Published online Apr 15, 2023. doi: 10.4239/wjd.v14.i4.412
Peer-review started: September 19, 2022
First decision: December 12, 2022
Revised: December 20, 2022
Accepted: January 9, 2023
Article in press: January 9, 2023
Published online: April 15, 2023
Diabetes mellitus (DM) is characterized by persistently elevated blood glucose concentration that lead to multisystem complications. There are about 400 medicinal plants cited to have a beneficial effect on DM. We must choose products wisely based on data derived from scientific studies. However, a major obstacle in the amalgamation of herbal medicine in modern medical practices is the lack of clinical data on its safety, efficacy and drug interaction. Trials of these herbal products often underreport the side effects and other crucial intervention steps deviating from the standards set by Consolidated Standards of Reporting Trials. Due to a lack of knowledge of the active compounds present in most herbal medicines, product standardization is difficult. Cost-effectiveness is another issue that needs to be kept in mind. In this mini-review, we focus on the anti-hyperglycemic effect of herbal products that are commonly used, along with the concerns stated above.
Core Tip: Diabetes mellitus is an age-old disease. The journey for its remedy came down from nature’s lap. Even in today’s world, half of diabetes patients have used herbal medicines once in their lifetime. It is important to know the active molecule and its interaction with other drugs, which will help to predict therapeutic efficacy and also to standardize the products. A major hindrance is the lack of clinical data providing its safety and efficacy. This review focuses on the dose and efficacy of herbal products that are commonly used, along with the concerns stated above.
- Citation: Giri S, Sahoo J, Roy A, Kamalanathan S, Naik D. Treatment on Nature’s lap: Use of herbal products in the management of hyperglycemia. World J Diabetes 2023; 14(4): 412-423
- URL: https://www.wjgnet.com/1948-9358/full/v14/i4/412.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i4.412
Diabetes mellitus (DM) is an age-old disease. It is characterized by persistently elevated blood glucose concentration that manifests as passing large quantities of sweet-tasting urine. Its existence was found in 1550 BC in an Egyptian papyrus. In India, Charak and Susruta also reported the sweet taste of urine in polyuric states, which attracted ants and other insects in 400-500 BC[1]. Before the advent of allopathic medicine, plants and plant products derived from nature were the only place of trust for people for years. Then modern medicine came in the realm. Interestingly, many allopathic drugs have an herbal background.
Most prescribed drug metformin’s origin is linked to Galega officinalis which was used as herbal medicine in the 19th century in Europe[2]. This plant is rich in guanidine. In the 1930s, guanidine derivatives were in day to day practice, but because of toxicity, they were removed from the market. Metformin which is a dimethyl-biguanide, re-entered into the clinical practice as an antimalarial agent and presently, after 65 years of its discovery, this drug holds the first place in the management of DM. Similarly, alpha-glucosidase inhibitors like voglibose, acarbose and miglitol are derived from microbes[3]. Phlorizin is a compound found in the bark of the apple tree. In 1835, its glucosuric effect was documented. Many years later, from this observation, sodium-glucose cotransporter-2 (SGLT-2) inhibitors were invented[4]. So the study of natural products is expected to open the door for the development of novel drugs in the modern management of diabetes in the future.
Nevertheless, some areas of concern need to be addressed while using herbal products. These are the potential side effects, drug interactions, lack of product standardization and increasing cost. A major obstacle in the amalgamation of herbal medicine in modern medical practices is the lack of clinical data on its safety and efficacy. There is a need to conduct randomized control trials (RCTs) comparing herbal drugs with existing oral hypoglycemic drugs (OHAs). There are about 400 medicinal plants claimed to have beneficial effect in DM. Many of those products have overall health benefits but minimal effect on hyperglycemia. Here in this mini-review, we focus on the anti-hyperglycemic effect of herbal products that are commonly used, along with the concerns stated above.
Two authors (Giri S and Roy A) conducted the initial search in both ‘PubMed database’, and ‘Google Scholar’ for relevant articles. The references of these articles were also searched for additional relevant studies. The keywords used in the search were: ‘Herbal Products’; ‘HbA1C’; ‘Natural treatment’; ‘phytochemicals’; ‘Fasting blood glucose’; ‘HOMA-IR’. Only publications in English language were included. Kamalanathan S, Naik D and Sahoo J selected the relevant articles to be included.
The prevalence of herbal medicine use among diabetes patients is reported to be as high as 58.5%[5]. Plant products have been used as herbal remedies individually or in formulations. GlycaCare-II is an herbal formulation supplement for subjects with DM that contains cinnamon, bitter melon, vijayasar, gurmar, jamun extract and a bioavailability enhancer piperine. Majeed et al[6] showed that this formulation has similar potential as metformin in the reduction of glycated hemoglobin (HbA1c) and fasting blood sugar (FBS). Diabecon, diasulin, and pancreatic tonics are similar formulated herbal drugs commonly available in market. However, one of the fundamental issues with these herbal formulations is that active ingredients are not precisely defined. But it is essential to define the active compounds to determine the therapeutic efficacy and standardization of a product.
Most commonly used plants in the formulated herbal drugs are cinnamon gurmar, cumin, black cumin, psyllium, sesame, barberry, aloe, vijayasar, bael, fenugreek, jamun, ginger, little gourd, neem, sweet potato, amla, bitter melons, garlic, turmeric, guduchi. Dose, efficacy, active molecules, cost of these herbal products are described in Table 1.
| Herbal product | Active molecule | Part of plant | Dose | FBS fall (mg/dL) | HbA1C fall (%) | Cost (Rs.) | Ref. |
| Cinnamon | Procyanidin type A polimer | Bark | 0.5-6 g | 2-111 | 0-1.2 | 811/400 g | [8,11] |
| Gurmar | Gymnemic acid | Leaf | 0.4-10 g | 6-81 | 0.3-1.5 | 799/60 cap | [15,16] |
| Cumin | Thymoquinone | Seed | 0.1-0.5 g | 3-56 | 1-1.8 | 99/100 g | [17,18] |
| Psyllium | NA | Husk | 6.8-10.5 g | 20-53 | 1-1.6 | 105/100 g | [21,22] |
| Sesame | Sesamine | Seed | 0.2 g or 30 mL | 34-52 | 0.7-1.1 | 399/1 kg | [24,25] |
| Barberry | Berberine | Root, stem, bark | 0.9-1.5 g | 57-68 | 1.4-1.9 | 810/60 cap | [28] |
| Aloe | Acemannan | Leaf | 600-1000 g | 13-44 | 0.4-0.7 | 121/100 g | [29] |
| Vijayasar | Epicatechin | Bark | 1-4 g | 32-43 | 0.4 | 365/1 kg | [30] |
| Fenugreek | 4-OH isoleucin | Seed | 1-100 g | 15-41 | 0.2-1.5 | 199/200 g | [31,32] |
| Bael | Aegeline | Seed, leaf, fruit pulp | 5-20 g | 34-41 | 1.9 | 325/400 g | [34,35] |
| Jamun | Gallic acid | Seed | 10 g | 18-33 | 0.4-0.6 | 265/250 g | [37] |
| Ginger | Gingerol, shogaol | Rhizome | 1.6-2 g | 10-29 | 0.04-1.1 | 400/300 g | [38] |
| Little gourd | Pectin | Leaf, fruit | 0.5-1 g | 20-25 | 0.6-0.7 | NA | [42] |
| Neem | Nimbidiol | Root, bark | 1 g | 23 | 1.5 | 119/100 g | [44] |
| Sweet potato | Anthocyanins | Leaf, tuber | 4 g | 10-19 | 0.2-0.3 | NA | [45] |
| Amla | Gallic acid | Fruit | 0.5-10 g | 13-15 | 0.4-0.5 | 209/200 g | [46,47] |
| Bitter melon | Momordin, charantin | Whole plant | 0.8-4 g | 5-15 | 0.3 | 399/500 g | [51] |
| Garlic | Allicin | Bulb | 0.9-1.5 g | 4-10 | 0.2-0.8 | 485/400 g | [54] |
| Turmeric | Curcumin | Rhizome | 0.5-2.1 g | 2-9 | 0.02-0.9 | 599/500 g | [55] |
| Guduchi | Palmatine | Stem | 0.5-1.5 g | 5-8 | 0.2-0.5 | 150/60 cap | [57] |
| Jack fruit | Proanthocyanidin, flavonoids | Leaf | 30 g | 29 | 0.25 | 266/400 g | [62] |
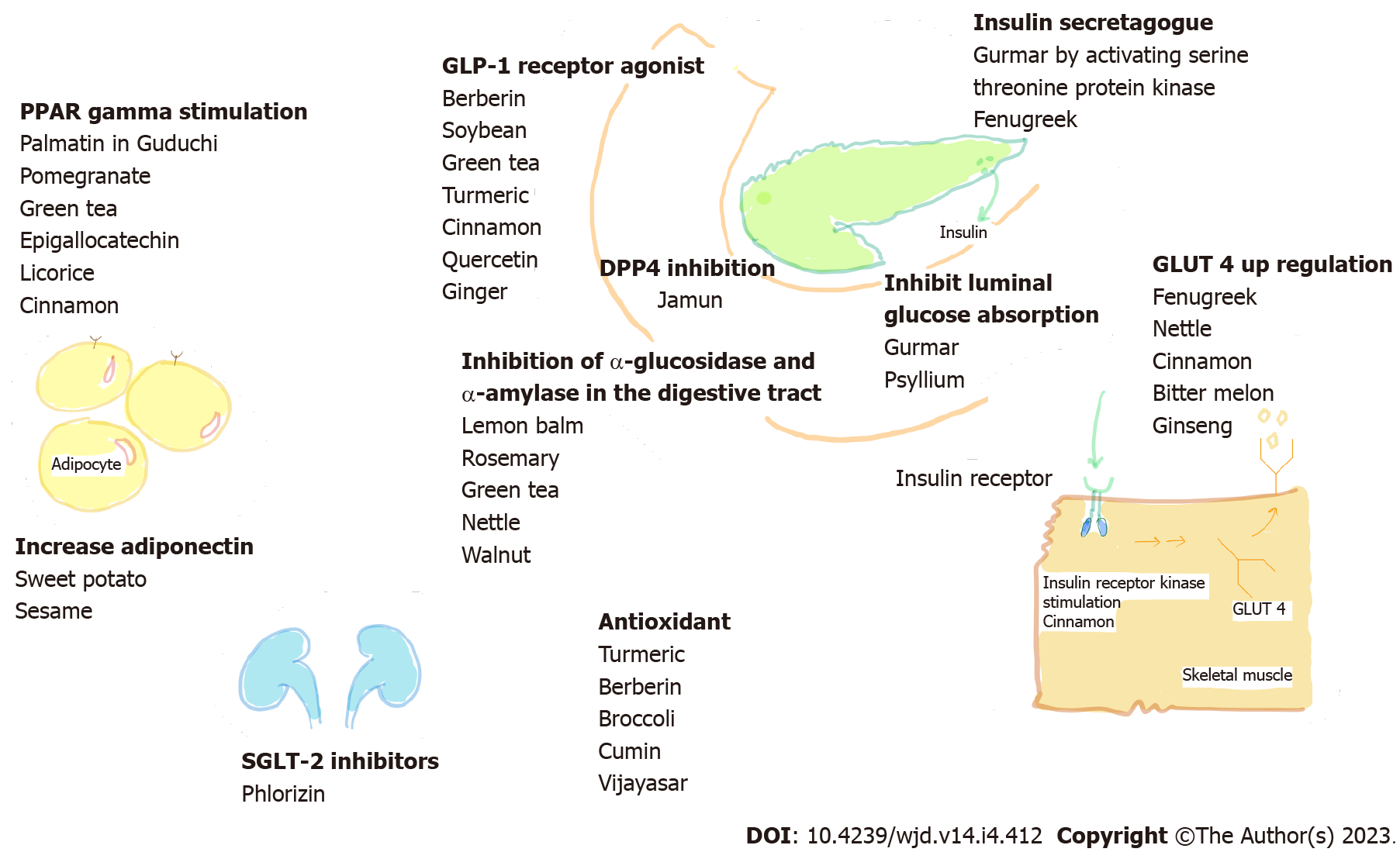
Active compound of great interest are quercetin, palmatin, berberin, gymnemic, gurmarin, phlorizin, kaempferol, rosmarinic acid, cyanidin, rutin, catechin and ellagic acid[7]. Various natural products of plant origin have been reported to target on multiple sites (Figure 1).
These are discussed in a decreasing order of their efficacy.
Cinnamon's dried bark is used as a spice for many recipes. Since time immemorial, it has been an essential traditional medicine against diabetes. Its bark powder is sold in the hard gelatine capsule formulation. Sharma et al[8] from India, in a double blind RCT, studied the effect of 3 g and 6 g of cinnamon powder in 150 newly diagnosed diabetes individuals who were OHA naïve. Over 3 mo, significant glycemic control status (mean FBS fall 111 mg/dL and mean HbA1c fall 1.2%) was achieved in the cinnamon group. Similarly, a study from Iran compared the effect of cinnamon powder with probiotics (Lactobacillus acidophilus) on blood glucose in 136 patients[9]. A significant drop in FBS (33 mg/dL) was observed in them who consumed both cinnamon powder and probiotics. It is possible that cinnamon brings out the effect by modification of gut microbiome because its active ingredient cinnamaldehyde has anti-microbial properties.
On the contrary, a significant effect on blood glucose (fall by 11 mg/dL) was not observed in another Iranian RCT where 3 g of cinnamon powder was used over a period of 2 mo[10]. Similarly, Hasanzade et al[11] concluded that 1 g of cinnamon had no effect compared to placebo on glycemic control over one month. The heterogeneity of these results might be due to the variable duration of follow-up or due to differences in ethnicity and body composition of study participants. A study was designed to evaluate the glucose lowering efficacy of cinnamon with different body mass index (BMI) where 140 diabetes patients were randomly assigned to 4 groups: Cinnamon (BMI ≥ 27, BMI < 27) and placebo (BMI ≥ 27, BMI < 27)[12]. At the end of 3 mo, glycemic outcomes were significantly more prominent (FBS fall by 20 mg/dL vs 6 mg/dL, P < 0.001) in patients with higher BMI in cinnamon group. When adjusted for BMI, visceral fat and homeostatic model assessment for insulin resistance (HOMA-IR) index by univariate model analysis, it was evident that glycemic outcomes were mediated through the decrement in insulin resistance. Therefore, it can be concluded that cinnamon has an antidiabetic effect. It acts though modification of gut microbiota and more of use in patients with higher BMI.
It is a perennial climber found in India and Africa. Various studies used 0.4-10 g/d gymnema leaf powder. It is available in tablet or capsule form. Its active compound, gymnemic acid is believed to block glucose absorption in the small intestine[13]. Gurmarin, another molecule in this product, has anti-sweetener activity. Li et al[14] from Pakistan demonstrated the effect of 1g powder on 32 middle aged diabetic patients in a non-randomized trial. After one month, mean FBS decreased by 81 mg/dL. Fall in HbA1C ranges from 0.32% to 1.57% in different studies[15,16].
The effect of 100-500 mg of cumin on FBS reduction ranges from 3 mg/dL to 56 mg/dL[17,18]. The formulation used are oil or powder form. On the other hand, 2-3 g of black cumin powder can reduce FBS by 17-23 mg/dL and HbA1C by 0.3%-0.6%[19,20]. Both types of cumin have thymoquinone as their active component which acts as an antioxidant.
Psyllium husk 6.8-10.5 g/d consumption reduces FBS from 20-53 mg/dL and HbA1C from 1%-1.6% with a significant decrement of insulin resistance (HOMA-IR reduction of 5.5)[21,22]. In a meta-analysis by Xiao et al[23], there were no major side effects on psyllium consumption. Water soluble fiber makes a barrier in the intestine for the absorption of glucose and other reducing sugars. It also influences release of various gut peptide, especially ghrelin and peptide YY and insulin. Alteration of gut flora is another possible mechanism that helps to control hyperglycemia. As in most of the studies, psyllium is found to have a consistent effect on glycemic control, which can be considered a good alternative for diabetes management.
The active compound is sesamine. FBS reduction ranges from 34 mg/dL to 52 mg/dL[24]. HbA1C reduction ranges from 0.7%-1.1%[25]. Dose of sesame used in various studies is 200 mg/d. Sesame oil consumption favorably changes insulin resistance, despite its modest effect on FBS. Although canola oil consumption increases FBS, when both oils are mixed for cooking, the beneficial effects of sesame oil is retained[26]. A blend of 20% cold-pressed un-refined sesame oil and 80% physically refined rice bran oil as cooking oil also lowered hyperglycemia and improved the lipid profile in a study by Devarajan et al[27]. Moreover, the combination of sesame oil blend and glibenclamide treatment in these patients significantly improved hyperglycemia.
The hypoglycemic effect of berberine was reported in 1988 when it was used to treat diarrhoea in diabetes patients in China. It is found in the roots, rhizomes, stems and bark of berberis. In a study on 36 diabetes patients, Yin et al[28] showed that the hypoglycemic effect of berberine (HbA1C fall 1.4%, FBS fall 68 mg/dL, PPBS fall 158 mg/dL) was similar to that of metformin (HbA1C fall 1.9, FBS fall 57 mg/dL, PPBS fall 138 mg/dL) over 3 mo of treatment. Usual dose of berberine 500 mg TID sometimes causes abdominal discomfort but, 300 mg TID is a well-tolerated dose.
It is a houseplant. Aloe vera gel is prepared from the leaf pulp. Aloe juice is an exudate from the outer skin of the leaves. And 600 to 1000 g of gel powder brings about 6-44 mg/dL fall in FBS and 0.4% to 0.7% fall in HbA1C[29]. The active compound acemannan is a mucopolysaccharide.
It is found as a component of many herbal products. The dose is 1-4 g of bark powder. A flexible dose open trial by Indian Council of Medical Research[30], 2-4 g/d Vijayasar, brought down blood glucose to the target range in 67 (69%) of 97 patients by 3-mo treatment. FBS, PPBS and HbA1c were decreased by 32 mg/dL, 45 mg/dL and 0.4%, respectively. No side effects were reported. In an RCT by Maurya et al[29], efficacy of aloe vera, vijayasar and their combination was compared to 1 mg of glimepiride. It was found that aloe (FBS reduction by 43 mg/dL) and vijayasar (by 43 mg/dL) showed synergism (by 54 mg/dL) for blood glucose control, but they were inferior to glimepiride (by 72 mg/dL). Its active principle epicatechin augments insulin release by increasing the cyclic adenosine monophosphate level. Flatulence has been reported; otherwise it is safe. It can be concluded that supplementation of 4g powder can be considered for the treatment diabetes.
It is a short lived plant and used for texture, flavor and color of food. Its health-promoting effect is outlined in Ayurvedic medicine. Usual dose is 1-100 g of seed extract powder. Its active compound amino acid 4-hydroxy isoleucine stimulates glucose induced insulin secretion from the perfused pancreas in vitro. The human trial showed a decrease in FBS range from 15 to 41 mg/dL, a decrease in HbA1C from 0.2% to 1.46% and HOMA-IR from 0.44 to 0.68. Singh et al[31] from India compared 500 mg fenugreek with 5 mg glipizide in 60 diabetes patients. The patients were randomized into three groups. They received either fenugreek seed extract 500 mg twice a day, glipizide 5 mg once daily, or a combination of glipizide 2.5 mg and fenugreek seed extract 500 mg once daily for 3 mo. It was found that both had significant effect on glycemic control. Glipizide monotherapy was more efficacious (mean FBS fall 58 mg/dL) in controlling hyperglycema than fenugreek monotherapy (mean FBS fall 41 mg/dL). However, it is fenugreek which reduced glycemia and dyslipidemia simultaneously and so this plant deserves a place in the management of metabolic syndrome. Another RCT from China[32] showed that 2 g of fenugreek powder when added to patients with uncontrolled blood glucose who were already on sulfonylurea for more than one year can further reduce the mean FBS by 33 mg/dL and HbA1C by 1.46%. Similarly, when added to metformin, it can further reduceblood glucose by 10 mg/dL[33]. Indeed it can be an add-on remedy for DM.
In an RCT by Yaheya and Ismail[34], fenugreek seed powder 20 g (FG) and dried bael leave powder 5 g (BL) were compared with OHA. Four groups were set up. Groups 1 to 4 received FG, BL, FG+BL and OHA, respectively. After 4 mo, PPBS was compared to baseline. The highest reduction in glucose was observed in those patients who received a combination of FG and BL, suggesting that these two products may have a synergistic effect. BL showed a comparable reduction in PPBS to standard OHA. Similarly, an RCT from India showed that 20 g of bael leaf juice can reduce glucose by 34 mg/dL when added to OHA treatment over 2 mo[35]. Its active molecule, aegeline is proposed to upregulate the translocation of glucose transporter type 4 (GLUT 4). These results clearly indicate that bael is an inexpensive dietary supplement that has potential to improve glycemic control.
In India, its kernel is used as household remedy for diabetes. Gallic acid and other phenolic compounds in Jamun are responsible for its anti-glycemic effect. Its seed, leaf, stem bark and fruit are used as herbal medicine. In an open labeled RCT by Acharya et al[36], 10 g of jamun seed powder was compared with 500 mg metformin in 30 newly diagnosed type 2 DM patients over 6 mo. Jamun reduced mean FBS by 18 mg/dL and HbA1C by 0.4%, whereas metformin reduced them by 41 mg/dL and 1.4%, respectively. Fall in PPBS was not significant. Another RCT from India showed that jamun, when added to the existing OHA, brought about a significant reduction in both FBS (33 mg/dL) and PPBS (43 mg/dL) over 3 mo[37]. In most of the trials, leaves and seeds of jamun were used for the treatment of diabetes. In contrast, tea extracts prepared from the leaves did not show a hypoglycaemic effect.
Its active compound gingerol and shogaol is thought to have antiglycemic property. It is claimed to have three significant properties-immunomodulatory, anticancer, and anti-inflammatory. A number of RCTs were performed to show its effect on blood glucose, but most of them show a modest reduction in glycemic parameters. Carvalho et al[38] showed that consumption of ginger powder 1.2 g/d over 3 mo can reduce mean FBS by 29 mg/dL. Similarly, an RCT by Makhdoomi Arzati et al[39] showed mean FBS reduction by 26 mg/dL and HbA1C reduction by 0.4% by 2 g of ginger powder in 10 wk. When added to standard treatment, 3 g powder of ginger decreased FBS by a further 19 mg/dL and HbA1C by 0.7% over 3 mo[40]. Although these results are encouraging, Mahluji et al[41] found that 2 g of ginger did not produce any effect on FBS and HbA1C but reduced serum insulin resistance over 2 mo.
It is an edible perennial vegetable. It has been widely used as an ingredient in traditional herbal medicine for the treatment of several diseases, including DM. Its leaf and fruit extract is formulated as a natural therapy. Several trials have shown that 500 mg to 1000 mg of coccinia powder can have a moderate glucose lowering effect. Wasana et al[42] found a reduction in insulin resistance along with a reduction of glycemic parameters (mean FBS by 25 mg/dL, mean HbA1C by 0.6%). Active compound pectin, triterpenes are responsible for its effect on blood glucose.
Neem is considered a miraculous tree for its medicinal effects. It is rich in alkaloids, flavonoids and terpenoids. Its root and stem bark contain nimbidiol, which is a diterpenoid that causes intestinal disaccharidase and glucoamylase inhibition[43]. Pingali et al[44] included 80 diabetes patients who were on metformin. Neem extract was prepared from its leaves and twigs and patients were randomly assigned to take capsules of 250 mg, 500 mg and 1000 mg of this extract. After 3 mo, significant reduction in FBS (23 mg/dL), HbA1C (1.5%) and HOMA-IR (2.6%) was noticed in the 1000 mg group. It can certainly be a weapon to combat DM as a herbal product.
This plant is native to the tropical and subtropical belts. Apart from cooking, it is also used in traditional medicine for DM. Its active compounds are isolated from leaves and tuber. It is rich in anthocyanins, polyphenols and flavonoids. Ludvik et al[45] have shown that 4 g powder of sweet potato can reduce FBS from 10 to 19 mg/dL and reduce HbA1C by 0.21% - 0.3%.
Various studies used 1-10 g of amla powder. The average fall in FBS is 13 mg/dL and fall in HbA1C is 0.5%[46,47]. Active compounds are gallic acid, ellagic acid, quercetin, and chebulinic acid[48]. Triphala, a combination of amla, haritaki and bibhitaki, is considered to have a pleiotropic effect in ayurvedic medicine. Nevertheless, a systematic review by Phimarn et al[49] fails to establish any effect on blood glucose.
It is commonly used as an alternative therapy for the treatment of diabetes. Different doses (from 800 mg to 6 g/d) and different parts of this plant such as leaves, fruit pulp, seeds and whole plant have been studied for antidiabetic effect. Momordin and charantin are active compounds. Kim et al[50] conducted an RCT with 2.3 g of bitter melon powder on 96 diabetic subjects. At the end of 3 mo, the mean FBS reduction was only 5 mg/dL without any significant impact on other glycemic parameters. An open-label, randomized, active-controlled, multicentric, phase III study from India[51] compared 800 mg bitter melon fruit extract with metformin. Eighty-three subjects received bitter melon and 40 subjects received metformin. After 15 wk, mean fall in FBS and HbA1C in the bitter melon group was 14 mg/dL and 0.28% and in the metformin group 25 mg/dL and 0.62%, respectively. This study showed non-inferiority of bitter melon to metformin, although its effects were modest. Similarly, a weaker antidiabetic effect has been exhibited in comparison to glibenclamide 5 mg in a trial by Rahman et al[52].
Since antiquity, garlic has been part and parcel of many Indian dishes and herbal medicine. Garlic powder is formulated in capsule form. It has allicin, a sulfur-containing amino acid that can combine with cysteine and other sulphydryl group containing amino acids and spares insulin from inactivation[53]. Kumar et al[54] demonstrated that garlic, when added to metformin treatment, helps in further blood glucose reduction, although the effect is insignificant. Reduction of glycemia is modest in various studies.
Turmeric is used in food preparation as a spice. It has versatile pharmacological effects described by both in vitro and in vivo studies. Its bioactive molecule is curcumin which is present in the rhizome of this plant. Its active peroxisome proliferator-activated receptor gamma (PPAR-γ) is similar to thiazolidinedione. Despite its efficacy in in vitro studies, human trials fail to document any significant effect. Its bioavailability is a major hindrance to its efficacy. FBS reduction ranges from 2 to 9 mg/dL. The commonly used dose is 450-2100 mg/d[55].
A study on water extract or powder form of a mature stem of tinospora by Roy[56] and Mishra et al[57] demonstrated that 500-1500 mg capsule can reduce FBS by 5-8 mg/dL and HbA1C by 0.22%-0.54%. Its active compound, palmatine, is known to stimulate PPAR-γ).
The discovery of novel SGLT-2 inhibitors dates back to 1835 when phlorizin was isolated for the first time from the barks of an apple tree by French chemists[58]. It is mainly found in the young shoots, roots, leaves and barks of the apple tree, while in fruit, it is most abundant in the seeds. Nevertheless, seeds of ripe fruit contain a toxic cyanogenic glycoside[59], so seeds of unripe fruit seeds are to be used. Apple, as an intact fruit, does not have glucose-lowering properties. Moreover, the bioavailability of natural phlorizin is less as it is hydrolyzed by lactase-phlorizin hydrolase in the brush border of the small intestine. Apart from the apple tree, quercetin, strawberry, rose hip and pear have phenolic components with SGLT-2 inhibitory effects. When consumed as food item, these may not bring about a reasonable effect due to the presence of carbohydrates within these fruits.
Its root extract has been used widely in Chinese medicine as antidiabetic therapy. However, evidence is not sound in human studies[60]. The active compound is glycyrrhizic acid. Due to its 11-beta hydroxysteroid dehydrogenase-2 enzyme inhibitory property, it can cause hypokalemia, hypertension and rhabdomyolysis[61].
Rao et al[62] from India demonstrated the effect of jack fruit leaf flour on 40 diabetes patients in a RCT. They found that replacing an equal volume of wheat flour in daily meals with jackfruit flour could significantly lower the blood glucose level (mean FBS by 29 mg/dL, and mean HbA1C by 0.25%)[62]. However this finding needs confirmation by further RCTs.
An ayurvedic hypoglycemic formulation consisting of seeds of mango, seeds of bitter melon, seeds of jamun, and leaves of gurmar were tried in fairly large sample size (n = 350), which revealed a statistically significant reduction in blood glucose levels in DM[63]. A polyherbal formulation named BGR-34 was developed by the Council of Scientific and Industrial Research, Government of India.
Similarly, nettle, pomegranate, shilajit, beans, tea, ginkgo biloba, saffron lack sufficient clinical data in diabetes management although these are cited as antihyperglycemic medicine in Ayurveda. Central Council for Research in Ayurvedic Sciences recommends certain fruits and vegetables for diabetes patients. Those are fenugreek, bitter melon, garlic, unripe banana, jamun, amla, pomegranate, bael, guava, apple, and orange.
In common belief, herbal products are regarded to be very safe to consume. This is because most previous trials did not monitor side effects. This is a myth. We know about Chinese herb nephropathy due to aristolochia used for obesity. Among antidiabetic drugs, ginseng can cause insomnia, anxiety, and hypertension. Due to its estrogenic effects, it can cause breast tenderness and vaginal bleeding. Garlic, fenugreek, cinnamon and ginger can cause increased bleeding tendency due to the presence of a coumarin like compound. Aloe can also prolong bleeding time[64]. So these products must be stopped if the patient is on anticoagulants or patient plans an operation. Gastrointestinal side effects are quite common with ingestion of these natural products. Apart from these, fenugreek can also cause facial swelling and itching. As it contains mucilage, absorption of other drugs can be compromised. Both fenugreek and bitter melon are contraindicated in pregnancy. Alfa and beta momorcharin in bitter melon have abortifacient effect[65]. On the other hand, neem products have contraceptive property[66]. Bitter melon has been reported to cause hemolytic anemia in glucose 6 phosphate dehydrogenase deficient individuals (due to presence of vicine) and convulsion in children[65]. Side effects of amla are mild headache, fever, gastritis and increased bleeding tendency[67]. Aloe vera, turmeric, and ginseng have Cytochrome P450 (CYP) enzyme-inducing or inhibitory properties. Particularly, aloe vera can inhibit CYP3A4 and CYP2D6; thereby, it has the potential to alter levels of pioglitazone and repaglinide[68]. Similarly, consumption of neem can reduce the bioavailability of glipizide. Turmeric can inhibit P-glycoprotein 1, which is an efflux pump, and thereby increases glyburide concentration[69]. So intake of these products may lead to significant drug interaction.
Product standardization of these herbal formulations is not tightly regulated. Unlike allopathic medicines, herbal products are obtained from nature. The chemical composition of these herbs may alter based on the season and growing conditions. For example, ginsenoid, the active moiety in ginseng, varies from 36% to 112%[70]. Herbal medicine sold in India as antidiabetic remedy was found to contain glibenclamide as an adulterant[71]. Bioassays need to be developed for biological standardization and toxicological assessment. Many a time, heavy metals are found in various ayurvedic products much are above their acceptable range[72]. All these need to be considered before using those.
Even though these products are readily available, processed plant products sold in the market in the proper formulation are costly. Cost of the products based on the price mentioned in Amazon online shopping app. at the time of writing of the article are mentioned in Table 1. The most popular drug metformin is a cheap drug. On head-to-head comparison studies with a low dose of metformin, it is evident that most of these products are inferior to metformin. Therefore cost-effectiveness has to be considered before consuming those.
Although many OHAs in modern medicine have a natural origin, consuming them in their original form may not bring out much benefit as we have discussed with the example of metformin. On the other hand, we have seen isolation of phlorizin paved the way to the discovery of modern SGLT 2 inhibitors. It is worth to find out the active molecule and their mechanisms of action not only for a better understanding of their effects but also for product standardization.
DM is a chronic disease and it is associated with multiple comorbidities. So, its remedies should be chosen wisely based on the data on their safety, efficacy and drug interactions. In this article, we have given an overview of herbal products with anti-hyperglycaemic effects based on various RCTs. We often use them as food items but in sub-optimal doses. We have also mentioned doses and proper formulation from the right part of the plant used in various clinical trials. Nonetheless, these trials of natural products often underreport the important steps of the interventions, thereby deviate from the standards set by Consolidated Standards of Reporting Trials. These need to be brought under a regulatory framework which will eventually generate faith in these herbal medicines. Last but not the least, cost-effectiveness should also be kept in mind before using them.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ariyachet C, Thailand; Zeng Y, China S-Editor: Gao CC L-Editor: Ma JY-MedE P-Editor: Gao CC
| 1. | Holt RIG, Cockram CS, Flyvbjerg A, Goldstein BJ. Textbook of Diabetes. 5th ed. John Wiley & Sons, Inc., 2017. [Cited in This Article: ] |
| 2. | Bailey CJ. Metformin: historical overview. Diabetologia. 2017;60:1566-1576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 451] [Cited by in F6Publishing: 495] [Article Influence: 70.7] [Reference Citation Analysis (0)] |
| 3. | Matsuo T, Odaka H, Ikeda H. Effect of an intestinal disaccharidase inhibitor (AO-128) on obesity and diabetes. Am J Clin Nutr. 1992;55:314S-317S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 78] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Rieg T, Vallon V. Development of SGLT1 and SGLT2 inhibitors. Diabetologia. 2018;61:2079-2086. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 152] [Cited by in F6Publishing: 185] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 5. | Kifle ZD, Bayleyegn B, Yimer Tadesse T, Woldeyohanins AE. Prevalence and associated factors of herbal medicine use among adult diabetes mellitus patients at government hospital, Ethiopia: An institutional-based cross-sectional study. Metabol Open. 2021;11:100120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 8] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 6. | Majeed M, Majeed A, Nagabhusahnam K, Mundkur L, Paulose S. A randomized, double-blind clinical trial of a herbal formulation (GlycaCare-II) for the management of type 2 diabetes in comparison with metformin. Diabetol Metab Syndr. 2021;13:132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Egbuna C, Awuchi CG, Kushwaha G, Rudrapal M, Patrick-Iwuanyanwu KC, Singh O, Odoh UE, Khan J, Jeevanandam J, Kumarasamy S, Chukwube VO, Narayanan M, Palai S, Găman MA, Uche CZ, Ogaji DS, Ezeofor NJ, Mtewa AG, Patrick-Iwuanyanwu CC, Kesh SS, Shivamallu C, Saravanan K, Tijjani H, Akram M, Ifemeje JC, Olisah MC, Chikwendu CJ. Bioactive Compounds Effective Against Type 2 Diabetes Mellitus: A Systematic Review. Curr Top Med Chem. 2021;21:1067-1095. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 63] [Article Influence: 21.0] [Reference Citation Analysis (1)] |
| 8. | Sharma P, Sharma S, Agrawal R, Agarwal V, Singhal S. A randomised double blind placebo control trial of cinnamon supplementation on glycemic control and lipid profile in type 2 diabetes mellitus. Australian J Herbal Med. 2012;24:108-119. [Cited in This Article: ] |
| 9. | Mirmiranpour H, Huseini HF, Derakhshanian H, Khodaii Z, Tavakoli-Far B. Effects of probiotic, cinnamon, and synbiotic supplementation on glycemic control and antioxidant status in people with type 2 diabetes; a randomized, double-blind, placebo-controlled study. J Diabetes Metab Disord. 2020;19:53-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Talaei B, Amouzegar A, Sahranavard S, Hedayati M, Mirmiran P, Azizi F. Effects of Cinnamon Consumption on Glycemic Indicators, Advanced Glycation End Products, and Antioxidant Status in Type 2 Diabetic Patients. Nutrients. 2017;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 11. | Hasanzade F, Toliat M, Emami SA, Emamimoghaadam Z. The Effect of Cinnamon on Glucose of Type II Diabetes Patients. J Tradit Complement Med. 2013;3:171-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Zare R, Nadjarzadeh A, Zarshenas MM, Shams M, Heydari M. Efficacy of cinnamon in patients with type II diabetes mellitus: A randomized controlled clinical trial. Clin Nutr. 2019;38:549-556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 13. | Kanetkar P, Singhal R, Kamat M. Gymnema sylvestre: A Memoir. J Clin Biochem Nutr. 2007;41:77-81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | Li Y, Zheng M, Zhai X, Huang Y, Khalid A, Malik A, Shah P, Karim S, Azhar S, Hou X. Effect of-gymnema sylvestre, citrullus colocynthis and artemisia absinthium on blood glucose and lipid profile in diabetic human. Acta Pol Pharm. 2015;72:981-985. [PubMed] [Cited in This Article: ] |
| 15. | Baskaran K, Kizar Ahamath B, Radha Shanmugasundaram K, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol. 1990;30:295-300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 184] [Cited by in F6Publishing: 142] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Shanmugasundaram ER, Rajeswari G, Baskaran K, Rajesh Kumar BR, Radha Shanmugasundaram K, Kizar Ahmath B. Use of Gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J Ethnopharmacol. 1990;30:281-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 103] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Hendre A, Sontakke A, Phatak R, Patil S, Jadhav S. Role of Cumin in Management of Type 2 Diabetes Mellitus with respect to its Antidiabetic and Antioxidant Property. Int J Res Pharm Sci. 2020;11:4157-4161. [DOI] [Cited in This Article: ] |
| 18. | Jafari S, Sattari R, Ghavamzadeh S. Evaluation the effect of 50 and 100 mg doses of Cuminum cyminum essential oil on glycemic indices, insulin resistance and serum inflammatory factors on patients with diabetes type II: A double-blind randomized placebo-controlled clinical trial. J Tradit Complement Med. 2017;7:332-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Kaatabi H, Bamosa AO, Badar A, Al-Elq A, Abou-Hozaifa B, Lebda F, Al-Khadra A, Al-Almaie S. Nigella sativa improves glycemic control and ameliorates oxidative stress in patients with type 2 diabetes mellitus: placebo controlled participant blinded clinical trial. PLoS One. 2015;10:e0113486. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 20. | Najmi A, Nasiruddin M, Khan R, Haque SF. Therapeutic effect of Nigella sativa in patients of poor glycemic control. Asian J Pharm Clin Res. 2012;5:224-228. [DOI] [Cited in This Article: ] |
| 21. | Ziai SA, Larijani B, Akhoondzadeh S, Fakhrzadeh H, Dastpak A, Bandarian F, Rezai A, Badi HN, Emami T. Psyllium decreased serum glucose and glycosylated hemoglobin significantly in diabetic outpatients. J Ethnopharmacol. 2005;102:202-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Abutair AS, Naser IA, Hamed AT. Soluble fibers from psyllium improve glycemic response and body weight among diabetes type 2 patients (randomized control trial). Nutr J. 2016;15:86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Xiao Z, Chen H, Zhang Y, Deng H, Wang K, Bhagavathula AS, Almuhairi SJ, Ryan PM, Rahmani J, Dang M, Kontogiannis V, Vick A, Wei Y. The effect of psyllium consumption on weight, body mass index, lipid profile, and glucose metabolism in diabetic patients: A systematic review and dose-response meta-analysis of randomized controlled trials. Phytother Res. 2020;34:1237-1247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Aslam F, Iqbal S, Nasir M, Anjum AA. White Sesame Seed Oil Mitigates Blood Glucose Level, Reduces Oxidative Stress, and Improves Biomarkers of Hepatic and Renal Function in Participants with Type 2 Diabetes Mellitus. J Am Coll Nutr. 2019;38:235-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Mohammad Shahi M, Zakerzadeh M, Zakerkish M, Zarei M, Saki A. Effect of Sesamin Supplementation on Glycemic Status, Inflammatory Markers, and Adiponectin Levels in Patients with Type 2 Diabetes Mellitus. J Diet Suppl. 2017;14:65-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 26. | Raeisi-Dehkordi H, Amiri M, Zimorovat A, Moghtaderi F, Zarei S, Forbes SC, Salehi-Abargouei A. Canola oil compared with sesame and sesame-canola oil on glycaemic control and liver function in patients with type 2 diabetes: A three-way randomized triple-blind cross-over trial. Diabetes Metab Res Rev. 2021;37:e3399. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Devarajan S, Chatterjee B, Urata H, Zhang B, Ali A, Singh R, Ganapathy S. A Blend of Sesame and Rice Bran Oils Lowers Hyperglycemia and Improves the Lipids. Am J Med. 2016;129:731-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 28. | Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57:712-717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 462] [Cited by in F6Publishing: 469] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 29. | Maurya AK, Jain A, Pathak A, Chaudhary P, Rajdan N. Efficacy of vijaysar, aloevera alone and their combination in the treatment of newly diagnosed cases of type 2 diabetes mellitus: a randomized single blind prospective study. Int J Basic Clin Pharmacol. 2017;6:962-967. [DOI] [Cited in This Article: ] |
| 30. | Flexible dose open trial of Vijayasar in cases of newly-diagnosed non-insulin-dependent diabetes mellitus. Indian Council of Medical Research (ICMR), Collaborating Centres, New Delhi. Indian J Med Res. 1998;108:24-29. [PubMed] [Cited in This Article: ] |
| 31. | Singh A, Rai J, Mahajan DS. Comparative evaluation of glipizide and fenugreek (Trigonella foenum-graecum) seeds as monotherapy and combination therapy on glycaemic control and lipid profile in patients with type 2 diabetes mellitus. Int J Basic Clin Pharmacol. 2016;5:942-950. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Lu FR, Shen L, Qin Y, Gao L, Li H, Dai Y. Clinical observation on trigonella foenum-graecum L. total saponins in combination with sulfonylureas in the treatment of type 2 diabetes mellitus. Chin J Integr Med. 2008;14:56-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 33. | Kaur M, Singh N, Sharma G, Singh D. To study the efficacy and tolerability of fenugreek seed powder as add-on therapy with metformin in patients of type-2 diabetes mellitus. Int J Basic Clin Pharmacol. 2016;5:378-383. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Yaheya M, Ismail M. Clinical Evaluation of Antidiabetic Activity of Trigonella Seeds and Aegle marmelos Leaves. World Appl Sci J. 2009;7:1231-1234. [DOI] [Cited in This Article: ] |
| 35. | Nigam V, Nambiar VS. Aegle marmelos leaf juice as a complementary therapy to control type 2 diabetes – Randomised controlled trial in Gujarat, India. Adv Integr Med. 2019;6:11-22. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Acharya S, Shivaprakash G, Baliga R, Adhikari P, Jyothi G, Pai MRSM. Effect of Eugenia jambolana on plasma glucose, insulin sensitivity and HDL-C levels: preliminary results of a randomized clinical trial. J Pharm Res. 2010;3:1268-1270. [DOI] [Cited in This Article: ] |
| 37. | Sidana S, Singh VB, Meena BL, Beniwal S, Singh K, Kumar D, Singla R. Effect of Syzygium cumini (jamun) seed powder on glycemic control: A double-blind randomized controlled trial. J Med Soc. 2017;31:185-189. [DOI] [Cited in This Article: ] |
| 38. | Carvalho GCN, Lira-Neto JCG, Araújo MFM, Freitas RWJF, Zanetti ML, Damasceno MMC. Effectiveness of ginger in reducing metabolic levels in people with diabetes: a randomized clinical trial. Rev Lat Am Enfermagem. 2020;28:e3369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 39. | Makhdoomi Arzati M, Mohammadzadeh Honarvar N, Saedisomeolia A, Anvari S, Effatpanah M, Makhdoomi Arzati R, Yekaninejad MS, Hashemi R, Djalali M. The Effects of Ginger on Fasting Blood Sugar, Hemoglobin A1c, and Lipid Profiles in Patients with Type 2 Diabetes. Int J Endocrinol Metab. 2017;15:e57927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 40. | Shidfar F, Rajab A, Rahideh T, Khandouzi N, Hosseini S, Shidfar S. The effect of ginger (Zingiber officinale) on glycemic markers in patients with type 2 diabetes. J Complement Integr Med. 2015;12:165-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 41. | Mahluji S, Attari VE, Mobasseri M, Payahoo L, Ostadrahimi A, Golzari SE. Effects of ginger (Zingiber officinale) on plasma glucose level, HbA1c and insulin sensitivity in type 2 diabetic patients. Int J Food Sci Nutr. 2013;64:682-686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 42. | Wasana KGP, Attanayake AP, Weerarathna TP, Jayatilaka KAPW. Efficacy and safety of a herbal drug of Coccinia grandis (Linn.) Voigt in patients with type 2 diabetes mellitus: A double blind randomized placebo controlled clinical trial. Phytomedicine. 2021;81:153431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 43. | Mukherjee A, Sengupta S. Characterization of nimbidiol as a potent intestinal disaccharidase and glucoamylase inhibitor present in Azadirachta indica (neem) useful for the treatment of diabetes. J Enzyme Inhib Med Chem. 2013;28:900-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 44. | Pingali U, Ali MA, Gundagani S, Nutalapati C. Evaluation of the Effect of an Aqueous Extract of Azadirachta indica (Neem) Leaves and Twigs on Glycemic Control, Endothelial Dysfunction and Systemic Inflammation in Subjects with Type 2 Diabetes Mellitus - A Randomized, Double-Blind, Placebo-Controlled Clinical Study. Diabetes Metab Syndr Obes. 2020;13:4401-4412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 45. | Ludvik B, Hanefeld M, Pacini G. Improved metabolic control by Ipomoea batatas (Caiapo) is associated with increased adiponectin and decreased fibrinogen levels in type 2 diabetic subjects. Diabetes Obes Metab. 2008;10:586-592. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 46. | Akhtar MS, Ramzan A, Ali A, Ahmad M. Effect of Amla fruit (Emblica officinalis Gaertn.) on blood glucose and lipid profile of normal subjects and type 2 diabetic patients. Int J Food Sci Nutr. 2011;62:609-616. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 47. | Usharani P, Fatima N, Muralidhar N. Effects of Phyllanthus emblica extract on endothelial dysfunction and biomarkers of oxidative stress in patients with type 2 diabetes mellitus: a randomized, double-blind, controlled study. Diabetes Metab Syndr Obes. 2013;6:275-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Huang HZ, Qiu M, Lin JZ, Li MQ, Ma XT, Ran F, Luo CH, Wei XC, Xu RC, Tan P, Fan SH, Yang M, Han L, Zhang DK. Potential effect of tropical fruits Phyllanthus emblica L. for the prevention and management of type 2 diabetic complications: a systematic review of recent advances. Eur J Nutr. 2021;60:3525-3542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 49. | Phimarn W, Sungthong B, Itabe H. Effects of Triphala on Lipid and Glucose Profiles and Anthropometric Parameters: A Systematic Review. J Evid Based Integr Med. 2021;26:2515690X211011038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 50. | Kim SK, Jung J, Jung JH, Yoon N, Kang SS, Roh GS, Hahm JR. Hypoglycemic efficacy and safety of Momordica charantia (bitter melon) in patients with type 2 diabetes mellitus. Complement Ther Med. 2020;52:102524. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 51. | Suthar AC, Pai VG, Kadam Y, Tongaonkar A, Kale S, Deshpande AB, Kolke S, Tanna S, Deshpande SV, Chawla P, Biswas D, Sharma S. Efficacy and Safety of PDM011011 Capsules as Compared to Metformin in Subjects with Type-2 Diabetes Mellitus: An Open-Label, Randomized, Active-Controlled, Multicentric, Phase III Study. J Diabetes Mellitus. 2016;6:38-48. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Rahman IU, Khan RU, Rahman KU, Bashir M. Lower hypoglycemic but higher antiatherogenic effects of bitter melon than glibenclamide in type 2 diabetic patients. Nutr J. 2015;14:13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 53. | Khan R. Effects of garlic on blood glucose levels and HbA1c in patients with type 2 diabetes mellitus. J Med Plant Res. 2011;5:2922-2928. [Cited in This Article: ] |
| 54. | Kumar R, Chhatwal S, Arora S, Sharma S, Singh J, Singh N, Bhandari V, Khurana A. Antihyperglycemic, antihyperlipidemic, anti-inflammatory and adenosine deaminase- lowering effects of garlic in patients with type 2 diabetes mellitus with obesity. Diabetes Metab Syndr Obes. 2013;6:49-56. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 55. | Adab Z, Eghtesadi S, Vafa MR, Heydari I, Shojaii A, Haqqani H, Arablou T, Eghtesadi M. Effect of turmeric on glycemic status, lipid profile, hs-CRP, and total antioxidant capacity in hyperlipidemic type 2 diabetes mellitus patients. Phytother Res. 2019;33:1173-1181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 56. | Roy K. Tinospora cordifolia stem supplementation in diabetic dyslipidemia: an open labelled randomized controlled trial. Funct Foods Health Dis. 2015;5:265-274. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 57. | Mishra S, Verma N, Bhattacharya S, Usman K, Himanshu D, Singh P, Anjum B. Effect of Tinospora cordifolia as an add - on therapy on the blood glucose levels of patients with Type 2 diabetes. Int J Basic Clin Pharmacol. 2017;4:537-541. [DOI] [Cited in This Article: ] |
| 58. | Ehrenkranz JR, Lewis NG, Kahn CR, Roth J. Phlorizin: a review. Diabetes Metab Res Rev. 2005;21:31-38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 655] [Cited by in F6Publishing: 613] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 59. | Lu Y, Yeap Foo L. Constitution of some chemical components of apple seed. Food Chem. 1998;61:29-33. [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 71] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Alizadeh M, Namazi N, Mirtaheri E, Sargheini N, Kheirouri S. Changes of Insulin Resistance and Adipokines Following Supplementation with Glycyrrhiza Glabra L. Extract in Combination with a Low-Calorie Diet in Overweight and Obese Subjects: a Randomized Double Blind Clinical Trial. Adv Pharm Bull. 2018;8:123-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Yang LY, Yin JH, Yang J, Ren Y, Xiang CY, Wang CY. Liquorice-induced severe hypokalemic rhabdomyolysis with Gitelman syndrome and diabetes: A case report. World J Clin Cases. 2019;7:1200-1205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 6] [Cited by in F6Publishing: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 62. | Rao AG, Naik KS, Unnikrishnan AG, Joseph J. Efficacy of green jackfruit flour as a medical nutrition therapy replacing rice or wheat in patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled study. Nutr Diabetes. 2021;11:18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Panda AK. Efficacy of Ayurveda Formulation Ayush-82 (IME-9) in Newly Diagnosed Type 2 Diabetics: Retrospective Analysis of Individual Data. J Tradit Med Clin Natur. 2017;6:250. [DOI] [Cited in This Article: ] |
| 64. | Lee A, Chui PT, Aun CS, Gin T, Lau AS. Possible interaction between sevoflurane and Aloe vera. Ann Pharmacother. 2004;38:1651-1654. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 65. | Basch E, Gabardi S, Ulbricht C. Bitter melon (Momordica charantia): a review of efficacy and safety. Am J Health Syst Pharm. 2003;60:356-359. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 244] [Cited by in F6Publishing: 253] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 66. | Patil SM, Shirahatti PS, V B CK, Ramu R, M N NP. Azadirachta indica A. Juss (neem) as a contraceptive: An evidence-based review on its pharmacological efficiency. Phytomedicine. 2021;88:153596. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 67. | Hashem-Dabaghian F, Ziaee M, Ghaffari S, Nabati F, Kianbakht S. A systematic review on the cardiovascular pharmacology of Emblica officinalis Gaertn. J Cardiovasc Thorac Res. 2018;10:118-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 68. | Djuv A, Nilsen OG. Aloe vera juice: IC₅₀ and dual mechanistic inhibition of CYP3A4 and CYP2D6. Phytother Res. 2012;26:445-451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 69. | Neerati P, Devde R, Gangi AK. Evaluation of the effect of curcumin capsules on glyburide therapy in patients with type-2 diabetes mellitus. Phytother Res. 2014;28:1796-1800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 70. | Vuksan V, Sievenpiper JL. Herbal remedies in the management of diabetes: lessons learned from the study of ginseng. Nutr Metab Cardiovasc Dis. 2005;15:149-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 71. | Kulambil Padinjakara RN, Ashawesh K, Butt S, Nair R, Patel V. Herbal remedy for diabetes: two case reports. Exp Clin Endocrinol Diabetes. 2009;117:3-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 72. | Saper RB, Phillips RS, Sehgal A, Khouri N, Davis RB, Paquin J, Thuppil V, Kales SN. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold via the Internet. JAMA. 2008;300:915-923. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 313] [Cited by in F6Publishing: 258] [Article Influence: 16.1] [Reference Citation Analysis (0)] |