Abstract
Keywords
1. Introduction
Any interference with the complex process of tooth eruption leads to dental retardation or subsequent dental impaction. Tooth impaction happens when a tooth eruption fails to happen during its general timeline (1). Symptomatic impaction commonly involves patients in their 20s and rarely affects older individuals (2). After mandibular molars, maxillary canines comprise most of the tooth impactions (3). Tooth-size arch-length discrepancies, failure of primary canine root resorption, prolonged retention or an early loss of the primary canine, cysts, and neoplasms locally provoke canine tooth impaction. Furthermore, hereditary disorders such as malposed tooth germ and alveolar cleft or systemic conditions like endocrinopathies, fever, and irradiation may induce tooth impaction (4).
Impacted canine increases the risk of unfavorable sequelae, such as ankylosis, infection, cyst formation, external resorption of the impacted or neighboring teeth, internal resorption of the impacted tooth, and loss of arch length (5). Therefore, physicians and dentists should consider maxillary canine in any suspected patient to avoid the side effects of mismanagement (6, 7). Herein, we present an infectious impacted canine with uncommon clinical manifestations, which was misdiagnosed as acute bronchitis at the initial presentation.
2. Case Presentation
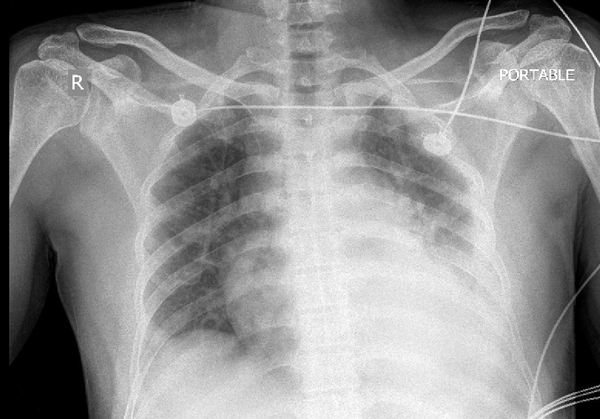
In July 2017, a 38-year-old male presented with pleuritic chest pain, dyspnea, tachycardia, and fever. Two days after the disease onset, swelling and erythema of the face, cheek, eyelids, fever, cold sweating, nasal congestion, hyposmia, and purulent rhinorrhea were added to the previous symptoms. At the time of admission, physical examination revealed fever (temperature: 38°C), a painful localized swelling and erythema on the right cheek, and diminished left lung sounds. Despite the unremarkable past medical history, the chest X-ray (CXR) showed blunted left costophrenic angle indicative of pleural effusion (Figure 1). After ruling out cardiovascular problems by electrocardiography (ECG) and echocardiography, he underwent lung computed tomography (CT) scan without contrast.
Initial CXR illustrating left side.
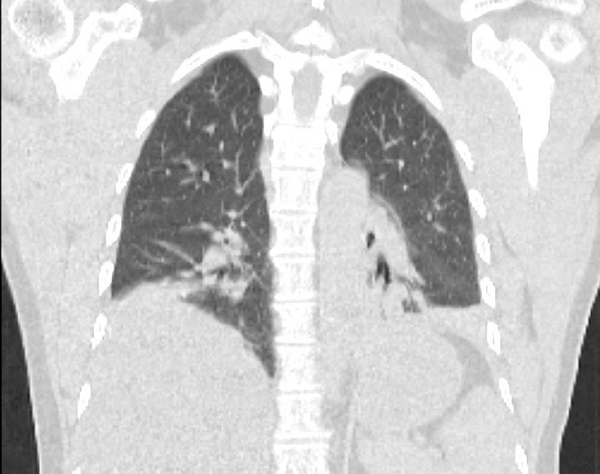
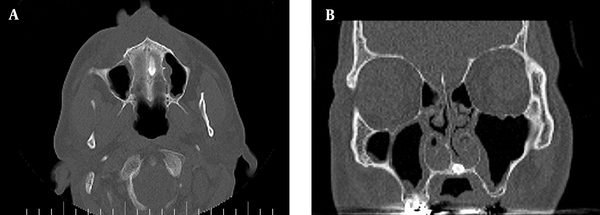
The CT scan displayed linear atelectasis and fibrotic bands on the left lung base. Also, pleural thickening and the presence of fluid and air bubbles in the left pleural space indicated previous pneumothorax or empyema (Figure 2). Laboratory abnormalities including leukocytosis (WBC = 13400 / cmm), elevated erythrocyte sedimentation rate (ESR = 45 mm/hr), and hyperglycemia (fasting blood sugar = 157 mg/dL) were also detected. His condition was misdiagnosed as acute bronchitis, and he received clindamycin and clarithromycin for three days. Since symptoms worsened and vital signs persisted, he underwent a head CT scan, which detected mucosal thickening of maxillary and ethmoidal sinuses along with soft tissue density in the nasal cavity (Figure 3A and B). Since his hyperglycemia increased the suspicion for rhinocerebral mucormycosis, the patient was referred to the Shahid Sadoughi hospital, which a referral center in Yazd, Iran.
CT scan of the chest.
Facial CT scan showing maxillary canin impaction in the left side (A), coronal view of maxillary canin impaction in the left side (B).
After chest tube insertion during the second admission, pleural fluid analysis supported an exudative pleural effusion (glucose: 31 mg/dL, lactate dehydrogenase (LDH): 689 IU/L, protein: 4.1 g/dL, albumin: 2.6 g/dL, neutrophil: 82%, and lymphocyte: 11%). The nasal endoscopy findings, including severe nasal floor swelling and the exposed necrotic nasal septum cartilage from nasal septum mucosal ulcerations, approved nasal septum abscess. After extensive debridement of infectious parts, excessive purulent nasal discharge was aspirated. Subsequently, the patient received broad-spectrum antibiotics (vancomycin, meropenem, clindamycin, teicoplanin, and amphotericin B) that cover possible Staphylococcus aureus and mucormycosis. Amphotericin B was discontinued after necrotic septum culture confirmed the growth of S. aureus and excluded fungal infection.
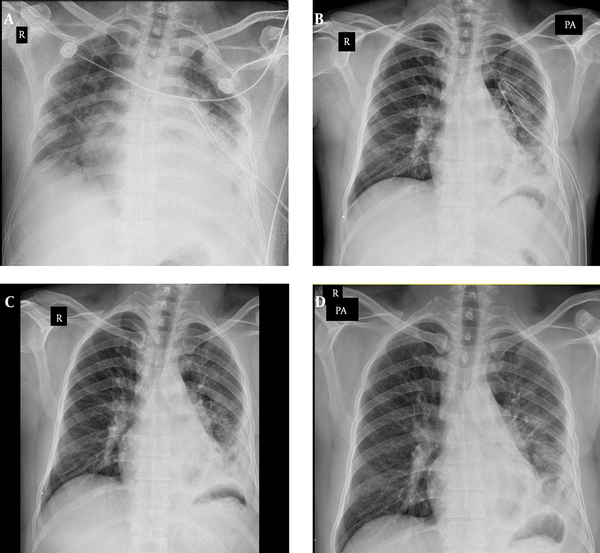
Oral and maxillofacial surgery consult ordered a cone-beam CT (CBCT), through which the infectious impacted canine was diagnosed. The patient was transported to our hospital and underwent surgical extraction of the impacted canine. Three days after surgery, despite hyperglycemia, other symptoms improved significantly, and he was discharged with stable and good general condition (Figure 4A - D).
CXR control of left Chest tube (A). CXR control of left chest tube before surgical extraction (B). CXR control of left chest tube removal (C). Control CXR before patient discharge (D).
3. Discussion
The maxillary canine is located beneath the orbital floor in the upper parts of the anterior wall of the maxillary sinus, and its germ development starts at the 4th or 5th months of life. The maxillary canine generally travels across the mesial path to the distal aspect of the lateral incisor root. Then, it becomes upright and erupts vertically with the guidance of the lateral incisor root (8). Maxillary canine impaction involves 2% of the general population with female predominance (7). Family history of an impacted canine, physical examination in 9 - 10 years of age, and radiographic assessments facilitate early detection of this abnormality (9). Most tooth impactions originate from the palatine process of the maxilla, and the labial aspect of maxillary bone rarely becomes involved. Like this patient, tooth impaction is associated with various complications that warrant routine dental examination during childhood. Clinical presentations that indicate an impacted canine are as follows: Delayed eruption of permanent canine beyond 14 - 15 years of age, absence of normal labial canine bulge, presence of palatal bulge, and delayed eruption, distal tipping, or migration (splaying) of the lateral incisor (7). Various clinical and radiographic evaluations are required to prove the presence and location of the impacted canine. The position of adjacent teeth, the amount of space in the dental arch, bone contours, and the mobility of teeth should be assessed carefully during physical examination (7). Panoramic, lateral, occlusal, and periapical are helpful radiographic views to identify the impacted canine (10).
Currently, CBCT is a three-dimensional imaging modality that locates canine impaction and distinguishes it from the adjacent teeth with high diagnostic accuracy (11, 12). Treatment for impacted canine is surgical excision or uncovering recommended for functional and aesthetic benefits (7). An impacted canine is usually painless; it can elicit severe discomfort when it becomes infected to pressure the adjacent nerves. These patients might also experience headaches, halitosis, gingival erythema, bleeding, swelling, and painful jaw movements (12). The spread of impacted canine infection to sinuses, brain, and circulatory system may lead to catastrophic consequences such as cardiac or cerebral damage or even death (13).
However, pleural space is an uncommon site of infection spread in infectious canine impaction and should be differentiated from other respiratory disorders such as acute bronchitis. Aside from complications related to local effects of canine impaction, it has shown mutual interactions with systemic pathologies like diabetes (14). Here, we reported hyperglycemia in this patient without a history of diabetes that remained unchanged a few months after discharge (14, 15).
3.1. Conclusions
This case report emphasized that patients with impacted canine might present with various local and systemic manifestations. A misdiagnosed and subsequent mismanaged impacted canine increases the risk of unfavorable complications and necessitates more complex treatments. Therefore, a thorough clinical examination and imaging (especially CBCT) should be performed to detect the impacted canine in suspected cases as soon as possible. Surgical treatment should be the first choice of therapy in these patients.
References
-
1.
Dekel E, Nucci L, Weill T, Flores-Mir C, Becker A, Perillo L, et al. Impaction of maxillary canines and its effect on the position of adjacent teeth and canine development: A cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2021;159(2):e135-47. [PubMed ID: 33388201]. https://doi.org/10.1016/j.ajodo.2020.10.015.
-
2.
Lovgren ML, Dahl O, Uribe P, Ransjo M, Westerlund A. Prevalence of impacted maxillary canines-an epidemiological study in a region with systematically implemented interceptive treatment. Eur J Orthod. 2019;41(5):454-9. [PubMed ID: 31369665]. https://doi.org/10.1093/ejo/cjz056.
-
3.
Hamada Y, Timothius CJC, Shin D, John V. Canine impaction – A review of the prevalence, etiology, diagnosis and treatment. Semin Orthod. 2019;25(2):117-23. https://doi.org/10.1053/j.sodo.2019.05.002.
-
4.
Hamada Y, Timothius CJC, Shin D, John V. Reprint of canine impaction - A review of the prevalence, etiology, diagnosis and treatment. Semin Orthod. 2021;27(1):27-33. https://doi.org/10.1053/j.sodo.2021.03.002.
-
5.
Al-Abdallah M, AlHadidi A, Hammad M, Dar-Odeh N. What factors affect the severity of permanent tooth impaction? BMC Oral Health. 2018;18(1):184. [PubMed ID: 30382922]. [PubMed Central ID: PMC6211474]. https://doi.org/10.1186/s12903-018-0649-5.
-
6.
Gisakis IG, Palamidakis FD, Farmakis ET, Kamberos G, Kamberos S. Prevalence of impacted teeth in a Greek population. J Investig Clin Dent. 2011;2(2):102-9. [PubMed ID: 25426603]. https://doi.org/10.1111/j.2041-1626.2010.00041.x.
-
7.
Manne R, Gandikota C, Juvvadi SR, Rama HR, Anche S. Impacted canines: Etiology, diagnosis, and orthodontic management. J Pharm Bioallied Sci. 2012;4(Suppl 2):S234-8. [PubMed ID: 23066259]. [PubMed Central ID: PMC3467862]. https://doi.org/10.4103/0975-7406.100216.
-
8.
Arriola-Guillen LE, Aliaga-Del Castillo A, Ruiz-Mora GA, Rodriguez-Cardenas YA, Dias-Da Silveira HL. Influence of maxillary canine impaction characteristics and factors associated with orthodontic treatment on the duration of active orthodontic traction. Am J Orthod Dentofacial Orthop. 2019;156(3):391-400. [PubMed ID: 31474269]. https://doi.org/10.1016/j.ajodo.2018.10.018.
-
9.
Kokich VG. Surgical and orthodontic management of impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2004;126(3):278-83. [PubMed ID: 15356485]. https://doi.org/10.1016/j.ajodo.2004.06.009.
-
10.
Margot R, Maria CL, Ali A, Annouschka L, Anna V, Guy W. Prediction of maxillary canine impaction based on panoramic radiographs. Clin Exp Dent Res. 2020;6(1):44-50. [PubMed ID: 32067406]. [PubMed Central ID: PMC7025989]. https://doi.org/10.1002/cre2.246.
-
11.
Mah J, Enciso R, Jorgensen M. Management of impacted cuspids using 3-D volumetric imaging. J Calif Dent Assoc. 2003;31(11):835-41. [PubMed ID: 14696835].
-
12.
Alhummayani FM, Mustafa ZA. A new guide using CBCT to identify the severity of maxillary canine impaction and predict the best method of intervention. J Orthod Sci. 2021;10:3. [PubMed ID: 34084759]. [PubMed Central ID: PMC8102933]. https://doi.org/10.4103/jos.JOS_41_20.
-
13.
Obiechina AE, Arotiba JT, Fasola AO. Third molar impaction: evaluation of the symptoms and pattern of impaction of mandibular third molar teeth in Nigerians. Tropical Dental Journal. 2001:22-5.
-
14.
Shiva A, Maboudi A, Arab S. A review of the complications and oral manifestation of diabetes mellitus. ClinExc. 2016;5(2):17-27.
-
15.
Kudiyirickal MG, Pappachan JM. Diabetes mellitus and oral health. Endocrine. 2015;49(1):27-34. [PubMed ID: 25487035]. https://doi.org/10.1007/s12020-014-0496-3.