Initial experience in uniportal video-assisted thoracoscopic surgery (VATS) for major lung resections—Australia’s first uniportal VATS teaching program
Introduction
Thoracic surgery has seen a natural evolution from open procedures to minimally invasive thoracoscopic techniques, viz; video-assisted thoracoscopic surgery (VATS). For over two decades VATS has shown significant reduction in post-operative pain and associated chest wall paraesthesia, morbidity and mortality, length of hospital stay with hastened recovery and return to pre-morbid baseline, whilst providing improved cosmetics (1). Despite these great improvements, thoracic surgeons have continued to explore techniques to improve access and thus further minimise post-operative complications and side-effects without compromising on the safety and efficacy of surgery. The past 20 years have seen conventional 3-port VATS evolve into 2-port VATS and subsequently into uniportal VATS surgery, which was first pioneered by Dr. Gaetano Rocco for simpler intra-thoracic procedures over a decade ago. More recently uniportal VATS has been developed by Dr. Diego Gonzalez-Rivas of A Coruña, Spain to perform complex major lung resections (1-3) and is rapidly being adopted around the world due to Dr. Gonzalez-Rivas’ willingness to travel around the world and make it available to thoracic surgeons with a keen interest (4).
Motivation
The senior author’s primary motivation to enhance our existing VATS program is multi-faceted. Firstly, uniportal VATS is a valuable addition to the thoracic surgeon’s repertoire, affording greater choice when delivering optimal patient care. Secondly, there are clear benefits to both the patient and the surgeon in certain cases. The breach of only a single intercostal space offers both a potential reduction in post-operative pain and chest wall paraesthesia as well as conferring a cosmetic advantage. Furthermore, Harris et al. performed a meta-analysis demonstrating a statistically significant reduction in chest tube drainage and overall morbidity. For the surgeon the obvious advantage is the approach to the target anatomy with a similar view to open surgery (4). For the hospital, a statistically significant reduction in hospital stay directly translates into improved cost-effectiveness. Thirdly, being a significant teaching thoracic service in Australasia, there is a strong incentive for the unit to continue to be proficient in all techniques and promote and nurture the growth and development of advanced thoracic surgery techniques to other units in the Australasian region.
Challenges
The authors perceived numerous challenges associated with development of a uniportal VATS program, which included patient selection, navigation of the conceptual and practical learning curve of the technique, optimal surgical and anaesthetic setup and availability of an immediate backup plan in case of emergency. Thus, with these challenges in mind we delayed the introduction of uniportal VATS until we had confirmed proctorship by Dr. Gonzalez-Rivas, with whom we could ensure the setup and delivery of a safe and efficient program initially at The Royal Melbourne Hospital, Melbourne.
In this article the authors highlight our experience with uniportal VATS at two centres in Melbourne including the importance of proctorship and case selection and our initial results reflecting hospital length of stay, subjective analysis on post-operative pain and outcomes.
Establishing a uniportal program
Our program comprises four full time thoracic surgeons split over two sites, with a cumulative total of greater than 50 years of VATS surgery experience. The two surgeons who elected to spearhead the uniportal program have a combined total of 30 years VATS surgery and therefore have a well-established foundation upon which to develop the competencies required for safe and efficient uniportal surgery. Prior to performing the first uniportal case, the two surgeons went through a rigorous set of criteria to select the most appropriate first case:
Age and pre-morbid fitness
It is important to select a younger patient with no major co-morbidities because they are physiologically more robust and would tolerate conversion to thoracotomy in the case of emergency.
Virgin chest
It is important to select a patient who has had no previous surgery or radiotherapy intervention to the chest, which could present significant adhesions and thus increase the risk of the surgery.
Tumour location and lung architecture
It is important to select initial cases with near-complete fissures, normal lung architecture and anatomy and peripherally located lesions. These features allow for easier intraoperative lung manipulation.
Proctorship
Having an experienced uniportal VATS surgeon to proctor the initial cases is of paramount importance. Many years of trial-and-error can be avoided and the learning condensed into a short timeframe. It provides an opportunity to discuss case selection for the uniportal approach, in particular to explore factors that may favour a uniportal approach versus factors that do not. Furthermore, prior to performing the first surgery, our proctor hosted a presentation session during which a variety of uniportal cases were highlighted, discussing the journey from case selection, optimal operative setup, tips to improve the surgical technique and potential pitfalls and how to salvage an emergency situation.
On the day of surgery, a pre-surgical briefing is held, led by the operating surgeon and the proctor. In this session, the case being performed is discussed in detail including the reason for surgery, the roles of each member of the team and the desired outcome of the surgery and the plan in case of an intra-operative complication. During surgery itself, the proctor was present alongside the operating team thereby ensuring maximal contemporaneous feedback. It is also important to note that when embarking on a new procedure for the first time, the remainder of the operating list is kept free from other cases. This ensures that there is no time pressure for the chosen case allowing for complete dedication to the case in question without competing interests.
First uniportal case completion in Australia with tips and tricks
We performed the first successful uniportal lobectomy in Australia on a 68-year-old female with a 28-mm adenocarcinoma in the left lower lobe with no clinical lymph node involvement. Her history included high-grade endometrial carcinoma, which, while being investigated, detected a suspicious lung nodule. This patient underwent a left lower lobectomy with lymph node dissection. Histology confirmed a moderately well differentiated adenocarcinoma of predominantly papillary origin, with a single hilar lymph node positive. Post-operative recovery was unremarkable with chest drains removed on day 1 and discharge home on day 4. At twelve months follow-up the patient is doing well with no recurrence of disease.
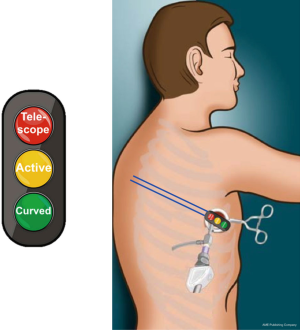
Proctorship shaped the way we perform uniportal VATS surgery (Figure 1). The key points include following a “traffic light” orientation in the chest wound with the thoracoscope (5 or 10 mm, 30 degree) being at the “red” light position at the superior aspect of the incision. The operating instruments held in the surgeons left or right hands being placed inferior to the thoracoscope in the “amber” light position and in the “green” light position at the inferior aspect of the wound is placed an “upturned” sucker. One of the greatest challenges in uniportal surgery is for the assistant to maintain the camera at the “red” light position in the wound (1). The authors addressed this by fixing a silastic sling to the patients’ drape, which acts as a harness in which the thoracoscope can be placed and held in the correct position without any chance of migration in the wound (Figure 2). Other tips are summarised in Table 1.
Table 1
| Tip | Advantage |
|---|---|
| Long, curved instruments | Minimises clash between instruments and maintains triangulation |
| Silastic sling “holder” | Maintains position of thoracoscope |
| Free movement of assistant | Minimises clashes between instrument and thoracoscope |
| Long, curved grasper for lung retraction | Problematic exposure |
| Table movement | Anterior for nodal dissection |
| Posterior for hilum exposure ( |
Results
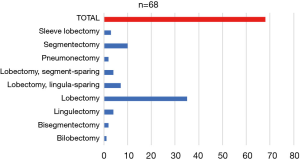
During the period February 2018 to February 2019 a total of 68 uniportal VATS anatomic lung resections were successfully performed. In comparison to multiport VATS the age group of patients operated using the uniportal approach was younger—median age 69 (range, 48–85) versus 64 (range, 29–81) years respectively. The complexity of cases varied from lobectomy/segmentectomy to sleeve lobectomy (Figure 3). Two cases required conversion, one requiring conversion to thoracotomy and another “conversion” to 2-port VATS; both for vessel injury.
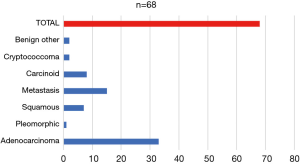
The vast majority of tumours resected were adenocarcinomas (Figure 4) with all non-small cell lung cancer (NSCLC) tumours being resected with clear margins. One sarcoma metastasectomy resulted in a microscopic positive margin (R1) in an S1/S3 bisegmentectomy. The R1 rate for malignancy was therefore calculated at 1/64 (1.6%).
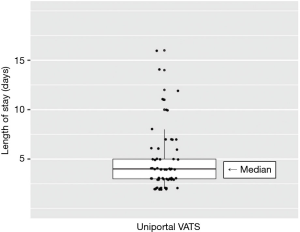
The median hospital stay was 4 days (95% CI: 2–15 days) (Figure 5). This is shorter than our historical multi-port VATS experience for major lung resections of 6 days (95% CI: 3–25 days); P<0.001 (Mann-Whitney test). Three patients required readmission post-discharge from hospital (late air leak =1; fever and effusion =1; failure to cope =1).
Subjective pain assessment of patients collectively demonstrated a reduction in pain when compared to conventional multiport VATS surgery in our institutions.
Conclusions
The authors report the results of Australia’s first dedicated uniportal VATS program. The program was simultaneously established in February 2018 at two major thoracic surgery centres in Victoria, which share the senior surgeon/author of this publication. In 12 months, 68 major anatomical lung resections were performed, 41 for NSCLC and 27 for other conditions, by uniportal VATS. It should be noted that the number of lung resections performed is reflective of the competitiveness that uniportal VATS offers in our institution considering we also perform robotic and 2- and 3-port VATS lobectomies routinely. The range in complexity varied from simple lobectomy/segmentectomy to sleeve resections. Our conversion rate was acceptably low with only one case out of the two requiring thoracotomy. Our results show that length of stay, time to chest drain removal and return to pre-morbid status is comparable, or possibly superior, to multi-port VATS surgery. Furthermore, subjective assessment of post-operative pain appears to be reduced in the uniportal group. This is currently being evaluated through a prospective analysis comparing uniportal VATS versus 2- and 3-port VATS at our institution. In our opinion thoracic surgeons who have prior VATS experience at performing lung resections should be able to make a smooth transition to uniportal surgery provided the following recommendations are closely followed. Firstly, it is vital that an expert proctor is engaged to help establish the program and provide on-site guidance during the initial case(s). We suggest the proctor be available for the initial 2–3 cases for those surgeons with greater than 10 years’ experience of complex VATS lung resections. For those surgeons with minimal VATS experience we suggest establishing 3- or 2-port approaches initially using a similar model of proctoring. Secondly, cases should be selected with particular attention to age and pre-morbid fitness, lung anatomy, tumour location and avoiding cases with prior thoracic surgical or radiotherapy interventions. When considering choice of access, one must always prioritise the triad of tenets of thoracic surgical oncology, i.e., (I) safe surgery, (II) complete resection and (III) maximal sensible preservation of parenchyma. The authors have demonstrated the introduction of a safe and efficient uniportal VATS program through strict adherence to the aforementioned recommendations and persisting through the initial learning curve, with results comparable to multi-port VATS.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Diego Gonzalez-Rivas) for the series “Teaching Uniportal VATS” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.03.13). The series “Teaching Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Individual informed consent was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Guerrero WG, González-Rivas D. Multiportal video-assisted thoracic surgery, uniportal video-assisted thoracic surgery and minimally invasive open chest surgery—selection criteria. J Vis Surg 2017;3:56. [Crossref] [PubMed]
- Shukla R, Vijayapuri S, Rahnavardi M, et al. Uniportal VATS left lower lobectomy. Asvide 2019;6:116. Available online: http://www.asvide.com/article/view/31135
- Reinersman JM, Passera E, Rocco G. Overview of uniportal video-assisted thoracic surgery (VATS): past and present. Ann Cardiothorac Surg 2016;5:112-7. [Crossref] [PubMed]
Cite this article as: Shukla R, Vijayapuri S, Rahnavardi M, Barnett SA, Wright GM. Initial experience in uniportal video-assisted thoracoscopic surgery (VATS) for major lung resections—Australia’s first uniportal VATS teaching program. J Vis Surg 2019;5:42.