Published online Sep 16, 2021. doi: 10.4253/wjge.v13.i9.382
Peer-review started: March 24, 2021
First decision: June 3, 2021
Revised: June 15, 2021
Accepted: August 12, 2021
Article in press: August 12, 2021
Published online: September 16, 2021
Crohn’s disease (CD) has a multitude of complications including intestinal strictures from fibrostenotic disease. Fibrostenotic disease has been reported in 10%-17% of children at presentation and leads to surgery in 20%-50% of cases within ten years of diagnosis. When symptoms develop from these strictures, the treatment in children has primarily been surgical resection. Endoscopic balloon dilation (EBD) has been shown to be a safe and efficacious alternative to surgery in adults, but evidence is poor in the literature regarding its safety and efficacy in children.
To evaluate the outcomes of children with fibrostenosing CD who underwent EBD vs surgery as a treatment.
In a single-center retrospective study, we looked at pediatric patients (ages 0-18) who carry the diagnosis of CD, who were diagnosed after opening a dedicated Inflammatory Bowel Disease clinic on July 1, 2012 through May 1, 2019. We used diagnostic codes through our electronic medical record to identify patients with CD with a stricturing phenotype. The type of intervention for patients’ strictures was then identified through procedural and surgical billing codes. We evaluated their demographics, clinical variables, whether they underwent EBD vs surgery or both, and their clinical outcomes.
Of the 139 patients with CD, 25 (18%) developed strictures. The initial interven
EBD is safe and efficacious as an alternative to surgery for palliative management of strictures in selected pediatric patients with CD.
Core Tip: Endoscopic balloon dilation (EBD) has been shown to be a safe and efficacious alternative to surgery in adults, but evidence is poor in the literature regarding its safety and efficacy in children. In our retrospective cohort, 22 of the 25 (88%) treated strictures were successfully managed by EBD and did not require any further surgical intervention during our follow up period. All patients who underwent EBD had no procedural complications, such as a perforation, showing that EBD is safe and efficacious as an alternative to surgery for palliative management of strictures in selected pediatric patients with Crohn’s disease.
- Citation: McSorley B, Cina RA, Jump C, Palmadottir J, Quiros JA. Endoscopic balloon dilation for management of stricturing Crohn’s disease in children. World J Gastrointest Endosc 2021; 13(9): 382-390
- URL: https://www.wjgnet.com/1948-5190/full/v13/i9/382.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i9.382
In pediatric Crohn’s disease (CD), intestinal strictures are a major cause of morbidity and one of leading causes for surgery with cumulative incidence of 20%-50% after 10 years of diagnosis[1]. It is estimated that strictures, defined by a luminal narrowing and thickening of the intestinal wall that results in obstructive clinical symptoms, are present in approximately 10%-17% of children at the time of diagnosis[2]. Strictures can appear at any point in the gastrointestinal tract, but most commonly appear in the ileocecal region and can cause symptoms, such as abdominal pain, bloating, emesis, decreased energy, and growth failure[3]. Surgery has been a mainstay treatment for intestinal strictures in pediatric CD with resection for longer strictures ( > 5 cm in length) or strictureplasty for simple, shorter strictures[4]. Strictureplasty is a surgical procedure that repairs a stricture by widening the narrowed area with intestinal conservation[5,6]. Post-operative complications from surgical resection include fistulas, leaks, short bowel syndrome, and recurrence of the stricture at the anasto
Given the high likelihood of surgery in a CD patient, attempts should be made to find alternatives to surgery in these patients. One such alternative is endoscopic balloon dilation (EBD), through which an endoscopist traverses the stricture with a balloon device that is then inflated in an effort to increase the diameter of the intestinal lumen. EBD has been demonstrated to be a safe and efficacious alternative to surgery in adults with CD, but there was a paucity of evidence regarding use in children until our initial publication in 2008[3,7]. Evolution of our knowledge regarding outcomes from fibrostenosing CD and anti-inflammatory effects of biologic therapy suggested stenosing disease evolves independently, which is propelled by local myofibroblast activity, soluble chemokines, and growth factors[9]. The accumulation of this understanding led to the eventual guidelines published by the European Crohn’s and Colitis Organization in 2016[10]. The aim of our study is to evaluate the longitudinal outcomes of children with CD who underwent EBD vs surgical resection as a treatment of their strictures in order to show that EBD is efficacious as an alternative to surgery for management of simple strictures in pediatric fibrostenosing CD.
In a single-center retrospective study, we looked at pediatric patients (ages 0-18) who carry the diagnosis of CD who were diagnosed after opening a dedicated Inflammatory Bowel Disease clinic on July 1, 2012 through May 1, 2019. We used diagnostic codes through our electronic medical record to identify patients with CD with a stricturing phenotype. The type of intervention for patients’ strictures was then identified through procedural and surgical billing codes. Patient demographics, disease characteristics and longitudinal clinical outcomes were obtained through review of the electronic medical record. Demographic data included: age at diagnosis of CD, age at time of procedure, body mass index (BMI) at time of procedure, and race. Disease characteristics included: modality of CD diagnosis, time (years) from diagnosis of CD until the development of symptomatic strictures, the Paris classification of disease, and medication at the time of the procedure. Symptomatic strictures were defined as new onset or worsening of baseline abdominal pain, post-prandial bloating, and/or emesis. Information obtained about the intestinal stricture and procedure(s) included the location, length, number of strictures, the presence of penetrating disease near the stricture site, the type of stricture intervention (EBD, surgery, or both), and if any medication was injected into the stricture at the time of EBD. Strictures were classified as simple, which were defined as single and < 5 cm, or complex, which were defined by multiple, > 5 cm or associated with a fistula.
All patients with complex strictures underwent surgical resection of their stricture sites rather than strictureplasty. All EBDs were done by a single provider, using the same technique (JAQ). First, a 0.25 mm soft tip guidewire was passed through the stricture. In the case of medication injected at the stricture site, 2 mg/kg up to 80 mg of triamcinolone was diluted in 5 mL of saline and was then injected into all four quadrants of the stricture area prior to dilation. A single patient received an injection of an infliximab biosimilar (0.5 mg/kg) diluted in 25 mL of saline at the stricture site before dilation. After the injection of the stricture, a through the scope controlled radial release (CRR) colonic balloon dilator was placed over the guidewire and serial dilations were done until the desired diameter was achieved to allow endoscope passage for inspection of the proximal bowel (Figure 1).
Of the 139 active patients diagnosed with CD in the study period, 25 (18%) developed intestinal strictures; 13 patients (52%) were male and 22 patients (88%) were Caucasian (Table 1). BMI was recorded in the 25 patients and nine (36%) were in the overweight BMI category (BMI > 85th and < 95th percentiles). Six of those patients had complex strictures and went directly to surgical resection. The mean age at diagnosis of CD was 13 years. In 23 of the 25 patients, diagnosis was made via upper and lower endoscopy with biopsies confirming CD, and the other two patients had stricturing and penetrating disease at the time of diagnosis, and CD was confirmed on histologic review of the surgically-resected specimen. Using the Paris Classification, CD location was classified as: ileocolonic (n = 20, 80%), distal 1/3 of the ileum with limited cecal disease (n = 3, 12%), colonic (n = 1, 4%), or upper disease proximal to the ligament of Treitz and ileocolonic (n = 1, 4%). CD behavior was classified as: stricturing (n = 11, 44%), stricturing and penetrating (n = 9, 36%), stricturing and perianal disease (n = 3, 12%), or stricturing, penetrating and perianal disease (n = 2, 8%). The mean time of development of symptomatic strictures from time of diagnosis was 1.5 years. Twenty (80%) of these strictures were located in the terminal ileum, 3 (12%) in the rectum, 1 (4%) in the duodenum, and 1 (4%) in the ascending colon (Figure 1).
| Surgery only, n = 8 | EBD only, n = 11 | Surgery and EBD, n = 6 | |
| Sex, n (%) | |||
| Male | 4 (50) | 6 (55) | 3 (50) |
| Female | 4 (50) | 5 (45) | 3 (50) |
| Age at diagnosis, n (%) | |||
| 0-10 | 1 (12) | 1 (9) | 1 (17) |
| 11-18 | 7 (88) | 10 (91) | 5 (83) |
| Race, n (%) | |||
| Caucasian | 7 (88) | 11 (100) | 4 (67) |
| African-American | 1 (12) | 0 | 2 (33) |
| BMI, n (%) | |||
| Underweight | 2 (25) | 2 (18) | 0 (0) |
| Normal | 0 | 7 (64) | 5 (83) |
| Overweight | 6 (75) | 2 (18) | 1 (17) |
| On biologic, n (%) | 6 (75) | 10 (91) | 5 (83) |
| On steroids, n (%) | 0 | 2 (18) | 1 (17) |
| Location of stricture, n (%) | |||
| Terminal ileum | 6 (75) | 2 (18) | 4 (66) |
| Ileocecal valve | 2 (25) | 5 (46) | 1 (17) |
| Colon | 0 | 1 (9) | 0 |
| Duodenum | 0 | 1 (9) | 0 |
| Rectum/anus | 0 | 2 (18) | 1 (17) |
| Average years of disease until development of stricture | 2.1 | 1.9 | 1 |
| Stricturing disease only, n (%) | 4 (50) | 8 (73) | 2 (33) |
| Stricturing and penetrating disease, n (%) | 4 (50) | 3 (27) | 4 (67) |
At the time of intervention, most patients (n = 21, 84%) were on biologic therapy; 11 patients were on infliximab or an infliximab biosimilar, 9 patients were on adalimumab, and one patient was on vedolizumab. Of the four patients not receiving biologic therapy, three patients were managed with azathioprine and one was managed with mesalamine alone. Three patients (12%) were on low-dose corticosteroids in addition to biologic therapy.
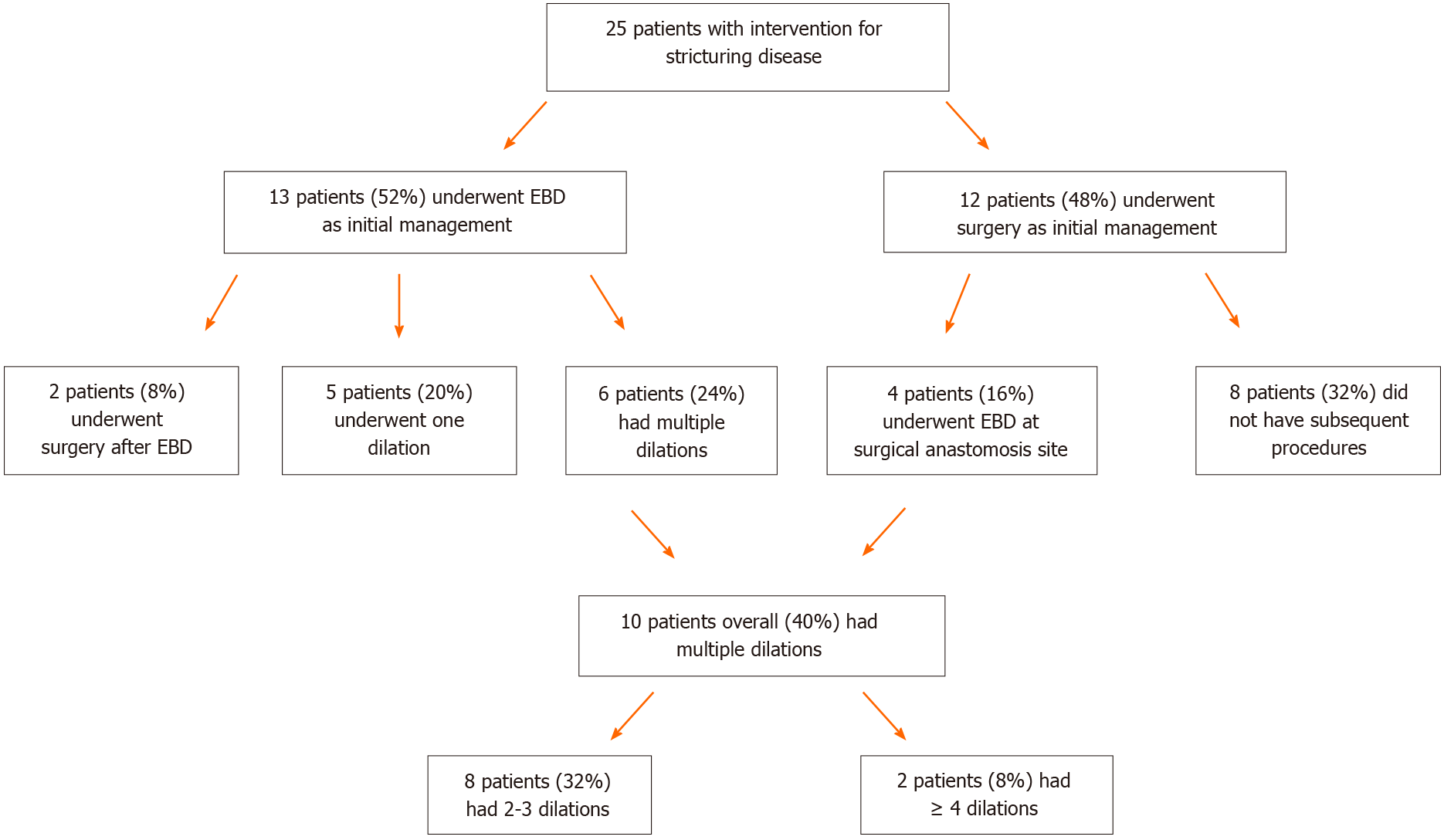
The initial intervention for a stricture was surgical resection in 12 patients (48%) and EBD in 13 patients (52%). However, 4 (33%) patients whom initially had surgical resection required follow-up EBD, and thus 17 total patients (68%) underwent EBD at some point in their treatment process. The frequency of EBD procedures performed on an individual patient was: one EBD (n = 7, 41%), 2-3 EBD (n = 8, 47%), 4 or more EBD (n = 2, 12%) (Figure 2). All patients that underwent EBD had strictures with a length less than or equal to 5 cm in length and inflammation was controlled with medications prior to EBD. Fifteen patients received a triamcinolone injection into the stricture site and one patient received an infliximab biosimilar injection at the stricture site. There were no post-EBD perforations, bleeding requiring intervention, or infections. Of the 8 patients who underwent successful surgical resection alone, 4 patients (50%) had a fistula present near the stricture site and 4 (50%) had strictures greater than 5 cm in length. Overall, 88% (15/17) with stricturing disease treated endoscopically did not require any further surgical interventions.
The natural history of CD in children suggests that most children present with inflammatory disease but a proportion will develop more complicated stricturing or penetrating disease[11]. Given the high overall rate of surgery in CD, the rate of recurrence of strictures post-surgery, and the risk of complications post-surgery, there exists the need for alternative interventions[6,7,12]. EBD offers a minimally invasive, therapeutic approach that can reduce or obviate the need for surgical intervention[13]. It has been shown to be efficacious in adult stricturing CD with overall reported technical success rate of 89.1% to 94.9% and associated clinical efficacy of 80.8%-82.3%[14,15]. Complications are also minimal in EBD compared to surgery with a complication rate averaging around 2% overall[16]. Here, we aim to demonstrate similar efficacy and safety in our pediatric CD cohort.
In our single-center cohort, 88% (15/17) of patients with stricturing CD treated via EBD did not require any further surgical interventions. This is a higher success rate than the adult literature where a meta-analysis of 33 studies showed that surgical intervention was avoided in 57% of adult patients who had undergone EBD[14]. In our cohort, there was a need for repeat EBD in 6/17 (35%) patients whom had initial EBD and a need for EBD after surgical resection in 4/12 (33%) patients. The adult literature cites that need for repeat EBD as 73.5% in a meta-analysis and 47% in another study, and the need for EBD after surgical resection at 62%[14,17]. It is difficult to compare our rates of success and need for repeat dilations to adult studies given the small number of patients in our study and a different range in follow up time. In our study, follow up ranged from 6 mo to 2 years compared to the two years used in adult literature[14,17].
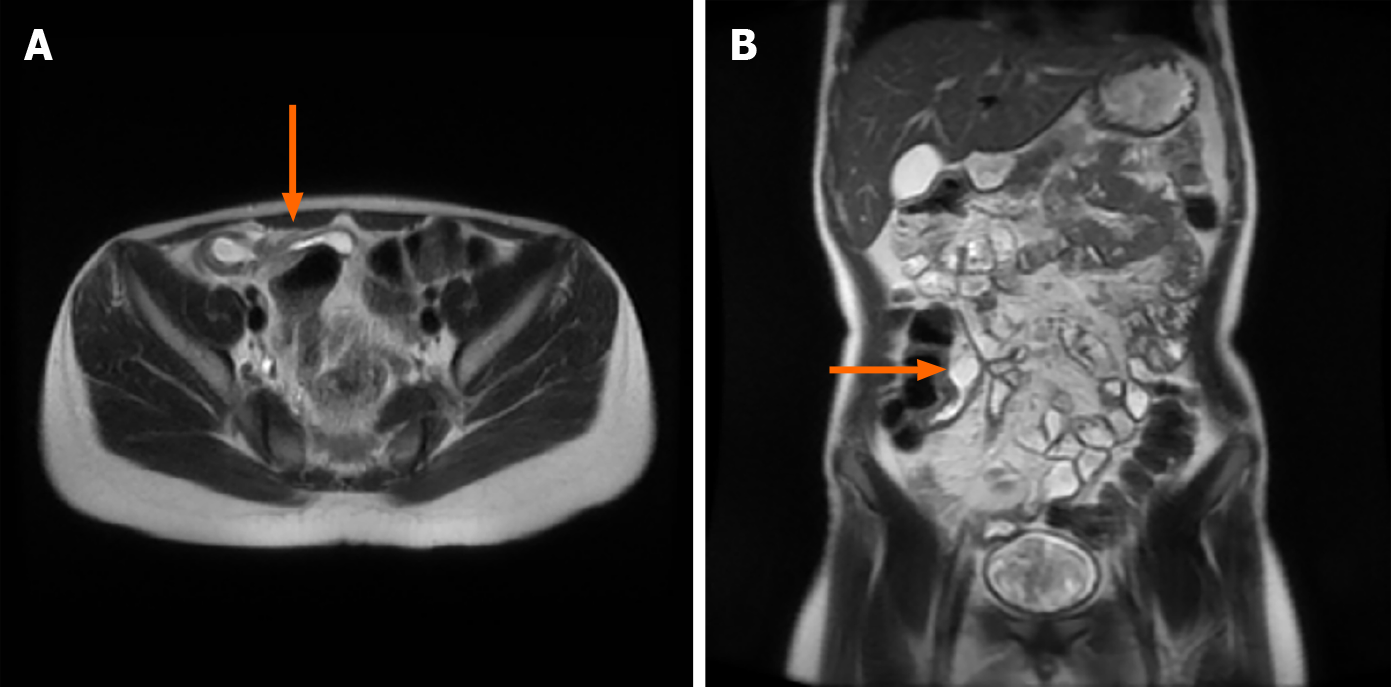
In our population, there were no complications of perforation, bleeding, or infection for any patient who underwent EBD. Although this is reassuring, our study is again limited by the small number of patients making it difficult to compare to the rate of complications in the literature which is around 2%[8]. In addition, patients who were deemed high risk by the adult literature, those with longer strictures (≥ 5 cm) and the presence of a nearby abscess or fistula, were not candidates for EBD and underwent primary surgical resection instead[14,17,18]. Our data does support previous literature about the safety of EBD in patients with uncomplicated, fibrostenotic, non-inflammatory and short segment strictures (< 5 cm in length) (Figure 3)[18].
The majority of our patients (15/17) also received intralesional steroid injection into the stricture site. This has been documented as effective by showing the reduction in the need for further endoscopic dilations and surgical interventions in a double-blinded controlled trial in pediatric patients[5]. One patient in our study received an injection of an infliximab biosimilar at the stricture site prior to dilation. This patient had a high-grade duodenal stricture at presentation of her disease which did not allow for tolerance of enteral nutrition. Due to severity of her clinical condition, surgical risk and after internal discussion and family approval, the suitability of this approach was felt to be acceptable. One study in the adult literature showed that injection of 40 mg of infliximab into strictures in six patients was successful[19]. All six patients at the final follow-up at six months described relief of obstructive symptoms and no patients were referred to surgery during the follow-up period[19]. Our patient did require two dilations with infliximab biosimilar injection, and she eventually had resolution of her symptoms and was able to advance to a regular diet. Although there are some smaller studies describing success of injection of biologics into strictures, this has not been proven to be fully efficacious due to the small number of patients that have received a biologic injection into their stricture site. In contrast, a multicenter study from the United States did not show that intra-lesional steroids or biologics lower the risk of further interventions or surgery[20].
In addition, our data suggests that there seems to be an interesting correlation with higher BMI and worsening disease. Six patients (66%) in the overweight BMI category (BMI > 85th and < 95th percentiles) were those patients with complex strictures that went directly to surgical resection. This correlates with a study that was published in the journal of Biomolecules in 2019 which showed that increased visceral adipose tissue, “creeping fat,” can worsen intestinal inflammation through increased altered adipocyte function and through deregulated leptin and adiponectin production[21]. Another recent prospective study from Australia suggested that visceral adipose tissue to subcutaneous adipose tissue ratio was positively associated with risk of stricturing disease behavior and elevated fecal calprotectin in patients with ileocolonic disease; however, these findings are controversial and ongoing research is required to better classify this correlation[22].
Though EBD is shown to be safe and efficacious based on our initial data and the data in the literature, it does have limitations. Surgical resection is still recommended as initial management in longer strictures or for complicated strictures due to an increased risk for perforation[18]. Before EBD is performed, it is recommended to characterize the number, nature and length of the stricture using magnetic resonance enterography or small intestine contrast ultrasonography[18]. Furthermore, EBD requires a skilled endoscopist who is comfortable performing these procedures, and this may not be available at all pediatric centers.
There has been a small amount of published data on EBD in pediatric fibrostenosing CD since our first publication in 2008. Our initial experience suggested that EBD was safe and efficacious in children with short and uncomplicated strictures secondary to fibrostenosing CD which we proceeded to implement in our active day to day care of pediatric CD with these results. Our study is limited by a modest follow-up interval and relatively small number of patients. Further research is most definitely needed in order to find the ideal role for EBD in the management of fibrostenosing CD in children and to further assess the long-term efficacy of the procedure when comparing to surgical intervention in children. We also need to determine if biologic injection at the site of a stricture is a superior option in prevention of stricture recurrence at the dilation site and need to develop ideal tools and techniques to reproducibly manage patients with CD-related intestinal strictures.
EBD is safe and efficacious as an alternative to surgery for palliative management of strictures in selected pediatric patients with CD with a high response rate and low complication rate directly related to the procedure.
Currently up to 75% of patients with Crohn's disease (CD) are expected to need surgery due to disease related complications. Intestinal fibrostenosing disease is a common complication and biologic therapy has not limited its appearance even with much improved clinical response rates. Due to a high risk for surgery, attempts to find alternatives to surgery need to be made. Endoscopic balloon dilation with adequate technique promises to have an important role in his area.
Endoscopic balloon dilation has already been shown to be efficacious in adults but no large case series involving pediatric patients exists currently in literature.
We aimed to evaluate the short and long term outcomes of CD who developed fibrostenosing disease and underwent endoscopic balloon dilation as primary or secondary therapy.
This is a single-center case series in which all subjects who were diagnosed with diagnosed between 2012 and 2019 were included in the study, and those that developed fibrostenosing disease were identified. Their records were then reviewed for types of interventions performed and outcomes. Patients were classified into primary surgical or endoscopy-treated subjects and those that subsequently required surgery or endoscopy were thus classified. Demographic data included: age at diagnosis of CD, age at time of procedure, body mass index (BMI) at time of procedure, and race. Disease characteristics included: modality of CD diagnosis, time (years) from diagnosis of CD until the development of symptomatic strictures, the Paris classification of disease, and medication at the time of the procedure.
We identified 139 subjects diagnosed with CD in this study period. Of these patients, 25 (17%) were noted to have a fibrostenotic lesion anywhere in the small and large bowel. 13 (52%) underwent primary endoscopic therapy vs 12 (48%) who underwent surgical management. Of the patients who went to surgery, 4 (16%) had to have further endoscopic treatment after surgery, compared to just 2 (8%) of those who had endoscopy as primary therapy. Of note, 5 (20%) required just one endoscopic therapy session for resolution of their stricture.
Endoscopic balloon dilation is a safe and effective treatment in children with CD-related fibrostenosing disease. Adequate patient selection is key to ensure a high success rate. Pediatric patients undergoing surgery for fibrostenosing disease should be cautioned that a 1 in 5 risk of requiring further endoscopic therapy is a distinct possibility.
Our data suggested an interesting correlation between higher BMI and risk of stricturing disease. Pediatric patients with BMI > 85% and < 95% had a higher risk of complex strictures requiring surgery. This brings into new light publications associating an increase in visceral adipose tissue with intestinal inflammation through dysregulated leptin and adiponectin production.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy; American College of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Salkic N S-Editor: Gao CC L-Editor: A P-Editor: Guo X
| 1. | Bernell O, Lapidus A, Hellers G. Risk factors for surgery and recurrence in 907 patients with primary ileocaecal Crohn's disease. Br J Surg. 2000;87:1697-1701. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 241] [Cited by in F6Publishing: 234] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 2. | Shaoul R, Karban A, Reif S, Weiss B, Shamir R, Tamir A, Davidovich O, Halevi J, Silver EL, Levine A. Disease behavior in children with Crohn's disease: the effect of disease duration, ethnicity, genotype, and phenotype. Dig Dis Sci. 2009;54:142-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Thienpont C, D'Hoore A, Vermeire S, Demedts I, Bisschops R, Coremans G, Rutgeerts P, Van Assche G. Long-term outcome of endoscopic dilatation in patients with Crohn's disease is not affected by disease activity or medical therapy. Gut. 2010;59:320-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 142] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 4. | Stenke E, Bourke B, Knaus U. Crohn's Strictures-Moving Away from the Knife. Front Pediatr. 2017;5:141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Di Nardo G, Oliva S, Passariello M, Pallotta N, Civitelli F, Frediani S, Gualdi G, Gandullia P, Mallardo S, Cucchiara S. Intralesional steroid injection after endoscopic balloon dilation in pediatric Crohn's disease with stricture: a prospective, randomized, double-blind, controlled trial. Gastrointest Endosc. 2010;72:1201-1208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 6. | Splawski JB, Pffefferkorn MD, Schaefer ME, Day AS, Soldes OS, Ponsky TA, Stein P, Kaplan JL, Saeed SA. NASPGHAN Clinical Report on Postoperative Recurrence in Pediatric Crohn Disease. J Pediatr Gastroenterol Nutr. 2017;65:475-486. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Foster EN, Quiros JA, Prindiville TP. Long-term follow-up of the endoscopic treatment of strictures in pediatric and adult patients with inflammatory bowel disease. J Clin Gastroenterol. 2008;42:880-885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Singh A, Agrawal N, Kurada S, Lopez R, Kessler H, Philpott J, Shen B, Lashner B, Rieder F. Efficacy, Safety, and Long-term Outcome of Serial Endoscopic Balloon Dilation for Upper Gastrointestinal Crohn's Disease-associated Strictures-A Cohort Study. J Crohns Colitis. 2017;11:1044-1051. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Speca S, Giusti I, Rieder F, Latella G. Cellular and molecular mechanisms of intestinal fibrosis. World J Gastroenterol. 2012;18:3635-3661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 177] [Cited by in F6Publishing: 177] [Article Influence: 14.8] [Reference Citation Analysis (1)] |
| 10. | Rieder F, Latella G, Magro F, Yuksel ES, Higgins PD, Di Sabatino A, de Bruyn JR, Rimola J, Brito J, Bettenworth D, van Assche G, Bemelman W, d'Hoore A, Pellino G, Dignass AU. European Crohn's and Colitis Organisation Topical Review on Prediction, Diagnosis and Management of Fibrostenosing Crohn's Disease. J Crohns Colitis. 2016;10:873-885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 160] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 11. | Vernier-Massouille G, Balde M, Salleron J, Turck D, Dupas JL, Mouterde O, Merle V, Salomez JL, Branche J, Marti R, Lerebours E, Cortot A, Gower-Rousseau C, Colombel JF. Natural history of pediatric Crohn's disease: a population-based cohort study. Gastroenterology. 2008;135:1106-1113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 427] [Cited by in F6Publishing: 420] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 12. | Singh VV, Draganov P, Valentine J. Efficacy and safety of endoscopic balloon dilation of symptomatic upper and lower gastrointestinal Crohn's disease strictures. J Clin Gastroenterol. 2005;39:284-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 13. | de'Angelis N, Carra MC, Borrelli O, Bizzarri B, Vincenzi F, Fornaroli F, De Caro G, de'Angelis GL. Short- and long-term efficacy of endoscopic balloon dilation in Crohn's disease strictures. World J Gastroenterol. 2013;19:2660-2667. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 38] [Cited by in F6Publishing: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Bettenworth D, Gustavsson A, Atreja A, Lopez R, Tysk C, van Assche G, Rieder F. A Pooled Analysis of Efficacy, Safety, and Long-term Outcome of Endoscopic Balloon Dilation Therapy for Patients with Stricturing Crohn's Disease. Inflamm Bowel Dis. 2017;23:133-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 141] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 15. | Bettenworth D, Bokemeyer A, Kou L, Lopez R, Bena JF, El Ouali S, Mao R, Kurada S, Bhatt A, Beyna T, Halloran B, Reeson M, Hosomi S, Kishi M, Hirai F, Ohmiya N, Rieder F. Systematic review with meta-analysis: efficacy of balloon-assisted enteroscopy for dilation of small bowel Crohn's disease strictures. Aliment Pharmacol Ther. 2020;52:1104-1116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 16. | Gustavsson A, Magnuson A, Blomberg B, Andersson M, Halfvarson J, Tysk C. Endoscopic dilation is an efficacious and safe treatment of intestinal strictures in Crohn's disease. Aliment Pharmacol Ther. 2012;36:151-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Winder O, Fliss-Isakov N, Winder G, Scapa E, Yanai H, Barnes S, Dekel R, Dotan I, Maharshak N. Clinical outcomes of endoscopic balloon dilatation of intestinal strictures in patients with Crohn's disease. Medicine (Baltimore). 2019;98:e16864. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Oliva S, Thomson M, de Ridder L, Martín-de-Carpi J, Van Biervliet S, Braegger C, Dias JA, Kolacek S, Miele E, Buderus S, Bronsky J, Winter H, Navas-López VM, Assa A, Chong SKF, Afzal NA, Smets F, Shaoul R, Hussey S, Turner D, Cucchiara S. Endoscopy in Pediatric Inflammatory Bowel Disease: A Position Paper on Behalf of the Porto IBD Group of the European Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2018;67:414-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 35] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 19. | Hendel J, Karstensen JG, Vilmann P. Serial intralesional injections of infliximab in small bowel Crohn's strictures are feasible and might lower inflammation. United European Gastroenterol J. 2014;2:406-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Atreja A, Aggarwal A, Dwivedi S, Rieder F, Lopez R, Lashner BA, Brzezinski A, Vargo JJ, Shen B. Safety and efficacy of endoscopic dilation for primary and anastomotic Crohn's disease strictures. J Crohns Colitis. 2014;8:392-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 21. | Bilski J, Mazur-Bialy A, Wojcik D, Surmiak M, Magierowski M, Sliwowski Z, Pajdo R, Kwiecien S, Danielak A, Ptak-Belowska A, Brzozowski T. Role of Obesity, Mesenteric Adipose Tissue, and Adipokines in Inflammatory Bowel Diseases. Biomolecules. 2019;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 22. | Bryant RV, Schultz CG, Ooi S, Goess C, Costello SP, Vincent AD, Schoeman S, Lim A, Bartholomeusz FD, Travis SPL, Andrews JM. Visceral Adipose Tissue Is Associated With Stricturing Crohn's Disease Behavior, Fecal Calprotectin, and Quality of Life. Inflamm Bowel Dis. 2019;25:592-600. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |