Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5297
Peer-review started: February 21, 2022
First decision: March 23, 2022
Revised: April 20, 2022
Accepted: May 13, 2022
Article in press: May 13, 2022
Published online: June 6, 2022
Dentition defect, a common clinical oral disease developed in humans, not only causes masticatory dysfunction and articulation difficulties but also affects facial appearance and increases the burden on the intestinal tract. Restorative treatment is the primary option for this disease. However, traditional restorations have many drawbacks, such as mismatch with the body, low reliability, and incomplete occlusal function recovery.
to analyze the efficacy of orthodontics combined with 3D printing guide plate implant restoration in treating patients with dentition defects and its influence on masticatory and phonic functions.
A prospective study was carried out in 86 patients with dentition defects who received implant prosthesis after orthodontic treatment in our hospital between January 2018 and January 2019. Those patients were divided into a control group and an intervention group with 43 patients in each group using a random number table. The control group received traditional implant restoration, whereas the intervention group received 3D printing guide plate implant restoration. Treatment outcomes, cosmetic appearance, dental function, implant deviation, and quality of life were compared between the two groups.
The overall response rate in the intervention group was significantly higher than that in the control group (95.35% vs 81.40%, χ2 = 4.071, P = 0.044). The number of cases with neatly trimmed cosmetic appearance (χ2 = 4.497, P = 0.034), complete coverage (χ2 = 4.170, P = 0.041), and normal occlusion (χ2 = 5.512, P = 0.019) in the intervention group was higher than that in the control group. After treatment, mastication, swallowing, and articulation were significantly improved in both groups. Masticatory (t = 2.980, P = 0.004), swallowing (t = 2.199, P = 0.031), and phonic functions (t = 3.950, P = 0.004) were better in the intervention group than those in the control group. The deviation value and the deviation angle (t = 5.440, P = 0.000) at the top (t = 6.320, P = 0.000) and middle parts of the implants (t = 22.295, P = 0.000) in the intervention group were lower than those in the control group after treatment. Functional limitations, psychosocial and physical pain and discomfort, and total scores decreased in both groups. The functional limitation (t = 2.379, P = 0.020), psychosocial (t = 2.420, P = 0.000), physical pain and discomfort (t = 6.581, P = 0.000), and total scores (t = 2.140, P = 0.035) were lower in the intervention group than those in the control group.
Orthodontic treatment combined with 3D printing guide plate implant restoration can significantly improve the masticatory and phonic functions, quality of life, and psychological health of patients with dentition defects. Therefore, it is highly recommended in clinic application.
Core Tip: In the present prospective study, we included 86 patients with dentition defects who underwent implant restoration after orthodontic treatment at our hospital between January 2018 and 2019. The patients were divided into two groups using a random number table: the patients in the control group were treated with implant prosthesis, and those in the intervention group were treated with 3D printing guide plate implantation. In terms of oral function after treatment, the patients in the intervention group had significantly better chewing, swallowing, and phonic functions than those in the control group. The above results demonstrate that the consistency of the implant with the body was significantly improved after 3D printing guide plate implantation, which had a positive effect on muscle strength recovery at the local lesions. The results of the present study support 3D printing guide plate implantation in routine clinical use.
- Citation: Yan LB, Zhou YC, Wang Y, Li LX. Orthodontic treatment combined with 3D printing guide plate implant restoration for edentulism and its influence on mastication and phonic function. World J Clin Cases 2022; 10(16): 5297-5305
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5297.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5297
Dentition defects is one of the most common oral diseases in clinical practice. Progression of this disease causes not only masticatory dysfunction and articulation difficulties but also aesthetic damage, seriously disturbing people’s quality of life[1]. Furthermore, the ability to chew foods at the lesions is markedly reduced, which increases the intestinal burden among patients[2]. Long-term dentition defects also leads to compensatory ptosis of the corner of the mouth, deepening of wrinkles, and other marked changes in appearance. Currently, restorative treatment is the primary method used to fix dentition defects. Through such treatment, oral function and aesthetics of patients can be effectively improved. However, there is a gap between the conventional implant prosthesis and the receptor, resulting in lower reliability of the prosthesis[3] impeding the occlusal recovery of the body[4]. Moreover, in patients with long-term edentulism, the adjacent teeth on both sides tilt to a certain extent, thereby presenting challenges to the denture repair. A study found that implantation aided by 3D printing guide plate can improve the reliability of prosthesis[5]. This study analyzed the effect of orthodontic treatment combined with 3D printing guide plate implantation in dentition defects in an effort to provide scientific verification for its clinical application.
This prospective study enrolled 86 patients with dentition defects who underwent implant restoration after orthodontic treatment at our hospital between January 2018 and 2019.
The inclusion criteria were as follows: (1) receiving treatment with orthodontics and desire for a fixed denture restoration; (2) no retention value among all residual teeth in the dentition defects; and (3) signing the informed consent. The exclusion criteria were as follows: (1) severe cardiovascular and cerebrovascular diseases; (2) cognitive dysfunction; (3) inability to perform in this study; and (4) intolerance to the implants or restorations used in this study. This study was approved by the Ethics Committee of our institution.
All patients were given an oral health examination. According to the imaging data, orthodontic treatment was adopted, and straight-wire technique or edgewise archwire fixation technique was opted for treatment. By observing the dislocation and inclination of teeth, the tooth space was adjusted in time to correct the lesion occlusion relationship. The patients in the control group received implant restoration: it was carried out in time based on the severity of dentition defects. Before operation, their oral cavity and surrounding skin were disinfected, sterile swabs were laid, and lidocaine (2% concentration) was administered for local anesthesia. Under the action of the guide plate, L-shaped or H-shaped incision was made on the periosteum and bone surface at the implantation point. After fully exposing the alveolar bone, drilling on the top of the alveolar ridge was performed, and the implant restoration was carried out by the imaging characteristics. After the operation, normal saline was used to clean the lesion and bleeding is stopped. After placing appropriate screws, soft tissues were sutured. Patients were given antibiotics routinely after operation, and the sutures were removed 7-10 d after operation.
Patients in the intervention group were treated with 3D printing guide plate implant restoration. Their lesions were scanned with computed tomography (CT) before operation. The model data of the patients were obtained using a 3Shape D700 series scanners from the United States. The occlusal relationship was simultaneously recorded using cone-beam CT and rubber molding. Occlusal rim was adopted for patients without malocclusion. After the relationship between the length, direction, and position of the implant was clear, the aforementioned data were imported into the 3D tool again for 3D reconstruction, and the preoperative plaster cast was confirmed using a laser scanner. The implant guide plate was prepared simultaneously based on real-time data registration during data reconstruction. Thereafter, the implant restoration was completed. Routine antibiotic treatment was administered postoperatively.
Efficacy: The efficacy was compared in the two groups after surgery. When the dentition defect was repaired and there was no difference in the physiological function and color between the local lesions and normal tooth condition, the treatment was considered significantly effective. When the dentition defect was roughly repaired and there was a slight difference in the physiological function and color between the local lesions and normal tooth condition, the treatment was considered effective. When the dentition defect was not effectively repaired and there was a significant difference in the physiological function and color between the local lesions and normal tooth condition, the treatment was considered ineffective. The overall response rate was calculated as follows: (effective + significantly effective)/ (total number of cases)[6].
Cosmetic appearance: Alignment, complete coverage, and occlusal normality after treatment were compared between the two groups.
Dental function: The masticatory, swallowing, and phonic functions were compared between the two groups before and six months after treatment. These variables were rated using a 5-level Likert scale, with higher scores indicating better outcomes[7].
Implant deviations in the 3D plane: Six months after treatment, CT was performed in both groups, and the data were inputted into the 3D tool for 3D reconstruction. The deviation values and the deviation angles at the top and middle parts of the implants were compared between the two groups.
Quality of life: The quality of life of patients was evaluated before and 6 mo after treatment using the Oral Health Impact Profile for Supported Partial Prostheses[8]. It was rated through the evaluation of the functional limitation, social interaction, and physical pain and discomfort of the patients. Higher scores it obtained, worse quality of life was among patients.
Data was analyzed using the SPSS 19.0 in this study, in which measurement data were measured as mean ± SD. An independent sample t-test was also conducted. Enumeration data were expressed as n (%), and comparison between groups were made by χ2 test. P < 0.05 indicated statistical significance.
There were 44 women and 42 men aged 36-61 years (average age: 45.67 ± 3.83 years). The average body mass index (BMI) was 24.90 ± 2.22 kg/m2. Seventeen patients had complete perioral dentition defect, 30 had lower tooth losses, and 39 had upper tooth losses. The patients were divided into two groups using a random number table; each group included 43 patients, and there was no significant difference in the types of dentition defect, sex, age, or BMI between the groups (P > 0.05) (Table 1).
| Group | Sex (male/female) | Dentition defects (full mouth/upper/lower) | Body mass index (kg/m2) | Age (yr) |
| Control group (n = 43) | 20/23 | 8/12/23 | 24.83 ± 2.24 | 45.60 ± 3.26 |
| Intervention group (n = 43) | 22/21 | 9/18/16 | 24.97 ± 2.22 | 45.74 ± 4.37 |
| χ2/t value | 0.186 | 2.515 | 0.291 | 0.168 |
| P value | 0.667 | 0.284 | 0.772 | 0.867 |
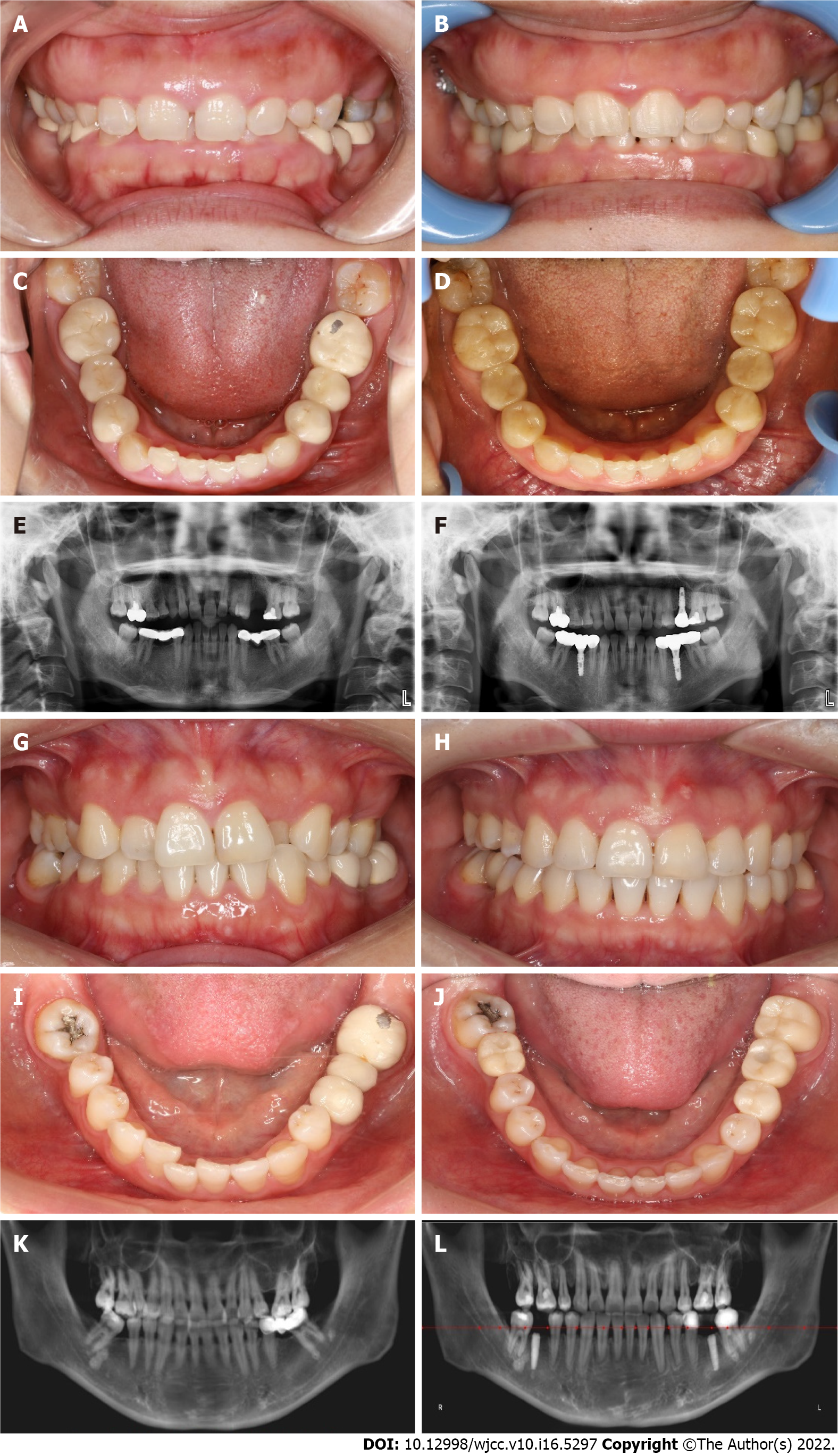
The overall response rate of the intervention group was significantly higher than that of the control group (95.35% vs 81.40%, χ2 = 4.071, P = 0.044). Further details are provided in Table 2. Pictures of typical cases are shown in Figure 1.
| Group | Significantly effective | Effective | Ineffective | Overall response rate |
| Control group (n = 43) | 15 (34.88) | 20 (46.51) | 8 (18.60) | 35 (81.40) |
| Intervention group (n = 43) | 25 (58.14) | 16 (37.21) | 2 (4.65) | 41 (95.35) |
| χ2/U value | 2.391 | 4.071 | ||
| P value | 0.014 | 0.044 | ||
The number of cases with neatly arranged cosmetic appearance (χ2 = 4.497, P = 0.034), complete coverage (χ2 = 4.170, P = 0.041), and normal occlusion (χ2 = 5.512, P = 0.019) was significantly higher in the intervention group than that in the control group. Further details are provided in Table 3.
| Group | Neatly trimmed cosmetic appearance | Complete coverage | Normal occlusion |
| Control group (n = 43) | 30 (69.77) | 29 (67.44) | 25 (58.14) |
| Intervention group (n = 43) | 38 (88.37) | 37 (86.05) | 35 (81.40) |
| χ2 value | 4.497 | 4.170 | 5.512 |
| P value | 0.034 | 0.041 | 0.019 |
Before treatment, swallowing, masticatory, and phonic functions did not significantly differ between the groups (P > 0.05). After treatment, masticatory, swallowing, and phonic functions significantly improved in both groups. The masticatory (t = 2.980, P = 0.004), swallowing (t = 2.199, P = 0.031), and phonic functions (t = 3.950, P = 0.004) were significantly better in the intervention group than those in the control group. Further details are provided in Table 4.
| Group | Masticatory function | Swallowing function | Phonic function | |||
| Before | After | Before | After | Before | After | |
| Control group (n = 43) | 1.91 ± 0.29 | 3.09 ± 0.43 | 2.65 ± 0.48 | 3.63 ± 0.54 | 2.56 ± 0.98 | 3.26 ± 0.98 |
| Intervention group (n = 43) | 1.98 ± 0.27 | 3.37 ± 0.49 | 2.67 ± 0.47 | 3.86 ± 0.41 | 2.58 ± 0.59 | 3.97 ± 0.64 |
| t value | 1.154 | 2.821 | 0.225 | 2.255 | 0.133 | 4.052 |
| P value | 0.252 | 0.006 | 0.822 | 0.027 | 0.894 | 0.000 |
The deviation values and the deviation angle (t = 5.440, P = 0.000) at the top (t = 6.320, P = 0.000) and middle parts of the implants (t = 22.295, P = 0.000) in the intervention group were significantly lower than those in the control group (Table 5).
| Group | Top (mm) | Middle (mm) | Angle (°) |
| Control group (n = 43) | 1.66 ± 0.97 | 1.51 ± 0.28 | 2.95 ± 1.23 |
| Intervention group (n = 43) | 0.54 ± 0.34 | 0.43 ± 0.15 | 1.78 ± 0.69 |
| t value | 7.122 | 22.295 | 5.440 |
| P value | 0.000 | 0.000 | 0.000 |
Before treatment, functional limitation, psychosocial and physical pain and discomfort, and total scores did not significantly differ between the groups (P > 0.05). After treatment, functional limitation, psychosocial and physical pain and discomfort, and total scores decreased in both groups. Functional limitations (t = 2.379, P = 0.020), psychosocial (t = 2.420, P = 0.000), physical pain and discomfort (t = 6.581, P = 0.000), and total scores (t = 2.140, P = 0.035) were significantly lower in the intervention group than in the control group. Further details are provided in Table 6.
| Group | Functional limitation | Physiological pain and discomfort | Psychological and social | Total score | ||||
| Before | After | Before | After | Before | After | Before | After | |
| Control group (n = 43) | 3.70 ± 1.52 | 1.70 ± 0.96 | 2.37 ± 1.57 | 1.21 ± 0.41 | 3.26 ± 1.54 | 1.56 ± 0.98 | 9.33 ± 2.54 | 4.47 ± 1.32 |
| Intervention group (n = 43) | 3.74 ± 1.38 | 1.21 ± 0.68 | 2.33 ± 1.32 | 0.65 ± 0.48 | 3.21 ± 1.77 | 1.09 ± 0.75 | 9.28 ± 2.48 | 2.95 ± 1.11 |
| t value | 0.148 | 2.721 | 0.148 | 5.773 | 0.130 | 2.466 | 0.086 | 5.755 |
| P value | 0.882 | 0.008 | 0.882 | 0.000 | 0.897 | 0.016 | 0.932 | 0.000 |
Dentition defect is a prevalent oral disease, and related research has found that nearly 60% of the patients with such disease will develop dental malformation, aggravating the case, which can cause a vicious spiral[9]. Orthodontic treatment before implantation can alleviate malocclusion and jaw malformation, make the mouth more desirable, and maintain the normal physiological alignment between the implant and the normal teeth in the mouth for a longer time. However, implants can only repair dentures, which makes it difficult to improve the beauty and function of teeth in the mouth. If implant restoration is directly implemented, it may expose the patients to the unfavorable implants and aesthetics, and reduce the repair effect because of abnormalities such as the loss of anterior teeth. Therefore, orthodontic treatment before implantation can potentially improve the outcomes of subsequent implant repair[10]. In the treatment of patients with dentition defects, an implant guide plate constitutes a pivotal part in the treatment of multiple missing teeth and poor alveolar bone[9]. Implant guide plates play a considerable guiding role, particularly for doctors with little experience. Therefore, in the course of implant application, the selection of an appropriate implant guide plate plays a decisive role[10]. The fabrication of implant guide plates has many advantages, and plaster casts are routinely used for their preparation. Although the fabrication process is simple, there have been few analyses of the internal bone tissue structure of the edentulous sites. After implantation, the risk of implant deviation increases markedly[11]. Simultaneously, it is necessary to rely on clinical experience during implantation[12]. During this process, the matching accuracy of the model and tooth may be insufficient owing to the use of the vacuum-formed pressure film technology. During model preparation, it was necessary to rotate the model repeatedly. This process may increase the unreliability of the implant guide plate and further enlarge the offset after treatment. With the continuous clinical application of 3D technology, the anatomical position of the dentition defect site is fully considered in the preparation of the model and its accuracy is greatly improved.
In this study, we found that the efficacy in the intervention group was better than that in the control group, and the aesthetics also significantly improved. In the treatment of dentition defects, a substantial inflammatory response inevitably occurs in the alveolar bone of the lesion site, which is markedly destructive to both the bone surface and the periosteal structure. A meta-analysis of studies comparing the clinical outcomes of denture restorations and implants for the treatment of edentulism showed that implant restorations are more effective in the treatment of edentulism than dentures[13]. However, challenges still exists. During implant restoration, the mismatch between the implant and anatomical position of the body[14] causes tooth wear in the gingival and oral tissues[15], and the continuous inflammatory response in gingival tissues[16] further damages the local aesthetics[17]. Involuntary muscle spasms can also be caused by mismatched implant restorations[17], and abnormal changes in appearance can occur as the disease progresses[18]. Complications, due to unpredictability such as pulpal necrosis, root resorption, loosening, and loss of teeth are often observed after dental implantation that therefore not often promoted clinically[19]. In this study, the deviation values at the top and middle parts of the implants in the intervention group were lower than those in the control group, which also confirmed the significant advantage of 3D printing guide plate implantation[20]. In a comparative study of traditional and 3D-printed implant plates, Suo et al[21] showed that 3D-printed implant plates had a significant accuracy advantage in the treatment of patients with dentition defects.
In terms of dental function after treatment, the masticatory, swallowing, and phonic functions of the intervention group were significantly better than those of the control group in our study, suggesting that with the use of 3D printing guide plate implantation, the matching of implants to the body is markedly improved, which has a positive role in the recovery of muscle strength at the local lesions. In addition, the quality of life of the intervention group was significantly higher than that of the control group, showing that through the improvement of the tooth function and aesthetics of the patients, the use of 3D printing guide plate implantation has a positive role in improving the quality of life of patients after surgery.
In summary, following the orthodontic treatment combined with 3D printing guide plate implant restoration in patients with dentition defects, the masticatory and phonic functions of the patients significantly improved, so did the quality of life and psychological health. On the basis of these findings, 3D printing guide plate implantation is recommended for clinical application.
To sum up, we have confirmed the significant advantages of 3D printing guide plate implantation, including significant recovery of muscle strength, significant improvement in oral function and quality of life, and a more aesthetic facial appearance in patients at the local lesion site 3D printing guided implant reconstruction is conducive to improving masticatory and phonic functions, and is recommended for clinical application.
Dentition defects are among the most common oral diseases in clinical practice. Progression of this disease causes not only masticatory dysfunction and articulation difficulties but also aesthetic damage among patients, seriously affecting their quality of life.
There exists a gap between the conventional prosthesis and the body, resulting in a decrease in the reliability of the prosthesis, consequently impacting the recovery of the occlusal relationship of the body.
This study aimed to investigate the influence of orthodontic treatment combined with 3D printing guide plate implantation on masticatory and language functions in patients with dentition defects.
The study included 86 patients with dentition defects who were divided into two groups using a random number table, with each group including 43 patients. The control group received traditional implant prosthesis, whereas the intervention group received 3D printing guide plate implantation.
In terms of dental function after treatment, the masticatory, swallowing, and phonic functions of the intervention group were significantly better than those of the control group.
Orthodontics combined with 3D printing guide plate implant restoration can significantly improve the masticatory and language functions of patients with dentition defects.
The results of this study on orthodontics combined with 3D printing guide plate implant restoration will lay the foundation for further clinical utility of this method.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, Oral Surgery and Medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hung SI, Taiwan; Palacios S, Spain S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Jie B, Yao B, Li R, An J, Zhang Y, He Y. Post-traumatic maxillofacial reconstruction with vascularized flaps and digital techniques: 10-year experience. Int J Oral Maxillofac Surg. 2020;49:1408-1415. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Bensi C, Costacurta M, Belli S, Paradiso D, Docimo R. Relationship between preterm birth and developmental defects of enamel: A systematic review and meta-analysis. Int J Paediatr Dent. 2020;30:676-686. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Schüttfort G, Höfler S, Kann G, Königs C, de Leuw P, Herrmann E, Stephan C, Haberl A. Influence of tenofovir exposure in utero on primary dentition. Eur J Pediatr. 2020;179:1761-1768. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Brignardello-Petersen R. Preterm birth seems to be associated with diagnosis of developmental enamel defects in primary dentition. J Am Dent Assoc. 2020;151:e91. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Ye J, Gong P. NGF-CS/HA-coating composite titanium facilitates the differentiation of bone marrow mesenchymal stem cells into osteoblast and neural cells. Biochem Biophys Res Commun. 2020;531:290-296. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Alkhalaf R, Neves AA, Banerjee A, Hosey MT. Minimally invasive judgement calls: managing compromised first permanent molars in children. Br Dent J. 2020;229:459-465. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Iturriaga MP, Cocio JA, Barrs VR. Cluster of cases of congenital feline goitrous hypothyroidism in a single hospital. J Small Anim Pract. 2020;61:696-703. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Malament KA, Margvelashvili-Malament M, Natto ZS, Thompson V, Rekow D, Att W. Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: Performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J Prosthet Dent. 2021;126:533-545. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Yin R, Zhao HJ, Li YC, Pan YP. [Evaluation of alveolar bone defects in patients with periodontitis with Angle Class II malocclusion and orthodontic history by cone beam CT]. Zhonghua Kouqiang Yixue Zazhi. 2021;56:769-776. [DOI] [Cited in This Article: ] |
| 10. | Meixner I, Hagl B, Kröner CI, Spielberger BD, Paschos E, Dückers G, Niehues T, Hesse R, Renner ED. Retained primary teeth in STAT3 hyper-IgE syndrome: early intervention in childhood is essential. Orphanet J Rare Dis. 2020;15:244. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Wu J, Wang WN, Yu H, Gao B. [Application of digital technology to rehabilitate a patient with tooth and dentition defects: a case report]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;55:754-756. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Wang CL, Lan ZD, Mao Q, Lin DF, Xu QJ, Liu CH. [Efficacy of Personalized Microanchorage Nail-assisted Rapid Expander in Expansion of Midpalatal Suture in Adults]. Kouqiang Jibing Yufang. 2020;28:657-663. [DOI] [Cited in This Article: ] |
| 13. | Peng K, Zhou Y, Dai Y, Wang Q, Hu Y, Dai Q. The effect of denture restoration and dental implant restoration in the treatment of dentition defect: a systematic review and meta-analysis. Ann Palliat Med. 2021;10:3267-3276. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Tian MT, Zhang MZ. [Development and Application of 3D Surgical Guide Combined with Periodontal Cortical Osteotomy]. Yixue Yanjiu Zazhi. 2020;26:738-742. [Cited in This Article: ] |
| 15. | Kramer K, Chavez MB, Tran AT, Farah F, Tan MH, Kolli TN, Dos Santos EJL, Wimer HF, Millán JL, Suva LJ, Gaddy D, Foster BL. Dental defects in the primary dentition associated with hypophosphatasia from biallelic ALPL mutations. Bone. 2021;143:115732. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Janssen NG, Schreurs R, de Ruiter AP, Sylvester-Jensen HC, Blindheim G, Meijer GJ, Koole R, Vindenes H. Microstructured beta-tricalcium phosphate for alveolar cleft repair: a two-centre study. Int J Oral Maxillofac Surg. 2019;48:708-711. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Batstone MD. Reconstruction of major defects of the jaws. Aust Dent J. 2018;63 Suppl 1:S108-S113. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Ye H, Ma Q, Hou Y, Li M, Zhou Y. Generation and evaluation of 3D digital casts of maxillary defects based on multisource data registration: A pilot clinical study. J Prosthet Dent. 2017;118:790-795. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Zhifang C, Wei Z. [Clinical application on restoration of dentition defects using tooth-alveolar bone grafts]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2016;34:364-368. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Liu CH, Mao Q, Wang CL. [Application and research progress of maxillary transverse expansion technique]. Kouqiang Jibing Yufang. 2020;28:689-697. [DOI] [Cited in This Article: ] |
| 21. | Suo WC, Zhou C, Wang HT. [Comparison of clinical application of traditional implant guide plate and 3D printed implant guide plate in dental implant restoration]. Shandong Yiyao. 2018;58:75-77. [DOI] [Cited in This Article: ] |