Abstract
Background:
Opioid poisoning is common and fatal childhood poisoning in Iran with nonspecific, hidden, vague, and misleading clinical manifestations in some cases.Objectives:
The aim of this study was to investigate and emphasize pruritus, as a neglected and helpful symptom in this important poisoning.Methods:
In this cross-sectional study, one hundred pediatrics patients (< 14 years) with opioid poisoning who were referred to Loghman Hakim Hospital, Tehran-Iran, from April 2018 to April 2019 were enrolled the study. Demographic data including age, sex, type of poisoning, clinical manifestations including pruritus, its onset, location, duration, and therapy, also laboratory findings including complete blood count (CBC) and Eosinophilia recorded in patient-specific information forms. The collected data were analyzed using SPSS 21 software.Results:
The patients’ mean age was 43.4 ± 31.4 months. Fifty-seven (57%) of them were male. Fifty-two (52%) of them reported Pruritus that in 84% observed in face. In 31% of children, itching resulted in skin scratches. The most common clinical manifestations were CNS depression (93%), respiratory suppression (68%), vomiting (52%), pruritus (52%), and meiosis (51%). There was no significant relationship between pruritus and gender, age, laboratory findings, family history of addiction, and allergy. Pruritus had a significant difference with Respiratory suppression (apnea, bradypnea, cyanosis), meiosis, vomiting, and redness of the skin (P-value: 0.05, 0.003, 0.009, and 0.002, respectively). Pruritus was controlled by naloxone in all of our patients.Conclusions:
According to the results of the present study, pruritus is a common and helpful clinical manifestation in children with opioid poisoning that helps the physician for correct diagnosis, especially in hidden clinical scenarios.Keywords
1. Background
Opioid poisonings are common and fatal poisoning in children in Iran (1, 2). Classic opioid toxidrome of respiratory depression, central nervous system (CNS) depression, and meiosis can produce severe morbidity and even death (3). Opioids can also cause multiple nonspecific findings in various organ systems (4). These signs and symptoms are similar to many other CNS depressant agents like Barbiturates, Clonidine, Baclofen, sedative-hypnotics, ethanol coma, and some other toxins (5). Pruritus is a symptom of opioid poisoning that did not occur in other CNS depressants poisoning; thus it is helpful in clinical diagnosis.
Sometimes the true history of opium poisoning is hidden by parents because of some legal, familial, social, and some other factors, and wide range of clinical manifestations and differential diagnoses make it a difficult scenario. Even in rare situations in which the assay results are available rapidly, the fact that several various classes of opioids and non-opioids can produce similar opioid effects limits the use of laboratory tests (5). Pruritus is poorly investigated in pediatric opium poisoning. The pathogenesis of opioid-induced pruritus is still not fully known, but two different mechanisms have been proposed, including peripheral and central histamine release that may be associated with other histamine release manifestations such as hypotension, flushing, and rhinorrhea (5). Facial areas innervated by the trigeminal nerve are mostly affected, probably due to the high concentration of opioid receptors in the nucleus of the trigeminal nerve (6).
Typically, patients scratch the nose, paranasal area, and upper part of the face, although generalized pruritus has also been reported (7). Xenobiotics that is commonly implicated in neural-mediated itch include tramadol, codeine, cocaine, morphine, butorphanol, and methamphetamine (5). Several treatment modalities have been tried for opioid-induced pruritus (OIP), most indicated a significant reduction in the frequency and severity of itching with naloxone (8).
2. Objectives
Pruritus is a helpful symptom for making a correct diagnosis of this important poisoning, but this valuable sign is frequently neglected by both parents and physicians. The aim of our study is to emphasize and evaluation of pruritus and related factors in opioid poisoning in children.
3. Methods
This cross-sectional descriptive study was conducted on one hundred pediatric (< 14 years) patients presenting with opioid poisoning in Loghman Hakim Hospital (referral poison center) from April 2018 to April 2019 in Tehran-Iran. The inclusion criteria were age under 14 years, and definitive diagnosis of opioid poisoning confirm by history, compatible physical examination, and positive urine rapid test, and the exclusion criteria were patients with indefinite diagnosis, co-ingestion, and negative urine toxicology test.
Sample size: Because we did not find a pervious similar study for sample size calculation, one hundred participants were enrolled according to convenience simple sampling using α = 95%, P = 50%, and D = 10%. Using a self-made questionnaire, demographics characteristics, type and amount of poisoned opioid agent, clinical manifestations, pruritus, and its location, presentation time, duration, and treatment modalities, also related major paraclinical parameters mainly complete blood count (CBC) and Eosinophilia were documented for each patient and statistically analyzed. The data were analyzed by descriptive and analytical statistics (ANOVA and t-test) with SPSS software version 21, chi-square when comparing two percentages, and t-test when comparing two means. The level of significance was set at a p-value of less than 0.05 (≤ 0.05). This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences. Ethics code: IR.SBMU.MSP.REC.1398.439.
4. Results
Out of 100 studied patients, 57% were male and 43%were female with mean age of 43.4+31.4 months, near half of them were between 1 - 3 years (Table 1).
Age Distribution Among Studied Patients
| Age (y) | No (%) |
|---|---|
| < 1 | 16 (16) |
| 1 - 3 | 48 (48) |
| 3 - 5 | 23 (23) |
| > 5 | 13 (13) |
| Total | 100 |
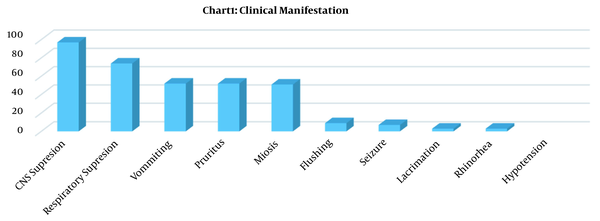
Type of opioid poisoning shows in all all of them were unintentional poisoning, the greatest proportion of poisonings was methadone (n = 65, 65%) especially methadone syrup (90%). Amount of ingested methadone was uncertain in 80% of cases, and in the remainder, the ingested methadone dose was 30.6 ± 11milligrams, although in the majority of them, the reported ingested methadone dose was small amount. Eighteen percent of our cases had a positive history of living with addicted parents (completely their father). The most frequent clinical manifestation in our patients were CNS depression (n = 93, 93%), respiratory suppression (apnea, bradypnea, cyanosis), (n = 68, 68%), vomiting (n = 52, 52%) and pruritus (n = 52, 52%), are illustrated in Figure 1.
Clinical manifestation among studied patients
Pruritus was observed in 52% of our patients, and most of them (84%) happened in face, only 12% had generalized itching. Pruritus leading to scratch & abrasion in 16 (31%) of cases. The pruritus was begun between 15 minutes and 360 minutes after ingestion, mean 90.1 ± 8.9 minutes, most of them (84%) occurred on face, and the mean duration of this sign was 5.5 ± 4.7 hours and lasted from 30 minutes to 24 hours.
As shown in Table 2, analytic analysis of cases with pruritus in relation to sex, age, and ingested opium showed that these differences were not statistically significant.
The type of opioid agents and pruritus in our patients was not statistically significant (P-value = 0.62). Patients with positive allergy history (n = 9, 19%) were prone to opioid-induced pruritus. (P-value = 0.04). As shown in Table 3, pruritus had a significant difference with respiratory suppression (apnea, bradypnea, cyanosis), meiosis, vomiting, and redness of the skin (P-value = 0.05, 0.003, 0.009, and 0.002, respectively).
| Sign or Symptom | Patient with Pruritus; 52 (52) | Patient Without Pruritus; 48 (48) | P-Value b |
|---|---|---|---|
| CNS depression | 48 (92) | 45 (94) | 0.41 |
| Respiratory suppression | 50 (96) | 24 (50) | 0.05 |
| Vomiting | 33 (64) | 19 (40) | 0.009 |
| Meiosis | 34 (65) | 17 (35) | 0.003 |
| Flushing/skin redness | 9 (17) | 0 | 0.002 |
| Seizure | 5 (10) | 2 (4) | 0.26 |
| Lacrimation | 3 (6) | 0 | 0.08 |
| Rhinorrhea | 3 (6) | 0 | 0.08 |
| Hypotension | 1 (2) | 0 | 0.32 |
In most of our patients (58%), CBC, including WBC and differentiation, was normal, and eosinophilia was not reported in any of them. All cases of opium-induced pruritus in our study were controlled with naloxone without any additional therapy except naloxone.
5. Discussion
This study is unique in the sense that we did not find any article emphasizing this symptom in opium poisoning. According to the results of the present study, pruritus is a common and helpful sign of acute opioid poisoning. In our study, more than half of them had pruritus, but we did not find any related research about this important sign in children. Opium and methadone poisoning is a common and fatal childhood poisoning in Iran (2, 9, 10). Alizadeh et al. about the epidemiological pattern and recent changes of acute pediatric poisoning in Mashhad during 2011- 2013 showed that this poisoning is common in children but changed from traditional opium to methadone poisoning (11).
Reich et al. reported that pruritus is a common adverse effect of chronic opioid treatment, and they found that the risk is increased when opioids are administered epidurally or intraspinally. In the present study, we found that pruritus was common and observed in 52% of children with acute oral opioid poisoning (7). Also, Benson et al. declared that opioid-induced pruritus (OIP) is one of the most common adverse effects of oral and neuraxial opioids (12). Huang et al.’s study on relative rates of pruritus associated with common drugs in adults showed that among all drugs investigated, heparin (1.11%), trimethoprim-sulfamethoxazole (1.06%), and calcium channel blockers (0.92%) were associated with the highest rates of pruritus, their study was conducted on adult and in chronic drug users (13). Szarvas et al. reported the induction of OPI after intrathecal and epidural opioids varies between 30 and 100% (14).
In the present study, we found that more than half of methadone-poisoned patients had pruritus, but in one study conducted by Sharif and Nouri about clinical signs and symptoms and laboratory findings of methadone poisoning, in children, they did not report any cases of methadone-induced pruritus. This difference may occur when pruritus is not told or considered by parents or physicians (15). Other researches about the clinical manifestation of opium poisoning in children and adults, such as Zamani et al. that conducted a study on 228 infants and 82 toddlers opium poisoned cases admitted to Loghman Hakim Hospital, 2001 - 2009, showed that the most usual sign of opium poisoning was meiosis (90%) followed by a decreased level of consciousness (88.4%), bradypnea (28.4%), and seizure (10.3%) without any cases with pruritus (16). Also, Ghaemi et al.’s study results showed similar results (17). In our study frequently observed clinical manifestations were CNS depression (93%), respiratory suppression (74%), vomiting (52%), pruritus (52%), meiosis (51%). Sixteen patients experienced skin abrasion. We did not find any reported article about pruritus in acute opioid poisoning in children. Pruritus in all of our patients controlled by naloxone, Miller et al. reported the effectiveness of the use of pure opioid antagonists for the prevention and treatment of opioid-induced pruritus as a common adverse effect of therapeutic use of oral opioid medications in adults (8). Khansari et al. declared that pruritus is a common adverse effect of opioids, although not harmful but can be troublesome with no proven pathogenesis and µ-opioid receptor antagonists or the serotonin 5-HT3 receptor antagonists of ondansetron have been effective for therapy (18).
Eosinophilia was not reported in our patients, which the reason may be that CBC was not performed manually in our patients. Haghpanah et al. reported that eosinophil count showed no difference in opium- or heroin-addicted adults with control group (19). The treatment of opioid-induced pruritus remains a challenge. Szarvas et al. reported that various drugs, including antihistamines, 5-HT3 receptor antagonists, opiate-antagonists, propofol, nonsteroidal anti-inflammatory drugs, and droperidol, have been studied for OIP (14). A meta-analysis of thirteen studies, including 1,138 patients, showed that naloxone acted as an effective treatment and prophylaxis of opioid-induced pruritus, nausea, and vomiting. Similar to our study, pruritus was easily controlled by naloxone in all of the cases (20). The limitation of our study is that quantitative blood test for opioids are not available in our hospital, and further study by prospectively designed multicenter studies and larger sample size is recommended.
5.1. Conclusion
According to the results of the present study, pruritus is a common, neglected, and helpful symptom of acute opioid poisoning in children that is easily controlled by opioid antagonists such as naloxone. Based on the results of this study, most cases of children with acute opioid toxicity experienced pruritus mainly in face and nose. This sign helps physicians in the diagnosis of this serious poisoning in hidden or obscure clinical situations.
Acknowledgements
References
-
1.
Soltaninejad K, Hassanian-Moghaddam H, Shadnia S. Methadone related poisoning on the rise in Tehran, Iran. Asia Pac J Med Toxicol. 2014;3(3):104-9.
-
2.
Shadnia S, Rahimi M, Hassanian-Moghaddam H, Soltaninejad K, Noroozi A. Methadone toxicity: Comparing tablet and syrup formulations during a decade in an academic poison center of Iran. Clin Toxicol (Phila). 2013;51(8):777-82. [PubMed ID: 23972442]. https://doi.org/10.3109/15563650.2013.830732.
-
3.
Kliegman RM, Behrman RE, Jenson HB, Stanton B. Nelson textbook of pediatrics e-book. Amsterdam: Elsevier Health Sciences; 2007.
-
4.
Yin S, Burns MM, Wiley JF. Opioid intoxication in children and adolescents. Netherlands: UpToDate; 2021. Available from: https://www.uptodate.com/contents/opioid-intoxication-in-children-and-adolescents.
-
5.
Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR. Goldfrank's Toxicologic Emergencies. 10th ed. New York, USA: McGraw Hill Professional; 2014.
-
6.
Reich A, Szepietowski JC. Opioid-induced pruritus: An update. Clin Exp Dermatol. 2010;35(1):2-6. [PubMed ID: 19663845]. https://doi.org/10.1111/j.1365-2230.2009.03463.x.
-
7.
Reich A, Stander S, Szepietowski JC. Drug-induced pruritus: A review. Acta Derm Venereol. 2009;89(3):236-44. [PubMed ID: 19479118]. https://doi.org/10.2340/00015555-0650.
-
8.
Miller JL, Hagemann TM. Use of pure opioid antagonists for management of opioid-induced pruritus. Am J Health Syst Pharm. 2011;68(15):1419-25. [PubMed ID: 21785031]. https://doi.org/10.2146/ajhp100475.
-
9.
Pirzadeh Z, Jamshidi M, Mollamohammadi M. Acute Poisoning in Children Referred to Qazvin Children Hospital (2009 to 2012). J Compr Ped. 2016;7(4). e40099. https://doi.org/10.17795/compreped-40099.
-
10.
Mansori K, Soori H, Farnaghi F, Khodakarim S, Mansouri Hanis S, Khodadost M. A case-control study on risk factors for unintentional childhood poisoning in Tehran. Med J Islam Repub Iran. 2016;30:355. [PubMed ID: 27453885]. [PubMed Central ID: PMC4934449].
-
11.
Alizadeh A, Zheani Asoudeh M, Abdi F, Moshiri M, Balali Mood M, Etemad L. Epidemiological Pattern of Acute Pediatric Poisoning in Mashhad, Iran During 2011 - 2013. Int J High Risk Behav Addict. 2016;6(2). e33707. https://doi.org/10.5812/ijhrba.33707.
-
12.
Benson JL, Campbell HE, Phillips CN. Opioid-induced pruritus. Consult Pharm. 2015;30(4):221-7. [PubMed ID: 25893700]. https://doi.org/10.4140/TCP.n.2015.221.
-
13.
Huang AH, Kaffenberger BH, Reich A, Szepietowski JC, Stander S, Kwatra SG. Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center. Medicines (Basel). 2019;6(3). [PubMed ID: 31382689]. [PubMed Central ID: PMC6789849]. https://doi.org/10.3390/medicines6030084.
-
14.
Szarvas S, Harmon D, Murphy D. Neuraxial opioid-induced pruritus: A review. J Clin Anesth. 2003;15(3):234-9. [PubMed ID: 12770663]. https://doi.org/10.1016/s0952-8180(02)00501-9.
-
15.
Sharif MR, Nouri S. Clinical Signs and Symptoms and Laboratory Findings of Methadone Poisoning in Children. Iran J Pediatr. 2015;25(1). https://doi.org/10.5812/ijp.176.
-
16.
Zamani N, Sanaei-Zadeh H, Mostafazadeh B. Hallmarks of opium poisoning in infants and toddlers. Trop Doct. 2010;40(4):220-2. [PubMed ID: 20807730]. https://doi.org/10.1258/td.2010.100134.
-
17.
Ghaemi N, Alikhani S, Bagheri S, Sezavar M. A Cross Sectional Study of Opioid Poisoning in Children at a Tertiary Center. Asia Pac J Med Toxicol. 2016;5(4):115-8.
-
18.
Khansari M, Sohrabi M, Zamani F. The Useage of Opioids and their Adverse Effects in Gastrointestinal Practice: A Review. Middle East J Dig Dis. 2013;5(1):5-16. [PubMed ID: 24829664]. [PubMed Central ID: PMC3990131].
-
19.
Haghpanah T, Afarinesh M, Divsalar K. A review on hematological factors in opioid-dependent people (opium and heroin) after the withdrawal period. Addict Health. 2010;2(1-2):9-16. [PubMed ID: 24494095]. [PubMed Central ID: PMC3905505].
-
20.
He F, Jiang Y, Li L. The effect of naloxone treatment on opioid-induced side effects: A meta-analysis of randomized and controlled trails. Medicine (Baltimore). 2016;95(37). e4729. [PubMed ID: 27631221]. [PubMed Central ID: PMC5402564]. https://doi.org/10.1097/MD.0000000000004729.