Abstract
Background:
Human T-Cell Leukemia Virus (HTLV) infection is endemic in Neyshabour, and even higher than other cities.Objectives:
The aim of this investigation was to determine the prevalence of HTLV antibodies among young females attending a large medical diagnostic laboratory in Neyshabour, during 2011 to 2015.Methods:
The researchers established this study by data, which were collected from the surveillance system. Based on HTLV-1 and HTLV-2 ELISA kit instruction, 5724 females were evaluated. Variables were age, year, and season. Data were analyzed by the SPSS software.Results:
According to the Enzyme Linked Immunosorbent Assay (ELISA) results, 117 (2.04 %) young females indicated evidence of antibodies to HTLV-1 and HTL -2. Most infected young females were aged 38 to 39 years (4.16%) and according to annual prevalence, the highest rates were found in 2012. Also, most infected young females had referred in October (3.16%).Conclusions:
The data obtained suggests that Neyshabour is a high endemic city of HTLV infected young females. Making them aware seems to be vital in avoiding transfer of HTLV infection, especially to the next generation. However, further investigations like population-based studies are required to confirm these resultsKeywords
Human T-lymphotropic Virus Seroepidemiology Women’s Groups Enzyme-linked immunosorbent assay Iran
1. Background
Human T-Cell Leukemia Virus (HTLV), a major source of adult T-cell leukemia and related diseases, is endemic to northeastern Iran and Neyshabur, and was detected to be higher than other cities, according to previous reports (1, 2). Japan, Africa, Caribbean Islands, and South America are the most prevalent for Human T-cell lymphotropic virus (3, 4).
The HTLV infection is considered as a public health challenge in endemic areas so that HTLV-1 and HTLV-2 infection rate has been reported as 0.26% and 0% in Mashhad (the first populous city in Razavi Khorasan), respectively (5, 6). According to a recent study, Neyshabour, as the second populous city in Razavi Khorasan, has a rate of 6.55% (2). The prevalence rates of HTLV-1 infection in successive three years of Sabzevar (the third populous city of Razavi Khorasan) study was 0.19%, 0.14%, and 0.09%, respectively (7).
The prevalence of HTLV-1 infection in pregnant females, in countries such as Ghana, Burkina-Faso, Gabon, Jamaica, Haiti, Japan (Okinawa), Italy, Greece, French Guyana, Brazil (Mato Grosso), Brazil (Sao Luis), Peru (Andes, Coast, Jungle, Lima), Argentina (Cordoba-Central) were found to be 2.1% (8), 1% (9), 2.1% (10), 3.8% (11), 4.2% (12), 3.9% (13), 0.02% (14), 0% (15), 4.2% (12), 0.2% (16), 0.2% (17), 1.3% (18) and 0.1% (19) respectively .
Modes of HTLV transmission are the same as human immunodeficiency Virus (HIV) (18) and for a long time, infected carriers remain asymptomatic so that these people serve as a potential source for the transmission of the virus (20). There are some studies, which have indicated that the north-eastern Iran has high endemicity of HTLV infection (1, 2, 21-23), yet they are not conducted on young females as a sensitive and important part of the society in this region.
2. Objectives
The aim of this investigation was to determine the prevalence of HTLV infection among young females attending a large medical diagnostic laboratory in Neyshabour, Northeast of Iran, during years 2011 to 2015.
3. Methods
3.1. Study Population
An epidemiologic survey was carried out in Neyshabur between 2011 and 2015 among healthy young females. A total of 5724 healthy individuals from Neyshabur, North-Eastern Iran, were included in this study. The prevalence of HTLV-1 and HTLV-2 infections was established by collected data from the surveillance system during 2011 to 2015. The sample of the study was a biased sample and also some other laboratories were involved in this study. The participant’s personal data were confidential. Investigated variables were age, year, and season.
3.2. Serological Assays and Confirmation Tests
The HTLV-1 and HTLV-2 kit (Dia. Pro Diagnostic Bioprobes, Italy) that had a sensitivity of 95% and specificity of 98% and Stat Fax 3200 (USA) ELISA reader were used based on available instructions (24). Based on laboratory policy, all borderline results were evaluated again after one month.
3.3. Statistical Analysis
Data were analyzed by SPSS version 20 (IBM SPSS Statistics for Windows, Version 20, Armonk, NY, IBM Corp.). The chi-square test with significance level of 0.05 was used.
3.4. Ethical Approval
Approval for this study was obtained from the Research and Technology deputy of ACECR, Mashhad Branch.
4. Results and Discussion
Overall, 5724 participants were evaluated in the present study. Participants' mean age was 28.22 ± 6 years. Overall, 117 (2.04 %) had evidence of antibodies to HTLV-1 and HTLV-2, according to the ELISA results. Most participants were aged 25 to 26 years old (Figure 1).
More detailed age-based distribution of women who referred for HTLV-1 & HTLV -2 screening during 2010 To 2015
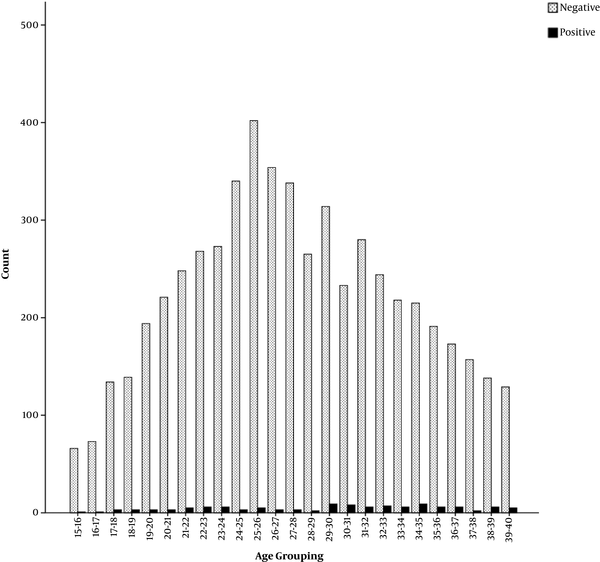
The prevalence was significantly more common in older than younger females (ranged from 15 to 40 years old) (Tables 1 and 2). Most infected young females were aged 38 to 39 years (4.16%). The total prevalence of HTLV-1 and HTLV- 2 in each year is indicated in Table 3; based on the results, the highest prevalence was found in 2012 and gradually decreased with passing time (P < 0.0001). Seasonal prevalence investigation demonstrated that 3.16% of infected young females had referred in October.
Age-Based Distribution of Women and Overall HTLV-1 and HTLV-2 Cases of Screening During 2010 To 2015
| Variable | No. | Positive Cases (%) | Odd Ratio (OR) | CL 95% | P Value |
|---|---|---|---|---|---|
| Age, y | |||||
| 15 - 28 | 3095 | 45 (1.45) | 1.908 | 1.31 - 2.78 | 0.001 |
| 29 - 40 | 2629 | 72 (2.74) |
More Detailed Age-Based Distribution of Women Who Referred for HTLV-1 and HTLV -2 Screening During 2010 to 2015a
| Age Grouping | Negative | Positive (%) | Total |
|---|---|---|---|
| 15 - 16 | 66 | 1 (1.49) | 67 |
| 16 - 17 | 73 | 1 (1.35) | 74 |
| 17 - 18 | 134 | 3 (2.19) | 137 |
| 18 - 19 | 139 | 3 (2.11) | 142 |
| 19 - 20 | 194 | 3 (1.52) | 197 |
| 20 - 21 | 221 | 3 (1.33) | 224 |
| 21 - 22 | 248 | 5 (1.97) | 253 |
| 22 - 23 | 268 | 6 (2.19) | 274 |
| 23 - 24 | 273 | 6 (2.15) | 279 |
| 24 - 25 | 340 | 3 (0.87) | 343 |
| 25 - 26 | 402 | 5 (1.22) | 407 |
| 26 - 27 | 354 | 3 (0.84) | 357 |
| 27 - 28 | 338 | 3 (0.89) | 341 |
| 28 - 29 | 265 | 2 (0.75) | 267 |
| 29 - 30 | 314 | 9 (2.78) | 323 |
| 30 - 31 | 233 | 8 (3.31) | 241 |
| 31 - 32 | 280 | 6 (2.09) | 286 |
| 32 - 33 | 244 | 7 (2.79) | 251 |
| 33 - 34 | 218 | 6 (2.68) | 224 |
| 34 - 35 | 215 | 9 (4.01) | 224 |
| 35 - 36 | 191 | 6 (3.04) | 197 |
| 36 - 37 | 173 | 6 (3.35) | 179 |
| 37 - 38 | 157 | 2 (1.26) | 159 |
| 38 - 39 | 138 | 6 (4.16) | 144 |
| 39 - 40 | 129 | 5 (3.73) | 134 |
| Year | Number | HTLV-1 & HTLV-2 -Positivity Percentage |
|---|---|---|
| 2015 | Positive: 10 Total: 1185 | 0.84 |
| 2014 | Positive: 18 Total: 1259 | 1.43 |
| 2013 | Positive: 24 Total: 1157 | 2.07 |
| 2012 | Positive: 39 Total: 1124 | 3.46 |
| 2011 | Positive: 26 Total: 999 | 2.60 |
The present study showed that participants were mostly aged 25 to 26 years old (Figure 1) because of the fact that pregnancy and marriage events usually take place in this range of age and women need to perform screening tests, including HTLV.
Some previous studies in Neyshabour have demonstrated that the prevalence of HTLV1, HTLV-1 and HTLV -2 among females (ranged 1 to 100) were 5.17 % and 4.94%, respectively (1, 2). In comparison with the current study, about 4.16% of infected young females were aged 38 to 39 years. After the year of 2012, the total HTLV-1 and HTLV- 2 prevalence begun to significantly decrease (Table 3). It is speculated that greater awareness of the public is more likely the reason of this promising decrease. The current results were also in agreement with the endemicity of HTLV in the general population of Neyshabour (2). It must be considered that age is the most important factor, which had the highest impact on infection. The researchers did not take account of older females of more than 40 years in the present study. Thus, the prevalence of HTLV-1 and HTLV- 2 was lower than the two mentioned studies. In 2013, another study indicated that the prevalence rate among young females, aged 13 to 19 and 20 to 35 were 0.26 and 2.13, respectively (22). Considering Tables 1 and 2, it is clear that the prevalence was more significantly common in older than younger females (ranged from 15 to 40 years old), however, it was not significant in detailed age grouping (P = 0.239).
The HTLV-1 antibodies seroprevalence among the pregnant females, who attended the antenatal clinic at the University of Nigeria Teaching Hospital was 0.5% (25). A study performed in Rio de Janeiro showed the prevalence among pregnant females was equivalent to 0.66% (26). A Japanese study reported that the prevalence rate of HTLV-1 among pregnant females was 0.1% (27). During two successive years (From March 2011 to April 2013), Hatami et al. (28) showed the prevalence of HTLV-1 was 0.5% among blood donor females (aged 17 to 59) in Mashhad. About 1864489 blood donations were evaluated for HTLV-1 by karimi et al., and there were 0.098% infected donators (29).
In the present study, 2.04% of healthy young females were positive for HTLV-1 and HTLV- 2 by the ELISA test during the five years. This highlights that Neyshabur is an endemic region for HTLV infection. Young females are most susceptible for vertical transmission of HTLV infection to next generations. The prevalence of the infection among pregnant females in Neyshabur is a little higher than other parts of Razavi Khorasan province (1). According to pregnancy, which usually takes place in young females and the high positivity rate (2.04 %) demonstrated in the present study; the researchers suggested that health authorities should pay more attention to this health matter. Also, screening must be carried out in all young females whether they have been married or not.
This study, for the first time indicated the seasonal prevalence of HTLV-1 and HTLV -2 from 2011 to 2015 (Table 4). The month of October had the highest referrals by infected young females (3.16%). However, this research did not find any significant relationship between month and HTLV infection.
| Month | Negative | Positive (%) | Total |
|---|---|---|---|
| April | 487 | 11 (2.2) | 498 |
| August | 440 | 10 (2.22) | 450 |
| December | 525 | 7 (1.31) | 532 |
| February | 464 | 10 (2.1) | 474 |
| January | 435 | 8 (1.8) | 443 |
| July | 510 | 13 (2.48) | 523 |
| June | 413 | 10 (2.34) | 423 |
| March | 442 | 11 (2.42) | 453 |
| May | 613 | 7 (1.13) | 620 |
| November | 503 | 13 (2.51) | 516 |
| October | 367 | 12 (3.16) | 379 |
| September | 408 | 5 (1.21) | 413 |
4.1. Conclusion
The data obtained suggests that Neyshabour, as a second populous city in Razavi Khorasan, is a high endemic city of HTLV infected young females. Making females aware in educational facilities seems to be vital to avoid the transfer of HTLV infection, especially to the next generations. Further investigations, such as population-based studies are required to confirm these results. Development of strategies seems to be necessary for decreasing this infection among young females in the main endemic city of Iran.
Acknowledgements
References
-
1.
Hedayati-Moghaddam MR, Fathimoghadam F, Eftekharzadeh Mashhadi I, Soghandi L, Bidkhori HR. Epidemiology of HTLV-1 in Neyshabour, Northeast of Iran. Iran Red Crescent Med J. 2011;13(6):424-7. [PubMed ID: 22737506]. [PubMed Central ID: PMC3371930].
-
2.
Salehi M, Shokouhi Mostafavi SK, Ghasemian A, Gholami M, Kazemi-Vardanjani A, Rahimi MK. Seroepidemiology of HTLV-1 and HTLV-2 Infection in Neyshabur City, North-Eastern Iran, during 2010-2014. Iran Biomed J. 2017;21(1):57-60. [PubMed ID: 26899860]. [PubMed Central ID: PMC5141255].
-
3.
Verdonck K, Gonzalez E, Van Dooren S, Vandamme AM, Vanham G, Gotuzzo E. Human T-lymphotropic virus 1: recent knowledge about an ancient infection. Lancet Infect Dis. 2007;7(4):266-81. https://doi.org/10.1016/s1473-3099(07)70081-6.
-
4.
Proietti FA, Carneiro-Proietti AB, Catalan-Soares BC, Murphy EL. Global epidemiology of HTLV-I infection and associated diseases. Oncogene. 2005;24(39):6058-68. [PubMed ID: 16155612]. https://doi.org/10.1038/sj.onc.1208968.
-
5.
Safabakhsh H, Jalalian M, Karimi G. Seroepidemiology of human T-cell lymphotropic virus type-1 (HTLV1) in Mashhad. Glob J Health Sci. 2014;6(5):99-104. [PubMed ID: 25168999]. [PubMed Central ID: PMC4825399]. https://doi.org/10.5539/gjhs.v6n5p99.
-
6.
Rafatpanah H, Fathimoghadam F, Shahabi M, Eftekharzadeh I, Hedayati-Moghaddam M, Valizadeh N, et al. No Evidence of HTLV-II Infection Among Immonoblot Indeterminate Samples Using Nested PCR in Mashhad, Northeast of Iran. Iran J Basic Med Sci. 2013;16(3):229-34. [PubMed ID: 24470868]. [PubMed Central ID: PMC3881255].
-
7.
Maghsudlu M, Safabakhsh H, Jamili P. Seroepidemiology of human T-cell lymphotropic virus type-I in blood donors of Northeastern Iran, Sabzevar. Asian J Transfus Sci. 2015;9(2):203-6. [PubMed ID: 26420946]. [PubMed Central ID: PMC4562147]. https://doi.org/10.4103/0973-6247.154255.
-
8.
Armah HB, Narter-Olaga EG, Adjei AA, Asomaning K, Gyasi RK, Tettey Y. Seroprevalence of human T-cell lymphotropic virus type I among pregnant women in Accra, Ghana. J Med Microbiol. 2006;55(Pt 6):765-70. [PubMed ID: 16687597]. https://doi.org/10.1099/jmm.0.46426-0.
-
9.
Collenberg E, Ouedraogo T, Ganame J, Fickenscher H, Kynast-Wolf G, Becher H, et al. Seroprevalence of six different viruses among pregnant women and blood donors in rural and urban Burkina Faso: A comparative analysis. J Med Virol. 2006;78(5):683-92. [PubMed ID: 16555290]. https://doi.org/10.1002/jmv.20593.
-
10.
Etenna SL, Caron M, Besson G, Makuwa M, Gessain A, Mahe A, et al. New insights into prevalence, genetic diversity, and proviral load of human T-cell leukemia virus types 1 and 2 in pregnant women in Gabon in equatorial central Africa. J Clin Microbiol. 2008;46(11):3607-14. [PubMed ID: 18845819]. [PubMed Central ID: PMC2576568]. https://doi.org/10.1128/JCM.01249-08.
-
11.
Maloney EM, Yamano Y, Vanveldhuisen PC, Sawada T, Kim N, Cranston B, et al. Natural history of viral markers in children infected with human T lymphotropic virus type I in Jamaica. J Infect Dis. 2006;194(5):552-60. [PubMed ID: 16897651]. https://doi.org/10.1086/506365.
-
12.
Tortevoye P, Tuppin P, Carles G, Peneau C, Gessain A. Comparative trends of seroprevalence and seroincidence rates of human T cell lymphotropic virus type I and human immunodeficiency virus 1 in pregnant women of various ethnic groups sharing the same environment in French Guiana. Am J Trop Med Hyg. 2005;73(3):560-5. [PubMed ID: 16172481].
-
13.
Maehama T. Human T cell leukemia virus-1 in pregnancy. Int J Gynaecol Obstet. 2004;87(3):247-8. [PubMed ID: 15548399]. https://doi.org/10.1016/j.ijgo.2004.07.024.
-
14.
Taylor GP, Bodeus M, Courtois F, Pauli G, Del Mistro A, Machuca A, et al. The seroepidemiology of human T-lymphotropic viruses: types I and II in Europe: a prospective study of pregnant women. J Acquir Immune Defic Syndr. 2005;38(1):104-9. [PubMed ID: 15608533].
-
15.
Tseliou PM, Spanakis N, Spiliotakara A, Markogiannakis A, Legakis NJ, Tsakris A. Prevalence of infection by HTLV-I/II among pregnant women and high-risk groups in the Peloponnese peninsula, Greece. Int J STD AIDS. 2006;17(8):543-6. [PubMed ID: 16925902]. https://doi.org/10.1258/095646206778145541.
-
16.
Ydy RR, Ferreira D, Souto FJ, Fontes CJ. [Prevalence of human T-cell lymphotropic virus (HTLV-1/2) infection among puerperae in Cuiaba, Mato Grosso, 2006]. Rev Soc Bras Med Trop. 2009;42(1):28-32. [PubMed ID: 19287932].
-
17.
Gessain A, Cassar O. Epidemiological Aspects and World Distribution of HTLV-1 Infection. Front Microbiol. 2012;3:388. [PubMed ID: 23162541]. [PubMed Central ID: PMC3498738]. https://doi.org/10.3389/fmicb.2012.00388.
-
18.
Alarcon JO, Friedman HB, Montano SM, Zunt JR, Holmes KK, Quinnan GV Jr. High endemicity of human T-cell lymphotropic virus type 1 among pregnant women in peru. J Acquir Immune Defic Syndr. 2006;42(5):604-9. [PubMed ID: 16773029]. [PubMed Central ID: PMC2683844]. https://doi.org/10.1097/01.qai.0000221680.52563.d5.
-
19.
Trenchi A, Gastaldello R, Balangero M, Irizar M, Cudola A, Gallego S. Retrospective study of the prevalence of human T-cell lymphotropic virus-type 1/2, HIV, and HBV in pregnant women in Argentina. J Med Virol. 2007;79(12):1974-8. [PubMed ID: 17935192]. https://doi.org/10.1002/jmv.21027.
-
20.
Tanajura D, Castro N, Oliveira P, Neto A, Muniz A, Carvalho NB, et al. Neurological Manifestations in Human T-Cell Lymphotropic Virus Type 1 (HTLV-1)–Infected Individuals Without HTLV-1–Associated Myelopathy/Tropical Spastic Paraparesis: A Longitudinal Cohort Study. Clin Infect Dis. 2015;61(1):49-56. https://doi.org/10.1093/cid/civ229.
-
21.
Rezvan H, Abolghassemi H, Kafiabad SA. Transfusion-transmitted infections among multitransfused patients in Iran: a review. Transfus Med. 2007;17(6):425-33. [PubMed ID: 18067646]. https://doi.org/10.1111/j.1365-3148.2007.00794.x.
-
22.
Salehi M, Mobini M. The seroepidemiological of Human T-lymphotropic virus on children, teenage and juveniles in Nyshabor city. Iran J Med Microbiol. 2015;9(3):31-5.
-
23.
Salehi M, Afrisham M. The seroepidemiological survey of HTLV1, 2 infections in Nyshabor city (Northeast of Iran). Lab Diagnos. 2014;6(23):35-8.
-
24.
Mortezaie Z, Bouzari M, Roghanian R. Evaluating the frequency of HTLV-Ι/II infection among blood donors, major thalassemic patients and individuals infected with hepatitis B and C viruses in Isfahan, Iran. Iran J Blood Cancer. 2012;4(2):75-80.
-
25.
Okoye AE, Ibegbulam OG, Onoh RC, Ezeonu PO, Ugwu NI, Lawani LO, et al. Seroprevalence and correlates of human T-cell lymphoma/leukemia virus type 1 antibodies among pregnant women at the University of Nigeria Teaching Hospital, Enugu, Nigeria. Int J Womens Health. 2014;6:849-55. [PubMed ID: 25258559]. [PubMed Central ID: PMC4174018]. https://doi.org/10.2147/IJWH.S64199.
-
26.
Monteiro DL, Taquette SR, Sodre Barmpas DB, Rodrigues NC, Teixeira SA, Villela LH, et al. Prevalence of HTLV-1/2 in pregnant women living in the metropolitan area of Rio de Janeiro. PLoS Negl Trop Dis. 2014;8(9). e3146. [PubMed ID: 25188386]. [PubMed Central ID: PMC4154655]. https://doi.org/10.1371/journal.pntd.0003146.
-
27.
Yamada T, Togashi T, Tsutsumi H, Imamura M, Okubo H, Okabe M, et al. Prevalence of human T‐lymphotropic virus type 1 carriers among pregnant women in Hokkaido, Japan. Microbiol Immun. 2014;58(8):427-31.
-
28.
Hatami H, Karimi GH, Safabakhsh HR. Seroepidemiologic prevalence of HTLV in voluntary blood donors in Mashhad. Sci J Iran Blood Transfusion Organization. 2012;9(2).
-
29.
Karimi G, Zadsar M, Pourfathollah AA. Seroprevalence and geographical distribution of human T-lymphotropic virus type 1 among volunteer blood donors in endemic areas of Iran. Virol J. 2017;14(1):14. [PubMed ID: 28137274]. [PubMed Central ID: PMC5282699]. https://doi.org/10.1186/s12985-017-0693-9.
