Oral Health Status and Dental Care of Disable Children
Rumana Nahid Ankhi1 , Mohima Benojir Hoque1* , Md Amanul Islam Bhuiyan2 , Mahmuda Akter3 and Sujoy Saha4
1Department of Public Health, ASA University, Dhaka, Bangladesh .
2Honourary Medical Officer at department of Orthodontics in Chattogram medical College, Dental Unit, Chattogram, Bangladesh .
3Department of Public Health and Human Service Administration, Fairleigh Dickinson University, Canada .
4Public Service Commission, Govt. of Peoples Republic of Bangladesh, .
Corresponding author Email: ankhident@gmail.com
DOI: http://dx.doi.org/10.12944/EDJ.04.02.05
Copy the following to cite this article:
Ankhi R. N, Hoque M. B, Bhuiyan M. A. I, Akter M, Saha S. Oral Health Status and Dental Care of Disable Children. Enviro Dental Journal 2022; 4(2). DOI:http://dx.doi.org/10.12944/EDJ.04.02.05
Copy the following to cite this URL:
Ankhi R. N, Hoque M. B, Bhuiyan M. A. I, Akter M, Saha S. Oral Health Status and Dental Care of Disable Children. Enviro Dental Journal 2022; 4(2). Available from: https://bit.ly/3RWjd56
Download article (pdf) Citation Manager
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 2022-05-15 |
|---|---|
| Accepted: | 2023-02-08 |
| Reviewed by: |
 Arezoo Alaee
Arezoo Alaee |
| Second Review by: |
 Aditi Singh
Aditi Singh |
| Final Approval by: | Dr. Shadia Elsayed |
Introduction
There are little national studies had been conducted on oral health status and dental care of children with disabilities in Bangladesh.Some studies with disable people were done with a control group. Persons with disabilities are more likely to be victims of violence or rape, according to a 2004 British study. “Children with Disabilities: Health and education Information (III) Almost all people suffer from dental problems in their life. Most of the disable people like mentally retarded, mute, speech or language impairment are unable to express their problems. Oral health is much more than healthy teeth. It includes the condition of oral cavity, teeth, gingiva, tongue, and other associated structures like buccal mucosa, salivary glands etc. Maintenance of oral hygiene is also difficult for them. So they suffer from dental diseases. As they required special management technique, they do not get the facilities from hospital because of some lacking. For the purpose of their proper care a study on these groups about their oral hygiene was conducted. It will help to rich the treatment facilities for them.
Methods and materials
A cross sectional study was conductedto assess the oral health status and dental care of children with disability through a purposive sampling technique. Data were collected from Centre for Rehabilitation and Paralyzed (CRP), Mirpur-14, Dhaka.The duration of my study period is from November-2017 to April- 2018.
Study Population
Children with disabilities and their parents who had attend at Pediatrics’ unit of CRP, Mirpur-14, Dhaka.As the study was conducted in short duration and with limited resources, the data was collected from 125 disable children.
Data collection instrument
- Torch, mirror, gloves and probe for examination.
- Disinfectant for sterilization purpose.
- Questionnaire paper.
Data collection technique
Data were collected by using a semi-structured questionnaire followed by face to face interview.
Data processing and Analysis
After collection of all data each questionnaire were checked to find whether the questionnaire was filled completely and consistently.Then all data were analyzed by following descriptive analytical method. Different tables, graphs and charts are constructed by using SPSS Statistics 17.0
Result
Children participating in the research programs were with various types of disabilities. Most of them were suffering from orthopedic impairment (28%), multiple disabilities (22%), developmental delay (18%), speech impairment (12%), mental retardation (11%), autism (5%), hearing impairment (4%), traumatic brain injury (3%), emotional disturbance (2%), deafness (1%), and other health impairment (11%).
As data collected from a rehabilitation centre there were all categorized people present from low socioeconomic condition to high socioeconomic condition. Most of disable children attending CRP, Mirpur were from lower class to higher class society.
All of the children attending in CRP followed a dietary chart given by them. Except these food 17.6% children like carbohydrates like rice, khicuri, potato etc, 22.4% like protein commonly egg and milk, 2.4% likes fatty food like fast food, 29.6% like sweet food like chocolate, sweets etc, 1.6% like carbonated beverages and juices. 25.6% children ateeverything; they did not have special choice.
59.2% of them drunks purified WASA supply water and 34.4% drunktube well water. Others drunk water from ponds and other sources like mineral water.
Most of the child was brushed their teeth every day. 80% brushedtheir teeth everyday and 20% did not brush their teeth everyday and among 20% some were never brushed their teeth.
72.8% children brushed their teeth once a day, 20% brushed their teeth twice a day and 7.2% children did not brush their teeth regularly.
64.8% brushed their teeth before breakfast, 2.4% brushed their teeth after breakfast, 1.6% brushed their teeth after lunch, 6.4% brushed their teeth after dinner and 17.4% before breakfast and after dinner ( Figure 01)
83% children brushed their teeth with toothpaste. 34.4% brushed their teeth less than 1 minute, 30% for 1 minute, 13.6% for 2 minutes, 14.4% for more than 2 minutes. 7.2% could not give specific information about their brushing duration (Table -01)
The appropriate method of brushing technique did not known by anyone. 55% brushes their teeth like brush upper teeth from above downward, lower from below upward and side to side movement, 30% side to side movement, 1% rolling the brush over teeth, 2% brush upper teeth from above downward, lower from below upward, 5% side to side movement and rolling the brush over teeth and 7% could not say about the technique (Figure -02)
39.2% changed their brush after 3 to 6 months, 35% changed brush when splay, 20% at every 2 months and 7% at every month. No one of them used electronic toothbrush and dental floss. 16% gave history of bleeding during brushing
Most common abnormal oral habit was bruxism and most of the children had multiple abnormal oral habits. 38.9% have mouth breathing, 30% have nail or object biting, 28% had thumb sucking and tongue thrusting and others have the abnormal habit like lip biting, cheek biting and unilateral mastication and there number is little (Figure-03)
11.2% were suffered from toothache, 10.4% from tooth sensitivity, 2.4% from mobility of tooth, 6.4% from gum bleeding. Calculus was found in 6.4% children, occlusal problem in 1.6%, and aesthetic problem in 7.2% children. 12% gave history of bad odor and 21.6% did not complaint for any oral health problem (Figure -04)
Table 02 shows that 34% of respondents did not follow proper oral health hygiene. They had taken care of their teeth by their own method. 20% informed by dental health professional, 18.4% by dentist, 1.6% by radio, 24% by television and 0.8% from printed materials
63% had never visited to a dentist and 20% visited dentist when they were suffered from dental pain. . 12% had visited dentist once a year and only 4% visited dentist for regular check-up.
55% do not take any treatment, 20% only receives oral check-up, 13.6% respondents have tooth restoration. 6.4% visit the dentist to extract their teeth and 4% only treated by medicine.
There was no missing teeth in 93% participants, 3% had missing deciduous tooth, 2% with missing permanent tooth and 2% did not have any tooth as they were patient of developmental delay.
On clinical examination there was 49% participants had dental caries, 19% had bleeding on probing, 10% with crowding, 8% with periodontal pocket, 7% with attrition, 4% with fluorosis and 3% with abrasion of teeth (Figure-05)
Halitosis was present in 60% of participants. Halitosis is measured by asking samples. Tongue condition was normal of 94% 0f participants. 2% of respondents had tongue tie and 2% had ulceration on tongue. Only 1% had hairy tongue and macroglossia (Figure -07)
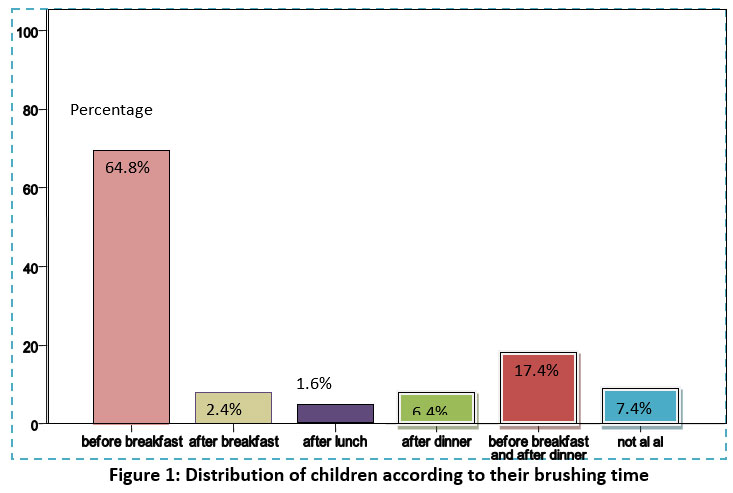 |
Figure 1: Distribution of children according to their brushing time. Click here to view Figure |
Table 1: Distribution of respondents according to the duration of their brushing teeth.
|
Duration of brushing |
Number |
Percentage |
|
Less than one minute |
43 |
34.4 |
|
One minute |
38 |
30.4 |
|
Two minutes |
17 |
13.6 |
|
More than two minutes |
18 |
14.4 |
|
Not specific |
9 |
7.2 |
|
Total |
125 |
100.0 |
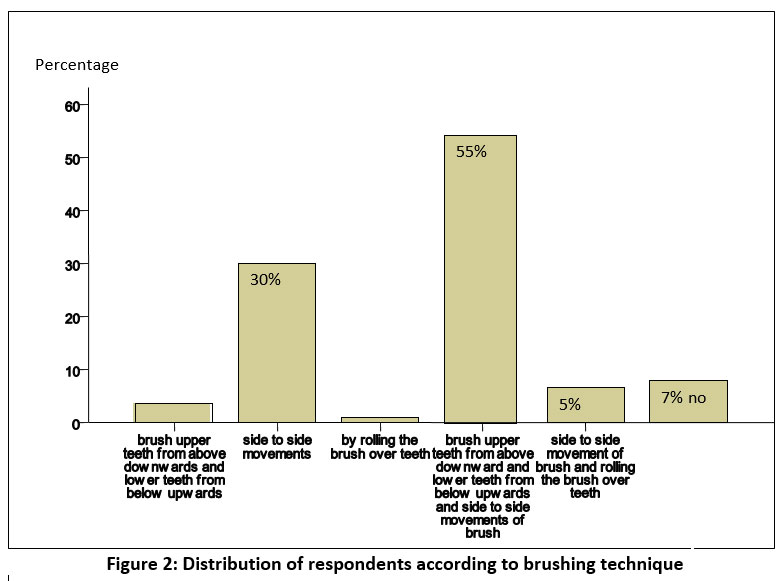 |
Figure 2: Distribution of respondents according to brushing technique. Click here to view Figure |
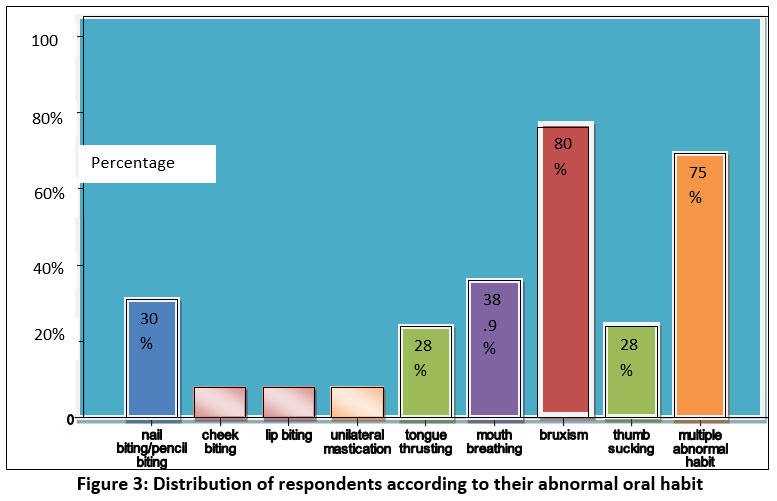 |
Figure 3: Distribution of respondents according to their abnormal oral habit. Click here to view Figure |
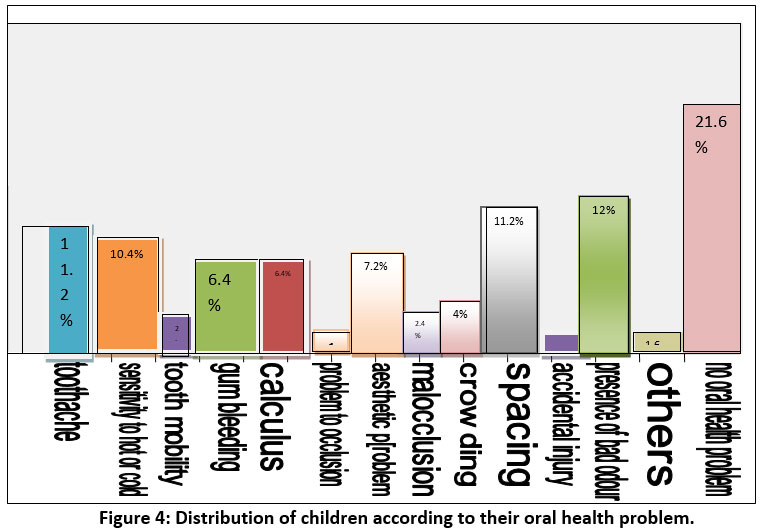 |
Figure 4: Distribution of children according to their oral health problem. Click here to view Figure |
Table 2: Distribution of respondents on the basis of their source of information, dental visit and received services
|
Source of oral health hygiene information |
Number |
Percentage |
|
Dental health personnel |
26 |
20.8 |
|
Dental health professionals |
23 |
18.4 |
|
Printed materials |
1 |
.8 |
|
Radio |
2 |
1.6 |
|
Television |
30 |
24.0 |
|
Others |
43 |
34.4 |
|
Total |
125 |
100.0 |
|
Dental visit |
Number |
Percentage |
|
Once a year |
15 |
12.0 |
|
At every six months |
6 |
4.8 |
|
When suffering from dental pain |
25 |
20.0 |
|
Never |
79 |
63.2 |
|
Total |
125 |
100.0 |
|
Dental services |
Number |
Percentage |
|
Oral checkup |
26 |
20.8 |
|
Prescribed drug |
5 |
4.0 |
|
Tooth extraction |
8 |
6.4 |
|
Tooth restoration |
17 |
13.6 |
|
No treatment |
69 |
55.2 |
|
Total |
125 |
100.0 |
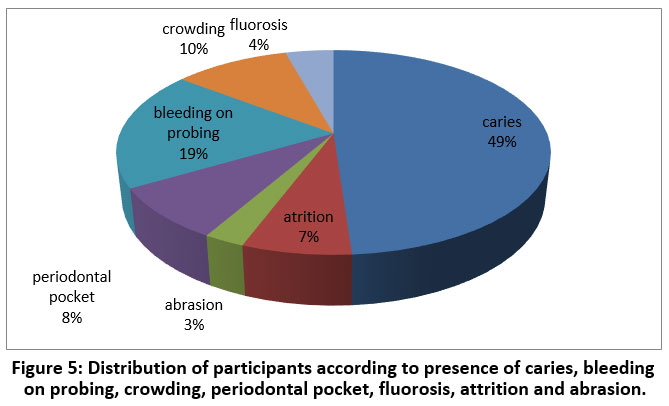 |
Figure 5: Distribution of participants according to presence of caries, bleeding on probing, crowding, periodontal pocket, fluorosis, attrition and abrasion. Click here to view Figure |
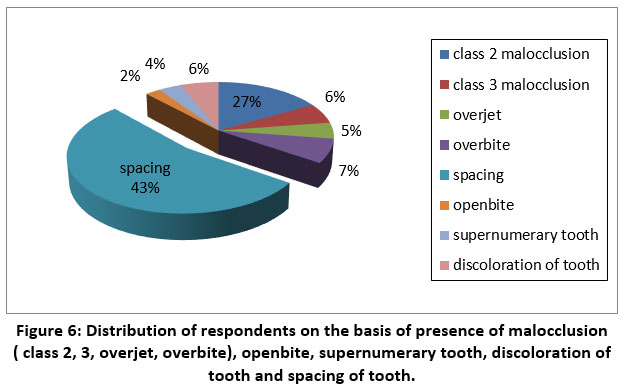 |
Figure 6: Distribution of respondents on the basis of presence of malocclusion ( class 2, 3, overjet, overbite), openbite, supernumerary tooth, discoloration of tooth and spacing of tooth. Click here to view Figure |
On clinical examination there were 27% patient with class 2 malocclusion, 43% with spacing, 7% with overbite, 6% with class 3 malocclusion, 6% with discoloration of tooth and 4% with supernumerary tooth. Respondents with open bite found only 2%.
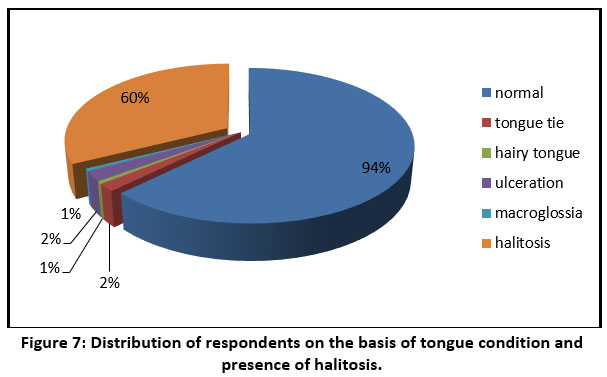 |
Figure 7: Distribution of respondents on the basis of tongue condition and presence of halitosis. Click here to view Figure |
Discussion
125 disable children were selected for the research purpose. Where the ages of the respondents were in between 7 months to 13 years. 16 children in 7 months to 2 years of age, 25 people 2 to 3 yrs of age, 22 children of 3 to 4 years, 20 of 4 to 5 years, 14 of 5 to 7 years and 28 children are of 7 to 13 years age group. Among 125 children there were 79 male and 46 female children. Most of them were illiterate because of their disability and below 5 of years old. Among the respondents 68% had mixed dentition and 32% had deciduous dentition there was no missing teeth in 93% participants, 3% had missing deciduous tooth, 2% with missing permanent tooth and 2% did not have any tooth as they were patient of developmental delay.
Children participating in the research programs were of different types of disabilities. Most of them were suffering from orthopedic impairment (28%), multiple disabilities (22%), developmental delay (18%), speech impairment (12%), mental retardation (11%), autism (5%), hearing impairment (4%), traumatic brain injury (3%), emotional disturbance (2%), deafness (1%), and other health impairment (11%).
As data were collected from a rehabilitation centre there were all categorized people present from low socioeconomic condition to high socioeconomic condition. Most of disable children attending CRP, Mirpur was from middle class to higher class society.
All of the children attending in CRP follow a dietary chart given by them. About 85% children are uncooperative with their parents to maintain their oral hygiene. Most of the children did not follow the proper brushing technique due to lack of knowledge of their parents. 7.2% could not give specific information about their brushing duration. Most of the children brush their teeth with fingers. 78.4% used tooth brush, 14.4% cleaned their teeth with fingers, .8% used meswak and 6.4% used some other methods or do not clean their teeth. I did not find anyone who knew the appropriate method of brushing technique. 55% brushed their teeth like brush upper teeth from above downward, lower from below upward and side to side movement, 30% side to side movement, 1% used to roll the brush over teeth, 2% brushed upper teeth from above downward, lower from below upward, 5% side to side movement and rolling the brush over teeth and 7% could not say about the technique. 39.2% change their brush after 3 to 6 months, 35% change brush when splay, 20% at every 2 months and 7% at every month change their brushes. No one of them use electronic toothbrush and dental floss. 16% gives history of bleeding during brushing. 67.2% children had abnormal oral habit and most common abnormal oral habit was bruxism and most of the children had multiple abnormal habits. According to data 80% children had bruxism, 75% with multiple abnormal oral habit. 38.9% had mouth breathing, 30% had nail or object biting, 28% with thumb sucking and tongue thrusting habit further others had the abnormal habit like lip biting, cheek biting and unilateral mastication and there number is little. Bruxism was the most common abnormal oral habit with bad oral hygiene. Majority of parents complaint about halitosis.
34% of respondents did not follow proper oral health hygiene. 20% had gained knowledge from dental health professional, 18.4% from dentist, 1.6% from radio, 24% by television and 0.8% from printed materials like journals, posters, books etc.63% had never visit to a dentist and 20% visited dentist when they were suffering from dental pain. . 12% visit dentist once a year and only 4% visit dentist for regular check-up.55% did not take any treatment, 20% only received oral check-up, 13.6% respondents had tooth restoration. 6.4% visited the dentist to extract their teeth and 4% only treated by prescribed drugs.
On clinical examination there was 49% participants had dental caries. Fahlvik-Planefeldt and Herrström observed a lower number of caries in autistic children (50% with caries compared to 70% in the control group) but without specifying the significance , while Namal et al. and Fakroom et al. did observe significant differences, with the former author even affirming that not having autism supposed a 3.99 times greater predisposition to dental caries. (I) 19% had bleeding on probing, 10% with crowding, 8% with periodontal pocket, 7% with attrition, 4% with fluorosis and 3% with abrasion of teeth. There were 27% patient with class 2 malocclusion, 43% with spacing, 7% with overbite, 6% with class 3 malocclusion, 6% with discoloration of tooth and 4% with supernumerary tooth. Respondents with open bite found only in 2%. Halitosis was present in 60% of participants. Tongue condition was normal of 94% 0f participants. 2% of respondents had tongue tie and 2% had ulceration on tongue. Only 1% had hairy tongue and macroglossia.
There was no participants with cleft lip or palate and with dentures. There was a similarity of my findings with the findings of El Khabit et al. Richaetal.and Al-Maweri et al. about severity of bruxism.(I)”
Conclusion
Disable children are much uncooperative to maintain their oral hygiene. Parents are always busy to take care of them according to the disability and do not give enough attention about oral hygiene. Though most of the parents help their child to brush their teeth but they do not know the appropriate brushing technique. As a result halitosis and plaque is present in their mouth. As in my study caries is present in only 49% participants but it will be increase with the time because of their bad oral hygiene . Attrition is only in 7% but bruxism presents in about 80% children, so caries and attrition will be increase in them with time.
Recommendations
After doing the study I have found that oral health status of the disable children is very bad and they do not know to take proper dental care. To improve this condition I want to recommend following steps:
- Arrangement of oral health program for all people because everyone should be aware about oral health.
- Special program for the disable children with their mother and father about brushing technique.
- Dental professionals should give special attention to disable children.
- As there is increased frequency of abnormal oral habit so habit breaking appliance should be introduced with the parents of disable children.
Acknowledgments
I would like to thank ASA University for granting the masters research work. The Department of Public Health, ASA University, Dhaka Bangladesh is highly appreciated for allowed the research work. I also profoundly grateful to the CRP, Mirpur, Dhaka, Bangldesh for their cooperation during the data collection procedure.
Conflict of Interest
There is no conflict of interests
Funding Sources
The author received no financial support for the research, authorship, and/or publication of this article.
References
- BegoñaBartolomé-Villar 1, Mª Rosa Mourelle-Martínez 2, Montserrat Diéguez-Pérez 3, Manuel-Joaquín de Nova-García 4. Incidence of oral health in paediatric patients with disabilities: Sensory disorders and autism spectrum disorder. Systematic review II. J ClinExp Dent. 2016;8(3):e344-51.
- Ceyhan Altuna Gunseli Guvena Ozlem Marti Akgunb Meltem Derya Akkurtb Feridun Basaka Erman Akbulutc. Oral Health Status of Disabled Individuals Attending Special Schools. European Journal of Dentistry, pp.381-95.
- Children with Disabilities: Health and Education Information ...https://www.disabled-world.com/disability/children/
- Eno Gaçe1, Manola Kelmendi2, Enika Fusha3. Oral Health Status of Children with Disability Living in Albania. 393Mater Sociomed. 2014 Dec; 26(6): 392-394,pp.392-94.
CrossRef - GagandeepMohinderpal Chadha, PradnyaKakodkar, VishwasChaugule, VidyaNimbalkar. Dental Survey of Institutionalized Children with Autistic Disorder. International Journal of Clinical Pediatric Dentistry, January-April 2012;5(1):29-32.
CrossRef - *ISIlÖzgül KALYONCU, IlknurTANBOGA ,18 Jan 2017. Oral Health Status of Children with Autistic Spectrum Disorder Compared with Non-authentic Peers. Iran J Public Health, Vol. 46, No.11, Nov 2017, pp. 1591-1593.
- My Blomqvist1*, Susanne Bejerot2,3 and Göran Dahllöf1. A cross-sectional study on oral health and dental care in intellectually able adults with autism spectrum disorder. Blomqvist et al. BMC Oral Health (2015) 15:81 DOI 10.1186/s12903-015-0065-z,pp.1-8.
CrossRef
.jpg)




