Published online Aug 28, 2021. doi: 10.4329/wjr.v13.i8.243
Peer-review started: January 28, 2021
First decision: May 6, 2021
Revised: May 18, 2021
Accepted: August 2, 2021
Article in press: August 2, 2021
Published online: August 28, 2021
Given the several radiological features shared by coronavirus disease 2019 pneu
To conduct a systematic review including the available studies evaluating com
Using pertinent keywords, we performed a systematic review using PubMed to select relevant studies published until October 30, 2020.
Of the identified 133 studies, 18 were eligible and included in this review.
Ground-glass opacity and consolidations are the most common computed to
Core Tip: In the coronavirus disease 2019 era, the differential diagnosis of pneumonitis, already challenging in patients with multiple comorbidities and polypharmacological therapy, has become even more challenging. The gold-standard technique for diag
- Citation: Perrone F, Balbi M, Casartelli C, Buti S, Milanese G, Sverzellati N, Bersanelli M. Differential diagnosis of COVID-19 at the chest computed tomography scan: A review with special focus on cancer patients. World J Radiol 2021; 13(8): 243-257
- URL: https://www.wjgnet.com/1949-8470/full/v13/i8/243.htm
- DOI: https://dx.doi.org/10.4329/wjr.v13.i8.243
The coronavirus disease 2019 (COVID-19) outbreak began in Wuhan, China, in late 2019 and rapidly spread worldwide at the beginning of 2020, when it was declared a global pandemic by the World Health Organization[1,2]. Many jurisdictions in several states carried out public health interventions to contain the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)[3]. Europe is now experiencing a second wave of contagion[4].
The virus has a specific tropism for the lower respiratory tract, and it is the cause of mild to severe respiratory infection[5].
Imaging has been widely employed to triage the massive load of acute respiratory referral due to COVID-19 by complementing the nucleic acid testing (i.e., the diag
Many of the hallmark CT findings are apparent on chest X-ray, which is prone to miss subtle GGO, even if relatively diffuse in extent. Nevertheless, chest X-ray has shown the potential to predict outcomes in relatively advanced disease stages, assess supervening complications, and monitor the disease course[10]. Lung ultrasound was suggested as a fast and feasible approach for triaging COVID-19 patients by identi
It is worth emphasizing that the imaging appearance of COVID-19 is non-specific, and the performance of different modalities dramatically relies on the disease prevalence. The typical manifestations may mimic or overlap with other infective and non-in
In the present article, we performed a systematic review of the literature focusing on differential radiological diagnosis between COVID-19 pneumonia and other infective and non-infective lung diseases, then discussing possibly helpful clinical elements and finally focusing on this issue in cancer patients.
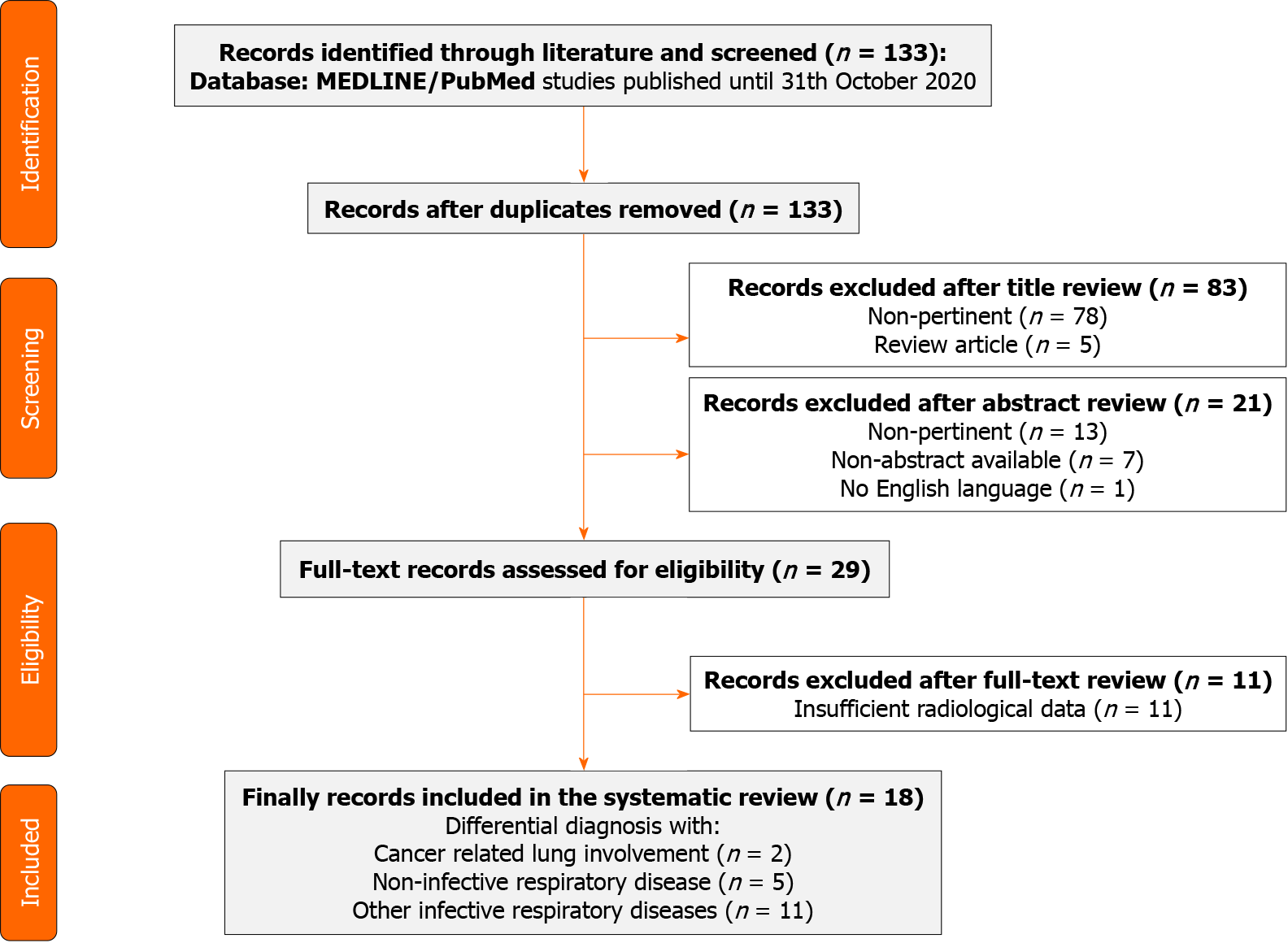
We conducted this systematic review according to the Preferred Reporting Items gui
Two authors (CC and FP) carried out a comprehensive systematic search for published articles on the MEDLINE/PubMed library until October 31, 2020. Given the absence of articles on this topic before December 2019, when the first COVID-19 outbreak started, no upper limit for the search was chosen.
The following search keywords were used: “COVID-19” AND “computed tomo
Retrospective studies, prospective studies, and case reports describing the difference between CT signs caused by SARS-CoV2 infection and other respiratory and non-respiratory diseases were included. Only English-language articles were considered eligible. Studies with insufficient radiological data or focused on non-CT radiological findings (i.e., ultrasound or radiography) were excluded. We planned qualitative ana
Narrative papers, such as commentaries and editorials, were excluded from the formal qualitative analysis, but the most relevant articles discussing the issue were considered in the discussion.
The study characteristics (first author, year of publication, type of study, number of patients included, disease of comparison assessed, and main radiological similarities and discrepancies, laboratory findings) were extracted from the included articles by a single author (FP). Two reviewers (FP and CC) initially performed the data extraction, and then it was independently reviewed by an additional reviewer (MB).
Any doubt or disagreement was discussed with a fourth investigator (SB) and resol
Of the 133 studies found in the search, 104 were initially excluded by title and abstract reading. After reading the full text of the remaining 29 articles, 11 were excluded because they missed relevant radiological information or comparison between diffe
Trial characteristics and the main results of the studies included are reported in Table 1. Among the 18 studies included, 5 were case report/case series[16-20], and 13 were retrospective[21-33]. All the studies described the typical radiological characteristics of COVID-19 pneumonia and addressed the radiological differential diagnosis issue. The difference between COVID-19 and non-infective respiratory diseases, namely: Systemic sclerosis and granulomatosis with polyangiitis (n = 2)[30,31], fat embolism (n = 1)[32], pulmonary contusion (n = 1)[33] were evaluated in 5 out of 18 studies. One study evaluated both heart failure-induced pulmonary edema and rheu
| Ref. | Yr | Type of study | Patients, n | Disease in differential diagnosis | Radiological similarities with COVID-19 disease | Radiological discrepancy with COVID-19 disease | Laboratory findings |
| Dai et al[16] | 2020 | Case series | 4 pts COVID-19 positive. 1 pts heart failure induced pulmonary edema. 1 pts rheumatic pneumonia. | Heart failure induced pulmonary edema. Rheumatic pneumonia. | Local or multiple GGOs. Patchy high-attenuation patterns. Sporadic or local interlobular septal thickening. Patchy GGOs and consolidations; interlobular septal thickening. | Butterfly sign. Peribronchial cuffing. Redistribution of blood flow in both lungs. | Normal WBC count, D-dimer, hs-CRP. RT-PCR for SARS-CoV-2 negative. Normal WBC and lymphocyte count, high hs-CRP, D-dimer, rheumatoid factor. RT-PCR for SARS-CoV-2 negative. |
| Orlandi et al[17] | 2020 | Case report | - | Systemic sclerosis ILD | Bilateral GGOs with or without consolidations. Reticulations. | Limited to lower lobes. Honeycombing pattern. | RT-PCR for SARS-CoV-2 negative |
| Shenavandeh et al[18] | 2020 | Case report | 1 | Granulomatosis with polyangiitis | GGOs and consolidation | Nodules and mass lesions | - |
| Chen et al[20] | 2020 | Case report | 1 | Pulmonary contusion | GGOs and consolidation | More consolidations. Less combined with pleural effusion and subpleural atelectasis. Different time evolution of lesions. | High WBC count and mild decreased of lymphocyte count |
| Mazouz et al[19] | 2020 | Case report | 1 | Fat embolism | Bilateral GGOs | Central and peripherical involvement | High CRP, alkalosis with hypoxemia, normal lymphocyte count. RT-PCR for SARS-CoV-2 negative. |
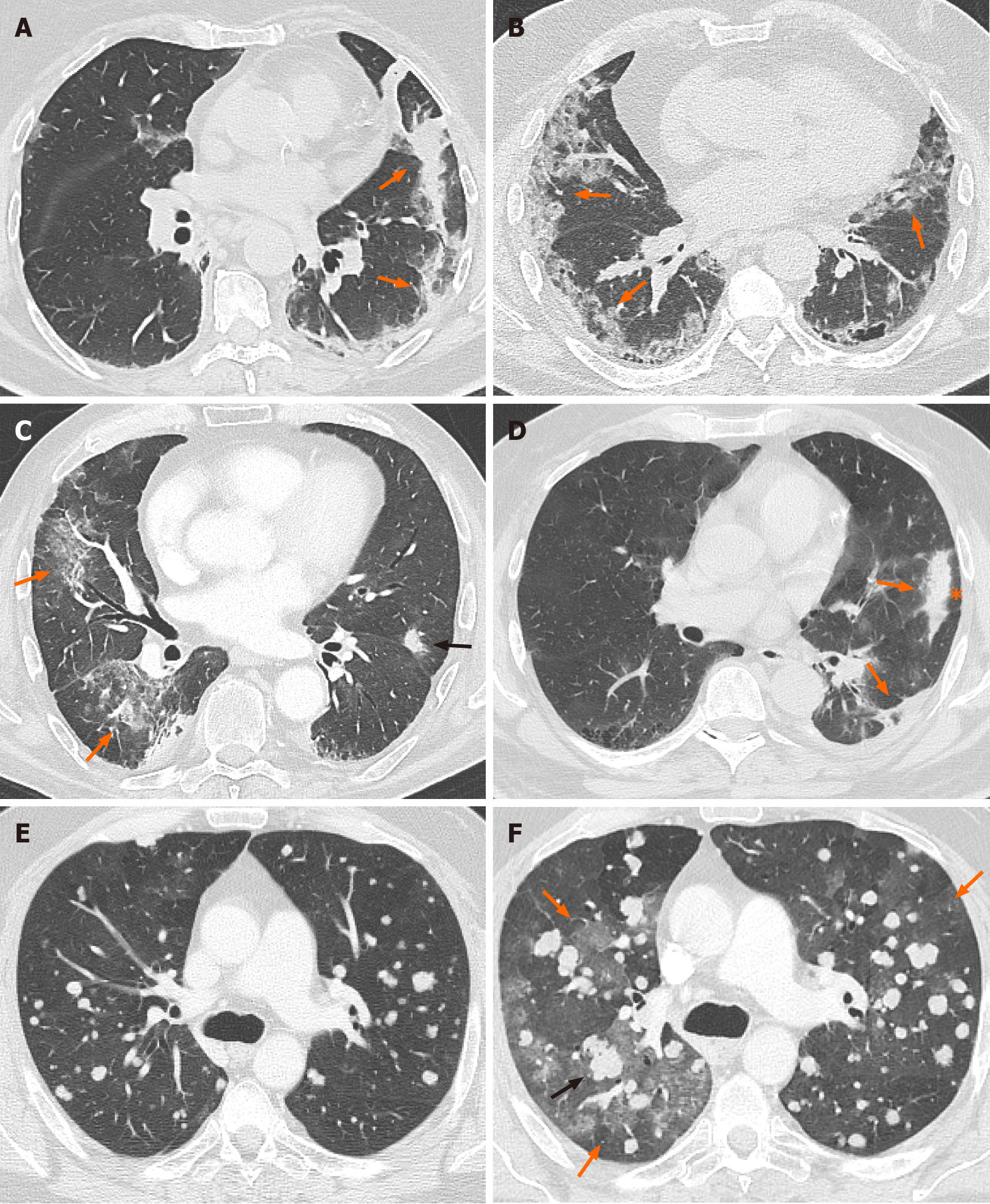
| Zhang et al[29] | 2020 | Retrospective | 157 pts COVID-19. 374 pts with early lung cancer. | Early lung cancer | Air bronchogram. Cystic change. | Less lobes and segments involved. Unilateral oval lesions. Pure or mixed GGOs. Lobulated sign, pleural retraction and vessel convergence sign. Less lymphadenopathies and pleural effusion. | Higher WBC and lymphocyte count, lower D-dimer level. |
| Zeng et al[28] | 2020 | Retrospective | 112 pts COVID-19 positive or suspected. 4 pts with radiation pneumonitis. | Radiation pneumonitis | GGOs with consolidation. Air bronchogram. Irregular intralobular or interlobular septal thickening. Fibrosis in late stage. | Onset within 6 mo after radiation. Slow evolution. Lesions confined to radiation fields. | High WBC count, D-Dimer, CRP and PCT, marked lymphopenia. RT-PCR for SARS-CoV-2 negative. |
| Himoto et al[27] | 2020 | Retrospective | 21 pts COVID-19 positive. 15 pts with viral or bacterial pneumonia. | Pneumococcal pneumonia, Moraxella pneumonia, Legionella pneumonia, not-specified bacterial or viral pneumonia. Pneumocystis pneumonia and interstitial pneumonia. | Bilateral peripherical GGOs. No cavitation, airway abnormalities, pleural effusion, and mediastinal lymphadenopathy. | Less lobes involved. No rounded morphology lesions. | RT-PCR for SARS-CoV-2 negative |
| Luo et al[22] | 2020 | Retrospective | 30 pts COVID-19 positive. 43 pts with viral or bacterial pneumonia. | Influenza pneumonia, Pneumocystis carinii pneumonia, Mycoplasma pneumonia and CAP. | GGOs with or without consolidation | Less lobes involved. Peribronchovascular distribution. Centrilobular nodules. Bronchial wall thickening. | WBC and lymphocyte count normal, but lower in COVID-19 positive patients. RT-PCR. |
| Xie et al[26] | 2020 | Retrospective | 12 pts COVID-19 positive. 16 pts COVID-19 negative. | COVID-19 negative | Bilateral multiple lung involvement, large irregular/patchy opacities, rounded opacities and linear opacities, crazy-paving patterns, interlobular septal, pleural and peribronchovascular interstitial thickening, air bronchograms, tree-in-bud patterns. | More central distribution of lesions. Less frequent rounded opacities. | Higher level of neutrophil count in COVID-19 negative. RT-PCR. |
| Bai et al[21] | 2020 | Retrospective | 219 pts COVID-19 positive. 205 pts with viral pneumonia. | Viral pneumonia | Bilateral, multiple GGOs, consolidation, nodules. Septal thickening. | More central + peripheral distribution. More air bronchogram, pleural thickening, pleural effusion and lymphadenopathy. | Higher WBC and lymphocyte count in patients with viral pneumonia. RT-PCR. |
| Chi et al[32] | 2020 | Retrospective | 17 pts COVID-19 positive. 51 pts with viral or bacterial pneumonia. | Influenza A and B. Adenovirus. Chlamydia pneumonia. Mycoplasma pneumonia. | - | INFLUENZA A: scattered and patchy shadows and nodular shadows in both lungs. INFLUENZA B: subpleural patchy shadows. ADENOVIRUS: consolidation near the pleura. CHLAMYDIA PNEUMONIAE: multiple GGOs and consolidations in both lungs. MYCOPLASMA PNEUMONIAE: bronchial wall thickening, centrilobular nodules, GGOs and consolidation. | Higher WBC count, RT-PCR |
| Li et al[24] | 2020 | Retrospective | 43 pts COVID-19 positive. 49 pts with CAP. | CAP | - | More nodular or consolidation shadows with or without patchy GGOs. Less fine mesh changes, small vessels dilatated, bronchiectasis and lesion with long axis parallel to the pleura. | RT-PCR |
| Liu et al[25] | 2020 | Retrospective | 165 pts COVID-19 positive. 118 pts with CAP. | CAP | - | More central distribution. More frequent single lesion. GGOs rapid changes in consolidation. Fibrous cord and bronchial wall thickening. | Normal WBC count, higher lymphocyte count and CRP. RT-PCR. |
| Zhou et al[31] | 2020 | Retrospective | 149 pts COVID-19 positive. 97 pts with CAP. | CAP (Streptococcus. pneumoniae) | - | More consolidation lesions, bronchial wall thickening, centrolobular nodules and pleural effusion. Less GGOs, crazy paving sign and abnormally thickened interlobular septa. | High WBC count, neutrophils count and CRP. Rt-PCR. |
| Liu et al[23] | 2020 | Retrospective | 122 pts COVID-19 positive. 48 pts with influenza pneumonia. | Influenza pneumonia | GGOs with consolidation. Nodules. Linear opacities. Interlobular septal thickening tree-in-bud sign. | More nodules, pleural effusions and tree-in-bud sign. Central + peripheral distribution. | RT-PCR for influenza or SARS-CoV-2. |
| Zhao et al[33] | 2020 | Retrospective | 31 pts COVID-19 positive. 18 pts with influenza pneumonia. | Influenza pneumonia | - | More consolidations and pleural effusions. | RT-PCR |
| Wang et al[30] | 2020 | Retrospective | 13 pts COVID-19 positive. 92 pts with influenza pneumonia. | Influenza pneumonia | GGOs and GGOs with consolidation | Inferior lobe involved. Cluster-like GGOs. Lesion with vague margin. Bronchial wall thickening. | Normal WBC count. Low lymphocyte count in Influenza B. No significative difference between two groups. RT-PCR. |
On the other hand, 11 studies explored the CT imaging differences between COVID-19 disease and other infective pneumonia. In particular, the differential diagnosis was performed with influenza pneumonia (n = 3)[23,30,33], community-acquired pneumo
Only two studies included cancer patients. One assessed the radiological discrepancies between COVID-19 disease with lung involvement and radiation pneumonitis[28]. In the other study, the differential diagnosis regarded early lung cancer[29].
In the majority of studies, detection of SARS-CoV-2 was performed by RT-PCR on throat/nasopharyngeal swab. The laboratory test was lacking in only one study, in which the final diagnosis was carried out based on clinical and epidemiological find
In the following paragraphs, the findings of the included studies are reported by topic.
The radiological difference between COVID-19 pneumonia and heart failure-induced pulmonary edema was evaluated by Dai et al[16].
Although GGOs and interlobular septal thickening were CT manifestations shared by both diseases, butterfly signs (patchy high attenuation patterns and large patchy high attenuation patterns in both lungs), peribronchial cuffing, and redistribution of blood flow in both lungs were typical in heart failure pulmonary edema.
Three rheumatologic diseases, namely systemic sclerosis, granulomatosis with polyangiitis, and rheumatic disease, often caused lung involvement with GGOs. Pre
According to Shenavandeh et al[18], pulmonary nodules, mass lesions, and consolidation caused by lung hemorrhage and infarction due to small vessel vasculitis were typical for granulomatosis with polyangiitis.
Finally, extensive patchy exudates and consolidations in both lungs, faint GGOs on edge, and interlobular septal thickening were characteristic features for rheumatic pneumonia observed by Dai et al[16].
Although GGOs and consolidation characterized pulmonary contusion (usually caused by traffic accidents, falls, bumps, and crashes), a higher proportion of consolidations often associated with bilateral pleural effusion and subpleural atelectasis was observed when compared to COVID-19 disease. In addition, the radiological evolution was different in the two illnesses. No signs or few sheet shadows may be observed in pulmonary contusion 4-6 h after injury. The lung returned to normal after 7-10 d. Otherwise, in the case of COVID-19, the radiological pattern was long-lasting[20].
As in COVID-19 disease, bilateral GGOs with multilobe central and peripheral involvement were observed by Mazouz et al[19] in the case of fat embolism.
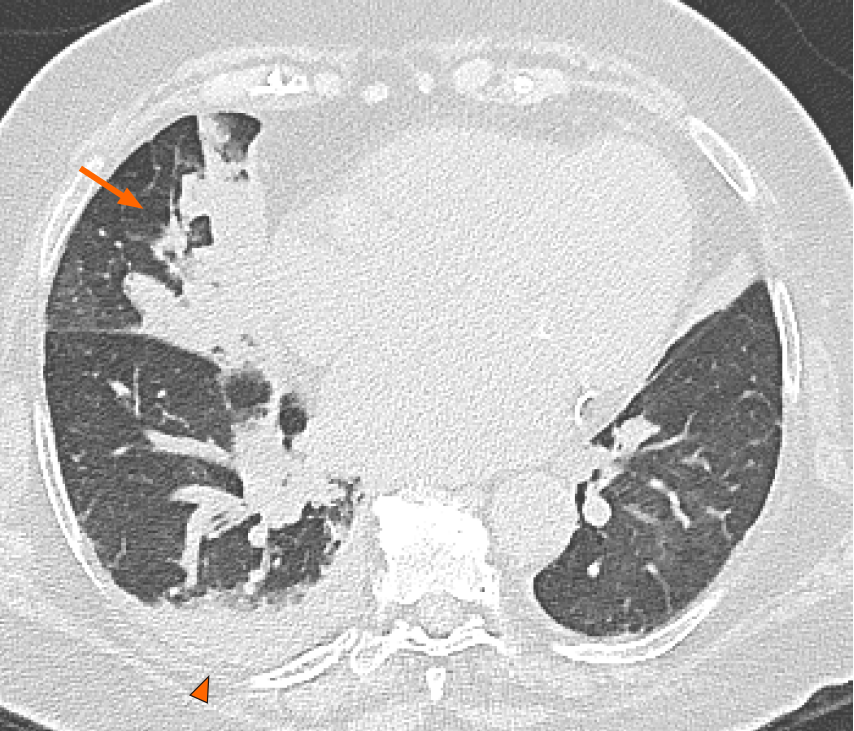
One out of two studies including cancer patients investigated the difference between COVID-19 disease and pulmonary toxicities caused by radiotherapy. GGOs with par
The study on cancer patients conducted by Zhang et al[29] focused on the simi
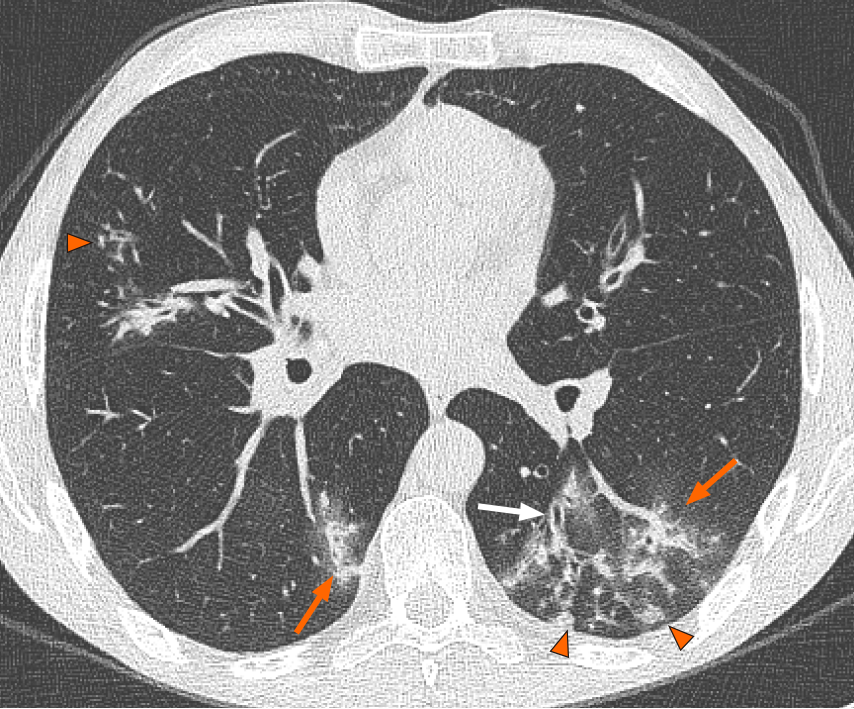
In a retrospective study, Himoto et al[27] used five chest CT criteria to distinguish COVID-19 pneumonia from other infective respiratory diseases, such as Pneumococcal pneumonia, Moraxella pneumonia, Legionella pneumonia, not-specified bacterial or viral pneumonia, Pneumocystis pneumonia, and non-specific interstitial pneumonia. The differential patterns evaluated were: (1) GGO-predominant lesions; (2) GGO- and peripheral-predominant lesions; (3) bilateral GGO-predominant lesions; (4) bilateral GGO- and peripheral-predominant lesions; and (5) bilateral GGO- and predominant peripheral lesions without nodules, airway abnormalities, pleural effusion, and me
Luo et al[22] developed an imaging score to distinguish COVID-19 pneumonia and non-COVID-19 pneumonia (Influenza pneumonia, Pneumocystis carinii pneumonia, Mycoplasma pneumonia, and CAP). Seven positive signs were identified: posterior part/lower lobe predilection, bilateral involvement, rounded GGO, subpleural band
Similarly, other authors found that pure/mixed GGOs, interlobular septal thi
Although GGOs and consolidations were present in both other viral pneumonia (adenovirus, influenza, parainfluenza, rhinovirus, and others) and COVID-19, central plus peripherical distribution, air bronchogram, pleural thickening, pleural effusion, and lymphadenopathy were more frequent in viral pneumonia[21].
Two studies investigated the differential radiological manifestations of COVID-19 lung disease and CAP. By using a new radiological model, Li et al[24] observed that CAP was characterized more often by nodular or consolidation shadows with or without patchy GGOs and more rarely by subtle mesh changes, dilatated small ve
Consolidation, nodules, pleural effusion, and tree-in-bud signs were the radiological manifestation in influenza pneumonia in the analysis by Liu et al[23] and Zhao et al[33]. The distribution of the lesions (bilateral lobe vs inferior lobe), their margin (clear vs vague), and the GGO lesion involvement pattern (patchy or GGO associated with consolidation vs cluster-like involvement) distinguished COVID-19 from influenza pneumonia, according to Wang et al[30].
The current review focuses on the differential diagnosis between COVID-19 disease and other respiratory and non-respiratory disorders.
Since the early phase of the pandemic, radiological imaging has been employed to assess the suspicion of COVID-19 pneumonia in patients selected by clinical triage, demonstrating the potential for a standardized assessment of the degree of pulmonary involvement and prognostication purposes. Moreover, it has been used as a tool capable of complementing the limited sensitivity and time-consuming laboratory testing process for the SARS-CoV-2 infection detection[34-37].
Such a practical approach has found application in an unprecedented pandemic scenario, where the prevalence of the disease was extraordinarily high, with the awareness that the imaging findings of COVID-19 pneumonia were non-specific as reflecting the diffuse alveolar damage and organizing pneumonia with features shared by a broad spectrum of disorders[38,39]. Despite the increasing knowledge about radiological imaging’s role in the pandemic, the actual diagnostic performance of di
Similarly, other studies included in the present analyses should be interpreted with caution due to limitations such as selection bias or the relatively limited number of patients. Given this awareness, it is noticeable how some CT imaging findings, namely mucoid impactions, centrilobular nodules, lobar consolidation, and significant pleural effusion, have been consistently found to be less frequent in COVID-19 than in other types of pneumonia (Figures 2-4). Thus, they are potentially helpful in everyday pra
Imaging findings typical of interstitial pneumonia may be found in asymptomatic COVID-19 patients[46]. Interestingly, incidental GGO showing accumulation of flu
When dealing with cancer patients, COVID-19 needs to be considered among di
Besides cancer progression, COVID-19 pneumonia has been investigated as a mimi
Radiotherapy and oncologic treatment, such as target therapy and immunotherapy, may induce lung toxicity, mimicking COVID-19 illness. Zeng et al[28] recruited suspected COVID-19 patients diagnosed with cancer and treated with radiation to explore the differential diagnosis between COVID-19 pneumonia and radiation pneu
In addition to immune checkpoint inhibitors, other anticancer drugs such as tyro
Although lymphopenia and a high level of D-dimer and C-reactive protein are often identified in COVID-19 patients, these laboratory findings are not unique and are inadequate to address the proper diagnosis, especially in cancer patients.
Our systematic review has several limitations, including the mostly retrospective nature and the heterogeneity of the included studies.
The patient’s global view of epidemiological, clinical, radiological, and laboratory elements could help the physician overcome the diagnostic difficulties in the COVID-19 era.
Several radiological features are shared by coronavirus disease 19 (COVID-19) pneu
The differential diagnosis of COVID-19 pneumonia is a radiological challenge.
To identify crucial radiological features of COVID-19 pneumonia reported by the literature and their differential diagnosis.
We performed a systematic review with a descriptive aim.
Ground-glass opacity and consolidations are the most common computed tomography lesions in COVID-19 pneumonia and other respiratory diseases. Of the identified 133 studies, 18 were eligible and included in this review. Single lesion associated with pleural effusion and lymphadenopathies distinguishes COVID-19 pneumonia from early lung cancer. Only two studies included cancer patients, and the differential diagnosis with early lung cancer and radiation pneumonitis was performed. The onset of the lesions in the radiation fields only allows the differential diagnosis between COVID-19 pneumonia and radiation pneumonitis.
Computed tomography scan is essential for the differential diagnosis of drug-induced pneumonitis, infectious pneumonia, and other conditions such as cancer progression.
The focus on patients with cancer evidenced a wide lack of data in this field, sugges
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fei C, Patel L S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395:1321-1322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 429] [Cited by in F6Publishing: 434] [Article Influence: 108.5] [Reference Citation Analysis (0)] |
| 2. | World Health Organization. Rolling updates on coronavirus disease (COVID-19): WHO characterizes COVID-19 as a pandemic. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. [Cited in This Article: ] |
| 3. | Sebhatu A, Wennberg K, Arora-Jonsson S, Lindberg SI. Explaining the homogeneous diffusion of COVID-19 nonpharmaceutical interventions across heterogeneous countries. Proc Natl Acad Sci USA. 2020;117:21201-21208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 4. | Looi MK. Covid-19: Is a second wave hitting Europe? BMJ. 2020;371:m4113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 5. | Ragnoli B, Malerba M. Focus on the Potential Role of Lung Ultrasound in COVID-19 Pandemic: What More to Do? Int J Environ Res Public Health. 2020;17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295:202-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1827] [Cited by in F6Publishing: 1641] [Article Influence: 410.3] [Reference Citation Analysis (0)] |
| 7. | Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging. 2020;35:219-227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 400] [Cited by in F6Publishing: 545] [Article Influence: 136.3] [Reference Citation Analysis (0)] |
| 8. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295:715-721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1617] [Cited by in F6Publishing: 1665] [Article Influence: 416.3] [Reference Citation Analysis (0)] |
| 9. | Han X, Fan Y, Alwalid O, Li N, Jia X, Yuan M, Li Y, Cao Y, Gu J, Wu H, Shi H. Six-month Follow-up Chest CT Findings after Severe COVID-19 Pneumonia. Radiology. 2021;299:E177-E186. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 374] [Cited by in F6Publishing: 336] [Article Influence: 112.0] [Reference Citation Analysis (0)] |
| 10. | Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, Jacobi A, Chung M, Bernheim A, Eber C, Concepcion J, Fayad ZA, Gupta YS. Clinical and Chest Radiography Features Determine Patient Outcomes in Young and Middle-aged Adults with COVID-19. Radiology. 2020;297:E197-E206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 183] [Cited by in F6Publishing: 213] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 11. | Peng QY, Wang XT, Zhang LN; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020;46:849-850. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 469] [Cited by in F6Publishing: 487] [Article Influence: 121.8] [Reference Citation Analysis (1)] |
| 12. | Poggiali E, Dacrema A, Bastoni D, Tinelli V, Demichele E, Mateo Ramos P, Marcianò T, Silva M, Vercelli A, Magnacavallo A. Can Lung US Help Critical Care Clinicians in the Early Diagnosis of Novel Coronavirus (COVID-19) Pneumonia? Radiology. 2020;295:E6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 221] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 13. | Colombi D, Petrini M, Maffi G, Villani GD, Bodini FC, Morelli N, Milanese G, Silva M, Sverzellati N, Michieletti E. Comparison of admission chest computed tomography and lung ultrasound performance for diagnosis of COVID-19 pneumonia in populations with different disease prevalence. Eur J Radiol. 2020;133:109344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 14. | Goyal N, Chung M, Bernheim A, Keir G, Mei X, Huang M, Li S, Kanne JP. Computed Tomography Features of Coronavirus Disease 2019 (COVID-19): A Review for Radiologists. J Thorac Imaging. 2020;35:211-218. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Kristjansson M, Bieluch VM, Byeff PD. Mycobacterium haemophilum infection in immunocompromised patients: case report and review of the literature. Rev Infect Dis. 1991;13:906-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47017] [Cited by in F6Publishing: 43210] [Article Influence: 2880.7] [Reference Citation Analysis (0)] |
| 16. | Dai WC, Zhang HW, Yu J, Xu HJ, Chen H, Luo SP, Zhang H, Liang LH, Wu XL, Lei Y, Lin F. CT Imaging and Differential Diagnosis of COVID-19. Can Assoc Radiol J. 2020;71:195-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 170] [Cited by in F6Publishing: 172] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 17. | Orlandi M, Lepri G, Bruni C, Wang Y, Bartoloni A, Zammarchi L, Cometi L, Guiducci S, Matucci-Cerinic M, Bellando-Randone S. The systemic sclerosis patient in the COVID-19 era: the challenging crossroad between immunosuppression, differential diagnosis and long-term psychological distress. Clin Rheumatol. 2020;39:2043-2047. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Shenavandeh S, Sefidbakht S, Iranpour P, Teimouri A, Hooshmandi S, Hooshmandi E, Athari M. COVID-19 and granulomatosis with polyangiitis (GPA): a diagnostic challenge. Rheumatology (Oxford). 2020;59:2170-2171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Mazouz S, Aissaoui O, Fehdi MA, Nsiri A, AlHarrar R. COVID-19 suspicion revealed to be fat embolism syndrome. Pan Afr Med J. 2020;36:104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 20. | Chen LR, Chen ZX, Liu YC, Peng L, Zhang Y, Xu Q, Lin Q, Tao YM, Wu H, Yin S, Hu YJ. Pulmonary contusion mimicking COVID-19: A case report. World J Clin Cases. 2020;8:1554-1560. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi LB, Wang DC, Mei J, Jiang XL, Zeng QH, Egglin TK, Hu PF, Agarwal S, Xie FF, Li S, Healey T, Atalay MK, Liao WH. Performance of Radiologists in Differentiating COVID-19 from Non-COVID-19 Viral Pneumonia at Chest CT. Radiology. 2020;296:E46-E54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 726] [Cited by in F6Publishing: 695] [Article Influence: 173.8] [Reference Citation Analysis (0)] |
| 22. | Luo L, Luo Z, Jia Y, Zhou C, He J, Lyu J, Shen X. CT differential diagnosis of COVID-19 and non-COVID-19 in symptomatic suspects: a practical scoring method. BMC Pulm Med. 2020;20:129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 23. | Liu M, Zeng W, Wen Y, Zheng Y, Lv F, Xiao K. COVID-19 pneumonia: CT findings of 122 patients and differentiation from influenza pneumonia. Eur Radiol. 2020;30:5463-5469. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 24. | Li Z, Zeng B, Lei P, Liu J, Fan B, Shen Q, Pang P, Xu R. Differentiating pneumonia with and without COVID-19 using chest CT images: from qualitative to quantitative. J Xray Sci Technol. 2020;28:583-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Liu KC, Xu P, Lv WF, Chen L, Qiu XH, Yao JL, Gu JF, Hu B, Wei W. Differential diagnosis of coronavirus disease 2019 from community-acquired-pneumonia by computed tomography scan and follow-up. Infect Dis Poverty. 2020;9:118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Xie S, Lei Z, Chen X, Liu W, Wang X, Dong Y, Guo Y, Duan Y, Cao H, Qin J, Lin B. Chest CT-based differential diagnosis of 28 patients with suspected corona virus disease 2019 (COVID-19). Br J Radiol. 2020;93:20200243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Himoto Y, Sakata A, Kirita M, Hiroi T, Kobayashi KI, Kubo K, Kim H, Nishimoto A, Maeda C, Kawamura A, Komiya N, Umeoka S. Diagnostic performance of chest CT to differentiate COVID-19 pneumonia in non-high-epidemic area in Japan. Jpn J Radiol. 2020;38:400-406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 28. | Zeng Q, Tang C, Deng L, Li S, Liu J, Wang S, Shan H. Differential Diagnosis of COVID-19 Pneumonia in Cancer Patients Received Radiotherapy. Int J Med Sci. 2020;17:2561-2569. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Zhang YJ, Yang WJ, Liu D, Cao YQ, Zheng YY, Han YC, Jin RS, Han Y, Wang XY, Pan AS, Dai JY, Sun QF, Zhao FQ, Yang QY, Zhang JH, Liu SJ, Da Q, Guo W, Li CQ, Zhang WT, Wu H, Chen XS, Ji AQ, Xiang J, Chen K, Feng XJ, Zhang XF, Cao QQ, Qin L, Li J, Zhou M, Lu Y, Wang CF, Yan FH, Li HC, Qu JM. COVID-19 and early-stage lung cancer both featuring ground-glass opacities: a propensity score-matched study. Transl Lung Cancer Res. 2020;9:1516-1527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Wang H, Wei R, Rao G, Zhu J, Song B. Characteristic CT findings distinguishing 2019 novel coronavirus disease (COVID-19) from influenza pneumonia. Eur Radiol. 2020;30:4910-4917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 31. | Zhou J, Liao X, Cao J, Ling G, Ding X, Long Q. Differential diagnosis between the coronavirus disease 2019 and Streptococcus pneumoniae pneumonia by thin-slice CT features. Clin Imaging. 2021;69:318-323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Chi Q, Dai X, Jiang X, Zhu L, Du J, Chen Y, Zheng J, Huang J. Differential diagnosis for suspected cases of coronavirus disease 2019: a retrospective study. BMC Infect Dis. 2020;20:679. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Zhao W, Xie X, Liu J. The importance of distinguishing COVID-19 from more common respiratory illnesses. Epidemiol Infect. 2020;148:e195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Sverzellati N, Milanese G, Milone F, Balbi M, Ledda RE, Silva M. Integrated Radiologic Algorithm for COVID-19 Pandemic. J Thorac Imaging. 2020;35:228-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 35. | Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, Schluger NW, Volpi A, Yim JJ, Martin IBK, Anderson DJ, Kong C, Altes T, Bush A, Desai SR, Goldin O, Goo JM, Humbert M, Inoue Y, Kauczor HU, Luo F, Mazzone PJ, Prokop M, Remy-Jardin M, Richeldi L, Schaefer-Prokop CM, Tomiyama N, Wells AU, Leung AN. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020;296:172-180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 610] [Cited by in F6Publishing: 563] [Article Influence: 140.8] [Reference Citation Analysis (0)] |
| 36. | Prokop M, van Everdingen W, van Rees Vellinga T, Quarles van Ufford H, Stöger L, Beenen L, Geurts B, Gietema H, Krdzalic J, Schaefer-Prokop C, van Ginneken B, Brink M; COVID-19 Standardized Reporting Working Group of the Dutch Radiological Society. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020;296:E97-E104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 457] [Cited by in F6Publishing: 536] [Article Influence: 134.0] [Reference Citation Analysis (0)] |
| 37. | Feng Z, Yu Q, Yao S, Luo L, Zhou W, Mao X, Li J, Duan J, Yan Z, Yang M, Tan H, Ma M, Li T, Yi D, Mi Z, Zhao H, Jiang Y, He Z, Li H, Nie W, Liu Y, Zhao J, Luo M, Liu X, Rong P, Wang W. Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nat Commun. 2020;11:4968. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 138] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 38. | Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary Pathology of Early-Phase 2019 Novel Coronavirus (COVID-19) Pneumonia in Two Patients With Lung Cancer. J Thorac Oncol. 2020;15:700-704. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 927] [Cited by in F6Publishing: 969] [Article Influence: 242.3] [Reference Citation Analysis (0)] |
| 39. | Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, Zerbi P, Rech R, Colombo R, Antinori S, Corbellino M, Galli M, Catena E, Tosoni A, Gianatti A, Nebuloni M. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis. 2020;20:1135-1140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 730] [Cited by in F6Publishing: 885] [Article Influence: 221.3] [Reference Citation Analysis (0)] |
| 40. | Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2352-2371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1269] [Cited by in F6Publishing: 1283] [Article Influence: 320.8] [Reference Citation Analysis (0)] |
| 41. | Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296:E115-E117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2088] [Cited by in F6Publishing: 1808] [Article Influence: 452.0] [Reference Citation Analysis (2)] |
| 42. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3542] [Cited by in F6Publishing: 3187] [Article Influence: 796.8] [Reference Citation Analysis (0)] |
| 43. | Raptis CA, Hammer MM, Short RG, Shah A, Bhalla S, Bierhals AJ, Filev PD, Hope MD, Jeudy J, Kligerman SJ, Henry TS. Chest CT and Coronavirus Disease (COVID-19): A Critical Review of the Literature to Date. AJR Am J Roentgenol. 2020;215:839-842. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 135] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 44. | Revel MP, Parkar AP, Prosch H, Silva M, Sverzellati N, Gleeson F, Brady A; European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI). COVID-19 patients and the radiology department - advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI). Eur Radiol. 2020;30:4903-4909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 212] [Cited by in F6Publishing: 244] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 45. | Silva M, Ledda RE, Schiebler M, Balbi M, Sironi S, Milone F, Affanni P, Milanese G, Sverzellati N. Frequency and characterization of ancillary chest CT findings in COVID-19 pneumonia. Br J Radiol. 2021;94:20200716. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Varble N, Blain M, Kassin M, Xu S, Turkbey EB, Amalou A, Long D, Harmon S, Sanford T, Yang D, Xu Z, Xu D, Flores M, An P, Carrafiello G, Obinata H, Mori H, Tamura K, Malayeri AA, Holland SM, Palmore T, Sun K, Turkbey B, Wood BJ. CT and clinical assessment in asymptomatic and pre-symptomatic patients with early SARS-CoV-2 in outbreak settings. Eur Radiol. 2021;31:3165-3176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 47. | Polverari G, Arena V, Ceci F, Pelosi E, Ianniello A, Poli E, Sandri A, Penna D. 18F-Fluorodeoxyglucose Uptake in Patient With Asymptomatic Severe Acute Respiratory Syndrome Coronavirus 2 (Coronavirus Disease 2019) Referred to Positron Emission Tomography/Computed Tomography for NSCLC Restaging. J Thorac Oncol. 2020;15:1078-1080. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 48. | Zou S, Zhu X. FDG PET/CT of COVID-19. Radiology. 2020;296:E118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 78] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 49. | Liu C, Zhou J, Xia L, Cheng X, Lu D. 18F-FDG PET/CT and Serial Chest CT Findings in a COVID-19 Patient With Dynamic Clinical Characteristics in Different Period. Clin Nucl Med. 2020;45:495-496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 50. | Boettcher AN, Hammoud DA, Weinberg JB, Agarwal P, Mendiratta-Lala M, Luker GD. Cancer Imaging and Patient Care during the COVID-19 Pandemic. Radiol Imaging Cancer. 2020;2:e200058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 51. | Nishino M, Hatabu H, Hodi FS. Imaging of Cancer Immunotherapy: Current Approaches and Future Directions. Radiology. 2019;290:9-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 52. | Kalisz KR, Ramaiya NH, Laukamp KR, Gupta A. Immune Checkpoint Inhibitor Therapy-related Pneumonitis: Patterns and Management. Radiographics. 2019;39:1923-1937. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 53. | Nishino M, Giobbie-Hurder A, Hatabu H, Ramaiya NH, Hodi FS. Incidence of Programmed Cell Death 1 Inhibitor-Related Pneumonitis in Patients With Advanced Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2016;2:1607-1616. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 406] [Cited by in F6Publishing: 487] [Article Influence: 69.6] [Reference Citation Analysis (0)] |
| 54. | Naidoo J, Wang X, Woo KM, Iyriboz T, Halpenny D, Cunningham J, Chaft JE, Segal NH, Callahan MK, Lesokhin AM, Rosenberg J, Voss MH, Rudin CM, Rizvi H, Hou X, Rodriguez K, Albano M, Gordon RA, Leduc C, Rekhtman N, Harris B, Menzies AM, Guminski AD, Carlino MS, Kong BY, Wolchok JD, Postow MA, Long GV, Hellmann MD. Pneumonitis in Patients Treated With Anti-Programmed Death-1/Programmed Death Ligand 1 Therapy. J Clin Oncol. 2017;35:709-717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 605] [Cited by in F6Publishing: 712] [Article Influence: 89.0] [Reference Citation Analysis (1)] |
| 55. | Naidoo J, Reuss JE, Suresh K, Feller-Kopman D, Forde PM, Mehta Steinke S, Rock C, Johnson DB, Nishino M, Brahmer JR. Immune-related (IR)-pneumonitis during the COVID-19 pandemic: multidisciplinary recommendations for diagnosis and management. J Immunother Cancer. 2020;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 56. | Sakai F, Johkoh T, Kusumoto M, Arakawa H, Takahashi M. Drug-induced interstitial lung disease in molecular targeted therapies: high-resolution CT findings. Int J Clin Oncol. 2012;17:542-550. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 57. | Azer SA. COVID-19: pathophysiology, diagnosis, complications and investigational therapeutics. New Microbes New Infect. 2020;37:100738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |