Published online May 27, 2012. doi: 10.4240/wjgs.v4.i5.131
Revised: October 27, 2011
Accepted: November 24, 2011
Published online: May 27, 2012
We report a case of adult intussusception caused by cecal adenocarcinoma that was treated by laparoscopy-assisted ileocecal resection following reduction by contrast enema and preoperative colonoscopy. A 68-year-old male with cecal cancer was admitted to our hospital because of colicky abdominal pain after taking a laxative. His abdomen was distended, and a mass was palpable in the right upper quadrant, which appeared as a target- or sausage-shaped lesion by ultrasonograhpy and computed tomography. A contrast enema using water-soluble material showed a cup-shaped filling defect characterized by intussusception in the ascending colon. This round defect with a clear margin was pushed gradually back into the cecum by the enema pressure. Re-occurrence of the intussusception is easily released by colonoscopy. We performed laparoscopy-assisted ileocecal resection of a protruding tumor measuring 6.5 cm × 5.0 cm × 3.5 cm from the cecum, with D3 lymph node dissection. Histological examination revealed a well-differentiated adenocarcinoma that had invaded the serosa without permeating the lymphatic or venous capillaries, as well as lymph node metastasis. The postoperative course was uneventful, and the patient has been well without evidence of disease recurrence for 5 years following the operation. Preliminary reduction of adult colonic intussusception before surgical resection is therefore an option in cases of an early and correct diagnosis of intussusception.
- Citation: Namikawa T, Okamoto K, Okabayashi T, Kumon M, Kobayashi M, Hanazaki K. Adult intussusception with cecal adenocarcinoma: Successful treatment by laparoscopy-assisted surgery following preoperative reduction. World J Gastrointest Surg 2012; 4(5): 131-134
- URL: https://www.wjgnet.com/1948-9366/full/v4/i5/131.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i5.131
Intestinal intussusception is relatively common in children whereby a proximal bowel segment invaginates into the lumen of a distal bowel segment; however, adult intussusception is rare[1-3]. It is estimated that only 5% of all intussusceptions occur in adults, accounting for approximately 1% of patients with bowel obstructions[4,5]. Moreover, colonic intussusception is less common than small intestinal intussusception, and is generally associated with malignancy[4].
The diagnosis of intussusception can be elusive for a long period because of the varied presenting symptoms and time course, and is frequently only established during laparotomy to investigate the obstructive symptoms[2,5]. Treatment of intussusception usually requires resection of the involved bowel segment, although reduction is possible if the segment involved is viable. However, such approaches to treating intussusception remain controversial, particularly in the colon where there is a high likelihood of an originating neoplasm[5,6].
We report a case of a 68-year-old male with cecal intussusception who was safely treated by laparoscopy-assisted ileocecal resection following preoperative reduction by water-soluble contrast enema and colonoscopy (CS).
A 68-year-old Japanese male visited a local clinician for abdominal pain sustained for 6 mo. CS revealed a cecal mass that proved to be an adenocarcinoma on biopsy, and the patient was referred to our hospital. He had been well with an unremarkable clinical history to that point. Although he was scheduled for elective ileocecal resection, he presented to our hospital with colicky intermittent abdominal pain after taking a laxative. Physical examination revealed a distended and mildly painful abdomen, with a palpable mass and tenderness in the right upper quadrant. Serum carcinoembryonic antigen (CEA) was high (4.8 ng/mL; normal range, < 3.4 ng/mL), but the other laboratory findings were almost within normal limits.
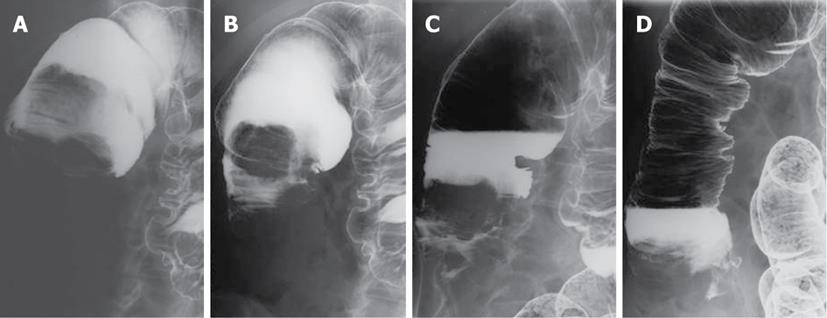
Ultrasonography of the mass in the right upper quadrant revealed a pattern of multiple concentric rings characteristic of intussusception (Figure 1). Computed tomography (CT) of the abdomen with intravenous contrast medium revealed a sausage-shaped soft tissue mass consisting of the outer intussuscipiens and the central intussusceptum, and containing mesenteric fat and mesenteric blood vessels (Figure 2). A water-soluble contrast-material enema showed an intralumenal, smooth, spherical filling defect representing the leading edge of the intussuscepted bowel at the proximal region of the ascending colon (Figure 3A). The pressure of enema succeeded in gradually moving the cecum (intussusceptum) outward from the ascending colon (intussuscipiens) (Figure 3B-D). Subsequent CS revealed a protruding mass at the leading point of intussusception in the ascending colon that was easily reduced. The patient then underwent laparoscopy-assisted ileocecal resection of the tumor with D3 lymph node dissection and primary anastomosis. The intussusception was released, and there were no ascites, swollen lymph nodes, or peritoneal disseminations.
Gross inspection of the resected specimen revealed a round, granular-surfaced tumor, measuring 6.5 cm × 5.0 cm × 3.5 cm, and protruding into the lumen. Histologically, the lesions were all well differentiated tubular adenocarcinomas that were invading the serosa (T3) without permeation of the lymphatic or venous capillaries. No lymph node metastasis was seen (Stage II), and the patient was followed up without adjuvant chemotherapy. The postoperative course was uneventful, and he has been well without evidence of disease recurrence for 5 years following the operation.
Intussusception of the bowel is defined as the telescoping of a proximal segment of the gastrointestinal tract within the lumen of an adjacent segment[1]. Intussusception in the adult is a rare entity that differs greatly in etiology compared with that seen in the pediatric population. We successfully treated a case of adult intussusception due to cecal adenocarcinoma using contrast enema and colonoscopy for reduction followed by laparoscopy-assisted ileocecal resection.
Sonographic or radiographic studies may distinguish between intussusception and other more common causes of intestinal obstruction. Intussusception can be confidently diagnosed on CT because of its virtually pathognomonic target-sign or sausage-shaped appearance[5,7,8]. It appears as a complex soft tissue mass, consisting of the intussuscepted mesenteric fat and a soft tissue rim representing the opposing walls of the intussuscipiens and the intussusceptum[7]. Accordingly, CT is very useful and less invasive in the diagnosis of adult intussusception with intestinal obstruction and peritoneal irritation[9-11].
Intestinal intussusception can be classified according to location (small intestine or colon) or according to the underlying etiology [neoplastic (benign or malignant), non-neoplastic, or idiopathic]. In adults, 80%-90% of intussusceptions are secondary to an underlying pathology, with approximately 65% due to benign or malignant neoplasm[7,9]. The incidence of malignancy is particularly high with colonic intussusception, at 50%-71%[9,12]. Intussusception in the colon and the presence of anemia are also regarded as independent preoperative predictors of malignancy[12]. When intussusception is suspected, water-soluble contrast enema is useful for diagnosis, on finding the characteristic cup-shaped filling defect, and for treatment due to the enema pressure.
The optimal therapeutic management of adult intussusception remains controversial due to the differing etiology between pediatric and adult populations. A precipitating lesion is found in 90% of adult intussusception cases, but in only 10% of pediatric patients[9,10,13]. Thus, a major point of controversy in adult intussusception is whether to reduce the intestine before resection of the bowel. Preoperative diagnosis is often difficult or delayed because of the nonspecific nature and varying duration of symptoms, thus treatment usually requires formal resection of the involved bowel segment[1,14,15]. Accordingly, several studies have recommended surgical resection of the intussusception without reduction as the preferred treatment in adults, because of the high risk of primary adenocarcinoma[4,10,13].
The downsides of reduction prior to resection include the theoretical risk of intralumenal tumor seeding, reduction of externally viable bowel despite mucosal necrosis, venous embolization of malignant cells, spillage of succus through inadvertent perforation, and anastomotic complication in cases of an edematous and weakened bowel[10]. However, while there are theoretic concerns, no rigorous studies have satisfactorily resolved this issue. In the present case, we chose preoperative reduction before resection due to the short time between symptom presentation and diagnosis as intussusception. As result, the patient was able to undergo laparoscopy-assisted surgery, and has been well without evidence of complications of recurrence for 5 years following the operation.
It should be noted, however, that because most patients with intussusception present with long-standing and varied symptoms, reductions prior to resection are probably suitable only in a limited number of cases[1,16,17], such as in adult colonic intussusception presented at an early stage. Most cases will require treatment by conventional open surgery.
In conclusion, intussusception occurs rarely in adults. It has a characteristic appearance by ultrasonography and CT, and comprises edematous bowel wall and lumenal mesentery. This study indicates that cases of short-duration adult intussusception, even at colonic sites, could be effectively treated by preoperative reduction followed by minimally invasive surgery using laparoscopy, thus avoiding extensive and invasive resection.
Peer reviewer: Harald R Rosen, MD, Professor, Department of Surgery, Vienna Medical School, St. Vincent Hospital, Stumpergasse 13, Vienna A-1060, Austria
S- Editor A L- Editor Hughes D E- Editor Zheng XM
| 1. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 428] [Cited by in F6Publishing: 449] [Article Influence: 29.9] [Reference Citation Analysis (1)] |
| 2. | d'Silva KJ, Dwivedi AJ, Shetty A, Prakash S. An unusual presentation of colon cancer in a young individual. Dig Dis Sci. 2005;50:1033-1035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Shioda Y, Koizumi S, Furuya S, Akira S, Kameyama N, Hamano N, Takahashi W, Tokunaga A, Tanaka N, Onda M. Intussusception caused by a carcinoma of the cecum during pregnancy: report of a case and review of the literature. Surg Today. 1993;23:556-561. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Zubaidi A, Al-Saif F, Silverman R. Adult intussusception: a retrospective review. Dis Colon Rectum. 2006;49:1546-1551. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 135] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Stewardson RH, Bombeck CT, Nyhus LM. Critical operative management of small bowel obstruction. Ann Surg. 1978;187:189-193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 133] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Shinoda M, Hatano S, Kawakubo H, Kakefuda T, Omori T, Ishii S. Adult cecoanal intussusception caused by cecum cancer: report of a case. Surg Today. 2007;37:802-805. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review: adult intussusception--a CT diagnosis. Br J Radiol. 2002;75:185-190. [PubMed] [Cited in This Article: ] |
| 8. | Martín-Lorenzo JG, Torralba-Martinez A, Lirón-Ruiz R, Flores-Pastor B, Miguel-Perelló J, Aguilar-Jimenez J, Aguayo-Albasini JL. Intestinal invagination in adults: preoperative diagnosis and management. Int J Colorectal Dis. 2004;19:68-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 365] [Cited by in F6Publishing: 354] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 10. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 648] [Cited by in F6Publishing: 630] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 11. | Yamada H, Morita T, Fujita M, Miyasaka Y, Senmaru N, Oshikiri T. Adult intussusception due to enteric neoplasms. Dig Dis Sci. 2007;52:764-766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Goh BK, Quah HM, Chow PK, Tan KY, Tay KH, Eu KW, Ooi LL, Wong WK. Predictive factors of malignancy in adults with intussusception. World J Surg. 2006;30:1300-1304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Eisen LK, Cunningham JD, Aufses AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 225] [Cited by in F6Publishing: 224] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 14. | Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, Lehur PA, Hamy A, Leborgne J, le Neel JC. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis. 2006;21:834-839. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 155] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Erkan N, Haciyanli M, Yildirim M, Sayhan H, Vardar E, Polat AF. Intussusception in adults: an unusual and challenging condition for surgeons. Int J Colorectal Dis. 2005;20:452-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 108] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 16. | Wang N, Cui XY, Liu Y, Long J, Xu YH, Guo RX, Guo KJ. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15:3303-3308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 142] [Cited by in F6Publishing: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 17. | Chang CC, Chen YY, Chen YF, Lin CN, Yen HH, Lou HY. Adult intussusception in Asians: clinical presentations, diagnosis, and treatment. J Gastroenterol Hepatol. 2007;22:1767-1771. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |