of your pregnancy. Your healthcare team will work together to ensure your health and the health of your baby are being adequately managed; (5) Delivery planning: Depending on the status of your IBD and any potential complications, your healthcare team will discuss the most appropriate mode of delivery for you, whether it’s vaginal or caesarean; and (6) Postpartum care: After giving birth, it’s important to continue managing your IBD with your healthcare team’s guidance. They will monitor your condition and make any necessary adjustments to your treatment plan. Remember that each person’s situation is unique, and the impact of IBD on pregnancy can vary. By working closely with your healthcare providers and following their advice, you can increase the likelihood of a healthy pregnancy and successful outcomes for both you and your baby | Yes, it is possible to have a baby if you have IBD. Many individuals with IBD go on to have successful pregnancies and healthy babies. However, there are certain factors to consider and steps to take to ensure a safe and healthy pregnancy: (1) Consult your healthcare team: Before attempting to conceive, it’s important to consult with your healthcare providers, including your gastroenterologist and obstetrician/gynecologist. They can assess your current health, the severity of your IBD, and your medication regimen to determine if you are in a good condition for pregnancy; (2) Pre-pregnancy planning: Your healthcare team will work with you to optimize your IBD management before pregnancy. This might involve adjusting your medication, addressing any nutritional concerns, and ensuring your IBD is well-controlled; (3) Medication management: Many IBD medications have been studied for their safety during pregnancy. Your doctors will help you balance managing your IBD symptoms with the potential risks to the baby. In some cases, medication adjustments might be necessary; (4) Disease activity: If possible, it’s generally recommended to conceive when your IBD is in remission or well-controlled. Active inflammation could potentially affect both your health and the health of the baby; (5) Prenatal care: Regular prenatal check-ups are crucial to monitor both your IBD and the progress of your pregnancy. Your healthcare team will collaborate to ensure both your well-being and the baby’s health; (6) Delivery planning: Depending on the state of your IBD and any potential complications, your healthcare providers will help you decide on the best mode of delivery for you; and (7) Postpartum care: After giving birth, it’s important to continue managing your IBD with your healthcare team’s guidance. They will monitor your condition and make any necessary adjustments to your treatment plan. Remember that each person’s experience is unique, and the impact of IBD on pregnancy can vary. By working closely with your healthcare providers and following their guidance, you can increase the likelihood of a successful pregnancy and a healthy baby |
| Q6 | As of my last knowledge update in September 2021, most biologic drugs used for treating IBD are typically administered through subcutaneous injections or intravenous infusions. However, new developments and advancements in medical treatments may have occurred since then. Tablet or oral formulations of biologic drugs are an area of ongoing research and development. These formulations aim to provide a more convenient option for patients who prefer oral medications over injections or infusions. Oral administration of biologics could potentially improve patient compliance and quality of life. To get the most accurate and up-to-date information about the availability of tablet forms of biologic drugs for IBD treatment, I recommend discussing this with your gastroenterologist or healthcare provider. They will be able to provide you with information about the latest treatment options and whether any tablet formulations are currently available or under development for IBD management. Always consult with a medical professional for personalized advice regarding your specific condition and treatment options | As of my last update in September 2021, the majority of biologic drugs for IBD were administered through subcutaneous injections or intravenous infusions. However, there have been ongoing efforts to develop oral formulations of biologics for IBD treatment to offer patients a more convenient option. Since I don’t have access to real-time information beyond September 2021, I recommend checking with your healthcare provider or gastroenterologist for the latest updates on available treatment options. If any tablet forms of biologic drugs for IBD have been developed since then, your healthcare provider will be able to provide you with accurate and current information about whether this option is available for you and whether it’s suitable for your specific condition | As of my last knowledge update in September 2021, most biologic drugs for IBD were administered through subcutaneous injections or intravenous infusions. However, there were ongoing research and development efforts to create oral tablet forms of biologic medications for IBD to provide a more convenient option for patients. If you are interested in exploring the possibility of receiving your biologic drug in tablet form, I recommend discussing this with your healthcare provider or gastroenterologist. They will have the most up-to-date information about available treatment options and whether any tablet formulations have been approved or are in development for IBD treatment. Your healthcare provider will consider your individual medical history, disease severity, and treatment preferences to determine the best course of action for your specific situation. Always follow the guidance of your healthcare provider when making decisions about your treatment plan |
| Q7 | People with IBD, which includes conditions like CD and UC, do have an increased risk of developing colorectal cancer compared to the general population. However, the exact level of risk can vary based on factors such as the type and duration of IBD, the extent of inflammation, and individual characteristics. Here are some general points to consider: (1) Type of IBD: Patients with UC, especially if it involves a larger portion of the colon and has been present for a longer time, tend to have a higher risk of colorectal cancer compared to those with CD; (2) Duration of disease: The longer you have had IBD, the higher your risk of developing colorectal cancer. The risk generally increases after about 8-10 yr of having the disease; (3) Severity of inflammation: Those who experience more severe and widespread inflammation in the colon are at a higher risk of colorectal cancer; (4) Family history: If you have a family history of colorectal cancer or other risk factors, your overall risk may be higher; (5) Regular monitoring: Regular surveillance colonoscopies are often recommended for individuals with IBD to detect precancerous changes or early-stage cancer. The frequency of these screenings depends on individual risk factors and your doctor’s recommendations; (6) Management and treatment: Proper management of IBD, including medication and lifestyle changes, can help reduce the risk of colorectal cancer. Working closely with a healthcare provider is essential; and (7) Advancements in treatment: With advancements in IBD treatment and management, the risk of colorectal cancer in IBD patients has been decreasing over time. It’s important to have open and regular discussions with your healthcare provider about your specific risk profile and the steps you can take to minimize your risk. They can provide personalized guidance based on your medical history, current condition, and any other relevant factors | I’m not a doctor, but I can provide some general information based on existing knowledge. People with IBD, such as CD or UC, do have an increased risk of colorectal cancer compared to the general population. The exact level of risk can vary widely based on several factors, including the type of IBD, the extent and severity of inflammation, the duration of the disease, family history, and other individual characteristics. As a rough estimate, it’s been suggested that individuals with extensive and long-standing UC may have a colorectal cancer risk that is several times higher than that of the general population. However, advancements in treatment and monitoring have helped reduce this risk over the years. It’s important to work closely with your healthcare provider who can assess your specific risk factors and recommend appropriate monitoring and management strategies. Regular colonoscopies and other surveillance measures are often recommended for individuals with IBD to detect any potential precancerous changes or early signs of cancer. Remember that your healthcare provider is the best source of information regarding your personal health and risk factors | I understand your concern, but it’s important to note that I am not able to provide personalized medical advice or predict individual outcomes. The risk of colorectal cancer associated with IBD can vary significantly from person to person. It depends on factors such as the type of IBD (CD or UC), the duration and severity of the inflammation, your family history, and other individual factors. Generally, individuals with long-standing and extensive UC have a higher risk of developing colorectal cancer compared to those with CD or those with milder forms of IBD. However, advancements in medical management and surveillance have helped reduce the overall risk over the years. To get accurate and personalized information about your risk of colorectal cancer with your specific inflammatory bowel disease, it’s best to consult with your healthcare provider. They can assess your medical history, current condition, and other relevant factors to provide you with the most appropriate guidance and recommendations. Regular monitoring and open communication with your healthcare team are key to managing your health effectively |
| Q8 | I am not a doctor, but I can provide you with some general information based on what is known up to my knowledge cutoff date in September 2021. Biological therapies, also known as biologics, are a type of treatment often used for IBD such as CD and UC. These therapies target specific components of the immune system to help reduce inflammation and control symptoms of IBD. Biologics can be effective in managing IBD symptoms and inducing and maintaining remission. However, like any medical treatment, biological therapies do carry potential risks and side effects. Some of these risks include: (1) Infections: Biologics suppress certain aspects of the immune system, which can increase the risk of infections. While on biologics, you may be more susceptible to certain types of infections. It’s important to discuss your individual risk factors and ways to mitigate infection risks with your healthcare provider; (2) Cancer: Some studies have suggested a possible increased risk of certain types of cancers, particularly lymphomas and skin cancers, in individuals using biologics. However, the overall risk appears to be relatively low, and the benefits of controlling inflammation and maintaining remission may outweigh the potential risks. Regular monitoring and communication with your healthcare provider are essential; (3) Allergic reactions: While uncommon, some people may experience allergic reactions to biologics; (4) Other side effects: Biologics can also have other side effects, such as injection site reactions, fatigue, headaches, and more. Your healthcare provider will monitor you closely and help manage any side effects. It’s important to note that the risks and benefits of biological therapy can vary depending on the specific type of biologic, your individual health status, and other factors. Your healthcare provider will carefully evaluate your situation and help you make an informed decision about whether biologic therapy is the right choice for you. Always consult your healthcare provider for personalized advice and recommendations based on your specific medical history, current health status, and the latest available medical knowledge. They can provide you with the most up-to-date information and help you weigh the potential benefits and risks of any treatment option | As of my last knowledge update in September 2021, I can provide you with some general information about the potential risks associated with biological therapy for IBD. However, please keep in mind that medical knowledge and research can evolve, so it’s important to consult with your healthcare provider for the most up-to-date and personalized information: (1) Infection risk: Biological therapies work by targeting specific components of the immune system. While they can help control inflammation and manage IBD symptoms, they can also suppress the immune response, which may increase the risk of infections. Infections could range from common ones like respiratory infections to potentially more serious ones. It’s important to discuss your risk factors and preventive measures with your healthcare provider. They will likely monitor you closely for any signs of infection while you are on biological therapy; (2) Cancer risk: There have been concerns about a potential increased risk of certain types of cancers in individuals using biological therapies for IBD. The risk seems to be relatively low, and it’s important to weigh this risk against the potential benefits of managing your IBD symptoms. Some studies have suggested a slightly elevated risk of lymphomas and skin cancers. However, the overall risk increase is considered small, and many patients benefit greatly from biologic therapies. Regular monitoring and communication with your healthcare provider are key to managing any potential risks; and (3) Individual factors: Your specific risk factors for infections and cancer will depend on various factors, including the specific type of biological therapy you are considering, your medical history, your overall health, and any other treatments you might be undergoing. Your healthcare provider will assess these factors to help you make an informed decision about the best treatment approach for you. It’s important to have an open and thorough discussion with your healthcare provider before starting any new treatment, including biological therapies. They will be able to provide you with the most relevant and up-to-date information based on your individual circumstances. Additionally, they can help you understand the potential benefits and risks of the treatment and work with you to develop a plan that maximizes the benefits while minimizing potential risks | Yes, individuals with IBD who undergo biological therapy do carry a certain level of risk for infections and potentially some types of cancers. However, the actual risk varies depending on several factors including the specific type of biological therapy, your medical history, and other individual factors: (1) Infection risk: Biological therapies can suppress the immune system’s response to inflammation, which can increase the risk of infections. While the risk is generally higher compared to individuals not on these medications, the extent of the risk can vary depending on the specific drug, your overall health, and how closely you’re monitored. It’s important to work with your healthcare provider to minimize this risk and to promptly address any signs of infection; and (2) Cancer risk: Some studies have suggested a slightly elevated risk of certain cancers, particularly lymphomas and skin cancers, in individuals using certain types of biological therapies. However, the overall risk increase is generally considered to be low. Again, the specific risk varies based on the type of medication and other individual factors. Regular monitoring and open communication with your healthcare provider are crucial to manage this risk. Ultimately, the decision to undergo biological therapy should be made in consultation with your healthcare provider, taking into consideration your overall health, disease severity, treatment alternatives, and potential benefits and risks. Your healthcare provider will be able to guide you through the decision-making process, help you understand the potential risks, and monitor your health closely throughout the course of treatment |
| Q9 | IBD, which includes conditions like CD and UC, has a complex and multifactorial etiology involving both genetic and environmental factors. While there is a genetic component to IBD, it is not solely determined by genetics, and the risk of passing the disease on to your children is not absolute. Here are a few points to consider: (1) Genetics: IBD does have a genetic component, meaning that if you have IBD, there is a slightly increased risk that your children may also develop the condition. However, the exact genetic contribution is not fully understood, and having a family member with IBD doesn’t guarantee that your children will develop it; (2) Environmental factors: Environmental factors, such as diet, lifestyle, and exposure to certain triggers, also play a significant role in the development of IBD. It’s not only about genetics. Your children’s risk could be influenced by a combination of genetic susceptibility and environmental factors; (3) Complex inheritance: IBD is considered a complex genetic disorder, meaning that it is influenced by multiple genes rather than being caused by a single gene. This complexity makes it challenging to predict the likelihood of transmission to your children; (4) Risk factors: If one parent has IBD, the risk of their children developing the disease is slightly higher compared to the general population, but it is still relatively low. If both parents have IBD, the risk may be higher than if only one parent is affected; and (5) Genetic counseling: If you are concerned about the potential transmission of IBD to your children, it’s a good idea to consult with a genetic counselor or a medical professional who specializes in this area. They can provide personalized information based on your medical history, family history, and current understanding of the genetic factors involved. Remember that genetics is just one piece of the puzzle, and many other factors contribute to the development of IBD. If you have concerns about IBD and its potential impact on your children, it’s best to have an open and thorough discussion with a healthcare provider who can provide guidance and address your specific situation | The transmission of IBD to children is not a straightforward process and can be influenced by a combination of genetic and environmental factors. While there is a genetic component to IBD, it doesn’t guarantee that your children will definitely inherit the condition. Here’s what you should consider: (1) Genetic predisposition: There is a genetic predisposition to IBD, which means that having a family member with the condition increases the risk of developing it. However, the genetics of IBD are complex and involve the interaction of multiple genes. It’s not a simple case of one gene causing the disease. This makes it difficult to predict with certainty whether your children will inherit IBD; (2) Environmental factors: Environmental factors play a significant role in the development of IBD. Factors such as diet, lifestyle, exposure to certain triggers, and the overall environment can contribute to the onset and severity of the disease. Even if your children have a genetic predisposition, environmental factors could influence whether or not they actually develop IBD; (3) Relative risk: Having a parent with IBD does increase the risk for children, but the actual risk remains relatively low. If one parent has IBD, the risk for their children is higher compared to the general population but is still not a certainty. If both parents have IBD, the risk may be slightly higher; (4) Genetic counseling: If you are concerned about the potential transmission of IBD to your children, it’s advisable to consult with a genetic counselor or a healthcare professional who specializes in this area. They can assess your specific situation, provide information about the genetic factors involved, and offer guidance on potential risks; and (5) Advancements in research: Medical knowledge and research are continuously advancing. There might be new insights and discoveries about the genetics and inheritance of IBD in the future that could provide a clearer understanding of the risks involved. Ultimately, while there is a genetic component to IBD, it is not the sole determinant of whether your children will develop the condition. Genetic predisposition combined with environmental factors contribute to the overall risk. If you have concerns about passing on IBD to your children, seeking guidance from medical professionals with expertise in this area is recommended | I understand your concern, but I’m not able to provide personalized medical predictions. The risk of transmitting IBD to your children depends on a combination of genetic and environmental factors. While there is a genetic predisposition to IBD, it’s not a guarantee that your children will inherit the condition. IBD is influenced by multiple genes, and the interplay between these genes and environmental factors makes it challenging to predict the exact likelihood of passing the disease on to your children. Genetic factors do increase the risk, especially if you or your partner have IBD, but many individuals with a family history of IBD do not develop the disease. If you are concerned about the potential transmission of IBD to your children, I recommend consulting a healthcare professional or a genetic counselor. They can provide more personalized information based on your medical history, family history, and current understanding of the genetics of IBD |
| Q10 | I am not a doctor, but I can provide you with some general information. The decision about whether to use biological therapy after a CD surgery depends on various factors, including the severity of your condition, the extent of the surgery, your overall health, and your doctor’s recommendations. Biological therapies, such as anti-TNF drugs (e.g., infliximab, adalimumab), are often used to treat CD because they can help reduce inflammation and manage symptoms. They may be recommended to help prevent flare-ups or recurrence of the disease after surgery. It’s important to have an open and thorough discussion with your gastroenterologist or healthcare provider about your treatment options. They can provide personalized advice based on your medical history, current condition, and specific circumstances. If you have concerns about biological therapy, make sure to express them to your doctor so they can address them and work with you to find the most appropriate treatment plan. Remember, the decision to use or avoid biological therapy should be made in consultation with a qualified healthcare professional who has a complete understanding of your individual situation | Whether or not you can avoid biological therapy after your first CD surgery depends on several factors, and it’s a decision that should be made in consultation with your healthcare provider. Here are a few points to consider: (1) Severity of CD: If your CD is severe and has a high likelihood of recurrence after surgery, your doctor might recommend starting or continuing biological therapy to help prevent flare-ups; (2) Extent of surgery: The type of surgery you underwent and the amount of affected intestine that was removed can influence the risk of recurrence. More extensive surgeries may be associated with a higher risk of disease recurrence; (3) Medical history: Your medical history, including how well you responded to previous treatments, any complications you’ve experienced, and your overall health, will play a role in determining your post-surgery treatment plan; (4) Risks and benefits: Your doctor will weigh the potential benefits of biological therapy in preventing disease recurrence against the risks and side effects associated with these medications; (5) Patient preference: Your preferences and comfort with different treatment options are important. If you have concerns about biological therapy, make sure to discuss them with your doctor; (6) Alternative treatments: There are various treatments available for CD beyond biological therapies. Your doctor might consider other medications, dietary changes, and lifestyle modifications based on your specific situation; and (7) Regular monitoring: Even if you don’t start biological therapy immediately after surgery, your doctor will likely recommend regular follow-up appointments and monitoring to detect any signs of disease recurrence early. Ultimately, the decision about post-surgery treatment should be a collaborative one between you and your healthcare provider. They can provide you with the most up-to-date information about treatment options, potential benefits, risks, and expected outcomes based on your unique medical history and current condition. It’s important to have an open and honest conversation with your doctor to ensure you make the best decision for your health | Yes, it is possible to avoid biological therapy after your first CD surgery, but the decision will depend on several factors, including the recommendations of your healthcare provider, the severity of your condition, and your individual circumstances. Here are a few things to consider: (1) Doctor’s recommendation: Your healthcare provider will assess your medical history, the extent of your surgery, the severity of your CD, and your risk of recurrence. Based on these factors, they will recommend a treatment plan, which may or may not include biological therapy; (2) Disease severity: If your CD is relatively mild and your surgery was successful in removing the affected area, your doctor might consider alternatives to biological therapy, such as traditional medications or lifestyle changes; (3) Risk of recurrence: CD has a tendency to recur even after surgery. If your doctor believes that your risk of disease recurrence is high, they may recommend starting or continuing with biological therapy to help prevent flare-ups; (4) Personal preference: Your preferences and comfort with different treatment options are important. If you have concerns about biological therapy, make sure to express them to your doctor. They can discuss the pros and cons of various treatments with you; (5) Alternative treatments: There are other treatments available for CD, such as immunosuppressive medications, corticosteroids, and lifestyle modifications. Your doctor may explore these options based on your specific situation; and (6) Regular monitoring: Regardless of the treatment plan, it’s likely that your doctor will recommend regular follow-up appointments and monitoring to track your disease progression and adjust your treatment if necessary. It’s crucial to have an open and thorough discussion with your healthcare provider about your treatment options. They can provide you with the information you need to make an informed decision about whether to pursue biological therapy or explore alternative treatments. Remember that your doctor’s expertise and understanding of your condition are essential in guiding your treatment journey |