Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.5030
Peer-review started: March 26, 2020
First decision: August 23, 2020
Revised: September 2, 2020
Accepted: September 28, 2020
Article in press: September 28, 2020
Published online: October 26, 2020
Posterior scleritis is a rare inflammatory ocular disease, characterized by severe and painful inflammation of the sclera. It is often misdiagnosed or underdiagnosed, due to its general and varying clinical presentation profile, which primarily involves pain and visual impairment but which can include eyelid edema, choroidal folds, serous retinal detachment, disc edema, hard exudates in fovea and subretinal mass. We report here a case of posterior scleritis, with symptoms of eye pain and red eye, initially misdiagnosed as acute conjunctivitis.
A 56-year-old man presented to a local hospital with complaint of pain and redness in the right eye. The initial diagnosis was acute conjunctivitis and he was given antibiotic eyedrops. Upon week-long continuance of the symptoms despite treatment, he presented to our hospital. Initial examination revealed a shallow anterior chamber in the right eye and vision reduction to 0.6. Further testing by optical coherence tomography, ultrasound biomicroscopy, and fundus photography indicated diagnosis of posterior scleritis. The patient was given methylprednisolone (oral) on a tapered reduction schedule (starting with 70 mg/d). According to the peaks and troughs of symptoms, compound betamethasone injection was administered into the bulb, culminating in discontinuation of the oral corticosteroid. Subsequent optical coherence tomography showed the subretinal fluid near the optic disc to be completely absorbed after treatment.
Posterior scleritis should be among the differential diagnosis of eye pain and redness, and diagnosis requires further ophthalmic accessory examination, such as by optical coherence tomography.
Core Tip: We report here a rare case of posterior scleritis, which was initially misdiagnosed as acute conjunctivitis due its presentation of non-specific clinical features, specifically eye pain and redness. Ophthalmic accessory examinations, such as optical coherence tomography, ultrasound biomicroscopy and fundus photography, should be conducted in the early stage of this disease; this will facilitate making the appropriate differential diagnosis and avoid delay in treatment, which could otherwise lead to the loss of vision.
- Citation: Li YZ, Qin XH, Lu JM, Wang YP. Monocular posterior scleritis presenting as acute conjunctivitis: A case report. World J Clin Cases 2020; 8(20): 5030-5035
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/5030.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.5030
Posterior scleritis is an uncommon inflammatory ocular disease, characterized by severe and painful inflammation of the sclera[1]. It accounts for only 2%-12% of all scleritis cases, mainly affecting patients between the ages of 45- to 49-years-old[2]. While ocular pain is an important manifestation of posterior scleritis prompting seeking out of treatment, most patients also experience diminution of vision[3]. Anterior uveitis is another common symptom in patients with posterior scleritis, with one study finding it in approximately 55% of patients[4]. Other rarer presentations include eyelid edema, choroidal folds, serous retinal detachment, disc edema, hard exudates in fovea, and subretinal mass[3].
Unfortunately, the general and varying clinical symptom profile described above underlies posterior scleritis being frequently misdiagnosed or underdiagnosed[5]. It is usually misdiagnosed as intraocular inflammation, orbital inflammation, ocular tumors, central serous chorioretinopathy, or Vogt-Koyanagi-Harada disease[6]. Sin et al[7] reported a case of nodular posterior scleritis that presented as a choroidal mass in a patient with systemic lupus erythematous in 2016. Alsharif et al[8] described a 30-year-old man with a history of painless subacute loss of vision for 5 mo in his left eye and was diagnosed as atypical posterior scleritis which was mimicking the amelanotic choroidal melanoma. However, ruling out the differentials to make an accurate diagnosis is critical for subsequent treatment.
A 56-year-old man visited our department with complaint of right eye pain and redness that had been diagnosed at a local hospital as acute conjunctivitis 1 wk ago.
The patient reported a 1-wk experience of pain and redness in his right eye (but no blurred vision) that prompted him to visit a local hospital, where he was diagnosed with acute conjunctivitis of the right eye. He was sent home with antibiotic eye drops to be applied for 1 wk. When he experienced no improvement in his symptoms, he presented to our department for treatment. We also gave the initial diagnosis of acute conjunctivitis, in accordance with the obvious eye redness. Levofloxacin eye drops were prescribed (6 times/d), but after 1 wk the pain and redness did not subside and the patient began to experience a decrease in vision.
The patient reported no history of systemic hypertension, diabetes mellitus, coronary heart disease, stroke, smoking, or obesity.
The visual acuity in the right eye was found to have reduced to 0.6. The conjunctiva of the right eye was also found to be obviously congested. The patient’s cornea was transparent but a shallow anterior chamber was found in the right eye. The right pupil appeared round and with normal light reflection. There was no opacity in the right lens. The intraocular pressure was within normal limits. However, ophthalmoscopy revealed retinal folds around the optic disk in the right eye. The left eye was normal overall.
Laboratory examinations included tests for complete blood count, liver function, erythrocyte sedimentation rate, C-reactive protein, autoantibody, rheumatoid immune antibody, syphilis antibodies, human immunodeficiency virus, herpes simplex virus 1 and hepatitis B virus. All results were within normal range. Immune complexes and tuberculosis were not detected.
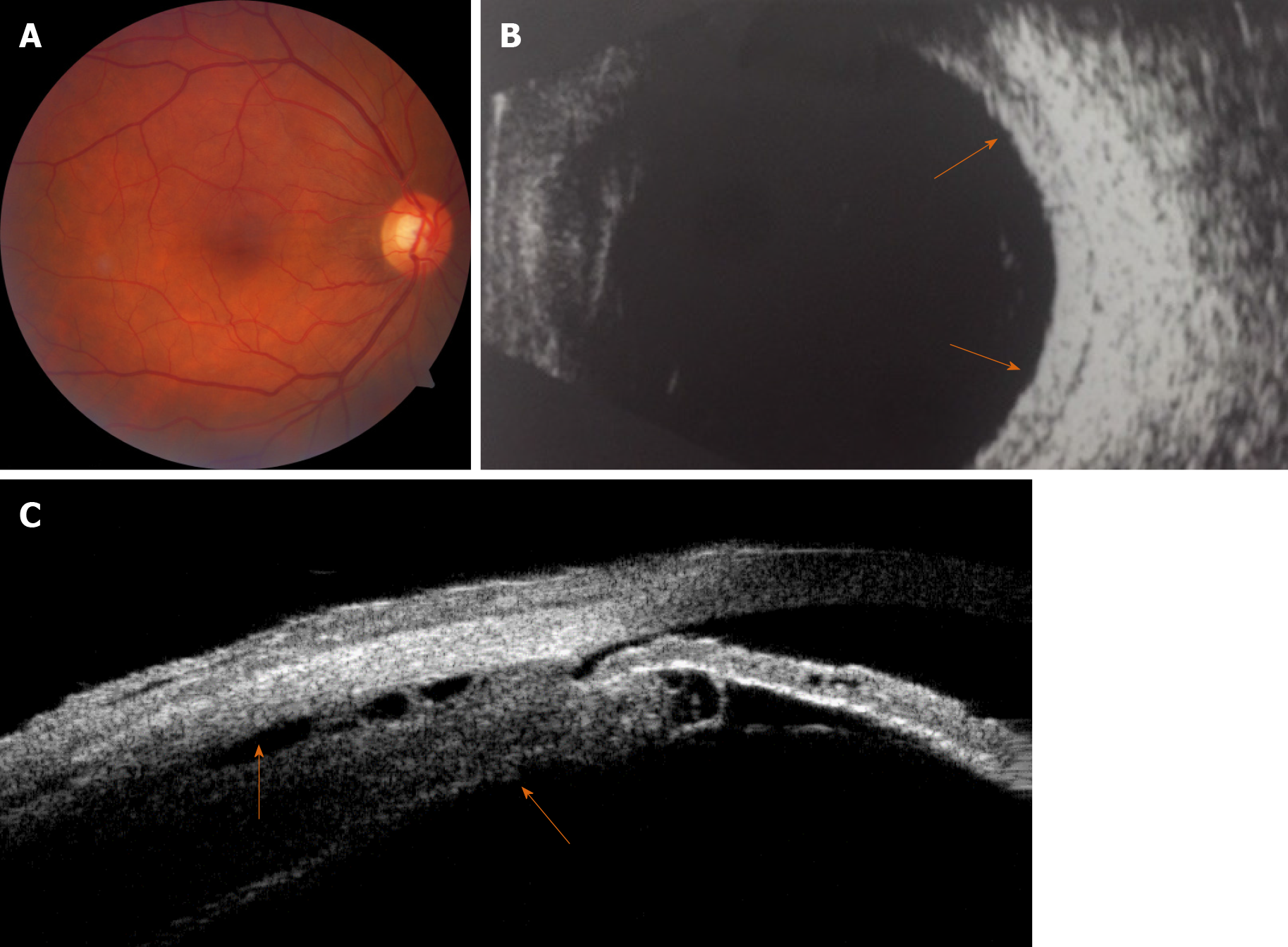
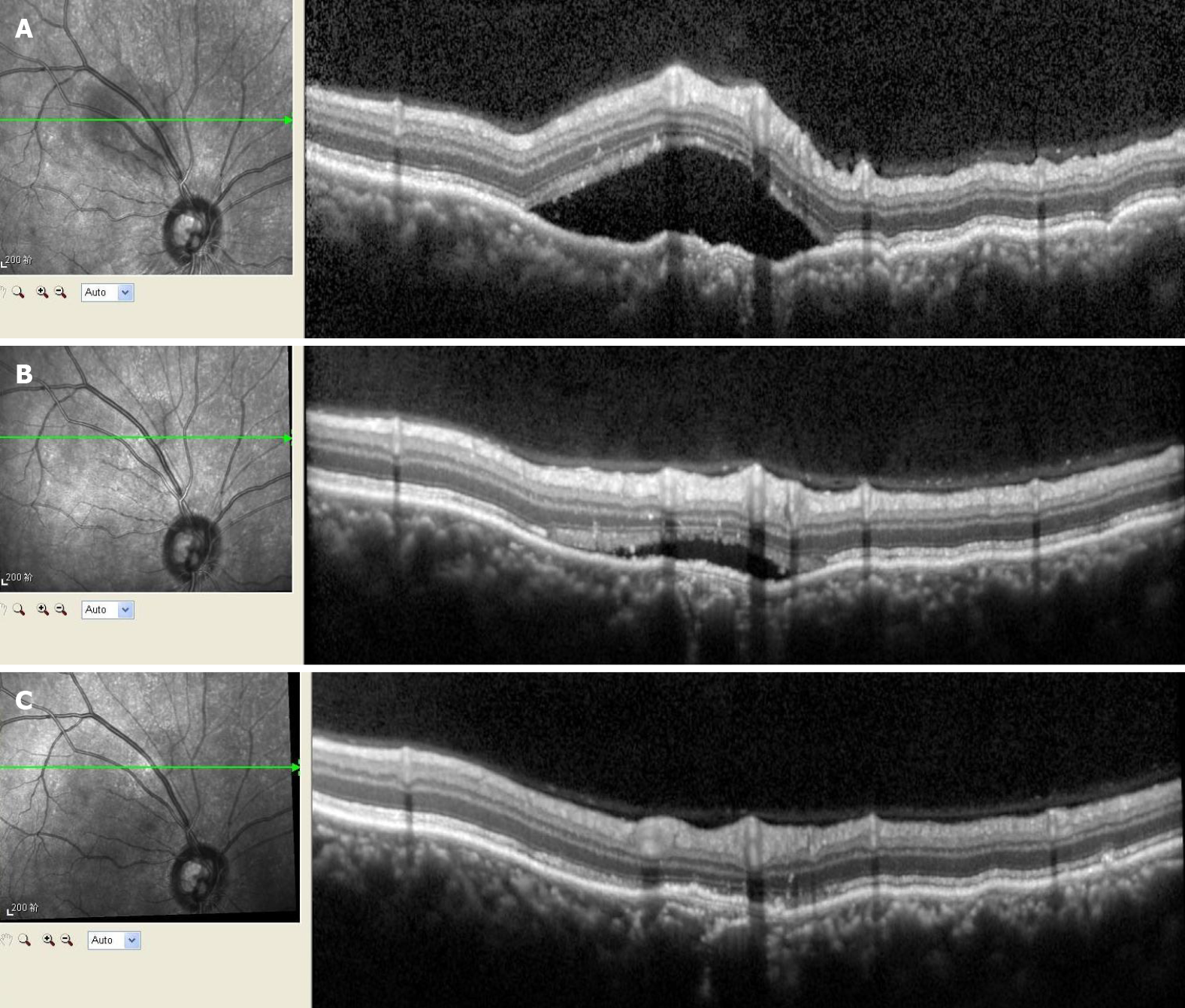
Fundus photography revealed retinal folds around the optic disk in the right eye (Figure 1A). B-scan ultrasonography revealed increased scleral thickening, with no 'T' sign (Figure 1B). Optical coherence tomography (OCT) showed the neuroepithelial layer to be raised and wrinkled, with fluid underneath it and above the temporal part of the optic disc (Figure 2A). Ultrasound biomicroscopy revealed edema and detachment of the ciliary body (Figure 1C).
Posterior scleritis.
The patient was given oral methylprednisolone (70 mg/d) on a gradual reduction schedule. To hinder the common side effects of methylprednisolone (i.e., electrolyte imbalance, gastric ulcer, osteoporosis), calcium tablet, potassium chloride tablet and omeprazole (20 mg/d) were prescribed. Tobramycin/dexamethasone ointment (before sleep) and non-steroidal anti-inflammatory eye drops (5 times/d) were prescribed as well. The treatment-induced relief of the redness and pain remained stable until the methylprednisolone was reduced to 30 mg/d. At that point, a compound betamethasone injection was administered into the bulb of the right eye. At 2 d later, the redness and pain became relieved again and finally the methylprednisolone was able to be reduced to zero.
As of the writing of this manuscript, the patient attends weekly follow-up visits and his right visual acuity has improved to normal. The retinal folds around the optic disk have been alleviated and OCT examination shows the subretinal fluid near the optic disc to be completely absorbed (Figure 2B and C).
The clinical signs of posterior scleritis may include concurrent ciliary or conjunctival congestion, anterior uveitis, retinal striae, disc swelling, serous detachment of the retina and limitation of extraocular motility[2]. Thus, diagnosis remans a challenge, more so because of the limited diagnostic modalities available. A variety of other etiologies for the common symptom of eye redness, such as episcleritis, conjunctivitis, blepharitis, anterior uveitis and keratoconjunctivitis sicca, must be considered in the differential diagnosis of scleritis[9]. In 2016, Mallick et al[10] reported on a 14-year-old male child who presented with eye redness and decreased vision, and was subsequently misdiagnosed with viral conjunctivitis. The authors described their finding of increased scleral thickening and the characteristic 'T' sign through B-scan ultrasonography in both eyes of this patient. Baltinas et al[11] also reported a case of infective conjunctivitis progressing to posterior scleritis in 2019. Ugurbas et al[12] in 2012 described a 29-year-old male diagnosed as posterior scleritis presenting with angle closure glaucoma and transient myopia who was suffering severe pain and vision loss in his right eye.
The patient in our case was misdiagnosed at a local hospital and incorrectly treated for acute conjunctivitis for 1 wk prior to presentation to our clinic. However, we also mistook the case for acute conjunctivitis, according to our observation of the obvious reddened right eye. It was not until the patient’s symptoms persisted despite our care that we performed further investigation and discovered the shallow anterior chamber in the eye. We infer that the increased scleral thickening may lead to crowded intraocular structures, pushing the iris and lens forward and ultimately decreasing anterior chamber volume. It was our detailed and varied imaging investigations (ultrasound biomicroscopy, B-scan ultrasonography, and OCT) that allowed us to make the correct diagnosis of posterior scleritis. In 2016, Duman et al[13] also described a similar case of a child with bilateral posterior scleritis, who had been misdiagnosed with conjunctivitis and uveitis 1 mo previous. Therefore, it is very important to distinguish posterior scleritis from other causes of red-eye, which can avoid delayed treatment.
Our patient was given methylprednisolone orally, on a taper-to-zero schedule. He currently attends weekly follow-up and his right visual acuity, eye pain and red-eye were improved after therapy for 2 mo. Accordingly, we advise accessory examinations, such as B-scan ultrasonography or OCT, should be conducted in the early stage of the disease to make an accurate diagnosis and institute appropriate treatment as early as possible. It is very important to make differential diagnosis in the case of eye pain and redness because of the non-specific clinical features of posterior scleritis and the threat of loss of vision.
Posterior scleritis should be among the differential diagnosis of eye pain and redness, and diagnosis requires further ophthalmic accessory examination, such as by optical coherence tomography.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Velázquez-Soto H S-Editor: Yan JP L-Editor: A P-Editor: Wu YXJ
| 1. | Bin Ismail MA, Lim RHF, Fang HM, Wong EPY, Ling HS, Lim WK, Teoh SC, Agrawal R. Ocular Autoimmune Systemic Inflammatory Infectious Study (OASIS)-report 4: analysis and outcome of scleritis in an East Asian population. J Ophthalmic Inflamm Infect. 2017;7:6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 2. | Kellar JZ, Taylor BT. Posterior Scleritis with Inflammatory Retinal Detachment. West J Emerg Med. 2015;16:1175-1176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kumar A, Ghose A, Biswas J, Majumder PD. Clinical profile of patients with posterior scleritis: A report from Eastern India. Indian J Ophthalmol. 2018;66:1109-1112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Calthorpe CM, Watson PG, McCartney AC. Posterior scleritis: a clinical and histological survey. Eye (Lond). 1988;2 (Pt 3):267-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 65] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Chapelle AC, Blaise P, Rakic JM. [Posterior scleritis]. Rev Med Liege. 2016;71:324-327. [PubMed] [Cited in This Article: ] |
| 6. | Dong ZZ, Gan YF, Zhang YN, Zhang Y, Li J, Zheng HH. The clinical features of posterior scleritis with serous retinal detachment: a retrospective clinical analysis. Int J Ophthalmol. 2019;12:1151-1157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Sin PY, Liu DT, Young AL. Nodular Posterior Scleritis Mimicking Choroidal Tumor in a Patient With Systemic Lupus Erythematous: A Case Report and Literature Review. Asia Pac J Ophthalmol. 5:324-329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Alsharif HM, Al-Dahmash SA. Atypical posterior scleritis mimicking choroidal melanoma. Saudi Med J. 2018;39:514-518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Galor A, Thorne JE. Scleritis and peripheral ulcerative keratitis. Rheum Dis Clin North Am. 2007;33:835-854, vii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Mallick J, Pujahari S, Maharana PK. Posterior scleritis presenting as conjunctivitis in a child. BMJ Case Rep. 2016;2016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Baltinas J, Weaver T, McCluskey P, Zagora S. Infective conjunctivitis progressing to posterior scleritis. Clin Exp Ophthalmol. 2019;47:795-796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Ugurbas SH, Alpay A, Ugurbas SC. Posterior scleritis presenting with angle closure glaucoma. Ocul Immunol Inflamm. 2012;20:218-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Duman R, Duman R, İnan S, Doğan M. Imitator of the conjunctivitis: Bilateral posterior scleritis in a child patient. Austin J Clin Ophthalmol. 2016;3:1069. [Cited in This Article: ] |