Critical Incident Reported in an Obstetric Unit of a Tertiary Care Hospital of a Developing Country, over a Period of Two Years ()
1. Introduction
A critical incident is an incident that can be potentially harmful to a patient during anesthetic management [1] . A near miss in an event under anesthesia care can possibly lead to negative outcome if not intervened timely [2] . One of the methods of establishing and improving safety in our practice is reporting, sharing and discussing our mistakes, at some forum like Critical Incident reporting. Department of Anaesthesiology at Aga Khan University Hospital, Karachi, Pakistan has a critical incident reporting mechanism in place since 1996 [3] .
As health care is moving towards specialty and sub-specialty based practices all over the world. It needs to be incorporated in our set up as well and as a first step, we start critical incident reporting in labor room suite where twenty four hours anesthesia services are available for one elective, one emergency theatre and labor room epidurals. Empty forms are available in both operating rooms of the Labor room operation room (LROR). These are filled on a voluntary basis by the medical and paramedical staff anonymously and are periodically reviewed and presented in academic meetings to educate, to increase awareness and to standardize and formulate guidelines. Specialty based critical incident reporting is of value as it is easier to bring changes or improve the system in relatively small clinical areas with a small group of people like pediatric, obstetric, pain etc. Although literature of critical incident in anesthesiology in general is reported, no report from any obstetric unit was found in literature.
In this audit, our aim was to report critical incidents and near misses specifically during conduct of obstetric anesthesia in LROR of our hospital. The secondary objective was to evaluate the contributing factors of human error.
2. Methods
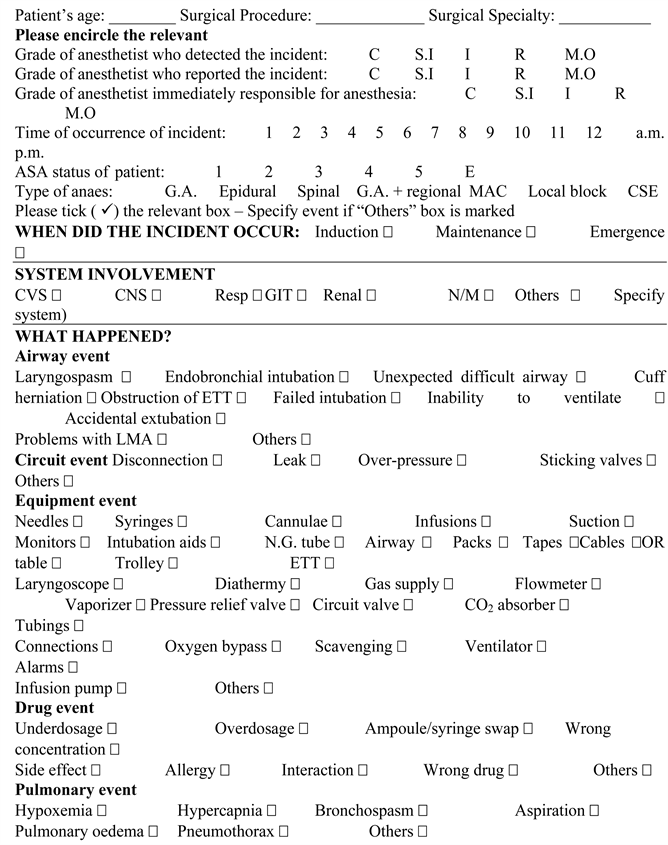
All reported incidents occurred in obstetric unit over a period of two years (July 2015 to June 2017) in labor room operation room of Aga Khan University Hospital. The forms are filled prospectively, voluntarily and anonymously in a predesigned critical incident form by anesthesia resident, medical officer and faculty (Appendix). All data variables on this form were entered in Statistical Package of Social Sciences Version 19.0 (SPSS). All forms were reviewed and all incidents were categorized on the basis of type of errors. The desired variables for this audit were segregated in a separate SPSS file. These were then reviewed and re-analyzed by primary investigator. The forms with incomplete contextual information were dealt separately. The following data was reviewed for all reports: surgical procedure, grade of anesthetist who reported the incident, American Society of Anesthesiologist (ASA) status, type of anesthesia, phase of anesthesia when the incident occurred, system involved, type of error, outcome and action taken. We included incidents where the patients encountered harm and “near misses” where the patients did not suffer harm but could have if left to progress. All consultants and trainees are encouraged to report by presenting the collected incidents at a given interval in our obstetric group meeting. The reports were classified as human, system, equipment or medication errors. Furthermore human errors were categorized on the basis of their contributing factors already present in the form. Human error is a social label which implies that the individual should have acted differently and thus is responsible for the consequence of that conduct. System error can be defined as an instruction that is either not recognized by an operating system or is in violation of the procedural rules. Equipment error includes faulty equipment. Medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer.
The following definitions were employed for the respective events: [4]
• Difficult tracheal intubation − >3 attempts
• Bradycardia/tachycardia − >20% deviation from baseline pulse rate
• Hypotension/hypertension − >30% deviation from baseline blood pressure
• Desaturation−SPO2 < 90%
• Difficult cannulation − >3 attempts
• Hypothermia-temperature < 35˚C
3. Results
During the review period 5511 anesthetics were administered and 55 critical incidents were reported. Two incidents happened in ward and labor room therefore excluded from our analysis. Henceforth, 53 reports were included in the analysis. Frequency, percentages and p-values were calculated.
Distribution of incidents reported was 20 and 33 critical incidents and near misses respectively. Forty one patients were ASA I and II. Incidents were reported more in elective patients (n = 40 p value < 0.05), during day time (08:00 a.m.-05:00 p.m.) (n = 47) and more frequently in patients who received regional anesthesia (n = 40 (75%)) (Table 1).
Twenty six out of 53 (49%) incidents occurred at induction of anesthesia and the rest during the pre-induction, maintenance, emergence and post anesthesia care unit.
For ease of understanding, the reports were first divided into critical incidents and near misses (33 + 20). Out of 33 critical incidents majority of the reported incidents involved the cardiovascular and musculoskeletal system (9 + 9 = 18 (54.5%)). Followed by neuromuscular system (n = 5), drug related incidents (n = 4), airway and respiratory system (n = 2), central nervous system (n = 2) and renal system (n = 1).
The cardiovascular system (n = 9) is one the most common system involved and the most frequent event was hypotension requiring treatment. Another system involved was musculoskeletal system and most common reports (n = 4) were during positioning no belt was applied in patients who received regional anesthesia (Table 2).
Twenty incidents were categorized as near misses which were further reviewed and sequenced as equipment, narcotics, infection control, medication and miscellaneous.
Five equipment related reports shown in Table 3 were pressure bag applied on a used drip with 250 milliliters of air, oxygen analyzer not working, suction not working because it was broken from its seal, suction disconnected from its base which was hidden at the back of anesthesia machine and malfunction of OR table in a patient who just received spinal and when we tried to make her lie, supine table started moving in Trendelenburg position. Narcotic and infection control related incidents contributed equally as shown in Table 2. Miscellaneous reports described were elective cases taken without consent, patient taken with wrong pre-op assessment form, surgical staff left the patient at emergence, patient left in Post-Anesthesia Care Unit (P.A.C.U) alone, no response on patients complain and power cable kept on patients arm.
Drug errors were separately looked at and it was found that medication is the main cause in 15% reports whether it is a human error or system error.
The incidents were also classified according to the type of error. Human error accounted for 57% followed by system error 19%, patient factors 13% and
![]()
Table 2. Analysis of critical incident categories (n = 33).
equipment failure 11%. Analysis of the causes of those 30 human errors revealed failure to check (equipment/drugs/doses) which was top on list resulted in 12 incidents, followed by lack of judgment (n = 8), haste (n = 5), heavy work load (n = 3) and lack of knowledge/experience (n = 1) and lack of assistance (n = 1).
Patient outcome was categorized as: no effect in 45 (85%) cases, minor physiologic disturbance in 7 (13%), severe physiological disturbance in 1 (2%) and zero morbidity and mortality.
4. Discussion
An audit is a systematic process whereby medical practice is assessed and improved [5] . Though literature is available on critical incident reporting in
![]()
Table 3. Analysis of near misses (n = 20).
anesthesia [6] [7] [8] but data is lacking in terms of specialty based critical incidents from the South Asian region. One of the objectives of these efforts is the use of critical incident reporting as one of the quality improvement method. It can be used as a tool for increasing awareness among anesthesiologist and trainees, preparation of policy/guidelines and their implementation, step to prevent medication error and identification of faulty equipment. It is of particular value in developing countries because of its low cost of setting and running the program. We have been using this tool in our department since 1996 and have found it useful.
The paradigm shift towards regional anesthesia over the past decades has made obstetric anesthesia safer and reduced mortality. Data relating to critical incident (CI) in obstetric anesthesia is deficient. Our result shows highest percentages of cardiovascular event in comparison to other reports where respiratory problems were commonest. Tay et al. from Singapore reported 297 critical incidents, where 77% were respiratory events with 35.7% laryngospasm [9] . Marcus et al. reported airway/respiratory events as 52.2% of all incidents [10] . We found only 6% airway/respiratory incidents. The reason behind this disparity is the rate (75%) of regional anesthesia which prevents airway/respiratory issues.
The highest incidents were found during the day time (8:00 a.m. - 5:00 p.m.), among elective patients mostly ASA I and ASA II patients. It does not mean that incidents do not occur during odd hour rather odd hour duties are more prone for critical incidents and morbidities. Direct consultant supervision is mostly responsible for appropriate reporting during these hours. Under reporting during on call hours is related to many factors like under supervision, denial of the fact that it is an error and desire to conceal if anything goes wrong. However, many investigators have concluded that voluntary reporting can result in underestimation of frequency of problems, but not necessarily the nature of problems [7] . Different causes of under reporting are present in literature with the reason of lack of ownership [11] , lack of interest in sharing the experience and lack of time to fill these forms [12] . Accuracy in filling contextual details is very important to capture the actual fact and to make sense out of it.
Drug errors (15%) were not very high but still very crucial in the practice of anesthesia and most of these incidents involve dispensing and administration issues. It has been recognized that obstetric patients are at a greater risk as we are dealing with two lives. Approximately 11.3% of our incidents were equipment related. This was lower compared to Vander Walt et al. who reported 14% which is nearer to our report but contrary to Tay’s report of 4.4% equipment related incidents [9] [13] .
Majority of incidents (59%) were related to human error which is similar to earlier reports (ref no). Though human errors are not easily correctable errors but contributing factors need to be identified with continuous reinforcement for adherence with guidelines and policies, change of attitudes and alteration of systems to ensure check and balance at different steps. Elhalawani recommends dividing human errors into organization accidents or unsafe act, and further divide unsafe act into intended and unintended action to get more useful information [14] . Human error reporting is the product of direct consultant supervision who observe and educate his/her trainee regarding his performance and motivate them to learn how to report it. Reinforcement and revision of existing protocol and processes as well as specific new protocols or structured courses in crisis management could be introduced. Effectiveness of these strategies in our practices is still required [15] .
Regarding outcome, our results demonstrated that majority of incidents resulted in no harm, and 13% lead to minor physiological disturbance and only 1 report of morbidity. The report of morbidity shows that spinal was instituted while doing co-load with crystalloids and patient became tachycardiac (up to 170/minute) and unconscious. She required intubation and resuscitated with fluid. The root cause of this incident was hypovolemia secondary to inefficient volume resuscitation at the time of spinal administration. Though there were two cannulas (18 G and 22 G), large bore cannula was swollen and no one noticed that how much fluid was infused. No mortality reported during this period could be because of vigilance, better monitoring and optimization of patients and quick response on these critical incidents.
Several safety issues were highlighted from our Critical incident reporting System (CIRS) which allowed us to assess errors in more details and recommend change in practice. Following are few actions taken on these incidents to prevent future incidents:
1) Incidents with educational value and increasing awareness: Some of issues highlighted and reinforced to all health provider teams in LROR were application of safety belt, removal of air from drips before applying pressure bags for rapid infusions was demonstrated and taught to trainees and technicians, demonstration of how to operate table and its problem shooting done for all team members, reinforcement of medication labels by clear adhesive tape to prevent the labels falling off and preventing syringe swaps.
2) Incidents where specific actions were taken: Poor quality ampoule of Succinylcholine which often causes injury to users was replaced with better drug and printed FLUSH labels were made available to prevent syringe swaps and writing errors.
Limitation of our study is it’s under reporting, less frequent reporting in odd hours and no previous baseline data to compare as it is novel in obstetric section.
CIRS is not the only method of evaluation of our system but it could be considered as a low cost method for partial evaluation of a system. It needs to be reinforced by other methods like feedback system, medication, clinical and equipment audits; and satisfaction surveys. Sharing of incidents in an open discussion of CIs in meeting of concerned group leads to more appropriate and acute actions and prevention of its reoccurrence. Reporting should not be for the sake of reporting rather the aim should be to share knowledge and improve quality of care.
5. Conclusion
Critical incidents reporting needs to be introduced and encouraged in all sub-specialties of anesthesia and critical care system at departmental, institutional and national level to improve patients safety, reduce morbidity and mortality and increase awareness and education.
Financial Support and Sponsorship
None.
Conflict of Interest
There is no conflict of interest.
Appendix
Critical Incident Reporting Form