Published online Jan 16, 2014. doi: 10.12998/wjcc.v2.i1.5
Revised: December 21, 2013
Accepted: January 6, 2014
Published online: January 16, 2014
Inflammatory pseudo-tumour (IPT) of the liver is a rare condition with the appearance of a tumour-like space occupying lesion. Aetiology and natural history is not known for these benign lesions, as they are commonly diagnosed as malignant lesions and frequently undergo surgical resection since spontaneous resolution is very rare. Multifocal IPT involving both lobes of liver are rarely reported. Here we report a unique case of multifocal IPT of the liver which resolved spontaneously within 5 wk period.
Core tip: Inflammatory pseudo-tumour (IPT) is extremely rare pre-operative diagnosis. It’s a benign condition which does not require surgical management and it rarely self resolves. Our case so unique in appearance that IPT generally are solitary and if multiple generally confined on lobe of liver. In our case this tumour mimicked metastasis and presented in bilobar presentation. It resolved in 5 wk something which is never reported in medical literature.
- Citation: Puri Y, Lytras D, Luong TV, Fusai GK. Rare presentation of self-resolving multifocal inflammatory pseudo-tumour of liver. World J Clin Cases 2014; 2(1): 5-8
- URL: https://www.wjgnet.com/2307-8960/full/v2/i1/5.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i1.5
Inflammatory pseudo-tumours (IPTS) represent a challenging clinico-pathologic entity due to their similarity with malignant lesions. Histo-pathologically these tumours are inflammatory myofibroblastic tumours or plasma cell granulomas. They were initially observed in the lung by Brunn et al in 1939, and subsequently in the liver by Pack et al[1] in 1953. Although in the liver they may rarely lead to biliary obstruction, portal hypertension and even cirrhosis, their clinical importance is primarily related to the difficult differential diagnosis from malignant tumours[2]. For this reason the main pattern of diagnosis is on post-resection histopathological processing. However, spontaneous resolution of these lesions has been reported as well. Here we present a case of multifocal liver IPT, which spontaneously resolved without any type of therapeutic intervention.
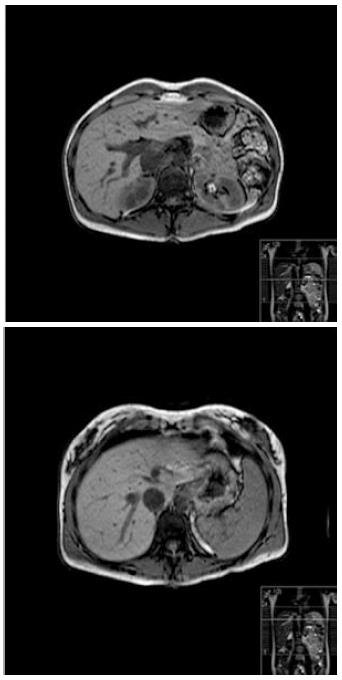
A 37-year-old Caucasian female was referred to our tertiary hepatopancreatobiliary surgical unit with symptoms of weight loss and malaise since one month. There are no pre-existing medical co-morbidities. Bloods results showed derangement of liver function tests with alkaline phosphatase of 174 U/L (normal range: 38-126), aspartate transaminase of 40 U/L (9-36), alanine transaminase of 43 U/L (10-28), and normal bilirubin. Regarding inflammatory markers only erythrocyte sedimentation rate was raised at 58 mm/h (2-12). Abdominal ultrasound revealed multiple bilobar lesions in the liver with maximum size of 3.5 cm adjacent to the porta hepatis. Multiditector computed tomography with a liver protocol demonstrated 5 lesions, non-enhancing and of low attenuation highly suspicious of metastatic origin (Figure 1). According to decision of the multidisciplinary team meeting, the patient was considered harbouring metastatic diseases of unknown primary and she underwent detailed investigations with upper gastrointestinal endoscopy, positron emission tomography (PET) scan, mammography, chest computed tomography scan and tumour markers as well. Apart from an abnormal uptake in the right lobe of the liver on PET scan there was no pathology revealed in any other study.
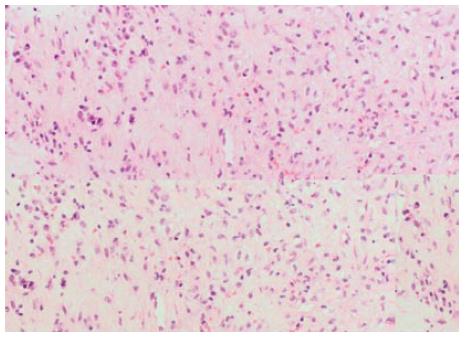
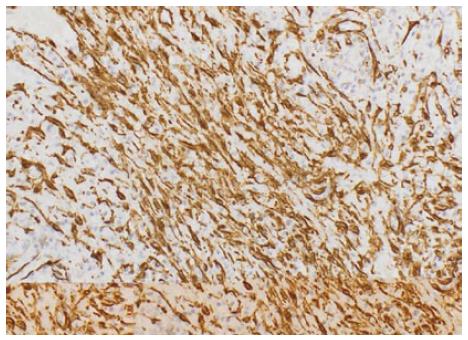
After failure in locating the primary, a percutaneous biopsy of a liver lesion was decided as next step in the diagnostic workup. Histopathology revealed a parenchyma of normal architecture but replaced by collagenous stroma admixed with inflammation. The stroma was composed of dense areas of fibrosis, myofibroblasts and fibroblasts. The inflammation consisted of a mixture of plasma cells, lymphocytes and eosinophils. Aggregates of xanthomatoushistiocytes were also seen. There was mild portal inflammation. Also few epithelioid granulomas were seen. Immunohistochemistry showed positivity of the spindle cells for smooth muscle actin and negativity for ALK-1 (Figures 2 and 3). Epstein barr virus and cytomegalovirus immunostains were negative as well. Ziel-Neelsan showed no evidence of acid-fast bacilli in specimen. The tissue sample was considered as highly suggestive of inflammatory pseudo-tumour.
Based on the existed evidence and according to patient’s consent, a wait and watch policy with follow-up imaging in 3 wk was decided. Magnetic resonance imaging (MRI) demonstrated significant reduction in the size of all liver lesions, measuring a maximum diameter of 1.5 cm as compared to the previous 3.5 cm. Follow-up MRI at two months showed almost complete resolution of the lesions. She was put on annual follow up with liver MRI and she remains asymptomatic and without evidence of any lesions on 2 year follow-up (Figure 4).
An IPT is a benign, tumour like lesion characterised by presence of certain chronic inflammatory cells namely plasma cells, lymphocytes and eosinophils. Although uncommon in presentation, they represent a challenge in differential diagnosis since they might lead to unnecessary surgical interventions if they are interpreted as malignant disease[3].
Their aetiology remains unclear. IPTs are known to be associated with chronic inflammatory conditions like Crohn’s disease[4], autoimmune disorders related to IgG4[5] or infective agents like Escherichia coli[6]. The main location in the liver is the right lobe but multifocal IPTs although extremely rare have been described as well[7]. In the present case, there was multifocal, bi-lobar distribution of these lesions while there was no association with any chronic condition. This is first of its kind case report from our unit who performs around 100 liver resections per year.
Diagnosis of IPT is considered quite difficult since the radiological features of these tumours are often mistaken as of malignant origin[1,8]. Definitive diagnosis is only possible following fine needle aspiration cytology or core biopsy[9]. Histologically, these tumours appear as densely hyalinised structures with dense collagen matrix and a whorl like pattern infiltrated by chronic inflammatory cells[10]. Similar histological pattern was observed in the present case.
Natural history of IPT is not well defined since the current evidence is mainly after an incidental radiological diagnosis which often leads to surgical resection. However complete spontaneous resolution of these lesions has been also observed within months[10]. Raised values of tumour markers as CA19-9 might confuse further the final diagnosis, but this was not observed in our case.
In conclusion, IPT might represent a considerable diagnostic challenge requiring high index of suspicion. The characteristic of spontaneous resolution highlights the necessity of regular, short-term, imaging follow-up in order to avoid aggressive unnecessary interventions.
A 37-years-old female without any medical co morbidities presented with short term history of weight loss and malaise and diagnosed with multiple liver lesions.
Multiple liver lesions.
Metastatic disease in liver, multifocal hepatocellular carcinoma, inflammatory pseudotumour.
Bloods results showed derangement of liver function tests with alkaline phosphatase of 174 U/L (normal range: 38-126), aspartate transaminase of 40 U/L (9-36), alanine transaminase of 43 U/L (10-28), and normal Bilirubin. Erythrocyte sedimentation rate was raised at 58 mm/h (2-12). Other blood tests including tumour were normal.
Multiditector computed tomography with a liver protocol demonstrated 5 lesions, non-enhancing and of low attenuation highly suspicious of metastatic origin.
Histopathology revealed a parenchyma of normal architecture but replaced by collagenous stroma admixed with inflammation. The stroma was composed of dense areas of fibrosis, myofibroblasts and fibroblasts. Immunohistochemistry showed positivity of the spindle cells for smooth muscle actin.
This patient did not require any treatment as inflammatory pseudo-tumour self-resolved completely and patient was completely asymptomatic even at 2 years follow up.
There are very case reports of this particular condition but these lesions are more frequently diagnosed because of routine use of cross sectional imaging. It is important to be aware of this particular condition to spare patient of major surgical procedure.
The biology pathophysiology and disease history of this particular condition is not completely known. This case report highlights importance of serial radiological examinations and unique place of fine-needle aspiration cytology in diagnosis of inflammatory pseudo tumours.
This is a brief, easy to read and interesting case report in which the authors show a patient with a usual clinical presentation.
P- Reviewers: Ong HT, Velayos B S- Editor: Cui XM L- Editor: A E- Editor: Wang CH
| 1. | PACK GT, BAKER HW. Total right hepatic lobectomy; report of a case. Ann Surg. 1953;138:253-258. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Papachristou GI, Wu T, Marsh W, Plevy SE. Inflammatory pseudotumor of the liver associated with Crohn’s disease. J Clin Gastroenterol. 2004;38:818-822. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Yamaguchi J, Sakamoto Y, Sano T, Shimada K, Kosuge T. Spontaneous regression of inflammatory pseudotumor of the liver: report of three cases. Surg Today. 2007;37:525-529. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Amankonah TD, Strom CB, Vierling JM, Petrovic LM. Inflammatory pseudotumor of the liver as the first manifestation of Crohn’s disease. Am J Gastroenterol. 2001;96:2520-2522. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Agaimy A, Märkl B. Inflammatory angiomyolipoma of the liver: an unusual case suggesting relationship to IgG4-related pseudotumor. Int J Clin Exp Pathol. 2013;6:771-779. [PubMed] [Cited in This Article: ] |
| 6. | Kim YW, Lee JG, Kim KS, Yoon DS, Lee WJ, Kim BR, Shin EA, Park YN, Choi JS. Inflammatory pseudotumor of the liver treated by hepatic resection: a case report. Yonsei Med J. 2006;47:140-143. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Mortelé KJ, Wiesner W, de Hemptinne B, Elewaut A, Praet M, Ros PR. Multifocal inflammatory pseudotumor of the liver: dynamic gadolinium-enhanced, ferumoxides-enhanced, and mangafodipir trisodium-enhanced MR imaging findings. Eur Radiol. 2002;12:304-308. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Schmid A, Jänig D, Bohuszlavizki A, Henne-Bruns D. Inflammatory pseudotumor of the liver presenting as incidentaloma: report of a case and review of the literature. Hepatogastroenterology. 1996;43:1009-1014. [PubMed] [Cited in This Article: ] |
| 9. | Sari A, Tunakan M, Ünsal B, Ekıncı N, Rezanko T, Elçın F, Aydoğdu Z. Inflammatory pseudotumor of the liver diagnosed by needle biopsy: report of three cases (one with neuroendocrine tumor of the rectum and lung). Turk J Gastroenterol. 2010;21:308-312. [PubMed] [Cited in This Article: ] |
| 10. | Rosa B, Moutinho-Ribeiro P, Pereira JM, Fonseca D, Lopes J, Amendoeira I, Cotter J. Ghost tumor: an inflammatory pseudotumor of the liver. Gastroenterol Hepatol (N Y). 2012;8:630-633. [PubMed] [Cited in This Article: ] |