Abstract
Background:
Erection is a dynamic multi-stage neurovascular phenomenon consisting of 4 phases. Conventional protocol of color Doppler study can easily overlook these ongoing dynamic events.Objectives:
Here, we tried to designate patterns for these dynamic spectral waveform changes of cavernosal arteries in patients with erectile dysfunction and subsequently better describe the extent of their underlying problem.Patients and Methods:
We evaluated 59 men who were referred for post-intracavernosal injection (ICI) color Doppler investigation of suspected erectile dysfunction (ED). The demographic data and medical history were recorded. Afterwards, first scan injection was done. Then scanning of cavernosal arteries was started about one minute after the injection and was continued thereafter. For better description of temporal changes in the waveform of cavernosal arteries, new patterns were defined and used. Patients were also classified based on previously known etiologic categories (i.e. arterial insufficiency, venous leak, mixed type, and normal response).Results:
The mean age was 45.6 ± 13.1 (24 to 74 ) years. Twenty-two were normal responders [considered as non-organic causes (37.3% of all patients)], 27 were classified as venous leakage, eight had arterial insufficiency and two were mixed type. Maximum PSV occurred before the fifth minute in 47 patients (92.2%). Eight patients completed all phases of erection in the first 5 minutes. We defined 8 patterns for the temporal changes in cavernosal arterial waveform. Pattern 5 was the most common pattern of venous leak; while, patterns 3 and 4 were considered as the uncommon group. Six patients demonstrated the uncommon patterns of venous leak (22.2%). Hypertension was more prevalent in the uncommon pattern of venous leak.Conclusions:
We highlight the considerable role of continuous evaluation starting one minute after intra cavernosal with ICI injection of the vasoactive agent for better description of the underlying pathologies of ED especially in patients with venous leak etiology.Keywords
1. Background
Nowadays color Doppler study of corpus cavernosum (CC) with intracavernosal injection (ICI) of vasoactive agents is the first step to investigate etiologic causes of male erectile dysfunction (ED) (1, 2). Diagnostic criteria are based mostly on the peak systolic velocity (PSV) and end diastolic velocity (EDV) values of the cavernosal artery spectral waveform that were first measured 5 minutes after injection and then repeated every 5 minutes afterward up to 30 minutes (1-4). However, erection is a multi-stage neurovascular phenomenon that needs the fine balance of contractile properties of trabecular smooth muscles in the CC. It consists of these phases: filling, congestion, rigidity and full erection (1). Noteworthy to know is that in most of the patients, maximum PSV happens in the first 5 minutes; moreover, in a minority of patients all the process of changes happen in the first 5 minutes (5). Conventional protocol of color Doppler study can easily overlook these ongoing dynamic events. For better description of these dynamic changes, we got an idea from the study of Fitzgerald al. (5) and tried to designate dynamic patterns for spectral waveform changes of cavernosal arteries in each patient.
2. Objectives
In this study, we tried to classify our patients based upon their patterns of changes in a dynamic study and to subsequently better describe their underlying problem.
3. Patients and Methods
This case series study was conducted in Hasheminejad Urology Center, Iran University of Medical Sciences (IUMS), from April 2011 till April 2012. We evaluated 59 men who were referred from a urology clinic for post-ICI color Doppler investigation of suspected ED.
The stages of the test and possible role of the study in their therapeutic plan were described comprehensively for each patient and then a written consent was obtained. The demographic data and medical history including duration of ED, history of diabetes, hypertension, cigarette smoking, drug history and previous interventions for vascular diseases were recorded. One of this study investigators (Gharib, MH.) performed all examinations with a linear (5-10 MHz) probe of ESAOTE Technos device (Italy, 2002). All tests were done in a private room. The probe was placed over the ventral aspect of the penis and scans were performed in longitudinal and transverse planes before injection of the vasoactive agent. We used papaverine hydrochloride because of the availability and acceptable price. For post-ICI assessment, first a maximum dose of 40 mg papaverine was injected into the right corpus covernosum, at the junction between the middle and distal third of the penile dorsal aspect. If maximum PSV did not reach 30 cm/s in 5 minutes, further injections of 20 mg doses of papaverine were also performed, up to a maximum total dose of 80 mg. Scanning started about one minute after the injection and each of the cavernosal arteries was evaluated continuously thereafter until either erection happened or PSV started to decline. Parameters such as PSV, EDV, minimum of resistive index (RI) and time to reach maximum PSV were recorded. Angle-corrected spectral traces were recorded continuously for subsequent evaluations. After the assessment, we observed patients for probable complications. If full erection happened, the patient was under observation and if erection persisted for more 3 hours, the patient was sent to the urologic emergency room for appropriate interventions.
Based on temporal changes in the waveform of cavernosal arteries, new patterns were defined. Patients were classified based on previously known etiologic categories (i.e. arterial insufficiency, venous leak, mixed type, and normal response) and also categorized into these new patterns. Data were entered into SPSS 18 software for statistical analysis.
4. Results
Fifty-nine patients with the mean age of 45.6 ± 13.1 (24 to 74) years were enrolled into this study. Twenty-two cases revealed normal response (non-organic causes as 37.3%), 27 were classified as venous leakage, eight with arterial insufficiency and two were considered as mixed type. The mean time to reach maximum PSV was 3.4 ± 0.8 minutes (median 3, range 2-5 minutes) in 51 patients without arterial insufficiency. Maximum PSV occurred before the fifth minute in 47 (92.2%). We defined 8 patterns for the temporal changes in cavernosal arterial waveform in our patients (Table 1). For classification, we considered four different aspects in our study:
1) Sufficiency of cavernosal arteries [for judgement of this sufficiency, we considered points such as maximum PSV during the study (cut point of 30 cm/s), amount of difference of PSV between the two sides (below or above 10 cm/s), acceleration time of each waveform (cut point of 80 ms) and pattern of blood filling in the arteries]
2) Competent filling of sinusoidal blood pools [including qualitative assessment of EDV (considered as satisfactory or not) and duration of EDV rise (at least one minute)]
3) Veno-occlusive capability of corpus cavernosum [even though a clinically assessed full erection is the best determinant. In Doppler study, long time persistence of vigorous diastolic flow (EDV more than 5 cm/s) would be the indicator].
4) Finally, how long did it take the study to be finished (below or above 5 minutes). We defined a PSV level more than 40 cm/sec as a requisite to consider the patient as having venous leak with no arterial component based on Benson et al. studies (6, 7). Those patients with a PSV between 30 and 40 who did not elicit erection were placed in category 2 under the label of mixed type. Patterns 3, 4 and 5 denote to previously known venous leak group and patterns 6, 7 and 8 are patients with normal response.
Distinguishing Features of the Eight Patterns Based on Data Obtained During a Dynamic Study
| Pattern | Max PSV a, Cm/s | Arterial Sufficiency | Sinusoidal Filling Competency | Veno-Occlusive Capability | Full Erection | Time Duration, min | Label |
|---|---|---|---|---|---|---|---|
| 1 | < 30 | No | No | No | No | > 5 | Arterial insufficiency |
| 2 | 30-40 | No | No | No | No | > 5 | Mixed |
| 3 | > 40 | Yes | No | No | No | < 5 | Venous leak (uncommon) |
| 4 | > 40 | Yes | No | No | No | > 5 | Venous leak (uncommon) |
| 5 | > 40 | Yes | Yes | No | No | > 5 | Venous leak (common) |
| 6 | > 40 | Yes | Yes | Yes | Yes | < 5 | Normal |
| 7 | > 40 | Yes | Yes | Yes | Yes | > 5 | Normal |
| 8 | < 30 | Yes | Yes | Yes | Yes | > 5 | Micropenis |
Table 2 shows the patient classification based on various patterns of arterial spectral waveform changes. Among all, 8 patients completed all phases of erection in the first 5 minutes (one with pattern 3 and 7 with pattern 6). Pattern 5 was considered as the common pattern of venous leak; while patterns 3 and 4 were considered as the uncommon group. In our study, six patients demonstrated the uncommon patterns of venous leak (22.2% of all patients with venous leak).
Information Regarding Various Patterns of Changes in the Spectral Waveform of Cavernosal Arteries a
| Defined Temporal SPECT Patterns in the Cavernosal Artery | ||||||||
|---|---|---|---|---|---|---|---|---|
| Pattern 1 | Pattern 2 | Pattern 3 | Pattern 4 | Pattern 5 | Pattern 6 | Pattern 7 | Pattern 8 | |
| Arterial Insufficiency | 8 (100) | - | - | - | - | - | - | - |
| Venous Leak | - | - | 1 (3.7) | 5 (18.5) | 21 (77.8) | - | - | - |
| Mixed Type | - | 2 (100) | - | - | - | - | - | - |
| Normal Response | - | - | - | - | - | 7 (31.8) | 14 (63.6) | 1 (4.6) |
Table 3 demonstrates comparison between patients with common and uncommon patterns of venous leak. The mean of PSV was not different between these two groups (57.7 vs. 52.5 cm/s, P = 0.38). Mean age and minimum recorded RI were higher in the uncommon group, although they did not show statistical significance (P = 0.14 and 0.22, respectively). Hypertension was more prevalent in the uncommon pattern of venous leak (P = 0.01). Smoking was more prevalent in patients with uncommon patterns; however, the difference was not statistically significant (P = 0.29). We detected one patient with micropenis who demonstrated normal pattern of changes in response to papaverine even though with a maximum PSV under 30 cm/s. We referred 5 patients to the emergency department because of prolonged erection. All of them were managed successfully without any sequel.
5. Discussion
In this study, we investigated continuous assessment of cavernosal arterial waveforms of patients with ED in comparison with its routine Doppler evaluation. The conventional method of post ICI of papaverine color Doppler study includes recording PSV and EDV values in the cavernosal artery spectral waveform 5 minutes after injection which is repeated every 5 minutes afterward up to 30 minutes (1, 4). We found that in most patients (92.2%), maximum PSV happened before the fifth minute. Fitzgerald et al. also showed this finding in a considerable percent of their patients (76%) (5). This emphasizes the need for early initial assessment of flow in cavernosal artery after the injection of papaverine.
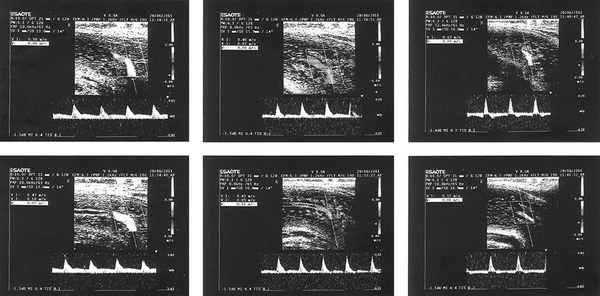
Four stages are defined for a process of penile erection. They are filling, tumescence, rigidity and full erection (1, 3, 4, 8). It is obvious that these events will result in a sequence of changes in the waveform of cavernosal artery. A process that can be chased meticulously in a continuous color Doppler protocol (Figure 1). Conventionally four groups of responses have been defined: arterial insufficiency, venous leak, normal response and a mixed pattern (9). For better delineation of dynamic changes during ultrasonography, we got the idea of categorizing waveform pattern changes during continuous assessment from the study conducted by Fitzgerald et al. (5) and defined 8 patterns of changes for arterial spectral waveform. In our classification, we considered subgroups for patients with the uncommon pattern of venous leak and those with normal response based on the response within the first 5 minutes after injection or thereafter (patterns 3 and 4; and patterns 6 and 7 respectively).
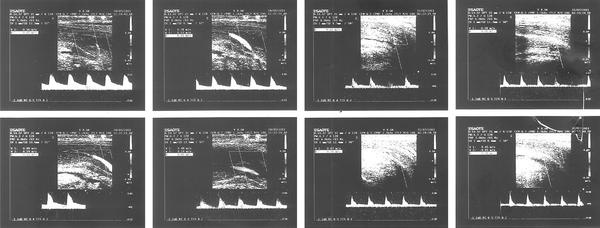
Sequence of changes was tracked in a continuous color doppler study in a normal responder (pattern 7)
We noticed that all phases of the response to papaverine occurred within the first 5 minutes in 13.8% of our patients (1 with pattern 3 and 7 with pattern 6). In conventional practice, for patients with pattern 3, we might need to repeat the injection or just judge based on the clinical fact that erection has not happened. The scenario is the same for cases with pattern 6. With maximum rigidity, systolic velocity starts to decline and the arterial system, especially helicine arterioles become progressively less visible (4). So here, we were not able to designate a normal response based on the findings of the study and just the occurrence of full erection would be the clue for our normal reports. These findings again clarify the importance of careful observation of changes both continuously and from the early beginning. We used to designate 4 groups to our patients based upon findings in the conventional study. In fact in the conventional study, the sufficiency of the arterial system and veno-occlusive mechanisms of corpus cavernosum are the mainstay of classification; however, we think that one more aspect should be delicately followed in the process of erection, and that is the appropriate reaction of sinusoidal blood pools in each CC. An important outcome of this dynamic study is distinction between patients formerly designated as having “venous leak”. Normally, a marked increase in PSV should result in concomitant significant rise in the diastolic blood flow. We believe that patterns 3 and 4 are related to a more decreased amount of trabecular smooth muscles and/or a change in the fibroelastic composition of CC, what we considered as the competency of filling of sinusoidal blood pools or in other words, effective congestion. Consequently, in color Doppler study, the diastolic flow will not rise to a favorable amount for an acceptable duration (Figure 2). These patients, although few (6 patients in this study), seem to have more aggravated problems and would not have a satisfactory response to common medications used for venous leak and should be directed for prosthesis placement. The meanage and the lowest recorded RI are higher in this group of venous leak, which we labeled arbitrarily as the uncommon group, compared to the common group (54.5 vs. 46.3 and 77.7 vs. 74.3, respectively). Although possibly due to the small number of patients, they did not show statistical significance (P value 0.14 and 0.22, respectively). We used minimum recorded RI as a measure for diastolic flow in patients. The probable extensive changes in tissue texture of patients with uncommon venous leak would result in a lesser degree of diastolic flow compared to the common pattern. As the patient grows older, the ratio of collagen type 3 (the elastic one) counts down and collagen type 1 gradually replaces it. Moreover, the content of trabecular smooth muscle also decreases up to 35% (1). The above mentioned changes would result in non-compliant sinusoids. We showed that the prevalence of systemic hypertension was statistically higher in this group. Hypertension and smoking have been introduced as other important factors involved in the extent of changes in the tissue texture of CC (1). However, in our study the prevalence of smoking was still not statistically significant in the uncommon venous leak group (P = 0.29). We think that the amount and duration of smoking (quantified in pack-year) may alter the pattern of response in patients with venous leak. As the pack-year of smoking inflates, the extent of tissue component alterations would increase. We had one patient that showed erection with PSV values below 30 cm/sec. He was a case of micropenis. The amount of blood flow directed to CC depends on the volume of recipient sinusoidal blood pools. It is obvious that in a patient with micropenis, a lesser amount of flow is needed to result in erection and the maximum PSV (one important determinant of flow) would be lower compared to other normal responders with a normal-sized penis, even below the required post injection PSV of more than 30 cm/s. While, in a continuous study, we can follow the normal sequence of changes in CC and easily denote that the patient has no vascular problem. In conclusion, we highlight a considerable role of early and continuous evaluation started one minute after ICI for better description of underlying pathologies of ED especially in patients with venous leak etiology. This study was just a “case series” to obtain a general concept about the benefits of a dynamic study. The patterns described here are just those seen in these 59 cases. In further studies with a larger sample size, it may be possible to declare new patterns or more sharply elucidate the characteristics of the aforementioned groups.
Continuous doppler waveform study of the cavernosal artery in patients with common and uncommon patterns of venous leak
Acknowledgements
References
-
1.
Sadeghi Nejad H, Brison D, Dogra V. Male Erectile Dysfunction. Ultrasound Clin. 2007:57-71. https://doi.org/10.1016/j.cult.2007.01.005.
-
2.
Yavas US, Calisir C, Kaya T, Degirmenci NA. A sign of arteriogenic insufficiency on penile Doppler sonography: retrograde flow in penile cavernosal-spongiosal communications. J Ultrasound Med. 2007;26(12):1643-8. [PubMed ID: 18029915].
-
3.
Reed Dunnick N. Textbook of Uroradiology. Williams and Wilkins; 2001.
-
4.
Mc Gahan JP. Diagnostic Ultrasound. Informa Healthcare. 2008:968-74.
-
5.
Fitzgerald SW, Erickson SJ, Foley WD, Lipchik EO, Lawson TL. Color Doppler sonography in the evaluation of erectile dysfunction: patterns of temporal response to papaverine. AJR Am J Roentgenol. 1991;157(2):331-6. [PubMed ID: 1853817]. https://doi.org/10.2214/ajr.157.2.1853817.
-
6.
Benson CB, Aruny JE, Vickers MA, Jr. Correlation of duplex sonography with arteriography in patients with erectile dysfunction. AJR Am J Roentgenol. 1993;160(1):71-3. [PubMed ID: 8416651]. https://doi.org/10.2214/ajr.160.1.8416651.
-
7.
Benson CB, Vickers MA. Sexual impotence caused by vascular disease: diagnosis with duplex sonography. AJR Am J Roentgenol. 1989;153(6):1149-53. [PubMed ID: 2683673]. https://doi.org/10.2214/ajr.153.6.1149.
-
8.
Meuleman EJ, Bemelmans BL, van Asten WN, Doesburg WH, Skotnicki SH, Debruyne FM. Assessment of penile blood flow by duplex ultrasonography in 44 men with normal erectile potency in different phases of erection. J Urol. 1992;147(1):51-6. [PubMed ID: 1729551].
-
9.
Quam JP, King BF, James EM, Lewis RW, Brakke DM, Ilstrup DM, et al. Duplex and color Doppler sonographic evaluation of vasculogenic impotence. AJR Am J Roentgenol. 1989;153(6):1141-7. [PubMed ID: 2683672]. https://doi.org/10.2214/ajr.153.6.1141.