Minimally Invasive Technique for Removal of a Mandibular Radicular Cyst : A Case Report
Hattan Zaki1 , Albraa B. Alolayan1 , Weam Mohammed Ahmed1 , Ebtihal Zain Alabdeen1 and Shadia Abdel-Hameed Elsayed1,2
1Taibah University Dental College and Hospital, Al-Madinah Al-Munawwrah, Saudi Arabia .
2Faculty of Dental Medicine for Girls, Al-Azhar University, Cairo, Egypt .
Corresponding author Email: shadiaelsayed@azhar.edu.eg
DOI: http://dx.doi.org/10.12944/EDJ.03.01.04
Copy the following to cite this article:
Zaki H, Alolayan A. B, Ahmed W. M, Alabdeen E. Z, Elsayed S. A. H. Minimally Invasive Technique for Removal of a Mandibular Radicular Cyst: A Case Report. Enviro Dental Journal 2021; 3(1). DOI:http://dx.doi.org/10.12944/EDJ.03.01.04
Copy the following to cite this URL:
Zaki H, Alolayan A. B, Ahmed W. M, Alabdeen E. Z, Elsayed S. A. H. Minimally Invasive Technique for Removal of a Mandibular Radicular Cyst: A Case Report. Enviro Dental Journal 2021; 3(1). Available From : https://bit.ly/3zNTUYK
Download article (pdf) Citation Manager
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 17-04-2021 |
|---|---|
| Accepted: | 25-06-2021 |
| Reviewed by: |
 Dr. Madhusudhan K
Dr. Madhusudhan K |
| Second Review by: | Dr. Ujjwal Koirala |
| Final Approval by: | Dr. Hitesh Vij |
Introduction
A large percentage of the work of oral and maxillofacial surgeons involves the management of radicular cysts. Cystic jaw lesions are characterized as non-painful, slow-growing lesions, unless they have been infected, with radiographic features such as well-defined corticated borders. A unique pathognomonic feature of these lesions is that cystic fluid can be aspirated from them.1 The traditional cyst enucleation approach required access by mucoperiosteal flaps and bone removal, particularly if the lesion overlying cortex was still intact. The procedure may be followed by apicoectomy or tooth extraction after complete lesion enucleation. Current good clinical practice for patients is to ensure that every treatment is simple. For both the patient and the operator, complexity often contributes to difficulty.2 Therefore, in this report, we present a simple intra-socket cystic removal technique that allows optimal outcome yet gives the patient the most comfortable surgical experience.
Case Report
An 18-year-old Asian female patient was referred to the specialty clinic of the Oral and Maxillofacial Surgery Department at Taibah University in Madinah, Saudi Arabia, for extraction of a badly decayed lower left second molar (Figure 1).
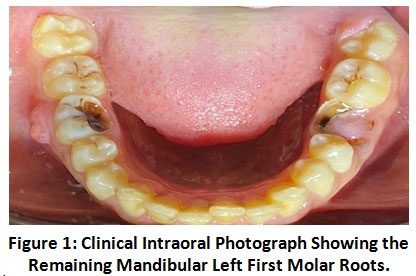 |
Figure 1: Clinical Intraoral Photograph Showing the Remaining Mandibular Left First Molar Roots. Click here to view Figure |
After a thorough clinical examination of the patient and an initial radiographic examination of the orthopantomogram, we found a well-circumscribed periapical radiolucent lesion that had well-defined corticated margins. It correlated to the remaining root apices of tooth #36 (Figure 2). The lower boundary of the lesion was hyperdense.
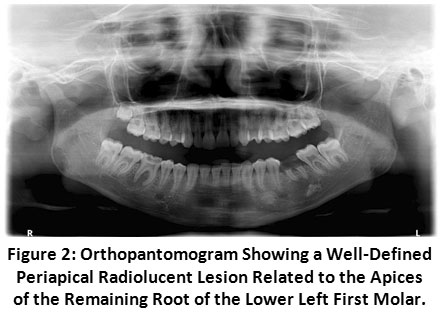 |
Figure 2: Orthopantomogram Showing a Well-Defined Periapical Radiolucent Lesion Related to the Apices of the Remaining Root of the Lower Left First Molar. Click here to view Figure |
Cone beam computed tomography (CBCT) identified a radicular radiolucent lesion with a width of 14.7 mm and a height of 8.2 mm (Figure 3).
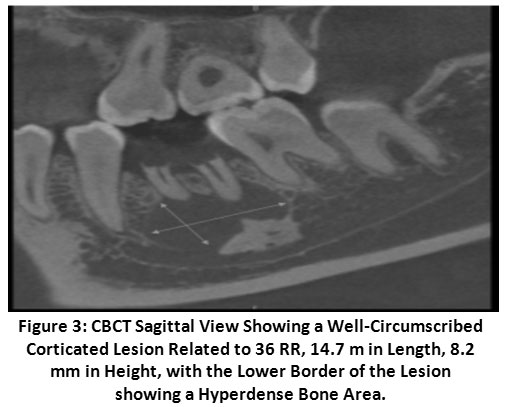 |
Figure 3: CBCT Sagittal View Showing a Well-Circumscribed Corticated Lesion Related to 36 RR, 14.7 m in Length, 8.2 mm in Height, with the Lower Border of the Lesion showing a Hyperdense Bone Area. Click here to view Figure |
The differential diagnosis of a periapical radiolucency with an ossified border included a radicular cystic lesion with a sclerotic border or a periapical sclerotic border granuloma.3–5 We discussed the procedure with the patient, who signed informed consent on the day of the surgery.
Management
The procedure was performed under local anesthesia. The results of the aspiration test were negative and we decided to begin the procedure by extracting the remaining roots. After simple extraction via luxation using apexo and then cross-bar elevators, we inspected the site and decided to enucleate the lesion without using any mucoperiosteal flaps through the extraction socket itself.
Using universal bone rongeurs, we removed the intervening interseptal bone. We started lesion enucleation occlusally and deepened it by using a bone curette with the aid of a large piece of gauze that was also used to push the curette. This technique was repeated on each side of the bony socket. The bony boundaries of the socket were very clean and during the process, the gauze also assisted in achieving hemostasis (Figures 4, 5).
After full excision of the lesion, we sutured the socket with two interrupted non-resorbable sutures on the hemostatic gel only, as we did not use any graft in this case. The patient was given post-extraction instructions and antibiotics and analgesics were administered. After 1 week, the sutures were removed.
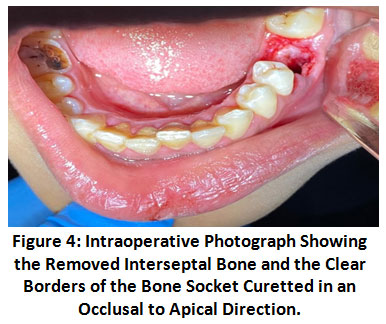 |
Figure 4: Intraoperative Photograph Showing the Removed Interseptal Bone and the Clear Borders of the Bone Socket Curetted in an Occlusal to Apical Direction. Click here to view Figure |
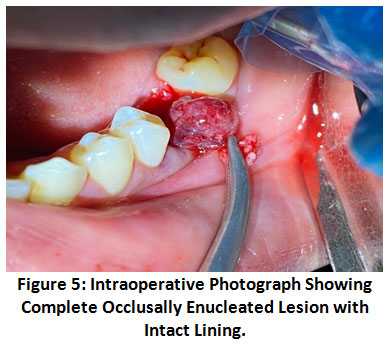 |
Figure 5: Intraoperative Photograph Showing Complete Occlusally Enucleated Lesion with Intact Lining. Click here to view Figure |
The excised lesion was immediately placed in 10% formalin and submitted to the histopathological department. The final biopsy report indicated a cystic process lined with stratified squamous epithelium marked by lymphocytic exocytosis and spongiosis. Connective tissue capsules revealed areas of hemorrhage, hemosiderin pigmentation, multinucleated giant cells that engulf cholesterol, and inactive odontogenic epithelium (Figure 6).
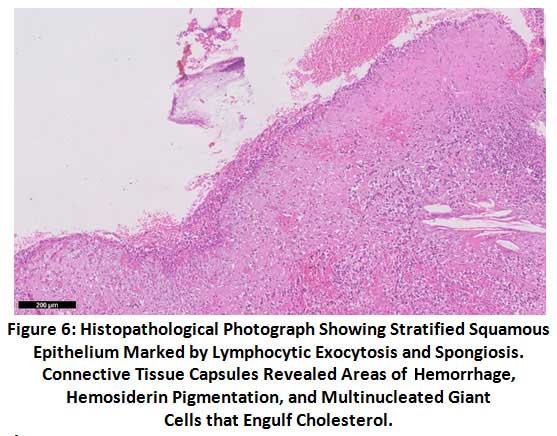 |
Figure 6: Histopathological Photograph Showing Stratified Squamous Epithelium Marked by Lymphocytic Exocytosis and Spongiosis. Connective Tissue Capsules Revealed Areas of Hemorrhage, Hemosiderin Pigmentation, and Multinucleated Giant Cells that Engulf Cholesterol. Click here to view Figure |
Discussion
Cystic lesions accompanied by areas of calcification have recently been reported to grow as a foreign body reaction in young patients, including in populations in Saudi Arabia as reported by Elsayed et al.6,7 The intra-socket method described in this report was our department’s first experience in using this approach. This method has the potential to prevent most postoperative complications precipitated by traumatic surgery itself, such as postoperative discomfort, edema, and reduced opening of the mouth. In addition, it may accelerate surgical intervention.3,8
One of the most important developments in dentistry in the last decade is CBCT. It can significantly improve the diagnosis and recovery planning of patients when used properly. CBCT may correctly describe the dimension, shape, and extent of a periapical lesion.9,10
Enucleation of the radicular cyst through the extraction socket in the posterior mandibular region is not a traditional method, but it has shown good accessibility because of the broad access through the remaining molar root site. It is difficult to remove a cystic lesion through the narrow sockets of other anterior or premolar areas. Being wider buccolingually and mesiodistally, the posterior mandibular region is a more appropriate site to use.
References
- Miloro M, Ghali GE, Larsen PE, Waite P. Peterson’s principles of oral and maxillofacial surgery. 3rd ed. London: People’s Medical Publishing House; 2012.
- Dandotikar D, Peddi R, Lakhani B, Lata K, Mathur A, Chowdary UK. Nonsurgical management of a periapical cyst: a case report. J Int Oral Health 2013;5:79–84.
- Martin LHC, Speight PM. Odontogenic cysts: an update. Diagnostic Histopathol 2017;23:260–5. https://doi.org/https://doi.org/10.1016/j.mpdhp.2017.04.006.
CrossRef - Karakasis DT, Ainatzoglou MD. Ossification in the wall of a radicular cyst: report of a case. J Oral Maxillofac Surg 1989;47:853–5. https://doi.org/https://doi.org/10.1016/S0278-2391(89)80046-1.
CrossRef - Shuff N, Jagtap R, Hansen M, Ruprecht A, Kashtwari D. Rare presentation of radicular cyst with review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:e67–8. https://doi.org/https://doi.org/10.1016/j.oooo.2020.03.030.
CrossRef - Elsayed S, Alolayan A, Farghal L, Ayed Y. Generalised hypercementosis in a young female seeking extraction: revision and update of surgical technique. J Coll Physicians Surg Pakistan 2019;29:1111–3. https://doi.org/10.29271/jcpsp.2019.11.1111.
CrossRef - Elsayed SA, Ayed Y, Alolayan AB, Farghal LM, Kassim S. Radiographic evaluation and determination of hypercementosis patterns in Al-Madinah Al-Munawwarah, Saudi Arabia: a retrospective cross-sectional study. Niger J Clin Pract 2019;22:957–60. https://doi.org/10.4103/njcp.njcp_614_18.
CrossRef - Weber M, Ries J, Büttner-Herold M, Geppert C-I, Kesting M, Wehrhan F. Differences in inflammation and bone resorption between apical granulomas, radicular cysts, and dentigerous cysts. J Endod 2019;45:1200–8. https://doi.org/https://doi.org/10.1016/j.joen.2019.06.014.
CrossRef - Elsayed SA, Althagafi N, Bahabri R, Alshanqiti MM, Alrehaili AM, Alahmadi AS. Retrospective radiographic survey of unconventional ectopic impacted teeth in Al-Madinah Al-Munawwarah, Saudi Arabia. Open Access Maced J Med Sci 2020;8:203–8. https://doi.org/10.3889/oamjms.2020.4533.
CrossRef - Niraj LK, Patthi B, Singla A, Gupta R, Ali I, Dhama K, et al. MRI in dentistry: a future towards radiation free imaging – systematic review. J Clin Diagn Res 2016;10:ZE14–9. https://doi.org/10.7860/JCDR/2016/19435.8658.
CrossRef
.jpg)




