Published online Jan 16, 2023. doi: 10.4253/wjge.v15.i1.1
Peer-review started: October 3, 2022
First decision: November 2, 2022
Revised: November 7, 2022
Accepted: December 21, 2022
Article in press: December 21, 2022
Published online: January 16, 2023
Gastric cancer (GC) represents the fourth leading cause of cancer death worl
Core Tip: Since its initial introduction in clinical practice endoscopic ultrasound has been considered a valuable tool for tumor and lymph nodes staging of gastric cancer, in order to establish the best therapeutic strategy for the patient. Moreover, in this new era of endoscopic mucosal resection or submucosal dissection and minimally invasive surgery, endoscopic ultrasound is increasingly important for early gastric cancer staging and therapeutic decision making and it can also have a role in the advanced phases of the disease, in facilitating palliative, minimally-invasive treatments.
- Citation: Rossi G, Petrone MC, Healey AJ, Arcidiacono PG. Gastric cancer in 2022: Is there still a role for endoscopic ultrasound? World J Gastrointest Endosc 2023; 15(1): 1-9
- URL: https://www.wjgnet.com/1948-5190/full/v15/i1/1.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i1.1
Gastric cancer (GC) represents the fourth leading cause of cancer death worldwide with a median survival less than 12 mo in advanced disease[1], and a global incidence that has decreased in the last few decades due to lifestyle improvement.
The incidence of GC is greater in men and certain geographic areas and many factors can influence its development, both environmental and genetic[2]. Risk factors for the development of GC are numerous. A significant impact on GC incidence is patient dietary habits (certain foods, alcohol consumption), smoking history, family history and Helicobacter pylori or Epstein-Barr virus infections[3].
Outcomes are favorable if cancer precursors are detected early and a high quality endoscopy represents the modality of choice for diagnosis in this phase. Moreover, GC morphologic classification at endoscopy is fundamental for oncologic diagnosis, staging and therapeutic decision making[4]. Furthermore, accurate clinical classification is important in determining cancer prognosis.
There are several options for GC treatment, however an accurate preoperative diagnosis is important to select the appropriate therapeutic decision. Endoscopic resection represents an option in early phases of disease and at the other end of the disease spectrum, neoadjuvant treatment indications have been expanded in locally-advanced cancers.
Several Classifications distinguish the tumor extension, histologic features or morphologic appearance at endoscopy.
The American Joint Committee on Cancer and the Union for International Cancer Control published their last edition of cancer staging systems in 2017 with Tumor Node Metastasis (TNM) system, employed for GC clinical and pathologic staging. TNM system represents cancer extension: T is tumor depth in the gastric wall, N the number of regional lymph nodes involved and M the presence of distant metastasis[5,6], as represented in Table 1.
| TNM staging | |
| T | |
| TX | Primary tumour cannot be assessed |
| T0 | No evidence of primary tumour |
| Tis | Carcinoma in situ |
| T1a | Tumour invades lamina propria or muscularis mucosae |
| T1b | Tumour invades submucosa |
| T2 | Tumour invades muscularis propria |
| T3 | Tumour penetrates subserosal tissue without invasion of visceral peritoneum or adjacent structures |
| T4a | Tumour penetrates serosa (visceral peritoneum) |
| T4b | Tumour directly invades adjacent organs or structures |
| N | |
| NX | Regional lymph nodes(s) cannot be assessed |
| N0 | No regional lymph node metastases |
According to TNM staging an early GC (EGC) is defined as a lesion limited to the gastric mucosa or submucosa (T1 at TNM staging) irrespective of lymph nodes spread. An advanced cancer is a lesion invading the muscolaris propria of the gastric wall or a cancer going beyond it[7]. The scope to resect with a minimally-invasive endoscopic resection in EGCs has increased and the specific evaluation of all the gastric layers with a highly-sensitive method such as endoscopic ultrasound (EUS) is central to deciding the best resection approach following the cancer extension (T).
In the new classification, if the tumor with its epicenter is located >2 cm from esophagogastric junction (EGJ) or it is located within 2 cm from EGJ but not involving the junction itself, this is considered as a gastric tumor. By proxy, the tumor with its epicenter located within 2 cm of EGJ involving the junction itself, this is considered as an esophageal tumor[8].
High-definition video-endoscopes have facilitated the detection and diagnosis of GC and enable the treatment of early phase EGCs with a minimal-invasive endoscopic resection in selected patients. The importance of endoscopic manoeuvres during the diagnostic tumor process is relevant, as washing off by water injection through the endoscopic channel the adherent mucus on gastric mucosa, aspirating gastric secretions present in the cavity and controlling the amount of the air insufflated. EGC diagnosis is mainly based on the two important endoscopic findings: A well-demarcated lesion and an irregularity in the surface in terms of color or gland pattern[9].
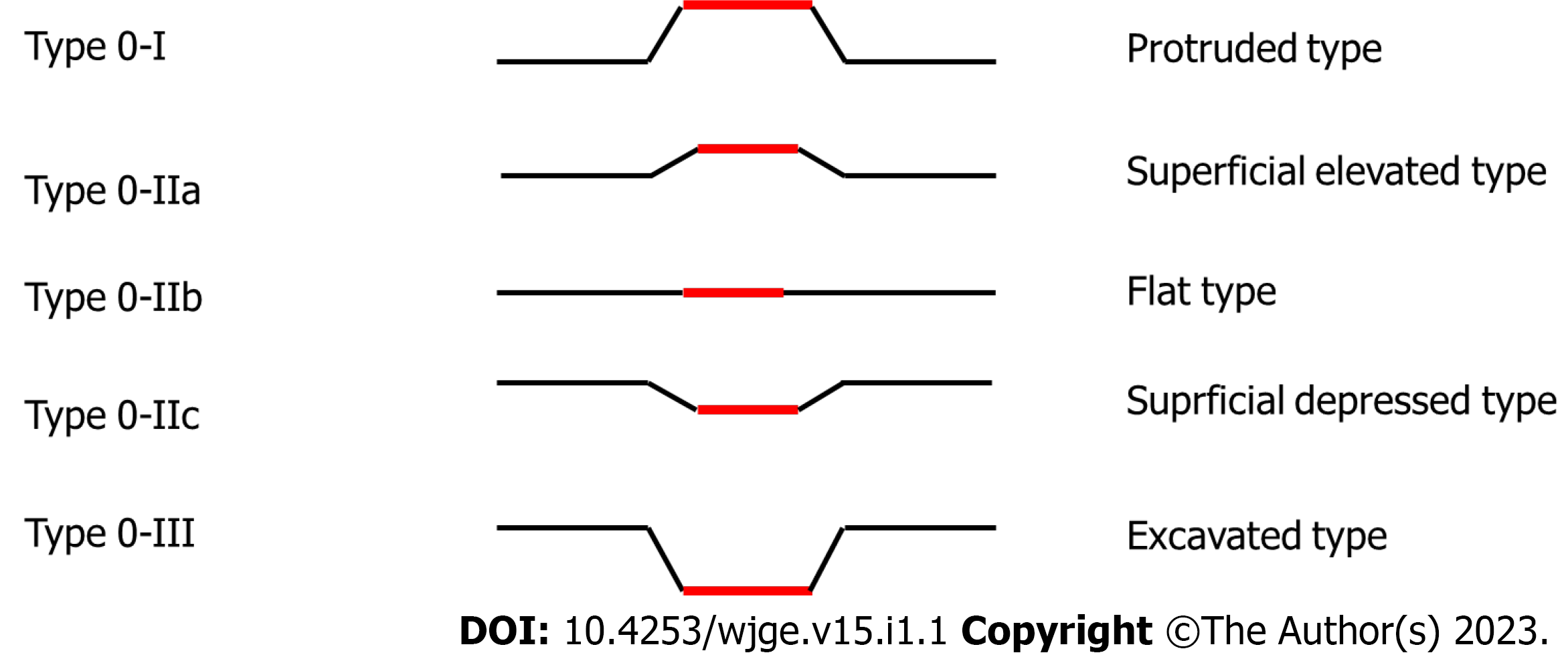
The morphologic growth pattern of GC is defined by Borrmann classification, which classified the tumor as polypoid (lesion type I), fungating (lesion type II), ulcerated (lesion type III) or infiltrative (lesion type IV)/invasive cancer. Furthermore, early lesions are also macroscopically classified as lesions type 0 as an extension of Borrmann classification and EGCs are further classified according to morphologic extension as protruded (type 0 and type I), slightly elevated (called type 0-IIa), flat (type 0-IIb), slightly depressed (type 0-IIc) and excavated (type 0-III), with mixture types also possible.
Concerning superficial cancers, in 2003 the Paris classification (Figure 1) for macroscopic gastrointestinal superficial lesions was introduced. This classification distinguished the differences between type 0-I and type 0-IIa lesions according to a tumor height of 2.5 mm[10], and it distinguished the submucosal (SM)1 and SM2 tumors on the basis of the depth of submucosal invasion > 500 μm[11].
Histological GC diagnosis is based on the endoscopic biopsies with forceps, however global endoscopic evaluation is fundamental in this phase of diagnosis. Parameters as shapes, colors and ulcerations reflect tumor invasiveness and are useful also during the next step in oncological man
Several histological classifications have been employed and the older Lauren histologic classification has been traditionally used in Western world[12]. This classification distinguishes the “intestinal type” characterized by glandular structures (intestinal metaplasia) comprising well differentiated columnar epithelial cells from the “diffuse type” characterized by pangastric infiltration by poorly cohesive clusters or solitary mucin-rich cells (called “signet ring cells”). Transmural extension through lymphatic invasion can produce a gastric wall thickening without causing a mass effect (so called “plastic linitis”). The intestinal-type GC can involve more often the distal part of the stomach and itis closely related to an environmental (Helicobacter pylori) and a specific-diet exposure. The diffuse-type GC interests people at a younger age and it carries a poorer prognosis.
The World Health Organization fifth tumors classification issued in 2019 is probably the most detailed classification system, describing apart from stomach adenocarcinomas, also other types of gastric tumors with decreased incidence[13,14]. The present classification has distinguished every single histologic type of GC (recently including also micropapillary carcinoma, gastric adenocarcinoma of the fundic gland type and undifferentiated carcinoma). Concerning gastric adenocarcinoma the common histologic subtypes described (as well as in fourth edition) are: The tubular, papillary, poorly cohesive, mucinous and mixed-type adenocarcinoma. Of these, tubular and papillary adenocarcinoma are graded as follows: low grade (well or moderately differentiated) and high grade (poorly differentiated). As new information, a molecular classification was introduced also in GC investigating: The Epstein–Barr virus-positive type, the microsatellite instability presence (the genomically stable type and chromosomally unstable type) and a large part of this classification were dedicated to precancerous lesions illustration (gastric dysplasia and adenomas).
EUS is a well-established procedure that was introduced almost 40 years ago in clinical practice, combining the endoscopic view with the ultrasound evaluation of target anatomic structures[15]. With the introduction in in the early 1990s of the linear echoendoscopes, EUS gained the ability to safely guide in “real time” a targeted biopsy of tissue with EUS-guided fine needle aspiration (FNA)[16]. During the last years EUS has become also an increasingly therapeutic modality including applications in the treatment of the advanced phases of neoplastic diseases.
Many improvements in echoendoscopes and processor technology have been made during the last decade, as well as many ultrasound tools and endoscopic devices have become integral in GC patient management.
EUS equipment consist of an ultrasound processor connected to an echoendoscope, with an ultrasound transducer attached at the distal tip of the instrument. The endoscope in return is connected to a standard video processor, permitting the endoscopic visualization: The complete system allows for simultaneous endoscopic and ultrasound imaging. Echoendoscopes work at variable frequencies, the most common ranging between 5 and 12 MHz: Higher frequencies allow a better resolution, but limit ultrasound beam penetration.
There are two types of echoendoscopes, radial and linear[17]. Radial transducers are used only for diagnostic purposes and they have individual piezoelectric elements of transducer around the distal tip in a 360° radial-array, producing an ultrasound image in a plane perpendicular to the long axis of the echoendoscope. Linear EUS scopes allow the real-time tissue sampling of targeted lesions and they can produce an ultrasound image in a parallel plane to the long axis of the scope (usually with a sector width between 100° and 180°). Different centers’ expertise drive the choice in using either radial or linear EUS scopes, but the use of a linear scope permits synchronous staging and tissue/Lymph node sampling.
Different brands of ultrasound processors are available on the market, all with incorporated add
Ultrasound elastography reports a measurement of tissue stiffness, evaluating EUS changes on the image before and after the application of a determined pressure exerted by the probe. This is based on the hypothesis that a not-pathological tissue is soft, and it deforms more than a malignant tissue which results more stiff. In GC the elastography plays a key role in lymph nodes characterization, differentiating benign vs malignant ones with different techniques: The qualitative or the semi-quantitative elastography[18]. Qualitative elastography differentiates the lesions according to their elasticity score on a color map but it can represent a subjective evaluation, extremely operator-dependent. “Strain ratio” and “strain histogram” elastography represent semi-quantitative and more objective techniques, resulting in a numerical ratio of “regions of interest or “ROI” (lesion ROI/normal tissue ROI) or through the strain histogram permitting a graphical representation (histogram) of pixels color distribution of lesion/lymph node stiffness.
In earlier phases Color Doppler ultrasound improved the ability to differentiate malignant lymph nodes by displaying macro-vessels architecture. Inflammatory lymph nodes are more vascularized, without changes in the hilar vessel architecture. Metastatic lymph nodes present peripheral or mixed vascularity and lose the hilar vascularization[19]. Color Doppler ultrasound can also guide the needle trajectory during biopsies avoiding bigger vessels and preventing bleedings. CE-EUS imaging is also a useful tool for malignant lymph nodes diagnosis. It works with the direct intravenous administration of a new second generation contrast (sulphur hexafluoride) followed by 10-20 mL of saline generating microbubbles in the vessels with a diameter of 0.1-0.4 mm.
An advantage of EUS in GC is to biopsy mainly suspected malignant lymph nodes in order to improve N staging in high-selected cases. Usually, the ultrasound evaluation is enough to establish the malignant nature of suspected enlarged lymph nodes, but EUS-FNA represents a valid tool in selected and discussed cases (by a multidisciplinary team) if biopsy can change the therapeutic management of the patient. In case of EUS-biopsy different needles are disposable on the market, with different tips morphologies, stylet materials and flexibility of the body. The choice of the correct needle is usually related to a preference of the ultrasonographer, the availability of rapid on-site evaluation in the reference hospital and the target tissue to sample. Two big types of needles are available, for cytology and histology, respectively FNA and fine needle biopsy (FNB). FNB needles are fundamental in case of subsequent molecular studies as in case of metastatic lymph-nodes. Needles sizes used in lymph nodes sampling are 19, 20, 22, 25 Gauge (G). The European Society of Gastrointestinal Endoscopy Guidelines recommend the use of 25 G or 22 G needle in case of solid masses or lymph nodes sampling, with an equally recommendation between FNA and FNB needles[20]. However, when a tissue core is the primary aim the society suggests the employment of larger needles calibers as 19 G FNA or FNB needles or 22 G FNB needles.
The traditional use of EUS use is during the diagnostic process of GC staging, in particular to detect tumor extension in the gastric wall (T) and the presence of pathologic lymph nodes (N) in the evaluable stations. Early stages of GC can be treated by endoscopic submucosal dissection (ESD), endoscopic mucosal resection (EMR) or laparoscopic surgery, whereas the intermediate stages need a neoadjuvant chemotherapy to improve long term prognosis results after the subsequent surgery[21]. Therefore, the evaluation of tumor depth invasion and the presence of malignant lymph nodes are the cornerstones of therapeutic management and decisions and EUS can be useful in this process.
EUS can have a role also to assess the presence of a metastatic disease during the ultrasound evaluation, for example visualizing hepatic secondary lesions in the visible liver segments (I, II, III, IV) during EUS examination. Hepatic hilum lesions or lymph nodes can also be visualized and sampled being as standard of care also in biliary and pancreatic diseases.
EUS distinguishes the distinct wall layers of gastrointestinal tract: superficial mucosa or lumen interface (M), muscularis mucosal layer or deep mucosa, submucosal layer, muscularis propria and finally serosa. Thus, EUS is useful to establish tumor depth penetration and following T state according to TNM classification. Tumor extension in gastric wall is fundamental to establish the correct lesion treatment.
EUS is a reliable modality for determining indications of less-invasive endoscopic resection for early GC[22,23]. Two resection technics are used to endoscopically remove EGCs: EMR and ESD. Compared to EMR the ESD technique is associated with higher “en-bloc” resection rates, higher R0 resections and a lower cancer recurrences but it is also associated with longer procedures in terms of time and higher perforation risks[24,25]. ESD is performed for these reasons in expert hands and high-volume centers, with the availability of a multidisciplinary team of specialists.
Moreover, the choice of endoscopic resection method depends on tumor size (ESD should be selected in case of tumor size greater than one centimeter) and different factors can influence the risk of malignant lymph node presence[26-29]. Different scenarios can be noticed in case of endoscopic curative resection: (1) Endoscopic resection is mostly curative in case of a poorly differentiated or diffuse cancer subtype confined to the mucosal layer, non-ulcerated and with a size ≤ 2 cm, but gastrectomy must be discussed within a multidisciplinary team; (2) In case of a well-differentiated cancer the endoscopic resection is considered as curative for lesions T1 SM1 (with the depth of invasion of the submucosal layer < 500 μm), possibly ulcerated and less than 3 cm in size; and (3) Well-differentiated cancers, not ulcerated and confined to the mucosal layer can be resected by ESD irrespective of size.
Accuracy of EUS in evaluating ECG invasion depth was described by various study, with a high grade of variability and an accuracy rate between 64.8% and 92%[30-35].
In 2019 a meta-analysis of 17 articles and 4525 lesions showed a moderate value for depth invasion evaluation in EGC with a sensitivity of 87% and specificity of 67%. Overall over-staging rate of mucosa (M) or SM1 and SM2 by EUS was 13.31% and 32.8% respectively, while the overall under-staging rate of SM2 was 29.7%[36]. Meta-analysis concluded that EUS has demonstrated a moderate diagnostic value for depth of invasion assessment in EGC remarking the attention by the endoscopists to the endoscopic factors affecting EUS accuracy in EGC: invasion depth, like the shape, size and differentiation of lesions. In this way the endoscopic evaluation before EUS staging is crucial to define tumor malignancy.
Finally, the endoscopic resection (particularly ESD) should be done by expert endoscopists, and the expertise of the endosonographer is fundamental to establish the extension of the tumor in gastric wall with the best sensitive way. Radial EUS-scope is widely used, however linear EUS-scope is widely used due to the opportunity to perform biopsies through the operative channel of the instrument. Lan et al[37] described a comparison of EUS accuracy in EGC staging with radial and linear echoendoscopes in balanced groups, concluding that linear EUS is more accurate to establish SM involvement and therapeutic decision in suspected EGCs compared with radial echoendoscopes. More in detail, diagnostic accuracy was much higher for patients who underwent linear EUS compared with radial EUS (90.9% vs 69.2%, P = 0.024). Sensitivity was 92.3% linear EUS and 90.9% for radial EUS. Specificity was 90.0% in linear EUS group, while the specificity was 60.7% in radial group. Univariate analysis showed that the type of echoendoscope was an associated risk factor (OR 0.225) of incorrect T1b staging in EGC patients.
As in case of other cancers in the last decade a significant positive impact of neoadjuvant treatment on locally advanced GC was seen. Although TOTAL STOMACH RESECTION remains the only potentially curative strategy in locally advanced disease the current available evidences suggest that neoadjuvant treatment improves overall survival, disease-free survival reducing the local recurrence rates in GC[38-42].
Neoadjuvant treatment is indicated in lesions extending to or beyond the muscularis propria (T2) and/or in presence of malignant EUS-visible lymph nodes (N+): stages IB–IIIC.
Therefore, the distinction between T1 or T2-T4 and N+ or N- results of paramount importance to decide therapeutic approach and EUS is an excellent method in addition to standard imaging exams in GC staging. Effectively EUS showed a good accuracy (> 90%) in various studies in establish T stage, less accurate in case of N staging, although previous studies have shown excellent accuracy of EUS in N staging[43-47].
Costa et al[48] investigated EUS accuracy in the selection of patients with gastric adenocarcinoma for neoadjuvant therapy (T2 and/or N+). Authors demonstrated an accuracy of 0.86, with a sensitivity and specificity of 88.5% and 83.1%, respectively. Accuracy was more effective in case of proximal and intestinal-type lesions.
During the last decade EUS is rapidly evolving from a diagnostic into a therapeutic procedure, due to the possibility to easily access to adjacent structures with a minimally invasive approach. In particular, the increase and the availability of dedicated devices for therapeutic EUS use has driven this process. Numerous therapeutic procedures can be performed under EUS-guidance, such as drainages (pancreatic fluid collections, biliary system after ERCP failure, gallbladder for acute cholecystitis in high-risk surgical patients) or gastroenteral-anastomosis. This was also facilitated by the introduction of dedicated lumen-apposing metal stents in clinical practice[49,50].
Therapeutic EUS in GC can have a role for biliary drainage in patients with obstructive jaundice and an advanced cancer or a post-resected disease in case of disease relapse. The efficacy of EUS-guided biliary drainage (EUS-BD) was already demonstrated, with a higher technical success rate respect to percutaneous procedure (96.7% vs 88.9%) and fewer adverse events[51].
A late complication of GC could be also the malignant gastric outlet obstruction. Recently ESGE guidelines of therapeutic EUS suggested to perform EUS-guided gastroenterostomy in an expert setting for malignant gastric outlet obstruction, as an alternative to enteral stenting or surgery[49].
Data on long-term efficacy and safety of these relatively new therapeutic EUS-guided procedures will come from randomized multicenter controlled trials in order to create specific flow-chart of treatment.
EUS in 2022 remains an important procedure in the context of GC staging, particularly before ECG endoscopic resection, to evaluate T or confirm N state but it can have a role also in confirmation the locally advanced disease in selected patients. EUS-guided therapeutic procedures are becoming useful to offer a minimally-invasive therapy to patients with advanced disease also in GC but larger datasets are needed in order to standardize clinical indications. Multidisciplinary teams and expertise of clinicians are crucial in the management of this disease.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Imai Y, Japan; Yuan X, China S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Zhang XY, Zhang PY. Gastric cancer: somatic genetics as a guide to therapy. J Med Genet. 2017;54:305-312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 2. | Yusefi AR, Bagheri Lankarani K, Bastani P, Radinmanesh M, Kavosi Z. Risk Factors for Gastric Cancer: A Systematic Review. Asian Pac J Cancer Prev. 2018;19:591-603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 119] [Reference Citation Analysis (0)] |
| 3. | Machlowska J, Baj J, Sitarz M, Maciejewski R, Sitarz R. Gastric Cancer: Epidemiology, Risk Factors, Classification, Genomic Characteristics and Treatment Strategies. Int J Mol Sci. 2020;21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 486] [Cited by in F6Publishing: 544] [Article Influence: 136.0] [Reference Citation Analysis (0)] |
| 4. | El Abiad R, Gerke H. Gastric cancer: endoscopic diagnosis and staging. Surg Oncol Clin N Am. 2012;21:1-19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 5. | Brierley JD, Gospodarowicz MK, Witteking C, eds. TNM Classification of Malignant Tumours. 8th ed. Oxford; Hoboken: John Wiley & Sons; 2017. [Cited in This Article: ] |
| 6. | Amin MB, Edge SB, Greene FL, et al, eds. AJCC Cancer Staging Manual, 8th ed. New York: Springer; 2017. [Cited in This Article: ] |
| 7. | Murakami T. Pathomorphological diagnosis. Definition and gross classification of early gastric cancer. Gann Monogr Cancer Res. 1971;11:53. [Cited in This Article: ] |
| 8. | Kumagai K, Sano T. Revised points and disputed matters in the eighth edition of the TNM staging system for gastric cancer. Jpn J Clin Oncol. 2021;51:1024-1027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Yao K. The endoscopic diagnosis of early gastric cancer. Ann Gastroenterol. 2013;26:11-22. [PubMed] [Cited in This Article: ] |
| 10. | The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58:S3-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1117] [Cited by in F6Publishing: 1197] [Article Influence: 57.0] [Reference Citation Analysis (3)] |
| 11. | Endoscopic Classification Review Group. Update on the paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005;37:570-578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 559] [Cited by in F6Publishing: 567] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 12. | LAUREN P. THE TWO HISTOLOGICAL MAIN TYPES OF GASTRIC CARCINOMA: DIFFUSE AND SO-CALLED INTESTINAL-TYPE CARCINOMA. AN ATTEMPT AT A HISTO-CLINICAL CLASSIFICATION. Acta Pathol Microbiol Scand. 1965;64:31-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4011] [Cited by in F6Publishing: 4105] [Article Influence: 146.6] [Reference Citation Analysis (0)] |
| 13. | Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA; WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1833] [Cited by in F6Publishing: 1673] [Article Influence: 418.3] [Reference Citation Analysis (2)] |
| 14. | Kushima R. The updated WHO classification of digestive system tumours-gastric adenocarcinoma and dysplasia. Pathologe. 2022;43:8-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Hisanaga K, Hisanaga A, Nagata K, Ichie Y. High speed rotating scanner for transgastric sonography. AJR Am J Roentgenol. 1980;135:627-629. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 34] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Vilmann P, Jacobsen GK, Henriksen FW, Hancke S. Endoscopic ultrasonography with guided fine needle aspiration biopsy in pancreatic disease. Gastrointest Endosc. 1992;38:172-173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 405] [Cited by in F6Publishing: 387] [Article Influence: 12.1] [Reference Citation Analysis (1)] |
| 17. | ASGE Technology Committee; Murad FM, Komanduri S, Abu Dayyeh BK, Chauhan SS, Enestvedt BK, Fujii-Lau LL, Konda V, Maple JT, Pannala R, Thosani NC, Banerjee S. Echoendoscopes. Gastrointest Endosc. 2015;82:189-202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Iglesias-Garcia J, Lindkvist B, Lariño-Noia J, Domínguez-Muñoz JE. Endoscopic ultrasound elastography. Endosc Ultrasound. 2012;1:8-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Hocke M, Ignee A, Dietrich C. Role of contrast-enhanced endoscopic ultrasound in lymph nodes. Endosc Ultrasound. 2017;6:4-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Polkowski M, Jenssen C, Kaye P, Carrara S, Deprez P, Gines A, Fernández-Esparrach G, Eisendrath P, Aithal GP, Arcidiacono P, Barthet M, Bastos P, Fornelli A, Napoleon B, Iglesias-Garcia J, Seicean A, Larghi A, Hassan C, van Hooft JE, Dumonceau JM. Technical aspects of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline - March 2017. Endoscopy. 2017;49:989-1006. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 222] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 21. | Mehmedović A, Mesihović R, Saray A, Vanis N. Gastric cancer staging: EUS and CT. Med Arch. 2014;68:34-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Sanomura Y, Oka S, Tanaka S, Noda I, Higashiyama M, Imagawa H, Shishido T, Yoshida S, Hiyama T, Arihiro K, Chayama K. Clinical validity of endoscopic submucosal dissection for submucosal invasive gastric cancer: a single-center study. Gastric Cancer. 2012;15:97-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Oka S, Tanaka S, Higashiyama M, Numata N, Sanomura Y, Yoshida S, Arihiro K, Chayama K. Clinical validity of the expanded criteria for endoscopic resection of undifferentiated-type early gastric cancer based on long-term outcomes. Surg Endosc. 2014;28:639-647. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 24. | Facciorusso A, Antonino M, Di Maso M, Muscatiello N. Endoscopic submucosal dissection vs endoscopic mucosal resection for early gastric cancer: A meta-analysis. World J Gastrointest Endosc. 2014;6:555-563. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 110] [Cited by in F6Publishing: 107] [Article Influence: 10.7] [Reference Citation Analysis (2)] |
| 25. | Pimentel-Nunes P, Mourão F, Veloso N, Afonso LP, Jácome M, Moreira-Dias L, Dinis-Ribeiro M. Long-term follow-up after endoscopic resection of gastric superficial neoplastic lesions in Portugal. Endoscopy. 2014;46:933-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 26. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 817] [Cited by in F6Publishing: 852] [Article Influence: 94.7] [Reference Citation Analysis (0)] |
| 27. | Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1723] [Cited by in F6Publishing: 1840] [Article Influence: 141.5] [Reference Citation Analysis (0)] |
| 28. | Gotoda T, Iwasaki M, Kusano C, Seewald S, Oda I. Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg. 2010;97:868-871. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 193] [Cited by in F6Publishing: 217] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 29. | Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1308] [Cited by in F6Publishing: 1270] [Article Influence: 52.9] [Reference Citation Analysis (0)] |
| 30. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20108] [Cited by in F6Publishing: 19772] [Article Influence: 2196.9] [Reference Citation Analysis (17)] |
| 31. | Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225-229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1134] [Cited by in F6Publishing: 1104] [Article Influence: 48.0] [Reference Citation Analysis (4)] |
| 32. | Akashi K, Yanai H, Nishikawa J, Satake M, Fukagawa Y, Okamoto T, Sakaida I. Ulcerous change decreases the accuracy of endoscopic ultrasonography diagnosis for the invasive depth of early gastric cancer. Int J Gastrointest Cancer. 2006;37:133-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Kim JH, Song KS, Youn YH, Lee YC, Cheon JH, Song SY, Chung JB. Clinicopathologic factors influence accurate endosonographic assessment for early gastric cancer. Gastrointest Endosc. 2007;66:901-908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 34. | Nakamura T, Tajika M, Kawai H, Yokoi T, Yatabe Y, Nakamura S. Is endoscopic urtrasonography (EUS) needed for deciding the indication for endoscopic submucosal dissection (ESD) of early gastric cancinoma? Stomach Intestine. 2005;40:779-790. [Cited in This Article: ] |
| 35. |
Sano T, Okuyama Y, Kobori O, Shimizu T, Morioka Y, “Early gastric cancer, ” Endoscopic diagnosis of depth of invasion.
|
| 36. | Shi D, Xi XX. Factors Affecting the Accuracy of Endoscopic Ultrasonography in the Diagnosis of Early Gastric Cancer Invasion Depth: A Meta-analysis. Gastroenterol Res Pract. 2019;2019:8241381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Lan Z, Hu H, Mandip R, Zhu W, Guo W, Wen J, Xie F, Qiao W, Venkata A, Huang Y, Liu S, Li Y. Linear-array endoscopic ultrasound improves the accuracy of preoperative submucosal invasion prediction in suspected early gastric cancer compared with radial endoscopic ultrasound: A prospective cohort study. J Gastroenterol Hepatol. 2020;35:118-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Serrano OK, Huang K, Ng N, Yang J, Friedmann P, Libutti SK, Kennedy TJ. Correlation between preoperative endoscopic ultrasound and surgical pathology staging of gastric adenocarcinoma: A single institution retrospective review. J Surg Oncol. 2016;113:42-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ, Falk SJ, Iveson TJ, Smith DB, Langley RE, Verma M, Weeden S, Chua YJ, MAGIC Trial Participants. Perioperative chemotherapy vs surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4120] [Cited by in F6Publishing: 4237] [Article Influence: 235.4] [Reference Citation Analysis (0)] |
| 40. | Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, Ducourtieux M, Bedenne L, Fabre JM, Saint-Aubert B, Genève J, Lasser P, Rougier P. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29:1715-1721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1216] [Cited by in F6Publishing: 1358] [Article Influence: 104.5] [Reference Citation Analysis (0)] |
| 41. | van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, Richel DJ, Nieuwenhuijzen GA, Hospers GA, Bonenkamp JJ, Cuesta MA, Blaisse RJ, Busch OR, ten Kate FJ, Creemers GJ, Punt CJ, Plukker JT, Verheul HM, Spillenaar Bilgen EJ, van Dekken H, van der Sangen MJ, Rozema T, Biermann K, Beukema JC, Piet AH, van Rij CM, Reinders JG, Tilanus HW, van der Gaast A; CROSS Group. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366:2074-2084. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3288] [Cited by in F6Publishing: 3648] [Article Influence: 304.0] [Reference Citation Analysis (0)] |
| 42. | Yoshikawa T, Tanabe K, Nishikawa K, Ito Y, Matsui T, Kimura Y, Hirabayashi N, Mikata S, Iwahashi M, Fukushima R, Takiguchi N, Miyashiro I, Morita S, Miyashita Y, Tsuburaya A, Sakamoto J. Induction of a pathological complete response by four courses of neoadjuvant chemotherapy for gastric cancer: early results of the randomized phase II COMPASS trial. Ann Surg Oncol. 2014;21:213-219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 43. | Spolverato G, Ejaz A, Kim Y, Squires MH, Poultsides GA, Fields RC, Schmidt C, Weber SM, Votanopoulos K, Maithel SK, Pawlik TM. Use of endoscopic ultrasound in the preoperative staging of gastric cancer: a multi-institutional study of the US gastric cancer collaborative. J Am Coll Surg. 2015;220:48-56. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 44. | Mocellin S, Marchet A, Nitti D. EUS for the staging of gastric cancer: a meta-analysis. Gastrointest Endosc. 2011;73:1122-1134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 45. | Cardoso R, Coburn N, Seevaratnam R, Sutradhar R, Lourenco LG, Mahar A, Law C, Yong E, Tinmouth J. A systematic review and meta-analysis of the utility of EUS for preoperative staging for gastric cancer. Gastric Cancer. 2012;15 Suppl 1:S19-S26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 111] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 46. | Mocellin S, Pasquali S. Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst Rev. 2015;2015:CD009944. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 47. | Pei Q, Wang L, Pan J, Ling T, Lv Y, Zou X. Endoscopic ultrasonography for staging depth of invasion in early gastric cancer: A meta-analysis. J Gastroenterol Hepatol. 2015;30:1566-1573. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 48. | Costa JM, Gonçalves B, Miguel Gomes M, Fernandes D, Gonçalves R, Soares JB. Accuracy of endoscopic ultrasound in gastric adenocarcinoma patient selection for neoadjuvant therapy. United European Gastroenterol J. 2019;7:278-286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 49. | van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M, Hucl T, Kunda R, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Perez-Miranda M, van Hooft JE. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:185-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 139] [Article Influence: 69.5] [Reference Citation Analysis (2)] |
| 50. | Rizzatti G, Larghi A. [Therapeutic endoscopic ultrasound: current indications and future perspectives.]. Recenti Prog Med. 2021;112:54-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 51. | Ogura T, Okuda A, Miyano A, Imanishi M, Nishioka N, Yamada M, Yamda T, Kamiyama R, Masuda D, Higuchi K. EUS-guided vs percutaneous biliary access in patients with obstructive jaundice due to gastric cancer. Dig Liver Dis. 2019;51:247-252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |