Abstract
Introduction:
Pure non-gestational ovarian choriocarcinoma is a rare malignant condition with aggressive behavior. The tumor arises from germ cells of ovarian. Few cases have been reported in the literature. We present a case of pure ovarian choriocarcinoma with disseminated tumor in pelvic.Case Presentation:
A 16-year-old girl was referred to Ghaem hospital, Mashhad University of Medical Sciences, Mashhad, Iran in April 2016 with acute abdominal pain, abdomino pelvic mass and vaginal bleeding. In addition, an extremely high level of sub unit of human chorionic gonadotropin β-hCG was detected. Based on the emergency condition, she underwent laparotomy and left salpingo-oophorectomy with suboptimal resection of the tumor. Histopathology revealed a tumor compatible with pure non-gestational ovarian choriocarcinoma. Adjuvant chemotherapy was performed based on 4 courses of bleomycin-etoposide-cisplatin (BEP) regimen. She is now under chemotherapy.Conclusions:
We recommend the use of minimally invasive, fertility-preserving surgeries in patients with non-gestational ovarian choriocarcinomas.Keywords
Pure Ovarian Choriocarcinoma Gestational Choriocarcinoma Human Chorionic Gonadotropin Ovarian Non-Gestational Choriocarcinoma
1. Introduction
Non-gestational ovarian choriocarcinoma is an extremely rare malignant germ cell tumor of the ovary with incidence of 1% of all ovarian germ cell tumor with less than 100 cases being reported worldwide (1). In a detailed summary and analysis, about 30 cases of pure non-gestational choriocarcinoma were reported (2). Non-gestational ovarian choriocarcinoma usually occurs along with other germ cell tumors. Frequently, it is seen in women of reproductive age especially in young women. There are no specific clinical symptoms which can distinguish the other forms of ovarian neoplasia. Indeed, radiological imaging is no differences with other type of adnexal mass. Increasing serum β-hCG level may help (3), but it is difficult to distinguish from other types of gestational ovarian choriocarcinomas. Therefore, at childbearing age, the presence of an adnexal mass with an increased serum β-hCG level and pelvic mass are suggestive of pure ovarian choriocarcinomas. Also, the absence of intrauterine trophoblastic disease may suspect the diagnosis (4). Confirmation of the diagnosis relies on the molecular analysis of DNA. It may identify the original features of two types of gestational or germ cell tumors (5). The combination of surgery along with chemotherapy is the standard treatment. Yang K reported survival 12 mounts of a case of a pure ovarian choriocarcinoma treated by cytoreductive surgery and adjuvant chemotherapy (6). However, in the study by Balat and colleagues, the patient died from brain metastases (7). Due to the rarity of this ovarian choriocarcinoma, we reported a case of Primary Pure non-gestational ovarian choriocarcinoma.
2. Case Presentation
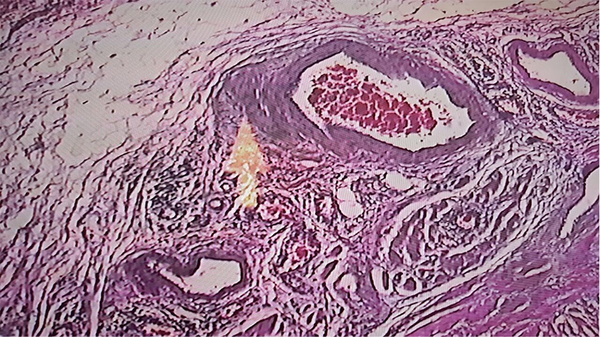
A 16-year-old nulliparous girl with 16 days delay in menstrual period was admitted in gynecology center with vaginal bleeding and abdominal pain and an abdominal mass. In addition to an ultrasonography report of a heterogeneous adnexal mass in the right adnexa of with approximate size of 80*92 mm and cystic-like hypo-echoic foci in the left adnexa with 66*33 mm size, as well as little fluid in the Douglas pouch suggested of ovarian tumor. The profile other tumor markers were reported in normal level, except serum Lactate dehydrogenase (LDH) concentration of 1239 U/L and raised titer beta human chorionic gonadotropin (β-hCG) (144,600 IU/L). The patient was referred to the oncology department of Ghaem hospital, Mashhad University of Medical Sciences, Mashhad, Iran in April 2016 for additional oncological workup while she was in emergency condition. In abdominal examination, a firm mass up to the level of umbilicus was palpable in the abdomen. Therefore, the patient underwent emergency laparotomy with initial diagnosis of ovarian tumor. The peritoneal cavity contained approximately 300 cc of sanguineous ascitic fluid, which was collected and sent for pathological and cytological examination. An extensive hemorrhagic necrotic tumor involving the uterine and both adnexa was observed. Left salpingo-oophorectomy was performed while optimal cytoreductive surgery was impossible. Since ineffective therapeutic strategy, fertility-preserving surgery was carried out and the specimen was sent for frozen section pathology, which was diagnosed to be a germ cell tumor of the ovary of choriocarcinoma type. The right ovary and uterine were preserved. The pathology report of ascetic fluid revealed few reactive mesothelial cells in a dirty hemorrhagic background with no atypical or neoplastic cells. Final pathology confirmed pure non-gestational ovarian choriocarcinoma (Figure 1). Any distant metastasis was not observed in the workup of the patient. Post-operative β-hCG titer was increased to 201,400 IU/L. After taking informed consent from the patient, she received four courses of adjuvant chemotherapy based on bleomycin-etoposide-cisplatin (BEP) regimen. In addition, ovarian suppression with oral contraceptive before initiation of adjuvant chemotherapy was considered. Now, she is under chemotherapy (Figure 2).
Microscopic View of the Tumor Specimen Sent for Pathologic Examination, Indicating an Ovarian Choriocarcinoma
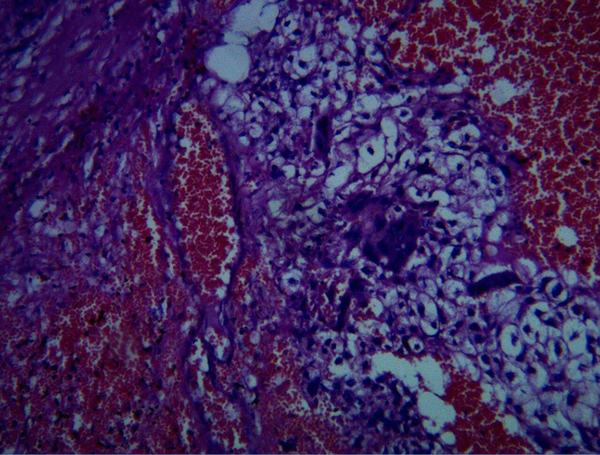
Microscopic View
3. Discussion
The breaking news of current study is the possibility of fertility-preserving methods for the treatment of non-gestational choriocarcinoma even in cases of extensive disease. In fact, this case and many other studies have shown that non-gestational ovarian choriocarcinoma occurs most frequently in reproductive age especially adolescents (8). Due to the nonspecific clinic and para clinic symptoms and signs, misdiagnosis of this rare tumor is very high. Serial β-hCG levels, in addition to accurate clinical examination and ultrasonography can differentiate this diagnosis. In the present study, the patient had an extremely high pre-operative level of β-hCG (144600 IU/L), which is in line with other reports (9, 10). Non-gestational ovarian choriocarcinoma regularly invades the adjacent organs and metastasizes to distant sites, especially brain and lung. Several previous studies have reported metastases of ovarian choriocarcinoma to distant sites (11). For instance, Rao et al. reported a solitary brain metastasis in a patient with non-gestational ovarian choriocarcinoma after two years of treatment (2). In addition, bilateral pulmonary metastases in a patient after the completion of chemotherapy was reported (6, 12). Although in the present study, the patient has no distant metastasis. This tumor most commonly occurs in young patients and unlike epithelial carcinoma the majority of cases are identified at early stage (13). However, our 16-year-old patient presented with an advanced stage. Because of nonspecific symptom of non-gestational ovarian choriocarcinoma, it may easily be mistaken for other ovarian tumors or even an ectopic pregnancy similar to our patient (3). Furthermore, the absence of intrauterine pregnancy and the relatively high level of β-hCG is the possibility of non-gestational ovarian choriocarcinoma. However, detection of this tumor is still an arduous challenge for the clinicians. The identification of the genetic origin of pure ovarian choriocarcinoma and the immunohistochemical study can confirm the different diagnosis between non-gestational and gestational choriocarcinoma of the ovary. Due to unavailability and expensiveness of this technique, it is used in limited centers (14). Based on this, we could not utilize molecular genetic analysis on the tumor from our patient. Treatment modality consists of surgery and adjuvant chemotherapy, also no definitive therapy has been established for pure ovarian choriocarcinomas. However, this strategy might be a conservative surgery. In the present study, since optimal cytoreductive surgery was impossible, ineffective therapeutic strategy with fertility-preserving surgery was performed. Many studies are in line with our study. In recent years, there is a growing trend toward performing fertility-preserving surgery (15). Unlike gestational choriocarcinoma of the ovary, this type of tumor is generally relatively less sensitive to chemotherapy. BEP chemotherapy (Bleomycin, Cisplatin, Etoposide) is the current regimen for germ cell tumors of the ovary. Therefore, our patient was treated with this regimen. This chemotherapy regimen is the most used regimen among the studies and in most cases, the patient had no complication of therapy or sign of recurrence, except for the study of Balat and colleagues, in which the patient died eventually (16). In contrast to gestational choriocarcinoma, poor prognosis is one of the features of this disease. Furthermore, prompt diagnostic measures and early initiation of therapy is important.
In conclusion, non-gestational ovarian choriocarcinoma is a rare malignant germ cell tumor of the ovary. Because the prognosis is worse than that of gestational type, early diagnosis and treatment are important factors for enhancing patient’s prognosis.
Acknowledgements
References
-
1.
Heo EJ, Choi CH, Park JM, Lee JW, Bae DS, Kim BG. Primary ovarian choriocarcinoma mimicking ectopic pregnancy. Obstet Gynecol Sci. 2014;57(4):330-3. [PubMed ID: 25105109]. https://doi.org/10.5468/ogs.2014.57.4.330.
-
2.
Rao KV, Konar S, Gangadharan J, Vikas V, Sampath S. A pure non-gestational ovarian choriocarcinoma with delayed solitary brain metastases: Case report and review of the literature. J Neurosci Rural Pract. 2015;6(4):578-81. [PubMed ID: 26752905]. https://doi.org/10.4103/0976-3147.169869.
-
3.
Koo HL, Choi J, Kim KR, Kim JH. Pure non-gestational choriocarcinoma of the ovary diagnosed by DNA polymorphism analysis. Pathol Int. 2006;56(10):613-6. [PubMed ID: 16984618]. https://doi.org/10.1111/j.1440-1827.2006.02016.x.
-
4.
Wang Q, Guo C, Zou L, Wang Y, Song X, Ma Y, et al. Clinicopathological analysis of non-gestational ovarian choriocarcinoma: Report of two cases and review of the literature. Oncol Lett. 2016;11(4):2599-604. [PubMed ID: 27073524]. https://doi.org/10.3892/ol.2016.4257.
-
5.
Mood NI, Samadi N, Rahimi-Moghaddam P, Sarmadi S, Eftekhar Z, Yarandi F. Pure ovarian choriocarcinoma: report of two cases. J Res Med Sci. 2009;14(5):327-30. [PubMed ID: 21772904].
-
6.
Xin L, Beier A, Tiede S, Pfiffer T, Kohler C, Favero G. Laparoscopic Fertility-preserving Treatment of a Pure Nongestational Choriocarcinoma of the Ovary: Case Report and Review of Current Literature. J Minim Invasive Gynecol. 2015;22(6):1095-9. [PubMed ID: 25939824]. https://doi.org/10.1016/j.jmig.2015.04.025.
-
7.
Choi YJ, Chun KY, Kim YW, Ro DY. Pure nongestational choriocarcinoma of the ovary: a case report. World J Surg Oncol. 2013;11:7. [PubMed ID: 23320455]. https://doi.org/10.1186/1477-7819-11-7.
-
8.
Jiao LZ, Xiang Y, Feng FZ, Wan XR, Zhao J, Cui QC, et al. Clinical analysis of 21 cases of nongestational ovarian choriocarcinoma. Int J Gynecol Cancer. 2010;20(2):299-302. [PubMed ID: 20134273]. https://doi.org/10.1111/IGC.0b013e3181cc2526.
-
9.
Gon S, Majumdar B, Barui G, Karmakar R, Bhattacharya A. Pure primary non-gestational ovarian choriocarcinoma: a diagnostic dilemma. Indian J Pathol Microbiol. 2010;53(1):178-80. [PubMed ID: 20090265]. https://doi.org/10.4103/0377-4929.59226.
-
10.
Ozturk E, Ugur MG, Cebesoy FB, Aydin A, Sever T, Balat O. Good prognosis for primary ovarian pure nongestational choriocarcinoma using the EMA/CO regime. Eur J Gynaecol Oncol. 2010;31(1):123-5. [PubMed ID: 20349799].
-
11.
Bohiltea R, Radoi V, Tufan C, Horhoianu IA, Bohiltea C. Abdominal pregnancy - Case presentation. J Med Life. 2015;8(1):49-54. [PubMed ID: 25914739].
-
12.
Haruma T, Ogawa C, Nishida T, Kusumoto T, Nakamura K, Seki N, et al. Pure Choriocarcinoma of the Ovary in Silver-Russell Syndrome. Acta Med Okayama. 2015;69(3):183-8. [PubMed ID: 26101195]. https://doi.org/10.18926/AMO/53526.
-
13.
Nogales FF, Dulcey I, Preda O. Germ cell tumors of the ovary: an update. Arch Pathol Lab Med. 2014;138(3):351-62. [PubMed ID: 24576031]. https://doi.org/10.5858/arpa.2012-0547-RA.
-
14.
Gerson RF, Lee EY, Gorman E. Primary extrauterine ovarian choriocarcinoma mistaken for ectopic pregnancy: sonographic imaging findings. AJR Am J Roentgenol. 2007;189(5):W280-3. [PubMed ID: 17954626]. https://doi.org/10.2214/AJR.05.0814.
-
15.
Chen YX, Xu J, Lv WG, Xie X. Primary ovarian choriocarcinoma mimicking ectopic pregnancy managed with laparoscopy -- case report. Eur J Gynaecol Oncol. 2008;29(2):174-6. [PubMed ID: 18459557].
-
16.
Balat O, Kutlar I, Ozkur A, Bakir K, Aksoy F, Ugur MG. Primary pure ovarian choriocarcinoma mimicking ectopic pregnancy: a report of fulminant progression. Tumori. 2004;90(1):136-8. [PubMed ID: 15143987].