Modified Y Splitting of Lateral Rectus in Treatment of Abnormal Vertical Eye Movements Combined with Globe Retraction in Duane Retraction Syndrome
A B S T R A C T
Duane retraction syndrome is the most frequently seen restrictive ocular motility disorders. It is clinically presented with limitation of horizontal movement, variable amounts of upshoots or downshoots and globe retraction combined with narrowing of the palpebral aperture on attempted adduction. An 8-year-old patient presented with severe restriction of abduction, reciprocal upshots or downshoots, and globe retraction combined with the palpebral fissure narrowing of on adduction. After the modified Y splitting of LR and recession of both horizontal rectus operation, all cosmetically disfiguring clinical features disappeared. In this case report modified Y splitting procedure and its long-term efficacy is presented.
Keywords
Duane retraction syndrome, modified Y splitting, force duction test, upshoot, downshoot, globe retraction
Introduction
Duane retraction syndrome (DRS) is the most frequently seen congenital cranial dysinnervation syndrome among ocular motility disorders. The frequency of DRS is 1-4% in the general population of strabismus patients. This syndrome is characterized by the limitation of abduction with or without limitation of adduction, narrowing of the palpebral aperture combined with globe retraction along with variable amounts of up shoots or down shoots on attempted adduction [1-3]. DRS as a congenital cranial dysinnervation disorder has been classified into three subtypes according to the basis of electromyography by Huber and limitation of horizontal muscle activation [4, 5]. DRS can also be differentiated on the basis of deviation in primary position as eso-DRS, exo-DRS, and ortho-DRS which is easier to use for surgical planning. The primary indication for surgery in these eyes is the correction of deviation in primary position and anomalous face turn. Rather than horizontal deviation, globe retraction, up shoots and/or down shoots narrowing of the palpebral aperture on attempted adduction can be cosmetically very disfiguring in most cases [2, 3, 6].
Several surgical alternatives can be performed to correct different clinical presentation of DRS such as horizontal rectus recessions, vertical rectus transpositions, periosteal fixation or splitting of LR [7-10]. In this article surgical result of modified Y splitting combined with both horizontal rectus recession in patient with Type I Duane syndrome who has absence of abduction, prominent globe retraction, severe narrowing of the palpebral aperture and reciprocal upshoot and downshoot in adduction are presented [11].
Case Report
An 8-year-old female patient with Type I Duane syndrome was presented orthophoria without any abnormal head posture in primary position. On clinical examination she had severe limitation in left eye’s abduction with significant globe retraction with prominent narrowing of the palpebral fissure and reciprocal up shoots or down shoots in adduction. Her visual acuity was 10/10 in the both eyes without correction. This means the patient was Type I DRS with cosmetically unacceptable configuration in adduction (Figures 1A-1C).
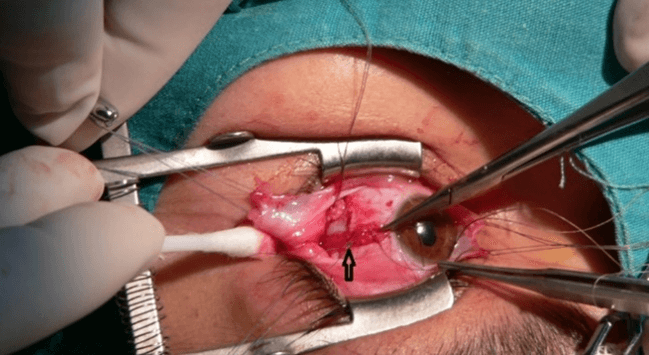
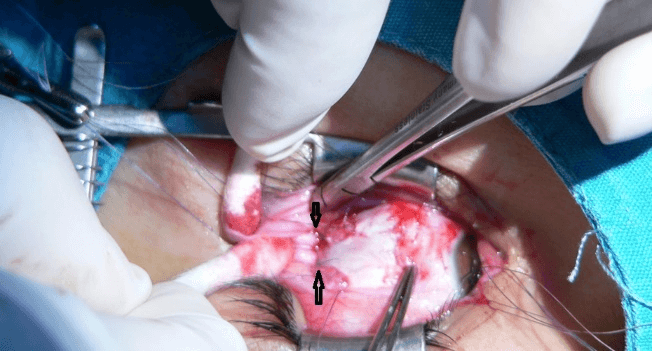
To treat her globe retraction and abnormal vertical eye movements in adduction she underwent surgical intervention in general anaesthesia. Intraoperatively, forced duction testing (FDTs) for lateral rectus muscles was severely positive. Any insertions pathologies such as abnormal muscle slips or foot plates attaching to the sclera were not observed any side of the muscles intraoperatively. The medial rectus muscle was recessed 5.5 mm and the lateral rectus was recessed 7 mm combined with modified Y-split. In modified Y splitting procedure to protect refusion of the middle split part of the LR muscle due to re-proliferation of muscle fibers, nonabsorbable separation sutures were placed around the split parts of the upper and lower halves, 5 mm behind the insertion, without scleral fixation as we describe previously (Figures 2A & 2B).
Figure 1A: Orthophoria in primary position.
Figure 1B: Limitation of abduction from central position in preoperative period.
Figure 1C: Duane Retraction Syndrome Type I: Upshoot, glob retraction combined combined with narrowing of the aperture on attempted adduction.
Figure 2A: Modified Y splitting; Nonabsorbable separation sutures was placed around the split parts of the upper halves on the marked side.
Figure 2B: Modified Y splitting; Separation sutures were placed around the both upper and the lower halves of Y splitting on the marked with arrow.
Five years after surgery, she was still orthotropic in primary position with no abnormal head posture. Her globe retraction, narrowing of the palpebral fissure and abnormal vertical eye movements were improved considerably without any recurrence (Figures 3A-3C).
Figure 3A: Orthophoria in primary position in postoperative period.
Figure 3B: Minimal abduction from the central position with persistatnt restriction postoperatively.
Figure 3C: Upshoot, glob retraction and narrowing of the aperture on adduction are disappeared after the modified Y splitting on LR combined with both horizontal rectus recession.
Discussion
In DRS upshoots and downshoots occurs in 25-39% of patients. The pathogenesis of globe retraction and over elevation or over depression in adduction can be presented by mechanical factors such as tight fibrotic muscles or anomalous insertions as well as innervational anomalies such as paradoxical innervation causing the co-contraction of both MR and LR in the same eye. The mechanical effect of these abnormal ocular movements can be described as due to a “bridle effect” or also known as the “leash effect” of the tight LR. In adduction following a small vertical movement a sudden slippage of the tight LR on the globe, causes either mechanical up shoot or down shoot. The upshoot and downshoot can occur reciprocally in same eye in mechanical type in contrast, only one of the upshoot or downshoot can happen in the innervational type [1, 3, 7, 9, 12, 13]. Our patient had reciprocal upshoot or downshoot and prominent restriction was observed in forced duction test of LR intraoperatively. According to these findings she had a mechanical type of abnormal vertical eye movements and glob retraction.
Forced duction tests is essential to evaluate the contracture or fibrosis in both MR and LR for planning surgery in DRS. Rogers and Bremmer have developed Y splitting surgery of the LR to treat abnormal vertical eye movements in cases with mechanical leash effect [14]. Y splitting of the LR can be performed either combined with or without recession operation. In Y splitting procedure each muscle half balances the other half part. When the eye attempt to depress in adduction the upper arm contracts, by this way, it prevents the globe from suddenly slipping down and vice versa in elevation [11, 14, 15].
For treatment of glob retraction either in the presence of co-contractions or mechanical restriction, simultaneous recession of both LR and MR are recommended. Y splitting of the LR combined with both horizontal rectus recession is reported to be an extremely effective procedure in the treatment of glob retraction associated with up shoot or down shoot [11, 15-18]. Sukhija et al. reported that combined Y-split recession procedure achieved a more significant improvement of abnormal vertical eye movements than recession without Y splitting [16]. But according to their observation combined surgery has higher incidence of postoperative complications. It is reported that modified Y splitting procedure is an effective surgery to maintain long term stabilization [11]. In this modified Y splitting procedure nonabsorbable separation sutures were placed around the both split parts of the upper and lower halves, 5 mm behind the insertion of muscle, without scleral fixation. By this way separated halves stay stable [11]. Our patient we performed modified Y splitting in LR combined with both horizontal rectus recession and all clinical signs such as globe retraction, narrowing of the palpebral fissure and abnormal vertical eye movements were improved. In orthotropic DRS Gaur and Sharma suggested that equal amount of recession of both MR with the use of adjustable suture and LR with Y splitting to achieve desirable outcome to treat glob retraction and abnormal vertical eye movements [6]. But adjustable surgery can be performed either as a two-stage procedure or intraoperatively under local anaesthesia [19]. Our 8-year-old patient had undergone modified Y splitting combined with horizontal rectus recession in general anaesthesia we did not prefer two stage procedure.
Akbari et al. prefer that 1-2 mm more recession of LR than the amount of MR recession [20]. in DRS without deviation in primary position to correct glob retraction and upshoot and downshoot. Rao et al. performed 5.0 to 9.0 mm recession of LR and Y splitting their patient [18]. It is generally recommended that MR recession is ranging from 5 to 6.5 mm and LR ranging from 7 to 9 mm [7, 13, 21]. We performed 5.5 mm recession of MR and 7 mm recession combined with modified Y splitting of LR in our case and did not observed any recurrence in 5 years period. DRS has varied clinical presentation; treatment alternatives should be individualized for the patients depend on clinical presentation and FDT. Modified Y splitting procedure combined with simultaneous recession of LR and the MR muscle is an effective procedure in the treatment of globe retraction associated with significant upshoot and downshoot in DRS in long term follow up in our patient.
Article Info
Article Type
Case ReportPublication history
Received: Wed 01, Jul 2020Accepted: Tue 27, Oct 2020
Published: Wed 18, Nov 2020
Copyright
© 2023 Ayse Gul Kocak Altintas. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.04.02
Author Info
Corresponding Author
Ayse Gul Kocak AltintasSaglik Bilimleri University, Ulucanlar Eye Hospital, Ankara, Turkey
Figures & Tables


References
- Mohan K, Sharma A, Pandav SS (2008) Differences in epidemiological and clinical characteristics between various types of Duane retraction syndrome in 331 patients. J AAPOS 12: 576-580. [Crossref]
- Kekunnaya R, Gupta A, Sachdeva V, Krishnaiah S, Rao BV et al. (2012) Duane retraction syndrome: series of 441 cases. J Pediatr Ophthalmol Strabismus 49: 164-169. [Crossref]
- Yüksel D, Orban de Xivry J, Lefèvre P (2010) Review of the major findings about Duane retraction syndrome (DRS) leading to an updated form of classification. Vision Res 50: 2334-2347. [Crossref]
- Assaf AA (2011) Congenital innervation dysgenesis syndrome (CID)/congenital cranial dysinnervation disorders (CCDDs). Eye (Lond) 25: 1251-1261. [Crossref]
- Huber A (1974) Electrophysiology of the retraction syndromes. Br J Ophthalmol 58: 293-300. [Crossref]
- Gaur N, Sharma P (2019) Management of Duane Retraction Syndrome: A Simplified Approach. Indian J Ophthalmol 67: 16-22. [Crossref]
- Kekunnaya R, Kraft R, Rao VB, Velez FG, Sachdeva V et al. (2015) Surgical management of strabismus in Duane retraction syndrome. J AAPOS 19: 63-69. [Crossref]
- Das JC, Chaudhuri Z, Bhomaj S, Sharma P (2000) Lateral Rectus Split in the Management of Duane's Retraction Syndrome. Ophthalmic Surg Lasers 31: 499-501. [Crossref]
- Yang S, MacKinnon S, Dagi LR, Hunter DG (2014) Superior rectus transposition vs medial rectus recession for treatment of esotropic Duane syndrome. JAMA Ophthalmol 132: 669-675. [Crossref]
- Sharma P, Tomer R, Menon V, Saxena R, Sharma A (2014) Evaluation of periosteal fixation of lateral rectus and partial VRT for cases of exotropic Duane retraction syndrome. Indian J Ophthalmol 62: 204-208. [Crossref]
- Altintas AGK, Arifoglu HB, Arikan M, Simsek S (2010) Clinical Findings and Surgical Results of Duane Retraction Syndrome. J Pediatr Ophthalmol Strabismus 47: 220-226. [Crossref]
- Pineles SL, Velez FG (2015) Accessory fibrotic lateral rectus muscles in exotropic Duane syndrome with severe retraction and upshoot. J AAPOS 19: 549-550. [Crossref]
- Kekunnaya R, Negalur M (2017) Duane retraction syndrome: causes, effects and management strategies. Clin Ophthalmol 11: 1917-1930. [Crossref]
- Rogers GL, Bremmer DL (1984) Surgical treatment of the up-shoot and down-shoot in Duane’s retraction syndrome. Ophthalmology 91: 1380-1382. [Crossref]
- Farid MF (2016) Y-split recession vs. isolated recession of the lateral rectus muscle in the treatment of vertical shooting in exotropic Duane retraction syndrome. Eur J Ophthalmol 26: 523-528. [Crossref]
- Sukhija J, Kaur S, Singh U (2014) Isolated lateral rectus recession with Y splitting versus anchoring of the lateral rectus muscle in patients with exotropic Duane syndrome. J AAPOS 18: 147-150. [Crossref]
- Velez FG, Velez G, Hendler K, Pineles SL (2012) Isolated Y-splitting and recession of the lateral rectus muscle in patients with Exo-Duane syndrome. Strabismus 20: 109-114. [Crossref]
- Rao VB, Helveston EM, Sahare P (2003) Treatment of upshoot and downshoot in Duane syndrome by recession and y-splitting of the lateral rectus muscle. J AAPOS 7: 389-395. [Crossref]
- Holmes JM, Hatt SR, Leske DA (2012) Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS 16: 136-140. [Crossref]
- Akbari MR, Manouchehri V, Mirmohammadsadeghi A (2017) Surgical treatment of Duane retraction syndrome. J Curr Ophthalmol 29: 248-257. [Crossref]
- Sachdeva V, Kekunnaya R, Gupta A, Bhoompally VR (2012) Surgical management of bilateral esotropic Duane syndrome. J AAPOS 16: 445-448. [Crossref]
