Introduction
Historically, recurrent patellar instability was surgically managed with lateral retinacular release, trochleoplasty, proximal or distal realignment surgery or a combination of these techniques. In the early 1990s, the significance of the medial patellofemoral ligament (MPFL) was recognized as the primary soft-tissue restraint to lateral displacement of the patella.1,2 Its contribution is reported to range from 50% to 60% in the range of 0° to 30° of knee flexion.1,3,4 After acute dislocation of the patella, the medial retinaculum and MPFL are frequently torn in as high as 94–98 % of patients.5,6 In the light of these findings, MPFL reconstruction has been gaining more and more popularity either alone or in combination with other procedures.7
Although both the anatomic and biomechanics of the MPFL have been well studied, a lack of knowledge regarding its morphology and attachment sites as well as its mechanical properties remains.8 It is believed that this is the reason why there is no consensus about which technique is considered the gold standard for MPFL reconstruction.9 Generally, MPFL reconstruction techniques can be divided into two broad categories; the ‘bone socket’ and ‘non- bone socket’ techniques. The former refers to the formation of tunnels or sockets in the patella in order to pass and fix the graft while the latter is about fixing graft to the cortical surface of the patella with sutures or with sutures anchors. With respect to bone socket approach, the fixation of the graft into the patella can be implantless or can be done with either an endobutton device or an interference screw fixation. A recent systematic review conducted by Desai et al. revealed that the two categories have comparable results in term of redislocation rates and patient outcomes making both of them an acceptable option for MPFL reconstruction.10
The purpose of this review is to examine the role of endobutton in MPFL reconstruction, the different related techniques and how this device is utilized to secure the graft into the patella.
Methods
A systematic electronic database search was undertaken using PubMed, Cochrane library and Scopus databases. The databases were searched until April 2023.The search terms used were [(Medial Patellofemoral Ligament) OR (MPFL)] AND (Reconstruction)]. All relevant studies were identified and additionally the reference lists of investigated studies were also examined. Non-human, cadaveric studies and those with no more than 5 patients are excluded.
Endobutton concept
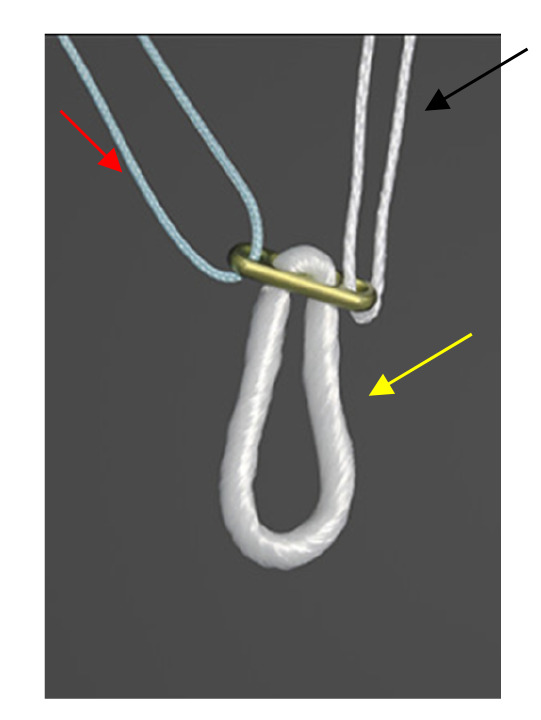
The endobutton was first introduced in 1993 by Rosenberg as a promising femoral fixation with semitendinosus grafts in anterior cruciate ligament (ACL) reconstruction. Endobutton is considered a cortical suspension device which in its most primitive form (Smith and Nephew, Andover, MA) consisted of an oval button with a woven loop passed through its 2 central holes.11 The loop serves to connect the graft to the button as well as to increase the length of the entire graft construct. In this type of fixation, resistance vectors are parallel and opposite to pullout forces, and are focused on the cortical bone of the distal femur, at the bone – hardware interface. In consequence, the smaller the contacts surface of the fixation device, the more considerable the load concentration. The contact surface of the fixation device can differ, depending on the design of the device.12
Currently, there are two main types of cortical suspension devices; fixed-loop and adjustable-loop (Figure 1). With the fixed-loop cortical suspension device, the graft is attached to a continuous suture loop connected to a button, which is flipped and then fixed at the cortical cortex, and the tunnel is filled with the graft without any implant. On the contrary, the second type of cortical suspension device has a button attached to the graft through the adjustable loop, and the loop is tightened to pull the graft through to the top of the tunnel. Both of them have advantages and disadvantages which should be taken into consideration. So, although fixed-loop devices yield good graft fixation when it comes to mitigating graft slippage and providing sufficient graft strength, the requirement of drilling the bone socket to a specific tunnel depth to flip a button raises concerns regarding bone preservation, stability of the tendon graft, and tendon-bone healing as a result of insufficient graft length. On the other hand, adjustable-loop devices address these challenges giving the surgeon the flexibility to adapt to different tunnel lengths intraoperatively, thus obviating the need for drilling a longer tunnel and maximizing the amount of graft within the tunnel by not leaving excess space in the bone tunnel. That being said, one serious drawback associated with these devices is the fact that their flexibility regarding loop length may allow for increased graft slippage postoperatively.13 With respect to which type of device is superior, it seems that both fixed loop and adjustable loop devices in ACL reconstruction provided good clinical and radiological outcomes.14,15
Over the last two decades, the endobutton fixation device has gained an increased popularity and become a trusted choice not only in ACL reconstruction but also in other areas of orthopaedic. With respect to MPFL reconstruction, the first procedure with endobutton was conducted in 1999 by Muneta et al.16
Technical considerations
Single tunnel medial patellofemoral ligament reconstruction
MPFL reconstruction was first described in 1992, using an allograft attached from the medial femoral condyle to the patella. Today, one popular technique involves drilling patella bone sockets or tunnels so as to pass and fix the graft. The first who used an endobutton device for the fixation of the graft into the patella was Muneta et al in 199916. His case series consisted of 6 patients. The graft selected was one of the three; gracilis tendon, semitendinosus tendon and iliotibial band allograft. The MPFL reconstruction was achieved by using a looped tendon graft with two small incisions at the medial edge of the patella and at the medial femoral epicondyle. Regarding the fixation of the graft into the patella, a 4.5-mm drill hole was made parallel to the articular surface from the middle of the medial edge to the center of the patella. Next, a second 3.2 drill hole was made to the anterior surface of the patella in an oblique fashion so that the connection of the 2 holes would create a curved pathway (Figure 2). The author believed that in this way the possibility of patella fracture postoperatively would be minimized. Depending on the size of the graft, the 4.5 drill hole at the medial edge of the patella was widened accordingly. Unfortunately, apart from the fact that the graft was fixed at the patella site with a button, the author did not mention more details about the fixation. Finally, after the determination of the isometric point, the femoral attachment of the graft was secured with a staple with the knee in 90° of flexion. The results were promising without incidences of redislocations. Among the complications reported, there was one patient with 10° of flexion loss while a difficulty in regaining deep flexion was also noticed. Moreover, one patient complained for hypoesthesia in the area innervated by the saphenous nerve. No patient-reported outcome scores were used to measure knee function.
A similar concept was also followed by Kumar et al. who performed MPFL reconstruction in 30 patients.17 His procedure was near to that mentioned above but there were also some important differences. So, reconstruction of the MPFL was also performed via two small incisions, at the superior-medial corner of the patella and at the medial aspect of the medial condyle, using a double strand gracilis graft. However, instead of a curved tunnel, this author decided to make a longitudinal tunnel in the patella (Figure 2). Specifically, a guide pin penetrated the patella having as starting point its proximal medial edge. The depth of the patella tunnel was limited to 20mm while the diameter was adjusted correlating with the graft size. The diameter of the reamer used was depended on the size of the looped graft while the rest of the tunnel was completed with the 4.5 mm drill. It is interesting to note that given the fact that the average patella width is 40- 49 mm and the shortest endobutton loop is 15 mm. To achieve at least 25 mm of graft in the patella bone socket, the total channel length must be at least 40 mm. So, we hypothesized that in most cases the author would not face the problem that the bone socket would be too short. No information was given about the company of the endobutton device. What is more, the femoral attachment was secured with a bioabsorbable screw with the knee in 30-45° of flexion. The clinical outcomes were excellent in terms of complications and patients’ functionality.
Another case series published by Khekma et al. aimed to restore MPFL anatomy using synthetic allograft (LARS Ligament, CORIN Ltd, Mersilene Tape MT, or AchilloCordPLUS Ligament, Neoligaments Ltd).18 For this purpose, MPFLs were reconstructed through graft endobutton fixation into the patella. The rationale of his technique was analogous with those mentioned above. However, the bone tunnel in the patella was 3.2 mm in size instead of 4.5mm. Beside this, one main divergence from the other techniques was the fact that with respect to femoral fixation the graft was passed through the tunnel (3.2mm) and secured in the lateral femoral cortex with an interference peek screw with the knee in flexion. The latter was feasible seeing that by using an artificial ligament as a graft there is no limitation about the length. No information was provided neither for the characteristics of endobutton used nor for how much graft was introduced into the patella tunnel. In general, excellent to good clinical results were observed with statistically important improvement in functional and radiological outcomes.
Finally, there are two other comparative studies which contrasted MPFL reconstruction through graft endobutton fixation into the patella with that using anchor fixation.19,20 The first study conducted by Astur et al. whose principles were much the same with Kumar et al. Nevertheless, the size of patella tunnel was 6mm regardless of graft’s size while the exact depth of the graft into the tunnel was not specified. No details about the characteristics of endobutton used were provided. The second study differed from the previous two in the fact that the graft chosen for the reconstruction was the semitendinosus tendon. Although there was information about the company of endobutton (Endobutton CL Fixation, Device Smith &Nephew, and Huntingdon, UK) details about the size of the patella tunnel as well as the depth of the graft into the tunnel were not given. The two studies reached in different deductions. Thus, while the first study found similar results among the two techniques the second one demonstrated that MPFL reconstruction via anchor fixation was superior
Dual tunnel medial patellofemoral ligament reconstruction
A case series study which is differentiated from the other 2 techniques was that of Toritsuka et al. published in 201021. In an attempt to recreate a more anatomical reconstruction, he decided to make two bone tunnels in the patella (Figure 2). Based on anatomical studies, he concluded that one bone tunnel is not satisfactory to recreate the normal anatomy of the MPFL, given that MPFL described as a fanlike structure and not as a single cord. In addition to this, two smaller drill holes are less likely to cause patellar fracture than a larger one. Furthermore, he chose to fix the graft on the femur with endobutton instead of screw or staple. Although he justified the endobutton option in terms of patella fixation, as it was proven that pull-out fixation was biomechanically superior to sutures or anchors, he did not mention the reason to do this for femur fixation. In detail, a double strand semitendinosus graft and two endobuttons (Smith and Nephew, Andover, MA) were used for the reconstruction. For the femoral side, the semitendinosus graft was passed through a No 6 braided polyester suture and doubled back on itself while for the patella side No 3 braided polyester sutures were put in the free ends of the graft in a Krakow fashion. After both the graft preparation and diagnostic arthroscopy, he proceeded with transverse incision extending from 1 cm medial to the medial edge of the patella to just posterior to the medial epicondyle. Under x-ray control, two guide wires were transversely inserted, one from proximal one-third of the medial edge of the patella and another from the center of the patella. Patellar guide wires were then overdrilled using a 4.5- mm cannulated reamer to create bone sockets 1cm in depth. Subsequently, another 2.4-mm guide wire was inserted from the femoral insertion site toward the proximal cortex of the lateral femoral condyle and was over-drilled using a 5–6mm diameter according the diameter of the graft. The two free ends of the graft were pulled into the bone sockets of the patella and fixed on its lateral side by tying the sutures over the endobutton. Next, the center of the graft was introduced into the femoral socket and fixed in a similar way with the knee in 45 degrees of flexion with proper tension applied. In this point, it should stressed that the author omitted to mention that for tying the sutures over the endobutton on patella side, it might be necessary to perform a small incision on the lateral aspect of the patella.
Kita et al. published two studies (case series) using a modification of the dual-tunnel MPFL reconstruction technique reported by Toritsuka.21,22 The differences were that the patellar bone sockets were 15 mm in depth instead of 10 mm and the depth of the femoral socket (20mm) was also noted. Additionally, it is of note that the femoral fixation performed first. It was not clearly stated but we hypothesized that regarding the femoral fixation the graft was passed through a loop in the middle two holes of the endobutton while for the patella fixation the graft was fixed by tying the sutures over the endobutton at 45° of knee flexion.
All of the 3 case series showed an increase in the Kujala scores with low rates of postoperative complications. Overall, form the 89 knees operated only two incidences of redislocation were reported while the number of fractures was also low (4). Among the most common complaints were a slight loss of knee flexion and a mild knee pain. The different technical characteristics of each study are shown in Table 1.
Summary
Among the many procedures for MPFL reconstruction, the bone socket techniques using endobutton devices seem to be a reliable choice with acceptable clinical outcomes. Interestingly, none of the studies used an adjustable loop device while it is also of note that many studies lack of important information about the company of the endobutton used and details about the fixation such as the size of the patellar tunnel and the depth in which the graft was introduced into the patella. Not only should these data not be omitted, but on the contrary a painstaking attention to detail is necessary. In this way, a better understanding will be provided when it comes to complications and it will also contribute to improve the technique. Finally, given that most of the studies are case series it is imperative more randomized controlled trials comparing the different techniques must be done so that a safer conclusion can be drawn regarding the outcomes.
Author contribution
Conceptualization, G.K.; methodology, G.K and I.V and E.G.; writing—original draft preparation, G.K.; writing—review and editing G.K and K.M.; supervision, C.K.Y.; Final manuscript approval, C.K.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest