Abstract
Background:
Breast cancer is a public health challenge in most populations and a cause of morbidity and mortality worldwide. Lack of reliable and valid tools for assessing predicting factors, which influence on breast self-examination behavior of Iranian women, is obvious. This study aimed at designing and evaluating the psychometric properties of this instrument.Objectives:
The purpose of this study was psychometric validation health action process approach (HAPA) scale for prediction of breast self-examination behavior among Iranian women over 40 years.Methods:
In this cross sectional study, the participants were registered women 40 years and older in urban health centers in Tehran, Iran. The 200 subjects were selected by multi-stage cluster sampling. Content and face validity have been verified by a panel of experts and participants. Using exploratory and structural equation modeling confirmatory factor analyses was conducted construct validity.Results:
Using explanatory factor analysis, 8 factors of health action process approach model were identified with appropriate variance explained (67.18%). The HAPA had an acceptable fit to the observations (χ2 = 2.21, df = 3, χ2/df = 1.35, P < 0.001, RMSEA = 0.049 (CI = 0.044, 0.056; AGFI = 0.90; P = 0.452; PGFI = 0.13).Conclusions:
The results of the present study suggested an initial for validity and reliability of the HAPA-based breast self-examination among Iranian women.Keywords
Health Action Process Approach (HAPA) Psychometric Breast Self-Examination
1. Background
Breast cancer is a public health challenge in most population and it is a globally cause of morbidity and mortality; based on reports of World Health Organization (WHO) in 2012, this disease is with approximately 14 million new cases (1).
Previous research conducted in Iran shows that breast cancer has a significant impact on life and that Iranian women are younger than developing countries for at least 10 years (2).
The process of cancer diagnosis and treatment can be advanced by early detection and it significantly reduces mortality and morbidity and improves women’s quality of life (3).
The previous studies have shown low partnership in breast self-examination (BSE) practice in Iranian women and over the past 2 decades, the incidence of breast cancer among them shows an alarmingly rapid increase (4). They also encounter a significantly higher risk of mortality due to the advanced stage of cancer at diagnosis (5) and breast cancer is considered as a health priority and statistic data strongly confirm this issue and the most effective and affordable method of improving survival and decreasing mortality is screening (6).
The culturally-based beliefs are compounding problems, so that they discourage from undertaking cancer screening measures (7).
Health Action Process Approach (HAPA) is a comprehensive model that has been developed in 2008 for assessing the health promotion behaviours, especially breast cancer (8). HAPA included constructs like risk perception, outcome expectancies, action self-efficacy, maintenance self-efficacy, action planning, coping planning, action control, behavioral intention, and recovery self-efficacy that could predict the health behaviors, especially breast self-examination. There is no valid Persian instrument to assess the influencing factors. This paper reports the process of developing the questionnaire, using the (HAPA) scale as its conceptual framework, and the results of initial reliability and validity testing.
2. Objectives
The aim of this study was the psychometric validation HAPA scale for prediction of breast self-examination behavior among Iranian women over 40 years.
3. Methods
This cross sectional study was a part of Ph.D. dissertation and Ethics Committee of Tarbiat Modares University approved with the clinical trial code IRCT2017061134472N1. All participants signed informed written consent.
First, a questionnaire included 40 items was developed based on HAPA and the existing literature on breast self-examination (9), and it was produced following a review of the literature and discussion with healthcare professionals. Then, a forward version was produced. After a accurate review and cultural adaptation few changes, this questionnaire was created. The temporary version of the research tool was provided and reviews revealed, there were no difficulties in answering the translating categories.
Then, a provisional version of questionnaire was pilot test. The mean time to complete questionnaire was 30.2 (SD = 6.3) min and 80% of the participants expressed that they had no problems completing the questionnaire and 97% demonstrated that there were no confusing and uncomfortable questions.
The findings of the pilot study were shown, a few more changes were made and all questions were carefully transformed, and the final version with 37 items was prepared and used in this research.
The validity of the instrument concepts was determined by a sample of 400 women over 40 years, who were to return to health centers and were eligible due to inclusion/exclusion criteria. The inclusion criterion was the lack of history of breast cancer in participants and their family. The exclusion criteria for women were unlettered Persian language and insufficient physical and mental health to fill in the questionnaire.
Both quantitative and qualitative approaches were performed to verify face validity of the questionnaire. In qualitative approach, 70 women over 40 years assessed each item for “ambiguity”, “relevancy”, and “difficulty”. In this process, 6 items need to be improved. For quantitative approach, from women who requested to appraise the questionnaire. Also, in order to measure the impact score for each item, they declared their view about importance of each item on a 5-point Likert scale.
The impact score of 1.5 or above was considered satisfactory, through which all items were retained in the questionnaire for subsequent. For qualitative method and in order to content analysis, an expert panel including 22 members consisting 8 health education and promotion expert, 7 reproductive health and gynecologist, 2 oncologist, and 5 psychologist checked all items and listed their recommendations into the questionnaire. The authors had considered any option in the expert panel to want their suggestion for a concept and also important issue that should be considered in the questionnaire, but it was missed and not present in primary version.
Moreover, they also evaluated the questionnaire for ‘grammar’, ‘wording’, ‘item allocation’, and for computing the quantitative content validity, the content validity index (CVI) and content validity ratio (CVR) were used. The necessity of an item was determined through CVR and the items with score < 0.418 were deleted according to Lawsh’s (10).
The simplicity, relevancy, and clarity of the items were assessed through CVI and the score of 0.78 or above was considered satisfactory for each statement (11).
In order to estimate the internal consistency, Cronbach’s alpha was used. Stability was assessed, using Pearson correlations and intraclass correlation coefficients (ICC) were calculated.
The participants completed their set of questionnaires. Sufficient reliability of the questionnaire, a HAPA scale of BSE behavior, was the main criterion for the validation method. For a research tool, an acceptable reliability is commonly set at 0.70 (12).
This study examined the psychometric properties of the breast self-examination in 2 independent samples of women over 40 years referred to health centers of Shahid Beheshti University of Medical Sciences (SBMU).
3.1. Sample 1
Sample 1 consisted of 210 women over 40 years referred to Shahid Beheshti University of Medical Sciences (SBUMS). First, a multistage cluster sampling was applied. From 10 health networks at Shahid Beheshti University of Medical Sciences (SBUMS), North, East, and Shemiranat networks were selected. Then, from each of these networks, 10 health centers were randomly selected and, then, 20 women were randomly assigned to each health center. The ideal sample size was estimated based on the need for exploratory factor analysis. A useful rule of thumb was regarding the relationship between sample size and model exploratory. Based on rule of thumb in exploratory factor analysis 10 or 20 participants are required and the minimum sample size required for an exploratory statistical analysis is 200 (13). On the other hand, according to Munro’s view about the sample size, 5 individuals per item is enough (14). Therefore, for 37-item questionnaire, a sample size of 37 × 5 = 185 were estimated and in order to increase the accuracy and dropping sample size, 210 people were calculated.
3.2. Sample 2
Sample 2 consisted of 200 women over 40 years referred to health centers of Shahid Beheshti University of Medical Sciences (SBUMS). North, East, and Shemiranat networks were selected. Then, from each of these networks, 5 health centers were randomly selected and, then, 40 women were randomly assigned to each health center. The ideal sample size was estimated based on the need for confirmatory factor analysis; then, based on this rule, 200 participants was estimated for the sample size.
In oder to assess the psychometric properties of the questionnaire were performed several statistical analyses.
The construct validity of the questionnaire was examined, using exploratory factor analyses (EFA) (15, 16). A principal component analysis with varimax rotation was performed to extract the underlying factors factor. Factor loadings equal or greater than 0.4 were considered appropriate (17). Eigenvalues above 1 and scree plots were used for determining the number of statements. The Kaiser-Meyer-Olkin measure (KMO = 0.70) and Bartlett’s test of sphericity (P < 0.001) were used to assess the appropriateness of the sample size for the factor analysis (18). Structural equation modeling was conducted, using AMOS 21. To determine the fit of the model, we applied the following 4 criteria that including chi-square, adjusted goodness-of-fit index (AGFI), root mean square error of approximation (RMSEA), and parsimony goodness goodness-of-fit index (PGFI). The chi-square test was used to compare the covariance matrix indication and it is a hypothetical model of the observed variables in the population (19).
Therefore, if chi-square test was non-significant, the fit will be acceptable.
An AGFI value range is between 0 and 1 and AGFI above 0.90 indicates a complete and well fitting model (20, 21) and a model with small values of PGFI indicates fit the data well (22) .All the statistical analyses and EFA were used by SPSS v.20 and CFA was conducted, using Amos v.21.
In order to estimate the internal consistency, Cronbach’s alpha coefficient was used, once for each concept and for the whole questionnaire.
The Cronbach’s alpha coefficient of 0.7 or higher was considered as acceptable criteria (15).
In addition, stability was assessed, using Pearson correlations and intraclass correlation coefficients (ICC) were calculated with a sub-sample of women over 40 years (n = 70), who completed the questionnaires twice with an interval of 2 weeks. The acceptable value for ICC was considered 0.4 or above (23).
The participants completed their set of questionnaires. Sufficient reliability of the questionnaire, a HAPA scale of BSE behavior, was the main criterion for the validation method. For a research tool, an acceptable reliability is commonly set at 0.70 (12).
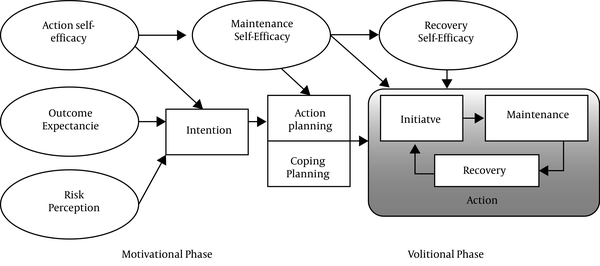
The HAPA consisted of 8 scales, each to be rated on a 5-point scale varying according to the content of the scales. The outcome was the performance of BSE for all scales (Figure 1) (8).
Health action process approach generic diagram (8)
3.3. Ethics
The Ethics Committee of Tarbiat Modares University approved the study (IR.TMU.REC.1395.328); all participants signed informed written consent.
3.4. Risk Perception
The participant perceived risk of morbidity of breast cancer was obtained. To evaluate the perceived risk, participants were asked to estimate the chance of facing breast cancer, for example,” my chances of getting breast cancer in the next 5 years are great” (24). Participants rated their odds in the future, using a separate 5-point scale from strongly disagree (score 1) to strongly agree (score 5).
3.5. Outcome Expectancies
Outcome expectancies structure were considered by 4 items based on Ajzen’s recommendations (25) and participant feedback. They were requested. “Having a breast self-examination every month will give me a feeling of control over my health” (26). Participants rated their odds in the future, using a separate 5-point scale from strongly disagree (score 1) to strongly agree (score 5).
3.6. Action Self-Efficacy
To measure the perceived action self-efficacy in BES, we applied 5 different items based on the Schwarzer’s recommendations (27). The following stems were applied “How sure are you that can overcome the following obstacles?” Responses were generated on 5-point scales, ranging from strongly disagree (score 1) to strongly agree (score 5) (9, 28).
3.7. Behavioral Intention
For evaluation of intention to seek BSE, 5 items were used form Ajzen (25) and Smith et al. (26): with replication from strongly disagree (score 1) to strongly agree (score 5).
3.8. Action Planning
Action planning was appraised with 3 items recommendation by Luszczynska and Schwarzer (9). Women rated strongly disagree (1) to strongly agree (5) whether they had constructed detailed plans regarding their BSE in terms of (A) “when”, (B) “where”, and (C) ”how” to act for the start a BSE.
3.9. Coping Planning
Coping planning was determined with 4 items, with same scale action planning. women graded if they had constructed plans in detail about (A) “what to do if their plans go under a trouble for doing BSE”, (B) “how to face the defeats in their plans for breast self-examination”, (C) ”how to stick with youre goals, even under in difficult situations, and (D) “what to do if their plans on how we answered your opponents in BSE. These items were made based on Schwarzer’s recommendations (9, 28).
3.10. Maintenance Self-Efficacy
The measured confidence of individuals in their ability to do BSE even if they were stopped by some barriers. We identified 6 barriers from previous research within BSE (29, 30) and also the feedback from this study, during the pilot phase of the HAPA inventory. answers were made in 5-point scales, ranging from strongly disagree (score 1) to strongly agree (score 5).
3.11. Action Control
Action control was assigned by a newly developed instrument consisting of 6 items, so that 2 items each addressed the different action control facets of comparative self-monitoring (items A and B), notice of standards (items C and D), and self-regulatory attempt (items E and F): (1) “I consistently monitored myself whether I did BSE frequently enough”, (2) “I consistently monitored when, where, and how long I did BSE”, (3) “I have always been understanding my prescribed training program”, (4) “I often had my BSE on mind”, (5) “I did BSE regularly”, and (6) “I took care as much as much as I intended to BSE” (31).
3.12. Recovery Self-Efficacy
The belief’s women were evaluated to see if they can recover themselves after being on a failure in BSE behavior (9). The females were asked to answer the following questions regarding their confidence, the ability to comeback to BSE after quitting this behavior, using a 5-point such as scale-up.
3.13. Breast Self-Examination Behavior
According to standard accepted criteria, BSE behavior was assessed as self-reported BSE within the past 1 month and intended screening with the next month (32). Two items assessed past behavior. “Have you accomplished BSE in the last month?” (Yes/No), and “How often have you accomplished BSE in the last 6 months?” Along a 7-point scale (never_once a month), and participants were also answered concurrent two questions: ”If you did not administrate BSE, please list the reasons why you have not done so”.
Items were summed with higher average score s, indicating more frequency of past BSE behavior (32).
4. Results
All of the females (100%) who participated in this study returned the HAPA on BSE behavior questionnaire. Their overall median was 45.6 (IQR: 42 - 48) years, with the majority (88%) of the women being married (Table 1).
| Variables | Total, N = 200 | Attended BSE Screening | Did Not Attended BSE Screening | P Valueb |
|---|---|---|---|---|
| Age | 45.6 (42 - 48)c | 44.45 ± 4.8 | 45.97 ± 5.6 | 0.2 |
| Educational level | 0.03 | |||
| Elementary | 75 (37.5) | 15 (7.5) | 60 (30) | |
| More than elementary | 125 (62.5) | 43 (21.5) | 82 (41) | |
| BMI | ||||
| Mean ± SD | 27 ± 4.9 | 25.87 ± 4.7 | 27.36 ± 4.9 | 0.02 |
| Normal weight (< 25) | 73 (36.5) | 15 (7.5) | 58 (29) | 0.05 |
| Overweight (25.5 - 29.9) | 84 (42) | 17 (8.5) | 67 (33.5) | |
| Obese (> 30) | 43 (21.5) | 4 (2) | 39 (19.5) | |
| Marital status | 0.01 | |||
| Single | 6 (3) | 1 (0.5) | 5 (2.5) | |
| Married | 176 (88) | 31 (15.5) | 145 (72.5) | |
| Separated | 5 (2.5) | 1 (0.5) | 4 (2) | |
| Divorced | 13 (6.5) | 4 (2) | 9 (4.5) |
4.1. Face Validity
In general, no major changes were needed to be made on the HAPA on BSE behavior scales except for some rewriter and visual improvements of the inventory so as to reduce complexity and to assure for consistency.
4.2. Content Validity
The final version of the questioner was average content validity (s-CVI/Ave) 0.80 indicating the adequate content validity.
4.3. Construct Validity
We assess the result of the Kolmogorov-Smirnov test and before performing factor analysis, was evaluated ceiling and floor effects. It was shown that there was no evidence against the normality (P > 0.05) (33). The Kaiser-Meyer-Olkin measure (KMO = 0.70) and Bartlett’s test of sphericity (P < 0.001). Eight factors were extracted; the results are shown in Table 2.
| Construct Name | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 |
|---|---|---|---|---|---|---|---|---|
| Risk perception | ||||||||
| Q1 | 0.636 | |||||||
| Q2 | 0.700 | |||||||
| Q3 | 0.722 | |||||||
| Q4 | 0.540 | |||||||
| Q5 | 0.594 | |||||||
| Q6 | 0.569 | |||||||
| Outcome expectancies | ||||||||
| Q7 | 0.544 | |||||||
| Q8 | 0.516 | |||||||
| Q9 | 0.641 | |||||||
| Q10 | 0.599 | |||||||
| Action self-efficacy | ||||||||
| Q11 | 0.504 | |||||||
| Q12 | 0.665 | |||||||
| Q13 | 0.539 | |||||||
| Q14 | 0.469 | |||||||
| Q15 | 0.426 | |||||||
| Action planning | ||||||||
| Q16 | 0.725 | |||||||
| Q17 | 0.583 | |||||||
| Q18 | 0.730 | |||||||
| Coping planning | ||||||||
| Q19 | 0.484 | |||||||
| Q20 | 0.596 | |||||||
| Q21 | 0.680 | |||||||
| Q22 | 0.661 | |||||||
| Maintenance self-efficacy | ||||||||
| Q23 | 0.611 | |||||||
| Q24 | 0.603 | |||||||
| Q25 | 0.544 | |||||||
| Q26 | 0.551 | |||||||
| Q27 | 0.667 | |||||||
| Q28 | 0.559 | |||||||
| Recovery self-efficacy | ||||||||
| Q29 | 0.499 | |||||||
| Q30 | 0.544 | |||||||
| Q31 | 0.603 | |||||||
| Action control | ||||||||
| Q32 | 0.486 | |||||||
| Q33 | 0.502 | |||||||
| Q34 | 0.523 | |||||||
| Q35 | 0.465 | |||||||
| Q36 | 0.447 | |||||||
| Q37 | 0.507 |
CFA showed that all the scales were nice indicators of their theoretical constructs. The fit to the BSE measurement model was sufficient (χ2 = 2.21, df = 3, χ2/df = 1.35, P < 0.001, RMSEA = 0.049) (CI = 0.044, 0.056; AGFI = 0.90; P = 0.452; PGFI = 0.13). The path diagram of CFA is presentated in Figure 2.
HAPA path model with standardized regression coefficients and beta coefficients of HAPA constructs (P < 0.05)
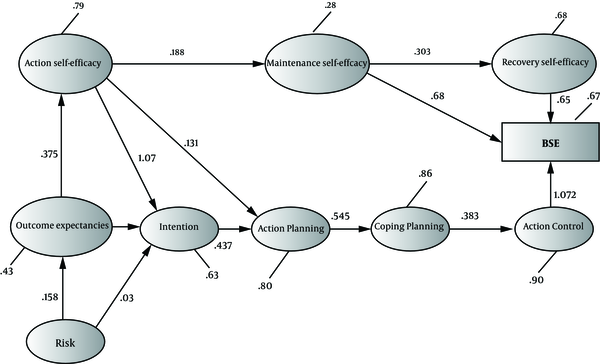
Using explanatory factor analysis, 8 factors of HAPA framework were identified with appropriate variance explained (67.18%) BSE behavior.
4.4. Reliability
4.4.1. Criterion Validity
The result of investigating the relationship between the motivational HAPA stage constructs and intention of BSE illustrates bivariate correlations of the motivational HAPA factors with intention (Table 3).
Summary of Health Action Process Approaches (HAPA) Psychometric Properties and Correlations with BSE Behavior
| Construct | Number of Items | Mean ± SD | Cronbach’s Alpha | ICCa | Correlation (r) with Breast Self-Examination Intention | Correlation (r) Breast Self-Examination Behavior |
|---|---|---|---|---|---|---|
| Risk perception | 6 | 14.61 ± 5.4 | 0.86 | 0.90 | 0.21b | 0.24c |
| Outcome expectancies | 4 | 16.8 ± 3.1 | 0.79 | 0.80 | 0.16b | 0.10c |
| Action self-efficacy | 5 | 9.2 ± 2.7 | 0.60 | 0.83 | 0.25b | 0.36c |
| Action planning | 3 | 5.56 ± 3.03 | 0.60 | 0.82 | 0.21b | 0.35c |
| Coping planning | 4 | 5.8 ± 2.4 | 0.83 | 0.80 | 0.46b | 0.39c |
| Maintenance self-efficacy | 6 | 12.01 ± 3.5 | 0.69 | 0.80 | 0.08 | 0.12c |
| Recovery self-efficacy | 3 | 5.04 ± 1.3 | 0.64 | 0.85 | 0.25b | 0.08 |
| Action control | 6 | 10.6 ± 2.12 | 0.70 | 0.78 | 0.44b | 0.32c |
The BSE intention was significantly associated with risk perception (r = 0.21, P < 0.05). Also, BSE intention was significantly associated with outcome expectancies (r = 0.16, P < 0.05), and BSE intention was significantly associated with action self-efficacy (r = 0.25, P < 0.05). The recovery self-efficacy significantly was related to BSE intention (r = 0.25, P < 0.05) and two planning factors, action planning (r = 0.21, P < 0.05) and coping planning (r = 0.46, P < 0.05) had an effect on BSE intention.
The BSE behavior was significantly associated with risk perception (r = 0.24, P < 0.05), and action control (r = 0.32, P < 0.05) was significantly associated with BSE behavior.
The bivariate correlations were significant between volitional HAPA stage constructs and BSE.
There was little and moderate-sized significant association between the HAPA volitional constructs breast self-examination behavior (r = 0.16 - 0.46).
5. Discussion
This study contains the initial phase of a larger research program that aimed at examining the effectiveness of the HAPA framework for the prediction of BSE behavior among 40-year old women. Overall, there is preliminary evidence that the HAPA scales are valid and reliable measures.
For the motivational stage constructs, there were large, significant correlation between measures of action self-efficacy and coping planning with intentions to adopt a BSE. These findings were consistent with the HAPA concepts (8), which have suggested high correlations between behavioral intentions and action self-efficacy. Research on a larger sample size of women is necessary to better understand these findings. In Luszczynska and Schwarzer’s study (9), action self-efficacy appeared as the best predictor of intention and planning. In the current study, planning affected breast self-examination ‘s behavior. In turn, emerged self-efficacy was the best and foremost predictor of BSE. But, in this study, coping planning had the greatest impact on breast self-examination behavior. Coping planning can help the participant to defeat barriers and to cope with difficulties by anticipating personal risk situation.
In this study, the risk perception founded correlations between behavioral intentions; BSE intention was predicted by risk perception. This finding was consistent with a study conducted by Rimal and Juon (34) and inconsistent with the other study (35).
Interestingly, there was a correlation between action self-efficacy and outcome expectancies with BSE intentions. In this study, it was shown that the correlation between action self-efficacy and behavioral intentions was upper than outcome expectancies and behavioral intentions. In another study, it was depicted that the correlation between action self-efficacy and behavioral intentions was lower than outcome expectancies and behavioral intentions (36).
According to the principles of HAPA scale, both outcome expectancies and action self-efficacies have a great impact on the prediction of behavioral intentions, while risk perception appears to be more of a “distal antecedent” informing behavioral intentions (8). Also, according to Bandura’s social cognitive theory, self-efficacy has the stronger effect than outcome expectancies on behavioral intentions (37). In another study, it was suggested that when efficacy beliefs are strong, the effect of risk perception is positive, but it is negative when efficacy beliefs are weak (34).
In the current study, action control was significantly associated with BSE intention. Action control was through self-regulatory process. This is largely dependent on individual self-efficacy and quality of performance planning to understanding competence and experience. This was confirmed in Daniel et al. study (38).
This study had some limitations. First, the generalization is limited because the convenient sample was drawn mainly from Iranian women. Furthermore, this study used self-report measures of BSE behavior that could have been over-reported or under-reported. Further studies are provided with the proper confirmation of their reported data in their design.
5.1. Conclusions
Overall, the findings of this study were supported by both reliability and validity of the HAPA for assessing predictors of breast self-examination intentions and behavior among women with 40 years and older.
Acknowledgements
References
-
1.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-86. [PubMed ID: 25220842]. https://doi.org/10.1002/ijc.29210.
-
2.
Didarloo A, Nabilou B, Khalkhali HR. Psychosocial predictors of breast self-examination behavior among female students: An application of the health belief model using logistic regression. BMC Public Health. 2017;17(1):861. [PubMed ID: 29100508]. [PubMed Central ID: PMC5670517]. https://doi.org/10.1186/s12889-017-4880-9.
-
3.
Azaiza F, Cohen M. Health beliefs and rates of breast cancer screening among Arab women. J Womens Health (Larchmt). 2006;15(5):520-30. [PubMed ID: 16796479]. https://doi.org/10.1089/jwh.2006.15.520.
-
4.
Jazayeri SB, Saadat S, Ramezani R, Kaviani A. Incidence of primary breast cancer in Iran: Ten-year national cancer registry data report. Cancer Epidemiol. 2015;39(4):519-27. [PubMed ID: 26070507]. https://doi.org/10.1016/j.canep.2015.04.016.
-
5.
Yousefi Kashi AS, Yazdanfar S, Akbari ME, Rakhsha A. Triple negative breast cancer in Iranian women: Clinical profile and survival study. Int J Cancer Manage. 2017;10(8). https://doi.org/10.5812/ijcm.10471.
-
6.
Bao Y, Kwok C, Lee CF. Psychometric properties of the modified breast cancer screening beliefs questionnaire among mainland Chinese women. Eur J Oncol Nurs. 2017;28:35-40. [PubMed ID: 28478853]. https://doi.org/10.1016/j.ejon.2017.02.006.
-
7.
Azami-Aghdash S, Ghojazadeh M, Sheyklo SG, Daemi A, Kolahdouzan K, Mohseni M, et al. Breast cancer screening barriers from the womans perspective: A meta-synthesis. Asian Pac J Cancer Prev. 2015;16(8):3463-71. [PubMed ID: 25921163].
-
8.
Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychol. 2008;57(1):1-29. https://doi.org/10.1111/j.1464-0597.2007.00325.x.
-
9.
Luszczynska A, Schwarzer R. Planning and self-efficacy in the adoption and maintenance of breast self-examination: A longitudinal study on self-regulatory cognitions. Psychol Health. 2003;18(1):93-108. https://doi.org/10.1080/0887044021000019358.
-
10.
Wilson FR, Pan W, Schumsky DA. Recalculation of the critical values for lawshe’s content validity ratio. Meas Eval Couns Dev. 2017;45(3):197-210. https://doi.org/10.1177/0748175612440286.
-
11.
Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459-67. [PubMed ID: 17654487]. https://doi.org/10.1002/nur.20199.
-
12.
Sklenarova H, Haun MW, Krumpelmann A, Friederich HC, Huber J, Thomas M, et al. Psychometric evaluation of the German version of the supportive care needs survey for partners and caregivers (SCNS-P&C-G) of cancer patients. Eur J Cancer Care (Engl). 2015;24(6):884-97. [PubMed ID: 25939448]. https://doi.org/10.1111/ecc.12325.
-
13.
Kline RB. Principles and practice of structural equation modeling. Guilford publications; 2015.
-
14.
Munro BH. Statistical methods for health care research. 5th ed. lippincott williams & wilkins; 2005.
-
15.
Hajizadeh E, Asghari M. Statistical methods and analyses in health and biosciences a research methodological approach. Tehran: Jahade Daneshgahi Publications; 2011. 395 p.
-
16.
Lawshe CH. A quantitative approach to content validity. Personnel Psychol. 1975;28(4):563-75. https://doi.org/10.1111/j.1744-6570.1975.tb01393.x.
-
17.
Sarallah S, Sadat TS, Jamshidi AR, Joan W. A multidisciplinary work-related low back pain predictor questionnaire: Psychometric evaluation of Iranian patient-care workers. Asian Spine J. 2016;10(3):501-8. [PubMed ID: 27340530]. [PubMed Central ID: PMC4917769]. https://doi.org/10.4184/asj.2016.10.3.501.
-
18.
Harrington D. Confirmatory factor analysis. Oxford University Press; 2009.
-
19.
Brown T. Methodology in the social sciences. Confirmatory factor analysis for applied research. 2nd ed. New York, US: Guilford Press; 2015.
-
20.
Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. 1st ed. Taylor & Francis; 2001.
-
21.
Hooper D, Coughlan J, Mullen M. Structural equation modelling: Guidelines for determining model fit. Electron J Business Res Meth. 2008;6(1):53-60. https://doi.org/10.21427/d7cf7r.
-
22.
Liu A. Structural equation modeling and latent variable approaches. Emerging trends in the social and behavioral sciences: An interdisciplinary, searchable, and linkable resource. John Wiley & Sons; 2015. p. 1-15. https://doi.org/10.1002/9781118900772.etrds0325.
-
23.
Haghighat S, Montazeri A, Zayeri F, Ebrahimi M, Weiss J. Psychometric evaluation of the Persian version of the lymphedema life impact scale (LLIS, version 1) in breast cancer patients. Health Qual Life Outcomes. 2018;16(1):132. [PubMed ID: 29954381]. [PubMed Central ID: PMC6025716]. https://doi.org/10.1186/s12955-018-0958-z.
-
24.
Lee JB. Breast cancer fear, mammography fear, and mammography adherence of African American women in Bridgeport, Connecticut. New York University; 2011.
-
25.
Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991;50(2):179-211. https://doi.org/10.1016/0749-5978(91)90020-t.
-
26.
Smith SM, Ford JS, Rakowski W, Moskowitz CS, Diller L, Hudson MM, et al. Inconsistent mammography perceptions and practices among women at risk of breast cancer following a pediatric malignancy: A report from the childhood cancer survivor study. Cancer Causes Control. 2010;21(10):1585-95. [PubMed ID: 20506037]. [PubMed Central ID: PMC2941535]. https://doi.org/10.1007/s10552-010-9587-5.
-
27.
Schwarzer R, Renner B. Social-cognitive predictors of health behavior: Action self-efficacy and coping self-efficacy. Health Psychol. 2000;19(5):487-95. [PubMed ID: 11007157].
-
28.
Schwarzer R, Sniehotta FF, Lippke S, Luszczynska A, Scholz U, Schüz B, et al. On the assessment and analysis of variables in the health action process approach: Conducting an investigation. Berlin. Freie Universität Berlin; 2003.
-
29.
Amoran OE, Toyobo OO. Predictors of breast self-examination as cancer prevention practice among women of reproductive age-group in a rural town in Nigeria. Niger Med J. 2015;56(3):185-9. [PubMed ID: 26229226]. [PubMed Central ID: PMC4518334]. https://doi.org/10.4103/0300-1652.160362.
-
30.
Tabari F, Abbaszadeh R, Torabi S, Amini F. Barriers of breast self-examination: A review study from Iranian researchers. Bali Med J. 2017;6(3):562. https://doi.org/10.15562/bmj.v6i3.639.
-
31.
Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: The health action process approach (HAPA). Rehabil Psychol. 2011;56(3):161-70. [PubMed ID: 21767036]. https://doi.org/10.1037/a0024509.
-
32.
Prestwich A, Conner M, Lawton R, Bailey W, Litman J, Molyneaux V. Individual and collaborative implementation intentions and the promotion of breast self-examination. Psychol Health. 2005;20(6):743-60. https://doi.org/10.1080/14768320500183335.
-
33.
Kim SH, Whitt W. The power of alternative Kolmogorov-Smirnov tests based on transformations of the data. ACM Transact Model Comput Simulat. 2015;25(4):1-22. https://doi.org/10.1145/2699716.
-
34.
Rimal RN, Juon HS. Use of the risk perception attitude framework for promoting breast cancer prevention. J Appl Soc Psychol. 2010;40(2):287-310. https://doi.org/10.1111/j.1559-1816.2009.00574.x.
-
35.
Garcia K, Mann T. From 'I wish' to 'I will': Social-cognitive predictors of behavioral intentions. J Health Psychol. 2003;8(3):347-60. [PubMed ID: 14670213]. https://doi.org/10.1177/13591053030083005.
-
36.
Rohani H, Eslami AA, Ghaderi A, Bidkhori M, Raei M. Development and psychometric evaluation of a health action process approach inventory for healthful diet among type 2 diabetes patients. Int J Prev Med. 2016;7:69. [PubMed ID: 27195101]. [PubMed Central ID: PMC4863400]. https://doi.org/10.4103/2008-7802.181333.
-
37.
Bandura A. Social cognitive theory: An agentic perspective. Annu Rev Psychol. 2001;52:1-26. [PubMed ID: 11148297]. https://doi.org/10.1146/annurev.psych.52.1.1.
-
38.
Daniel AO, Enoma IO, Omobude-Idiado SN. Application of protection motivation theory (PMT) and health action process approach (HAPA) in promoting women's adaptive engagement towards breast self examination. Academic Res Int. 2014;5(1):291.

