Published online May 26, 2024. doi: 10.12998/wjcc.v12.i15.2487
Revised: March 14, 2024
Accepted: April 9, 2024
Published online: May 26, 2024
Fracture of the lateral process of the talus (FLPT) is uncommon in clinical practice and can be easily missed or misdiagnosed. In recent years, as researchers from all over the world have further deepened their research on FLPT, there has been a breakthrough in the classification, and the methods and principles of clinical management have changed accordingly; however, there is still no standardized guideline for the diagnosis and management of FLPT, and there have been few relevant literature review articles related to this kind of fracture in the past at least 5 years. In this article, we review the clinical classification, classification-based therapeutic recommendations, and prognosis of FLPT, with the aim of providing a reference for the clinical diagnosis and management of this infrequent fracture.
Core Tip: To our knowledge, there are no standardized guidelines for the diagnosis and management of fracture of the lateral process of the talus (FLPT). Furthermore, no relevant review articles have been published in the past 5 years. Recently, there is some new progress in classification and management recommendations of FLPT; conse
- Citation: Wang CQ, Stöckle U, Dong SN, Li XG, Ling ZX. Management and classification of the fracture of lateral process of talus: An overview and literature update. World J Clin Cases 2024; 12(15): 2487-2498
- URL: https://www.wjgnet.com/2307-8960/full/v12/i15/2487.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i15.2487
Fracture of the lateral process of the talus (FLPT) accounts for less than 0.1% of all fractures and less than 10% of foot fractures[1]. It constitutes 10%-25% of all talar fractures[2] and ranks second only to talar neck fractures. The mechanisms underlying FLPT injury remain inconclusive. However, current literature suggests that forced dorsiflexion, inversion, eversion, and potential external rotation of the foot are all contributing factors[3-5]. Notably, during snowboarding, the motion and stress status of the foot becomes more complicated, increasing the risk of FLPT by approximately 17-fold[2,6-8], with FLPT accounting for 15% of all snowboarding-related ankle injuries and 34% of all snowboarding-related ankle fractures[2], also known as “snowboarders ankle” or “snowboarders fracture”, respectively. Although FLPT is the second most common type of talar fracture, clinical cases are rare, especially for isolated FLPT[9-11]. The first description of FLPT was published by Marotolli in 1943[12]; however, until now, the relevant research literature remains limited, mostly comprising case reports and lacking clinical research with a large sample size; therefore, there is still no consensus on the standardized management of FLPT. Herein, we conducted a literature review on the clinical classification, management, and prognosis of FLPT to provide a credible reference for the clinical diagnosis and management of FLPT.
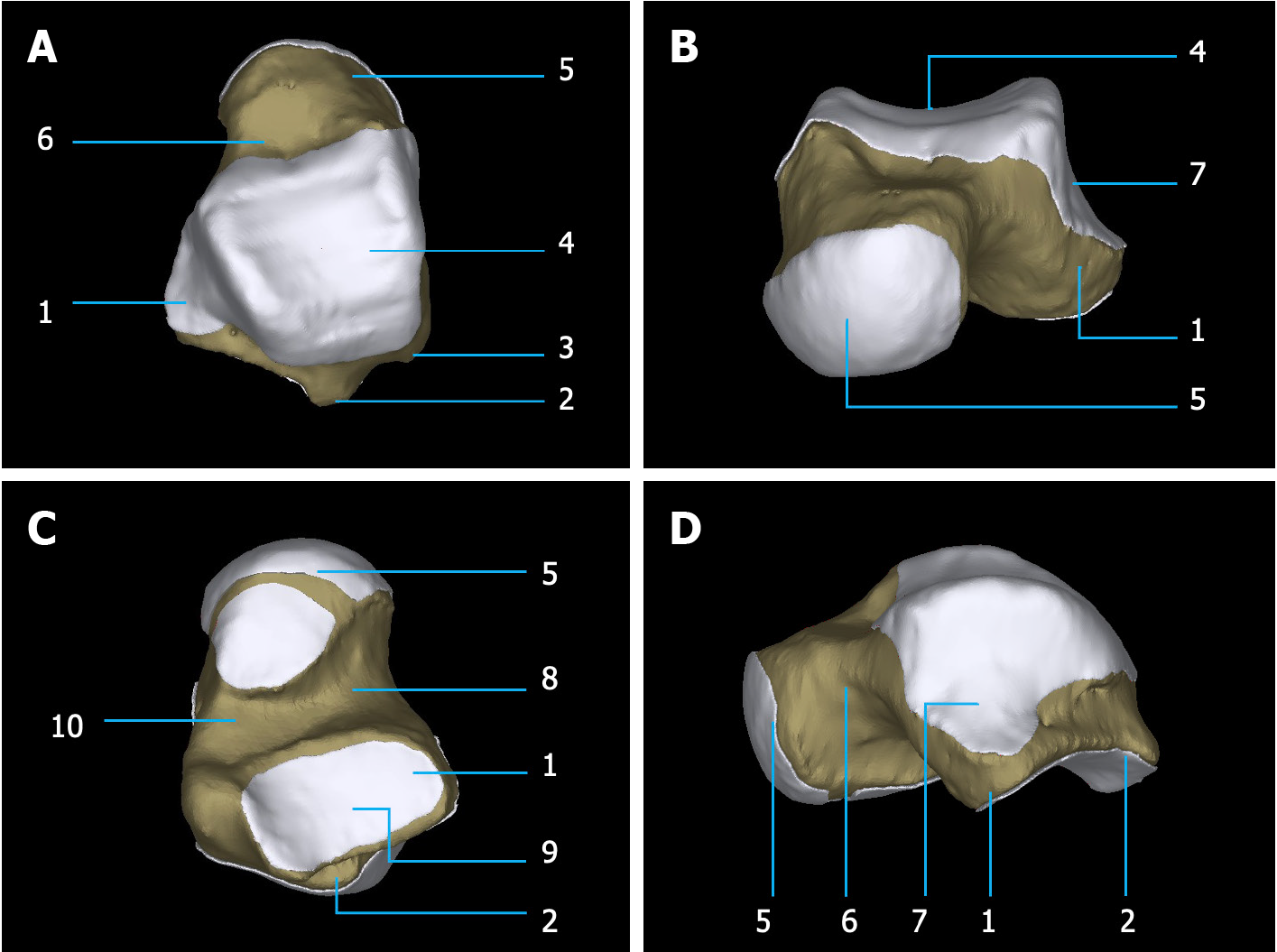
The talus is the most superior bone of the foot and sits on top of and is supported by the calcaneus[13]. It articulates with the calcaneus and three separate subtalar articular surfaces, making it the second largest tarsal bone. Serving as an osseous link between the leg and foot, approximately two-thirds of the talar surface is covered by articular cartilage, with few muscle or tendon origins or insertions, and it plays an important role in ankle motion[14]. The talus can be divided into three main parts as follows (Figure 1 and Video): The talar head, neck, and body, resembling a snail in the lateral view. The body of the talus has two projections-the posterior and lateral talar processes. The lateral process of the talus extends from the lateral surface of the talar body and is a wedge-shaped protuberance formed by the posterior part of the posterior subtalar articular surface toward the lateral side. It has two main articular cartilage surfaces, forming an articulation with the distal fibula at its lateral superior part and constitutes the outermost part of the posterior subtalar articulation at the underside. The lateral talocalcanean ligament originates at the tip of the lateral talar process. Therefore, FLPT is usually accompanied by damage to the articular cartilage or ligaments related to the subtalar and talofibular joints. Consequently, if missed, delayed, or improperly treated, FLPT may result in malunion or nonunion, which may subsequently lead to posttraumatic arthritis and instability of the subtalar joint. Therefore, one must pay close attention to any suspected FLPT, as well as ensure timely and accurate diagnosis and formulate appropriate treatment plans.
The definitive mechanism of injury in the FLPT is currently inconclusive, and according to existing research results, dorsiflexion, inversion, eversion, external rotation, and axial impaction are all causative factors[3-5]. Hawkins[15] and Fjeldborg[16] suggested that FLPT is caused by forced dorsiflexion combined with foot inversion; this mechanism of injury has been confirmed in several subsequent studies[17]. Some epidemiological studies on snowboarding injuries have suggested that the occurrence of foot and ankle injuries in this sport is associated with the complexity of specialized movements and the use of old soft-shell boots by athletes[18-20]. Although the mechanism of FLPT has not been clearly stated in these epidemiological studies, the athletes diagnosed with FLPT engaged in jumping and performing various difficult maneuvers in the air, leading to forced dorsiflexion and inversion upon landing, possibly contributing to the development of FLPT[21]. Cadaveric biomechanical experiments by Tinner and Sommer[1] showed that dorsiflexion of the foot, combined with eversion or external rotation, can also lead to FLPT. Jin et al[22] reported two cases of FLPT combined with rupture of the medial malleolar deltoid ligament, indirectly proving that eversion or external rotation violence encountered by the foot may also be a causative factor for FLPT. Other clinical studies and vitro biomechanical experiments have shown that FLPT is associated with dorsiflexion, axial impaction, eversion, and external rotation of the foot[5,22]. The authors believe that the causative factors of FLPT are diverse and that different types and intensities of injury violence may lead to significant differences in the fracture site, fragment size, degree of comminution, and displacement. For instance, according to the McCrory-Bladin classification, the mechanism of injury for type 2 and type 3 fractures is concomitant axial impaction violence associated with dorsiflexion and inversion of the foot during landing from a height, whereas type 1 fractures are due to dorsiflexion and inversion violence only. However, attention should be paid to establishing a timely and accurate diagnosis to avoid delays in management due to missed diagnoses, rather than on the correspondence between the mechanism of injury and fracture characteristics.
In 1965, Hawkins[15] summarized three main fracture patterns by analyzing the radiographic features of 13 FLPT cases (Figure 2).
Hawkins type 1: A simple fracture of the lateral talar process, with the fracture line extending downward from the talofibular joint surface to the posterior talofibular joint surface; this type of fracture is easily diagnosed on radiographs.
Hawkins type 2: Comminuted fracture of the entire lateral talar process with fracture lines involving both the talofibular and posterior subtalar joint surfaces.
Hawkins type 3: Chip fracture of the anterior-inferior portion of the posterior half of the lateral talar process, which can be visualized only on lateral radiographs. The fracture is located in the region of the tarsal sinus and involves only a small portion of the posterior subtalar joint, without any damage to the talofibular articular surface.
Hawkins[15] recommended that, regardless of the classification, closed reduction should be attempted first by placing the foot in a neutral or everted position and then palpating and manipulating the lateral talus process into an acceptable position under radiography. For Hawkins type 2 and type 3 fractures, as well as type 1 fractures with satisfactory closed reduction, conservative treatment is recommended by immobilizing the foot in a short-leg plaster cast in a neutral position without weight-bearing for 4 wk, and weight-bearing with the maintenance of the plaster cast is allowed in the next 2 wk. For Hawkins type 1 fractures in which displacement of the fractured fragment remains unsatisfactory after attempted closed reduction, both Hawkins[15] and Dimon[23] recommended surgical treatment with open reduction and internal fixation (ORIF). Subsequently, fragment resection or subtalar joint fusion could be considered if complications such as nonunion, malunion, and overgrowth were confirmed after ORIF. From our perspective, Hawkins' management recommendations, which are limited by the relatively backward medical level and conditions at the time, have limited reference value for the current clinical management of FLPT.
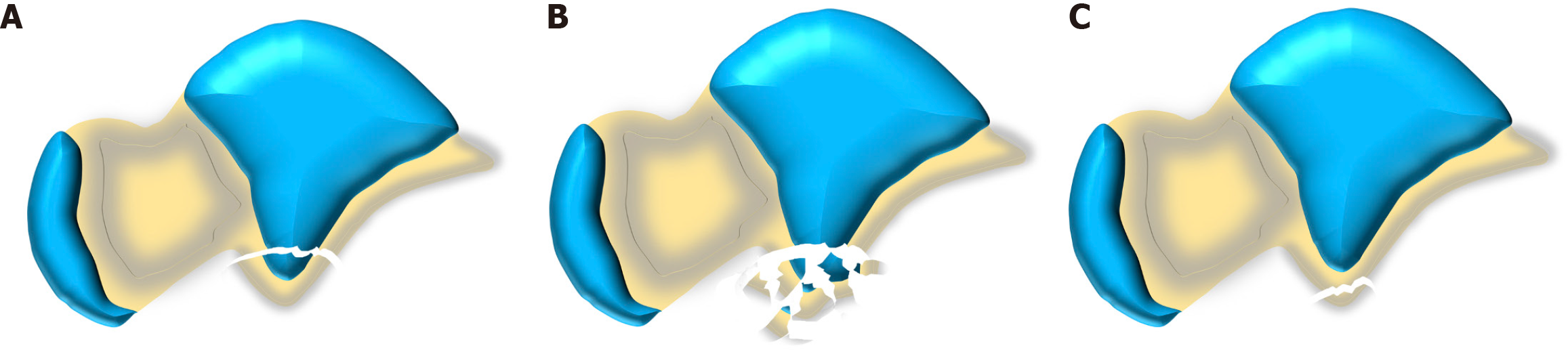
In 1996, in order to better reflect the relationship between fracture characteristics and mechanism of injury and subsequently to guide further managements, McCrory and Bladin[21] proposed a new classification of FLPT, also known as McCrory-Bladin classification (Figure 3).
McCrory-Bladin type 1: Chip fracture of the anterior-inferior portion of the lateral talar process, without any damage to the talofibular articular surface. This type corresponds to Hawkins type 3 fracture, which is also considered as the avulsion fracture of the anterior talofibular ligament.
McCrory-Bladin type 2: Simple fracture of the lateral talar process causing some damages to both the talofibular and subtalar articular surfaces. This type corresponds to Hawkins type 1 fracture; however, McCrory and Bladin[21] made some modifications by dividing it into two subtypes based on the displacement of the large fragment, defining an undisplaced fracture as type 2A and a displaced fracture as type 2B.
McCrory-Bladin type 3: Comminuted fracture of the entire lateral process with the involvement of both the talofibular and posterior subtalar articular surfaces. This corresponds to Hawkins type 2 fracture.
McCrory and Bladin[21] summarized some of the case reports and provided the following treatment recommendations. For flake fractures (Chip fracture, McCrory-Bladin type 1) and simple fractures with no or minimal displacement (< 2 mm, McCrory-Bladin type 2), satisfactory results can be achieved with a 6-wk short leg plaster cast immobilization, and partial weight bearing were also recommended during this period. For simple fractures with severe displacement (≥ 2 mm, McCrory-Bladin type 2), an ORIF should be used to reconstruct the integrality of articular surfaces. For comminuted FLPT (McCrory-Bladin type 3), surgical treatment becomes unavoidable, and the fracture should be anatomically reduced and solidly fixed if possible; if anatomical reduction cannot be achieved or the fracture is too comminuted to be fixed, resection of all comminuted fragments is recommended to prevent the development of posttraumatic subtalar osteoarthritis. McCrory and Bladin's recommendations for treatment, although summarized in only a few case reports available at the time, are still applicable nowadays. The McCrory-Bladin classification is the most widely used classification method for FLPT in clinical practice.
In 2004, Boack and Manegold[24] described a different classification that can be applied to fractures of both the lateral and posterior talar processes. The classification consists of four fracture types, each of which is divided into subtypes based on the severity of bone injury, degree of articular cartilage damage, and stability of the ligaments (Figure 4).
Boack's type 1: Chip fracture or avulsion fracture (< 0.5 cm). (1) 1a: An extra-articular fracture of the lateral talar process; (2) 1b: An isolated fracture of the medial tubercle of the posterior talar process; and (3) 1c: An intraarticular fracture of the lateral talar process;
Boack's type 2: Medium-sized fragment (0.5-1.0 cm) with varying degrees of displacement. (1) 2a: FLPT involving only the subtalar joint but not the talofibular joint; and (2) 2b: An isolated fracture of the lateral tuberosity of the posterior talar process.
Boack's type 3: A large fracture fragment (> 1.0 cm) with varying degrees of damage to both the ankle and subtalar joints. (1) 3a: A simple fracture of the lateral talar process, extending from the talofibular joint to the posterior surface of subtalar articulation; (2) 3b: Comminuted fracture of the entire lateral talar process; and (3) 3c: Comminuted fracture of the entire posterior talar process.
Boack's type 4: A severe fracture of either the lateral or posterior talar process combined with instability or luxation of the subtalar joint.
Boack and Manegold[24] recommended that conservative treatment is only indicated for Boack's type 1a FLPT with external immobilization in a short leg cast for 6 wk, during which time weight-bearing walking is allowed, whereas all FLPT involving damage to articular surfaces or with displacements should be treated surgically to reduce the risk of degenerative lesions in the subtalar joints. Type 1c FLPT can be treated arthroscopically with resection of the bony fragments, because even a small intraarticular fragment can damage the articular surface severely, leading to serious adverse outcomes. Although secondary subtalar osteoarthritis or instability after total resection of the lateral talar process has been reported[10], there have been no reports of these lesions occurring secondary to resection of free fragments of the lateral talar process. Arthroscopic evaluation of the extent of articular cartilage damage and fracture comminution is recommended for all Boack's type 2 FLPT, and the decision to perform arthroscopic resection of fragments or arthroscopic internal fixation is based on the results of the arthroscopic evaluation. Boack's type 3a FLPT is recommended to be managed by open or arthroscopic reduction because of the large size of the fracture fragments and their good integrity and subsequently fixed with one or two headless cannulated compression screws, which can avoid articular cartilage damage caused by the head of conventional screws and provide optimal results. The management of Boack's type 3b FLPT depends on the degree of comminution and the size of the fragments, and it is recommended to remove all the fracture fragments if the attempted ORIF fails. In Boack's type 4 FLPT with subtalar joint dislocation, approximately 50% of patients have severe concomitant articular cartilage damage. To manage these cases, Boack and Manegold[24] recommended that subtalar joint repositioning should be completed as soon as possible, along with the arthroscopic evaluation of cartilage damage and arthroscopic resection of fragments to minimize the possibility of sequelae.
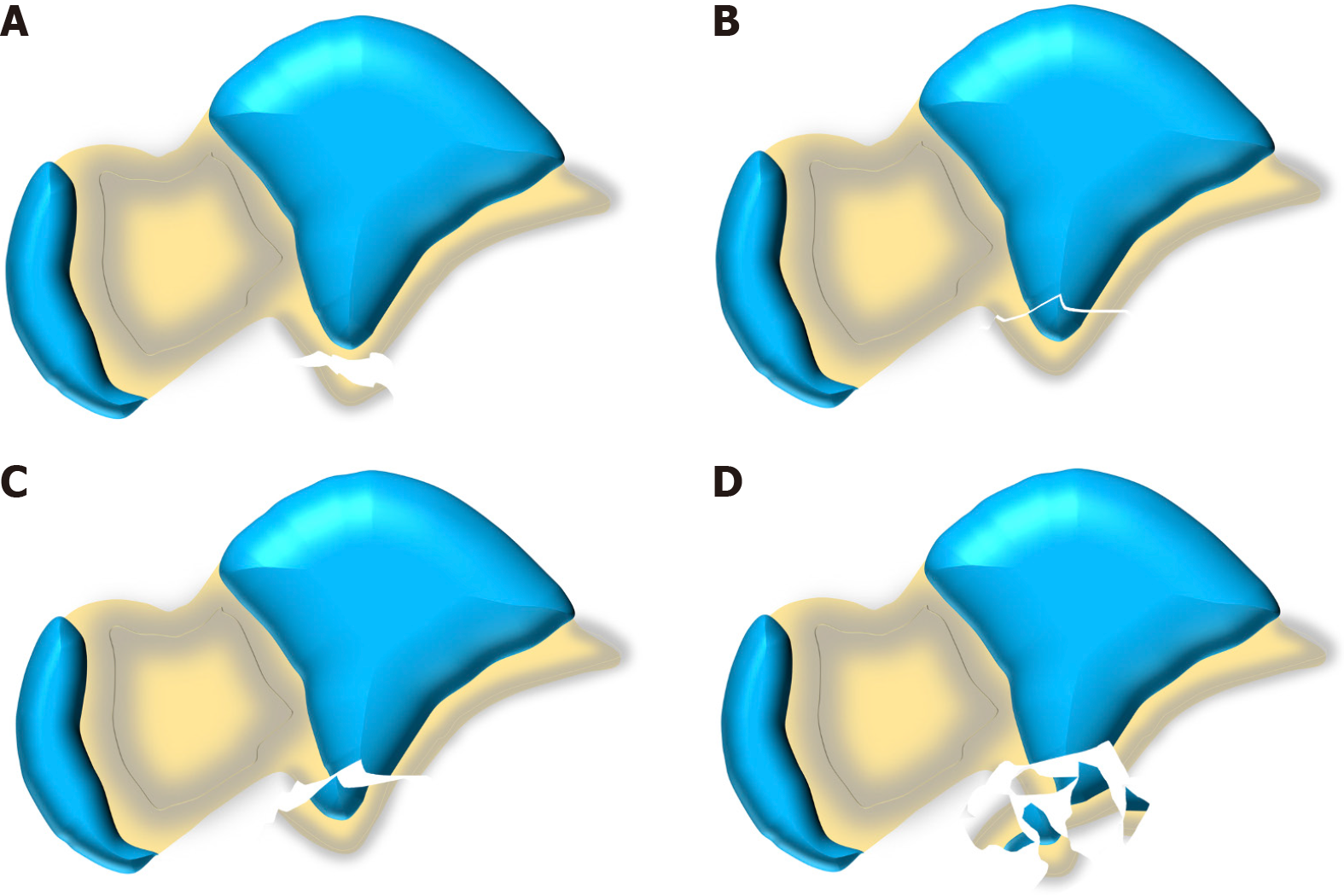
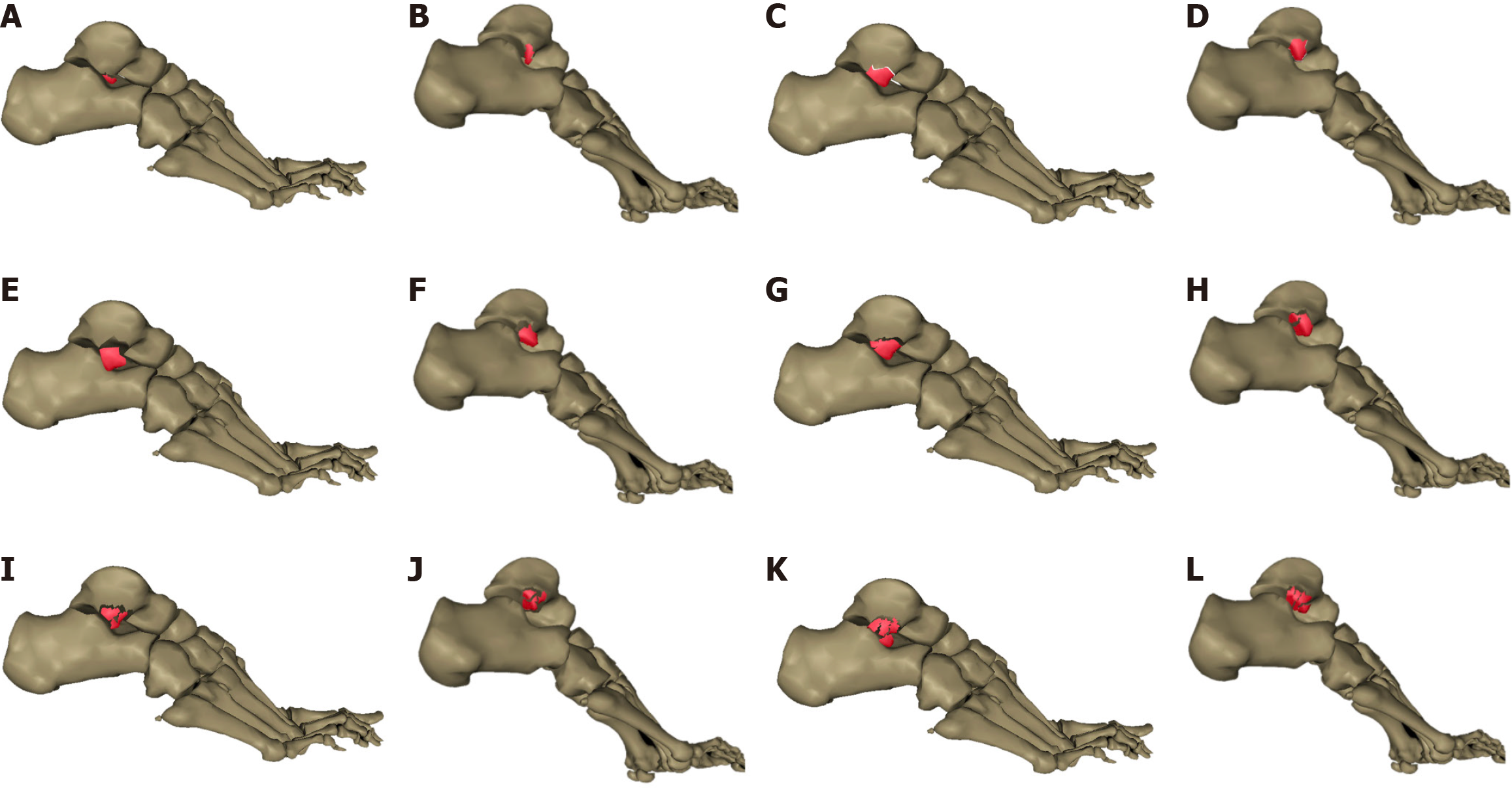
In 2018, Tinner and Sommer[1] as part of their study on FLPT, found that McCrory-Bladin type 1 FLPT cases are extremely rare, accounting for less than 5% of all FLPT cases. Moreover, McCrory-Bladin type 2 FLPT were considered to represent an ideal state because most of the large fragment fractures of the lateral talar process are usually not isolated; instead, they are often combined with at least one medium-sized fragment from the posterior subtalar articular facet, which was not severely comminuted, and therefore cannot be classified as McCrory-Bladin type 3 FLPT either. Consequently, they modified the McCrory-Bladin classification, with Tinner-Sommer types 1 and 2 FLPT remaining consistent with McCrory-Bladin types 1 and 2, whereas Tinner-Sommer type 3 was divided into three subtypes (Figure 5).
Type 3a: Simple fracture of the lateral talar process, with a medium-sized fragment originating from the posterior subtalar articular surface.
Type 3b: Comminution of the cranial metaphyseal bone of the lateral talar process based on the characteristics of type 3a fractures.
Type 3c: Nonreconstructable comminuted FLPT, corresponding to McCrory-Bladin type 3 fracture.
Although the Tinner-Sommer classification did not consider the displacement of fragments, it suggested that to better combine classification with management recommendations, the displacement of FLPT fragments should be evaluated before providing therapy. As a complement to the classification, they proposed their own criteria for evaluating the displacement of the fragments in FLPT as follows[1]: FLPT with an articular step of < 1 mm and a separation displacement of < 2 mm is defined as nondisplaced (or minimally displaced) fractures, whereas those with an articular surface step of ≥ 1 mm or a gap of ≥ 2 mm are defined as displaced FLPT.
According to the Tinner-Sommer classification[1], all FLPTs with no displacement or minimal displacement should be treated conservatively with cast or splint immobilization for at least 6 wk, during which partial weight bearing (< 10 kg) is allowed. For most Tinner-Sommer type 1 fractures, conservative management is recommended regardless of fracture displacement, whereas a small percentage of type 1 fractures combined with other injuries requiring surgical treatment, such as peroneal tendon slippage, can be managed surgically in conjunction with the surgical treatment of combined injuries, with either internal screw fixation or fragment resection, depending on the size of the fragments. Most of types 2 and 3 FLPT exhibit significant displacement and must be treated surgically. For type 2 and most type 3a FLPT, adequate bony connections can be formed between the major fragment and talar body after reduction, and fixation can be performed with one or two screws. In contrast, due to the presence of metaphyseal comminution in type 3b FLPT and a small percentage of type 3a fractures, the fragment did not have sufficient bone to hold screws; therefore, supportive fixation with a T-shaped osteoplate is recommended in such cases. Type 3c fractures are extremely comminuted, with no possibility of internal fixation, and resection of all fragments is recommended. In addition, compared with conservative treatment, surgical treatment offers the advantage of earlier postoperative articular function training. Therefore, the functional impairment of both the joint and muscle is significantly less than that of cast immobilization, which is especially important for young athletes who need to return to the arena as early as possible.
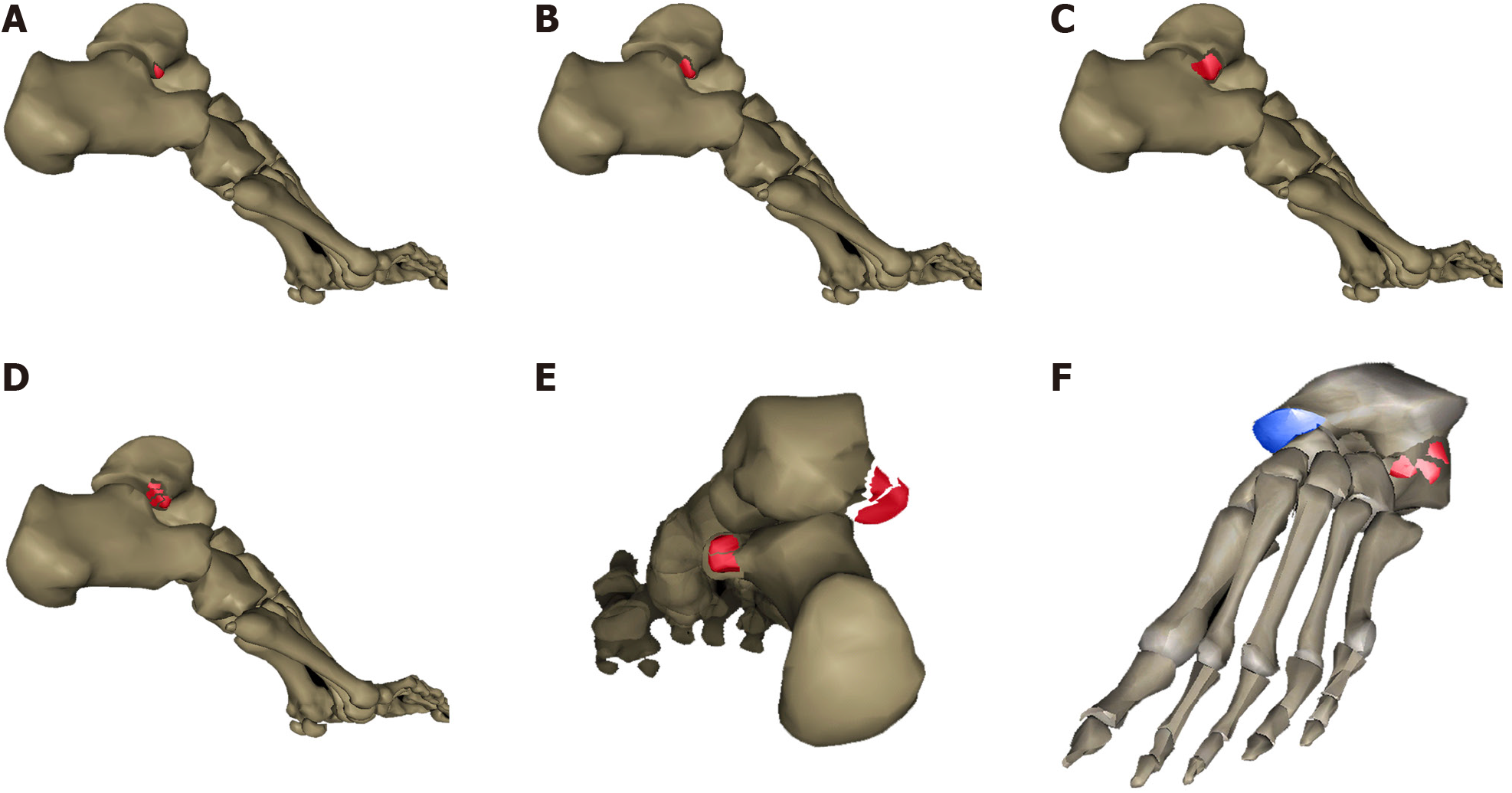
Wijers et al[25] noticed that a few FLPTs are combined with injuries to the sustentaculum tali, which could be considered a prestage of a full-blown subtalar or peritalar dislocation. Accordingly, by analyzing coronal computed tomography (CT) scans, Wijers et al[25] modified Boack's classification based on the severity, intraarticular or extraarticular location of the fracture, and possible joint dislocations ranging from types 1A to 4B (Figure 6). Type 1A: Small fragment, extraarticular; Type 1B: Small fragment, intraarticular; Type 2: Intermediate fragment, intraarticular; Type 3: Comminuted or severe fracture, intraarticular; Type 4A: FLPT combined with a sustentaculum tali fracture of the calcaneus without joint dislocation; Type 4B: FLPT combined with subtalar or peritalar dislocation.
From Wijers’ viewpoint[25], type 1A FLPT as well as nondisplaced type 1B and type 2 FLPTs can be treated conservatively, whereas surgical treatment is recommended for all other fracture types. In addition, he emphasized that type 4B FLPTs require closed reduction of the talus in the emergency department due to concomitant total subtalar or peritalar luxation.
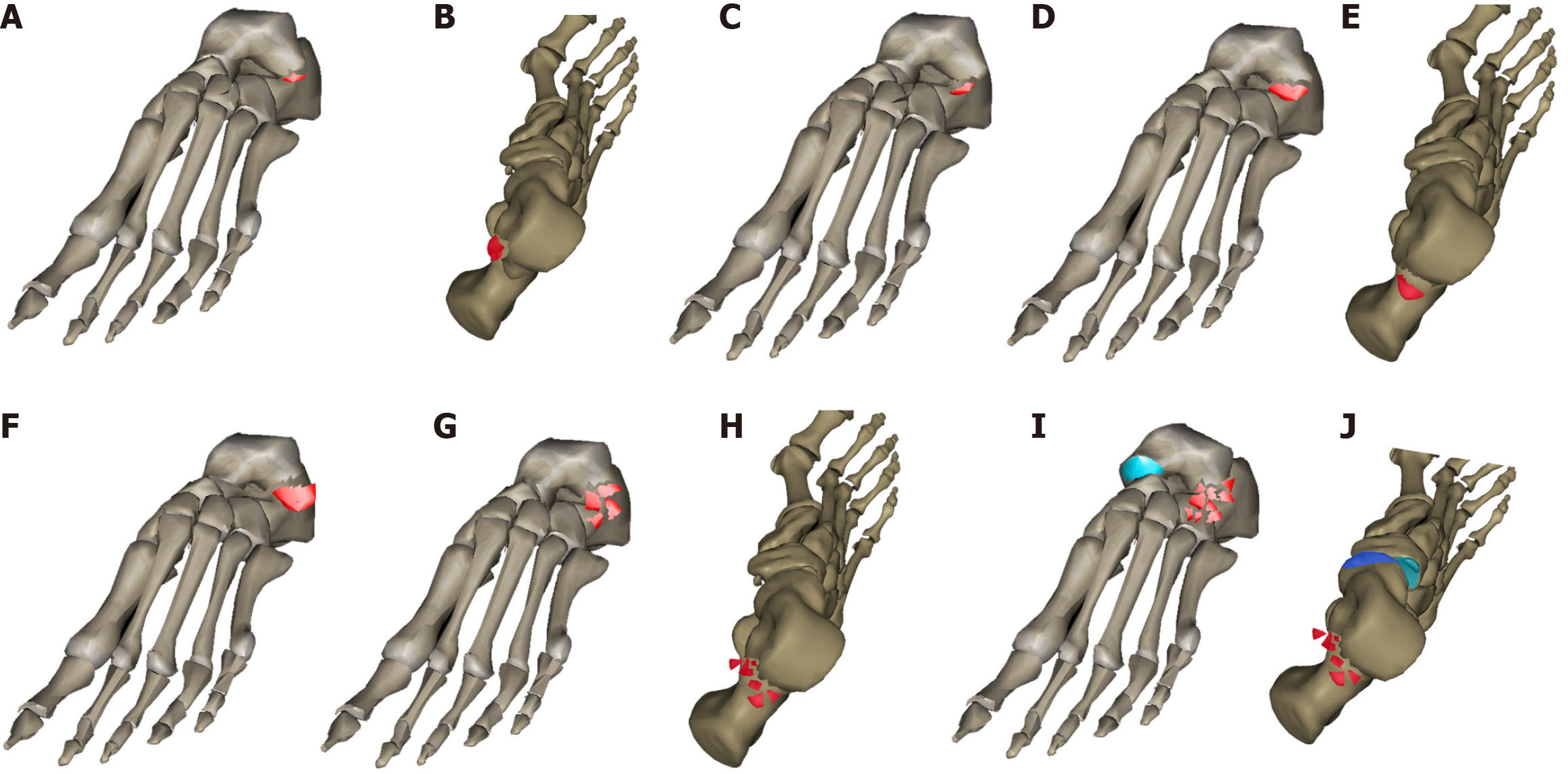
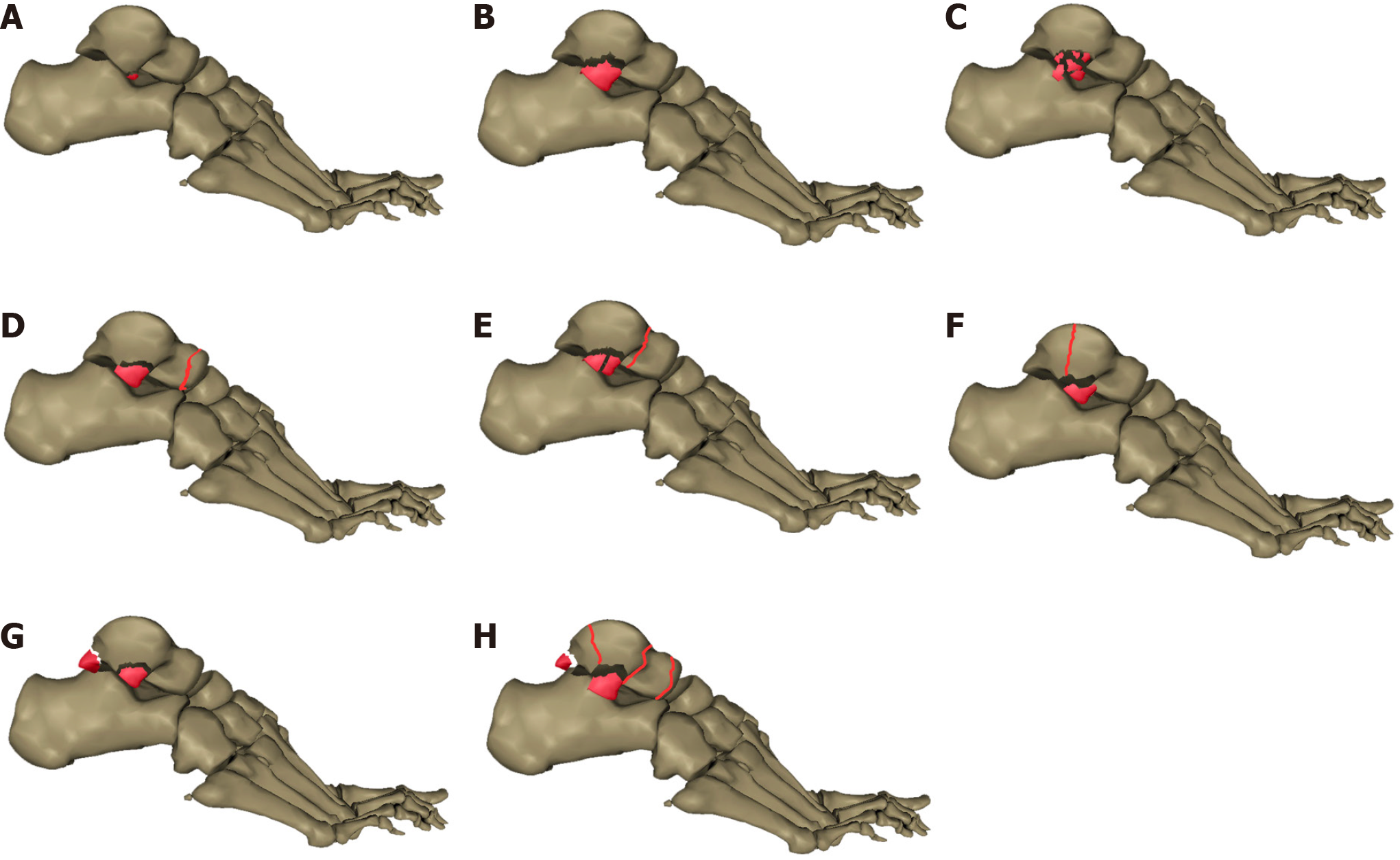
In 2023, the research team led by Wang et al[26] conducted a retrospective study of 43 FLPT cases and established a new classification system for FLPT based on CT features (Figure 7). This classification method broadly categorized FLPT into two major groups based on whether FLPT was combined with fractures of the ipsilateral talus; each major group was further divided into subtypes based on the fracture characteristics observed on CT scans.
Zhang's type 1: An isolated FLPT, further divided into three subtypes. (1) 1a: Chip fracture of the lateral talar process without involvement of the talofibular joint; (2) 1b: Simple fracture of the lateral talar process with the involvement of both the talofibular and subtalar joints; and (3) 1c: Comminuted fracture of the lateral talar process involving the articular surfaces.
Zhang's type 2: FLPT combined with fractures of other parts of the ipsilateral talus, with or without the involvement of the articular surfaces, was further divided into five subtypes. (1) 2a: FLPT combined with a fracture of the talar head; (2) 2b: FLPT combined with a fracture of the talar neck; (3) 2c: FLPT combined with a fracture of some other parts of the talar body (except for the lateral talar process, which has already been fractured); (4) 2d: FLPT combined with a fracture of the posterior talar process; and (5) 2e: FLPT combined with two or more fractures in other parts of the ipsilateral talus (except for the lateral talar process, which has already been fractured).
By analyzing the existing literatures and combining their own clinical experience, Wang et al[26] proposed a new classification for FLPT in 2023 and provided the corresponding treatment recommendations as follows: ORIF is best used for type 1a FLPT; type 1b FLPT should be better treated with fragments resection; type 1c FLPT should be treated conservatively with a plaster cast, and if fracture turned to be nonunion later, the fragments of a smaller size are resected surgically while the larger fracture fragments can be internally fixed with screws; finally, all type 2 FLPTs are recommended to be treated surgically with ORIF.
The prognosis of FLPT is related to many factors, including age, injury mechanism, fracture classification, management techniques, severity of articular cartilage damage, and presence of concomitant injuries. However, based on our literature review[25-29], we believe that the overall prognosis of FLPT is optimistic (Table 1).
| Ref. | Sample size | Classification | Treatments | Prognoses | Remarks regarding prognoses |
| Hawkins[15], 1965 | 13 | Hawkins type 1: 6; Hawkins type 2: 5; Hawkins type 3: 2 | All patients were treated conservatively as the initial treatment | 7 patients returned to normal motion without pain or limp. The remaining 6 had residual pain and/or limited motion and underwent subsequent fragments resection or joint fusion surgery, and ultimately 3 still had residual localized pain and mild limitation of movement | In Hawkins' day, the prognosis for conservatively treated patients was not that bad |
| von Winning et al[30], 2020[30] | 8 | All classified as McCrory-Bladin type 2 | ORIF with cannulated screws | All fractures healed completely; Mean AOFAS score was 81.4, mean FFI was 19.4, mean physical component summary score was 48.9, and mean mental component summary score was 51.9 | Delayed surgical managements did not significantly lead to a poor prognosis |
| Hörterer et al[6], 2019 | 22 | Hawkins type 1: 16; Hawkins type 2: 5; Hawkins type 3: 1 | ORIF: type 1; Fragments resection: type 2 and type 3 | 2 patients suffered minor surgical side infections. 12 patients developed symptomatic subtalar osteoarthritis, with no significant difference between types 1 and 2 fractures. Only 50% of the patients returned to the previous level of sports | The occurrence of secondary subtalar arthritis after ORIF and fragments resection was the same |
| Wijers et al[25], 2020 | 36 | Wijers type 1A: 1; Wijers type 1B: 6; Wijers type 2: 10; Wijers type 3: 11; Wijers type 4A: 6; Wijers type 4B: 2 | Conservative: 8; ORIF: 26; Subtalar joint fusion: 2 | 18 people were effectively followed up. The median AOFAS hindfoot score was 75 (range: 12-100) points. The median FFI score was 2 (range: 0-9) points. 3 (17%) patients had an excellent result, 8 (44%) patients had a good result, 5 (28%) patients had a fair result, and only 2 (11%) patients had a poor outcome | Patients who received timely and accurate managements were more likely to obtain a satisfactory prognosis |
| Ross et al[10], 2021 | 53 | McCrory-Bladin type 1: 7; McCrory-Bladin type 2: 23; McCrory-Bladin type 3: 23 | Conservative treatment was performed for 21 patients as the initial treatment to, of whom 14 underwent second surgery of fragments resection or subtalar joint fusion; ORIF was performed for 32 patients as the initial treatment. | For those whose initial treatments were conservative, PROMIS PF score was 53, FAAM-ADL was 88, FAAM-S was 75. There was no difference in the above indicators between patients who had or had not undergone second surgery. For those whose initial treatments were ORIF, PROMIS PF score was 56, FAAM-ADL was 90; FAAM-S was 77 | Long-term prognoses were closely related to fracture displacement, but less so to fragment size, subtalar joint compression injury, and treatment method. However, the rate of subsequent talar arthrodesis was higher in initial conservative treatment group |
| Wang et al[26], 2023 | 43 | Zhang's type 1a: 2; Zhang's type 1b: 1; Zhang's type 1c: 2; Zhang's type 2a: 1; Zhang's type 2b: 6; Zhang's type 2c: 18; Zhang's type 2d: 3; Zhang's type 2e: 10 | Conservative: 3; ORIF: 39; Fragments resection: 1 | AOFAS score: Zhang's type 1a: 91.5; Zhang's type 1b: 86.0; Zhang's type 1c: 90.5; Zhang's type 2a: 89.0; Zhang's type 2b: 76.7; Zhang's type 2c: 76.6; Zhang's type 2d: 91.3; Zhang's type 2e: 83.5. Complications including nonunion and arthritis were observed in only 7 (16.3%) cases | Prognoses of FLPT were related to simultaneous injuries of other parts of ipsilateral talus |
| Feng et al[28], 2023 | 42 | All fractures were classified as McCrory-Bladin type 3 | Arthroscopic internal fixation was performed for 24 cases by using a Double-pully technique combined with Kirschner wire. Open reduction and Kirschner wire fixation were performed for 18 patients | Among the patients treated arthroscopically, only 2 (8.3%) developed subtalar arthritis, with the primary symptoms being local pain and discomfort after exercising that was relieved by taking rest. After 12 months of surgery, the mean PROMIS PF score was 71.6, mean AOFAS score was 94.0, mean FAAM-ADL was 92.5, and mean FAAM-S was 94.4. Among those who underwent open reduction and Kirschner wire fixation, 6 (33.3%) patients developed subtalar arthritis. Consequently, 3 of them underwent a second surgery of subtalar joint fusion. After 12 months of surgery, the mean PROMIS PF score was 62.9, mean AOFAS score was 77.9, mean FAAM-ADL score was 72.1, and mean FAAM-S score was 78.6 | Arthroscopic-assisted surgery can help improve the prognoses of FLPT |
| Feng et al[29], 2023 | 33 | All fractures were classified as McCrory-Bladin type 2 | 21 patients were treated with double-tunnel subtalar arthroscopy combined with hollow compression screw internal fixation. The other 12 patients were treated with ORIF with hollow compression screw | For patients treated arthroscopically, no obvious complication was found. At the final follow-up, the mean AOFAS score was 95.8, mean FFI score was 12.3, mean FAAM-ADL score was 92.7, and mean FAAM-S score was 95.6. Among those who underwent ORIF with hollow compression screw, 2 (16.7%) patients developed local skin numbness associated with nerve injury. At the last follow-up, the mean AOFAS score was 94.8, mean FFI score was 14.4, mean FAAM-ADL score was 89.8, and mean FAAM-S score was 93.6 | For McCrory-Bladin type 2 FLPT, the use of compression screw internal fixation could achieve reliable results. However, compared to open surgery, arthroscopy procedure obtained mini trauma and better functions |
| Mui et al[31], 2020 | 1 delayed case | Not mentioned | ORIF with 2 headless compression screw, followed by an iliac autologous bone graft procedure and anterior talofibular ligament reconstruction with 2 suture anchors | An overgrowth of the tip of the lateral talar process led to pain while snowboarding. After 1 yr of the second surgery of the enlarged part excision, the patient returned to his previous level of motion without pain | Delayed FLPT cases can also lead to good long-term prognosis |
| Killen et al[32], 2018 | 2 delayed cases | Not mentioned | ORIF with a headless compression screw and anterior talofibular ligament reconstruction with a suture anchor | At 12 months after surgery, the mean AOFAS score was 90. Both patients regained recovery of full, activity without any residual pain or symptoms of instability | Delayed FLPT cases can also lead to good long-term prognosis |
In Hawkins's research[15], seven patients achieved satisfactory results without pain or limitation of motion after immobilization with a plaster cast for 8 wk, whereas six patients experienced temporary disability lasting for approximately half a year after the fracture, of which five patients experienced persistent pain on standing or walking and one patient suffered malunion. Additionally, among the five patients with persistent pain, three patients suffered nonunion and two suffered overgrowth that led to pain or limited dorsiflexion of the foot. Consequently, second surgeries, either fragment resection or subtalar fusion depending on the size of the fragments and secondary changes of the subtalar joint, were performed for all the six patients in whom conservative management failed.
von Winning et al[30] reported the midterm results of eight displaced McCrory-Bladin type 2 FLPT cases by conducting an average of 7-year follow-up after ORIF with cannulated screws. In the study, all fractures healed completely. In addition, one patient developed traumatic arthritis of the ankle (Bargon's grade I), and one patient with an associated calcaneus fracture developed subtalar arthritis (Bargon's grade III) and received subsequent subtalar joint arthrodesis. The study revealed good clinical results, with a mean American Orthopedic Foot and Ankle Society (AOFAS) score of 81.4, mean Foot Function Index (FFI) of 19.4, mean physical component summary score of 48.9, and mean mental component summary score of 51.9. However, unlike most other studies, von Winning et al[30] compared the prognosis between patients treated surgically within 14 d of the fracture and those who underwent surgical treatment after 14 d of the fracture. The results showed no statistically significant difference between the two groups, suggesting that delayed surgical management does not always lead to poor prognosis.
Hörterer et al[6] conducted a study involving 22 patients with FLPT, including 16 patients with Hawkins type 1 fractures, 5 with Hawkins type 2 fractures, and 1 case with Hawkins type 3 fracture. He performed ORIF for Hawkins type 1 fractures and fragment resection for types 2 and 3 fractures. The results showed that 9% of patients suffered minor surgical side infections, and 55% developed symptomatic subtalar osteoarthritis. Moreover, the patient-rated outcomes revealed only moderate-to-good score more than 3 years after surgery.
Ross et al[10] followed all patients with FLPT at a level I trauma center over a 10-year period, with a mean follow-up of 6.5 years. This is the most recent and comprehensive study on the prognosis of FLPT. This study finally collected data from 53 patients, among whom 21 (39.6%) underwent initial conservative treatment, whereas 32 (60.4%) received initial surgical treatment. They noted that the failure of conservative treatment was closely related to the displacement rather than the size of the fracture fragments, and that FLPT with displacement had a higher rate of failure when treated conservatively, whereas FLPT without displacement usually did not require additional surgical treatments. Nevertheless, the prognosis of patients who underwent subsequent surgery due to the failure of conservative treatment was comparable to that of patients who had satisfactory results after conservative treatment. On the contrary, they concluded that whether FLPT was combined with compression injury of the subtalar joint did not affect the long-term prognosis, and there was no statistically significant difference in the prognosis between patients who were successfully treated with conservative treatment and those who received surgical therapies (whether initial or not); however, the rate of subsequent talar arthrodesis was higher in the conservatively treated group.
In a study of 36 FLPT cases, Wijers et al[25] found that excellent and good prognoses accounted for 61%, whereas poor prognosis accounted for only 11% of the cases, regardless of management methods. In addition, concomitant injuries and delayed clinical visits contribute to poor prognosis, indicating that the majority of patients who received timely and accurate management are more likely to obtain a satisfactory prognosis.
An optimistic result was also presented by Wang et al[26]. He followed 43 FLPT cases for an average of 35.9 months and used the AOFAS score to evaluate the clinical prognosis. The results showed that AOFAS score was 91.5 ± 1.5 in type 1a, 86.0 ± 0 in type 1b, 90.5 ± 9.5 in type 1c, 89.0 ± 0 in type 2a, 76.7 ± 15.6 in type 2b, 76.6 ± 24.4 in type 2c, 91.3 ± 6.6 in type 2d, and 83.5 ± 11.0 in type 2e of fractures of Zhang's classification. Additionally, complications such as nonunion and arthritis were observed in only seven cases (16.3%).
We also reviewed the prognoses of patients with FLPT treated with different surgical techniques. Feng et al[28] performed arthroscopic internal fixation for 24 patients with McCrory-Bladin type 3 FLPT using a Double-pully technique combined with a Kirschner wire. The results showed that only two patients (8.3%) developed subtalar arthritis, with local pain and discomfort after exercising as primary symptoms relieved by taking rest. In another retrospective cohort study, Feng et al[29] compared the clinical outcomes between ORIF and arthroscopic-assisted fracture reduction and internal fixation in 33 patients with McCrory-Bladin type 2 FLPT, including 21 and 12 patients in the arthroscopy and ORIF groups, respectively. After a mean follow-up of 19.5 months, the author reported no significant difference in the AOFAS scores between the arthroscopy and ORIF groups at the final follow-up (95.8 ± 3.3 and 94.8 ± 3.7, respectively). However, the FFI was significantly lower in the arthroscopy group than in the ORIF group at the last follow-up (12.3 ± 5.3 and 14.4 ± 6.0, respectively). Additionally, no nerve or tendon complications were observed in the arthroscopy group, whereas two patients developed postoperative numbness in the dorsal region of the foot in the ORIF group. Finally, the author summarized that patients with McCrory-Bladin type 2 FLPT can obtain a good prognosis after internal fixation with compression screws; however, arthroscopic-assisted internal fixation is less invasive and more likely to lead to a better prognosis than ORIF.
Nevertheless, a good prognosis is also observed in delayed cases. Mui et al[31] presented a case of a 40-year-old male snowboard instructor with FLPT due to snowboarding. Unfortunately, the patient was initially misdiagnosed with an ankle sprain, and it was not until 6 months later that he was definitively diagnosed with FLPT. Subsequently, he underwent ORIF and an iliac autologous bone graft procedure, which resulted in a complete union of the fracture 3 months after surgery. In addition, the patient resumed his previous level of activity 5 months after surgery. However, at 18 months postoperatively, the patient complained of pain while snowboarding. A subsequent CT scan revealed complete fracture union and an enlarged lateral process forming an accessory anterolateral talar facet, which was confirmed as the cause of the pain. Finally, an additional surgery was performed to resect the enlarged part of the lateral process. A year after the second surgery, the patient was free from pain in the local region and had resumed normal sports activities. Similarly, Killen et al[32] reported cases of two patients who underwent reoperation due to nonunion after conservative treatment. Initially, they performed an open reduction of the fracture and used one or two headless cannulated screws for fixation. Subsequently, intraoperative examination showed a positive anterior drawer test; therefore, a suture anchor was placed in the distal fibula to repair the lateral ligament, and the extensor retinaculum and periosteum were used to reinforce the repair. The follow-up results at 12 months after surgery showed complete union and full range of motion in both patients, with no persistent discomfort and an average AOFAS score of 90.
In summary, FLPT is rare in clinical practice. Considering that the main symptoms are similar to lateral malleolar soft tissue injuries without specificity, it can be easily missed or misdiagnosed as an ankle sprain, resulting in delayed diagnosis and treatment, which may eventually lead to subtalar osteoarthritis and instability. Therefore, FLPT must always be considered when diagnosing a dorsiflexed inverted ankle injury, especially resulting from snowboarding.
Imaging examinations for FLPT are essential for establishing accurate diagnosis and classification. Ultrasonography, the use of which to diagnose FLPT has only been shown in one case report[33], is noninvasive, nonradiative, convenient, and targeted. However, with gradually increasing studies on the ultrasonographic features of fractures in the past few years, ultrasonography is expected to become a preliminary screening method for FLPT in the future. Although radio
The management principle for FLPT is currently controversial, and the selection of conservative treatment, fragment resection, and ORIF for a certain type of fracture is inconclusive, and lacks support from the results of clinical randomized controlled trials, as well as reliable consensus and guidelines. However, ongoing research worldwide has led to a more comprehensive understanding of the pathological and anatomical characteristics of FLPT. New classification systems have emerged constantly and guided the clinical treatment of FLPT more scientifically. However, more data from clinical studies are needed to summarize the pathological characteristics of FLPT to formulate more detailed and reliable treatment principles.
The prognosis of FLPT is related to several factors and cannot be simply generalized. However, based on the current literature, we believe that the overall prognosis of FLPT is good, even in delayed cases. To evaluate the prognosis of FLPT more scientifically, multicenter prospective randomized controlled clinical studies with large sample sizes are urgently required.
We would like to thank the foot and ankle surgical team of Center of Musculoskeletal Surgery, Berlin Charité Medical University Hospital, for the support and guidance.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Schmidt EJ, United States S-Editor: Zheng XM L-Editor: A P-Editor: Zhang XD
| 1. | Tinner C, Sommer C. Fractures of the Lateral Process of the Talus. Foot Ankle Clin. 2018;23:375-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Kirkpatrick DP, Hunter RE, Janes PC, Mastrangelo J, Nicholas RA. The snowboarder's foot and ankle. Am J Sports Med. 1998;26:271-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 154] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Berkowitz MJ, Kim DH. Process and tubercle fractures of the hindfoot. J Am Acad Orthop Surg. 2005;13:492-502. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Funk JR, Srinivasan SC, Crandall JR. Snowboarder's talus fractures experimentally produced by eversion and dorsiflexion. Am J Sports Med. 2003;31:921-928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Boon AJ, Smith J, Zobitz ME, Amrami KM. Snowboarder's talus fracture. Mechanism of injury. Am J Sports Med. 2001;29:333-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 83] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Hörterer H, Baumbach SF, Lemperle S, Altenberger S, Gottschalk O, Mehlhorn AT, Röser A, Walther M. Clinical outcome and concomitant injuries in operatively treated fractures of the lateral process of the talus. BMC Musculoskelet Disord. 2019;20:219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Chan GM, Yoshida D. Fracture of the lateral process of the talus associated with snowboarding. Ann Emerg Med. 2003;41:854-858. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Valderrabano V, Perren T, Ryf C, Rillmann P, Hintermann B. Snowboarder's talus fracture: treatment outcome of 20 cases after 3.5 years. Am J Sports Med. 2005;33:871-880. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Perera A, Baker JF, Lui DF, Stephens MM. The management and outcome of lateral process fracture of the talus. Foot Ankle Surg. 2010;16:15-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Ross H, Marchand L, Cardon J, Beals T, Barg A, Nickisch F, Haller JM. Patient-Reported Outcomes After Lateral Process Talus Fracture. J Orthop Trauma. 2021;35:e470-e474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Dale JD, Ha AS, Chew FS. Update on talar fracture patterns: a large level I trauma center study. AJR Am J Roentgenol. 2013;201:1087-1092. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Ali MKM, Mbah C, Alwadiya A, Milner S. How a minor trauma can cause long term disability! A misdiagnosed fracture of the lateral process of the talus-A case report and review of literature. EC Orthop. 2015;1:21-26. [Cited in This Article: ] |
| 13. | Drake R, Vogl AW, Mitchell AWM. Gray's Anatomy for Students. 5th ed. Amsterdam: Elsevier Pub, 2023: 627-628. [Cited in This Article: ] |
| 14. | Russell TG, Byerly DW. Talus Fracture. 2023 May 23. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] [Cited in This Article: ] |
| 15. | Hawkins LG. Fracture of the lateral process of the talus. J Bone Joint Surg Am. 1965;47:1170-1175. [PubMed] [Cited in This Article: ] |
| 16. | Fjeldborg O. Fracture of the lateral process of the talus. Supination-dorsal flexion fracture. Acta Orthop Scand. 1968;39:407-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Mukherjee SK, Pringle RM, Baxter AD. Fracture of the lateral process of the talus. A report of thirteen cases. J Bone Joint Surg Br. 1974;56:263-273. [PubMed] [Cited in This Article: ] |
| 18. | Bladin C, Giddings P, Robinson M. Australian snowboard injury data base study. A four-year prospective study. Am J Sports Med. 1993;21:701-704. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 97] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Bladin C, McCrory P. Snowboarding injuries. An overview. Sports Med. 1995;19:358-364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 64] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Pino EC, Colville MR. Snowboard injuries. Am J Sports Med. 1989;17:778-781. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 77] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | McCrory P, Bladin C. Fractures of the lateral process of the talus: a clinical review. "Snowboarder's ankle". Clin J Sport Med. 1996;6:124-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 70] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Jin XY, Xiao WY, He T, Dong YQ, Zhang C. Fracture of the lateral process of the talus with associated deltoid ligament injury: a report of 2 cases. BMC Surg. 2022;22:356. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 23. | Dimon JH 3rd. Isolated displaced fracture of the posterior facet of the talus. J Bone Joint Surg Am. 1961;43-A:275-281. [PubMed] [Cited in This Article: ] |
| 24. | Boack DH, Manegold S. Peripheral talar fractures. Injury. 2004;35 Suppl 2:SB23-SB35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Wijers O, Posthuma JJ, De Haas MBJ, Halm JA, Schepers T. Lateral Process Fracture of the Talus: A Case Series and Review of the Literature. J Foot Ankle Surg. 2020;59:136-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Wang Y, Wang Z, Zhu Y, Fu L, Deng X, Chen W, Zhang Y. New Classification Based on CT and Its Value Evaluation for Fractures of the Lateral Process of the Talus. J Foot Ankle Surg. 2023;62:644-650. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 27. | Sariali E, Lelièvre JF, Catonné Y. Fractures of the lateral process of the talus. Retrospective study of 44 cases. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:e1-e7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Feng SM, Xue C, Qi LE, Luo X, Jiang XW, Wang ML, Ma C. Internal fixation of McCrory-Bladin type III fracture of the lateral process of the talus with Kirschner wire Double-pully technique under subtalar arthroscopy. Zhonghua Chuangshang Zazhi 2023; 39: 899-905. [DOI] [Cited in This Article: ] |
| 29. | Feng SM, Luo X, Xue C, Chen J, Wang K, Shao CQ, Ma C. [Effect of hollow compression screw internal fixation in treating McCrory-Bladin type Ⅱ lateral process fracture of the talus: open versus arthroscopy surgery]. Zhonghua Yi Xue Za Zhi. 2023;103:2808-2812. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 30. | von Winning D, Lippisch R, Pliske G, Adolf D, Walcher F, Piatek S. Surgical treatment of lateral and posterior process fractures of the talus: Mid-term results of 15 cases after 7 years. Foot Ankle Surg. 2020;26:71-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Mui T, Sugimoto K, Sugioka S, Yamasaki T, Tanaka K, Isomoto S, Tanaka Y. Accessory Anterolateral Talar Facet Syndrome After Treatment of Neglected Fracture of the Lateral Process of the Talus: A Case Report. J Foot Ankle Surg. 2020;59:826-828. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 32. | Killen MC, Karpe P, Limaye R. Fractures of the Lateral Process of the Talus With Associated Ankle Instability: A Report of 2 Cases. Foot Ankle Spec. 2018;11:378-381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Copercini M, Bonvin F, Martinoli C, Bianchi S. Sonographic diagnosis of talar lateral process fracture. J Ultrasound Med. 2003;22:635-640. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Noble J, Royle SG. Fracture of the lateral process of the talus: computed tomographic scan diagnosis. Br J Sports Med. 1992;26:245-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Whitby EH, Barrington NA. Fractures of the lateral process of the talus--the value of lateral tomography. Br J Radiol. 1995;68:583-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |