Peri-Implantitis; What is in a Name?
Mihir Raghavendra Kulkarni
1Department of Periodontics, SDM College of Dental Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Sattur, Dharwad, India .
Corresponding author Email: mihir.mrk271@gmail.com
DOI: http://dx.doi.org/10.12944/EDJ.04.01.02
Copy the following to cite this article:
Kulkarni M. R. Peri-Implantitis – What is in a Name?. Enviro Dental Journal 2022; 4(1). DOI:http://dx.doi.org/10.12944/EDJ.04.01.02
Copy the following to cite this URL:
Kulkarni M. R. Peri-Implantitis – What is in a Name?. Enviro Dental Journal 2022; 4(1). Available From: https://bit.ly/3yn3V03
Download article (pdf) Citation Manager
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 08-06-2022 |
|---|---|
| Accepted: | 15-06-2022 |
| Final Approval by: | Dr Darpan Bhargava |
Definitions, nomenclature, terminology and other exercises of naming or describing things have been an inseparable part of science. While a litterateur may ponder the oft quoted Shakespearean question, “What’s in a name?” for scientific enquiry, name is everything. Periodontal literature is no stranger to the rigors of changing nomenclature. The disease entity currently called “Periodontitis” itself has seen a long process of updates in nomenclature, ranging from periodontoclasia, periodontosis, adult periodontitis, chronic periodontitis to the present term of “Periodontitis”.1, 2, 3
Peri-implantitis is one of the important diseases that can lead to the destruction of the bone supporting a dental implant and can eventually lead to the late failure of an osseointegrated dental implant.
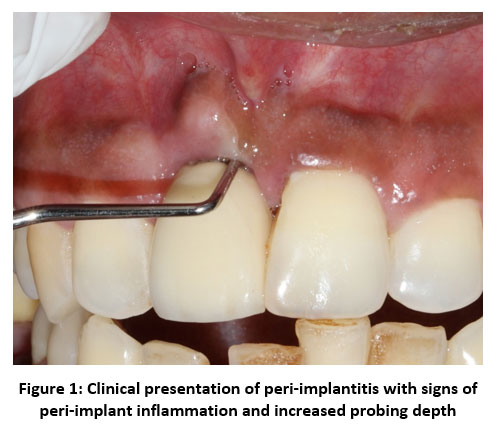 |
Figure 1: Clinical presentation of peri-implantitis with signs of peri-implant inflammation and increased probing depth |
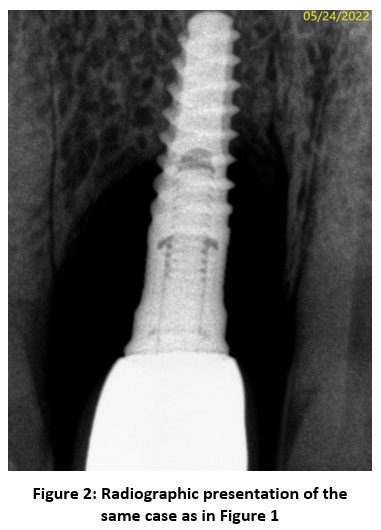 |
Figure 2: Radiographic presentation of the same case as in Figure 1 |
Peri-implant mucositis and peri-implantitis are a continuous disease spectrum and peri-implantitis can occur if peri-implant mucositis is left un-treated. Both these conditions are by definition a sequalae of dental biofilm induced inflammation.3 The diagnosis of peri-implantitis should be based on “combined outcome measures” including clinical as well as radiographic parameters and must not be based only on marginal bone level data.4 If due consideration is not given to clinical signs of inflammation, it is easy to mistake a case of normal crestal bone remodeling as one of peri-implantitis.
Functional remodeling of alveolar bone is a well-documented process that occurs early in the life of an osseointegrated implant.5 Excessive early crestal bone loss may occur due to factors such as improper positioning of the implant, lack of keratinized mucosa, extruded luting cement, excessive insertion torque, excessive surgical trauma to the bone, implant/abutment design characteristics and periimplantitis.6 Transient crestal de-mineralization can also appear as early bone loss.7 This indicates that factors other than the microbial biofilm, can cause crestal bone loss and such instances need to be separated from the clinical diagnosis of peri-implantitis.
Removal of the microbial plaque and plaque retentive factors is the mainstay of the management of peri-implantitis, and regeneration of the lost supporting structures always follows this. On the other hand, if factors other than the biofilm have induced the peri-implant bone loss, it is imperative to identify these factors so that the etiology can be addressed.
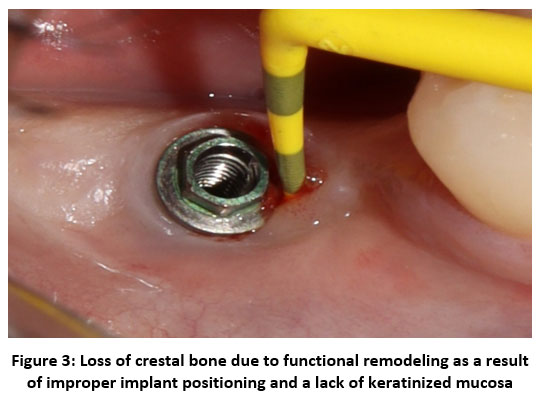 |
Figure 3: Loss of crestal bone due to functional remodeling as a result of improper implant positioning and a lack of keratinized mucosa. |
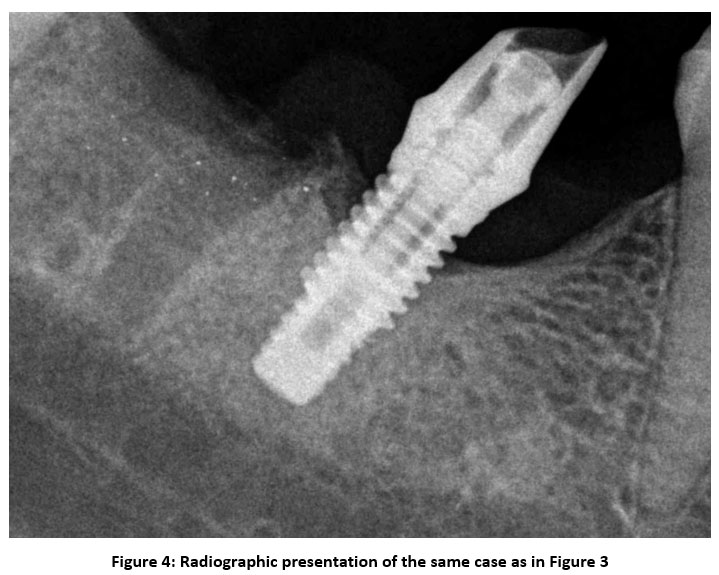 |
Figure 4: Radiographic presentation of the same case as in Figure 3. |
Also, mis-labeling any bone-loss as peri-implantitis may lead to over-treatment of the affected sites. If the bone loss is a part of functional remodeling, or re-establishment of peri-implant biologic width, it may not need to be treated at all.
It is vital for clinicians to understand that a mistake in nomenclature can change the entire treatment plan and prognosis and lead to un-favorable outcomes or iatrogenic injury. Hence, any peri-implant bone loss should always be examined in the context of clinical signs of inflammation and not directly labelled as peri-implantitis. Periodic radiographic assessment of crestal bone levels should be a part of routine post-implant maintenance care so that a timely and appropriate intervention can be done to extend the clinical service of an osseointegrated dental implant.
References
- Gracey CH, Hine MK, et al. Nomenclature in periodontia. J Periodontol. 1947; 18:112-4.
CrossRef - Flemmig TF. Periodontitis. Ann Periodontol. 1999; 4:32-8.
CrossRef - Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M, Tonetti MS. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018; 45:S1-S8.
CrossRef - Schwarz F, Alcoforado G, Guerrero A, Jönsson D, Klinge B, Lang N, Mattheos N, Mertens B, Pitta J, Ramanauskaite A, Sayardoust S, Sanz-Martin I, Stavropoulos A, Heitz-Mayfield L. Peri-implantitis: Summary and consensus statements of group 3. The 6th EAO Consensus Conference 2021. Clin Oral Implants Res. 2021; 32:245-253.
CrossRef - Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11-25.
- Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: myth or science? J Periodontol. 2002; 73:322-33.
CrossRef - Puisys A, Auzbikaviciute V, Minkauskaite A, Simkunaite-Rizgeliene R, Razukevicius D, Linkevicius R, Linkevicius T. Early crestal bone loss: Is it really loss? Clin Case Rep. 2019; 7:1913-1915.
CrossRef
.jpg)




