- Department of Neurosurgery, Institute of Neurosurgery, Catholic University, Rome, Italy
- Department of Pathology, Institute of Pathology, Catholic University, Rome, Italy
- Department of Neurosurgery, Institute of Neurosurgery, University of Verona, Verona, Italy
Correspondence Address:
Nicola Montano
Department of Neurosurgery, Institute of Neurosurgery, University of Verona, Verona, Italy
DOI:10.4103/2152-7806.170477
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Montano N, Bonaventura RD, Coli A, Fernandez E, Meglio M. Primary intramedullary neurocytoma: Case report and literature analysis. Surg Neurol Int 25-Nov-2015;6:178
How to cite this URL: Montano N, Bonaventura RD, Coli A, Fernandez E, Meglio M. Primary intramedullary neurocytoma: Case report and literature analysis. Surg Neurol Int 25-Nov-2015;6:178. Available from: http://surgicalneurologyint.com/surgicalint_articles/primary-intramedullary-neurocytoma-case-report-and-literature/
Abstract
Background:Primary intramedullary neurocytoma is extremely rare. Due to its rarity, it is difficult to collect a wide series in a single institution to perform a survival analysis and give indications about prognosis and treatment.
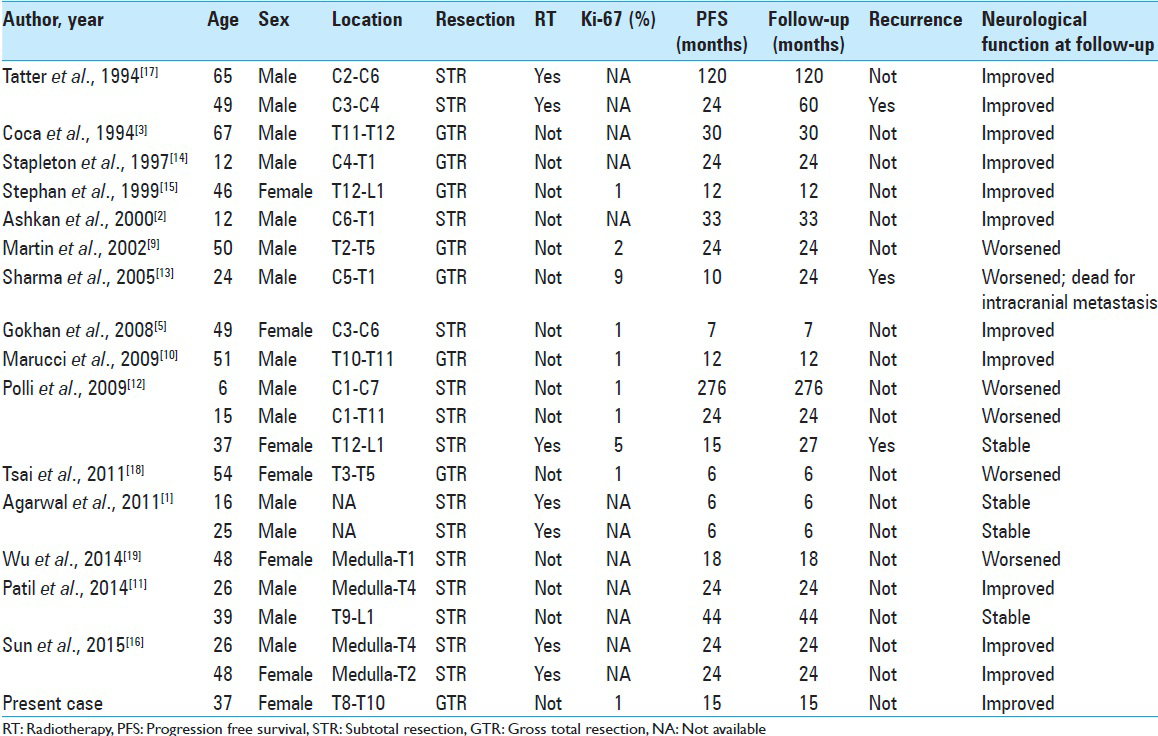
Case Description:Here, we report on a case of a 37-year-old woman with primary intramedullary neurocytoma and perform a systematic statistical analysis of cases reported in the literature. Of 21 articles found, 15 studies and the present case (22 patients) were eligible for the analysis. We studied the impact of age, sex, number of involved levels (≤2 vs. >2), entity of resection, postoperative radiotherapy (RT), proliferation index (Ki67) on the neurological outcome of patients, and on the recurrence of the tumor. Comparison of categorical variables was performed by the χ2 statistic. The Kaplan–Meier curves were plotted to calculate the progression-free survival (PFS) of these patients. P
Conclusions:We think that the goal of the surgery should be to preserve a good neurological function even if a residual tumor has to be left. Ki67 should be always evaluated due to its impact on the prognosis. Although adjuvant RT significantly improved the neurological function, its role in preventing the tumor recurrence is not clearly defined.
Keywords: Adjuvant radiotherapy, intramedullary neurocytoma, Ki67, progression-free survival, surgery
INTRODUCTION
Primary intramedullary neurocytoma, first described by Coca et al.,[
CASE REPORT
A 37-year-old woman was admitted because of a 9 months history of diffuse axial and low back pain. The neurological examination showed a hypesthesia in the left lower limb and bilateral hyperactive deep tendon reflexes. Spinal magnetic resonance imaging (MRI) with gadolinium showed an intramedullary lesion at T8–T9 level, with solid and cystic components, hypo- and hyper-intense on T2-weighted images and with dishomogeneous contrast enhancement after gadolinium administration associated to the cranial syrinx [
Figure 1
Spinal magnetic resonance imaging. (a) T2-weighted sagittal sequences showing the intramedullary lesion at T8–T9 level (yellow arrow), with solid (hypointense) and cystic (hyperintense) components. The cranial syringomyelia is evident (red arrow). (b) T2-weighted axial sequences demonstrating that the tumor is mainly located on the left spinal cord. T1-weighted sagittal (c) and axial (d) after gadolinium administration sequences showing the dishomogeneous contrast enhancement of the lesion
Figure 2
(a, ×400) H and E stain of the lesion showing a neoplasm composed of round to oval cells with finely speckled chromatin pattern and small nucleoli. Ganglion cell differentiation was commonly present among neurocytic cells. (b, ×400) Immunohistochemically, the neoplastic cells were positive for synaptophysin. The MIB-1 labeling index was 1% (not showed)
DISCUSSION
A literature search was made in the PubMed database including the following terms: Neurocytoma, spinal neurocytoma, neurocytoma of the spinal cord, intramedullary neurocytoma, and extraventricular neurocytoma. Twenty-one articles were found. We excluded from the analysis articles with a follow-up fewer than 6 months or with no information about the follow-up. Fifteen articles[
Among the considered potentially prognostic factors, we found a statistically significant better neurological outcome in the patients who underwent adjuvant RT (P = 0.04). All the patients with a number of involved levels ≤2 [
The primary intramedullary neurocytoma represents a challenge for a neurosurgeon. Preoperative radiological diagnosis can be difficult due to the rarity of this pathology. Moreover, the extremely variable features on MRI make the differential diagnosis very hard. Likewise astrocytoma, its signal can range from iso- to hypo-intensity on T1-weighted images and iso- to hyper-intensity on T2-weighted images, with homo- or hetero-geneous contrast enhancement.[
We tried to obtain some indications about the management of the primary intramedullary neurocytoma making an analysis of available cases in the literature. Although our study has some limitations, due to the heterogeneous nature of data, we think that the goal of the surgery should be to preserve a good neurological function even if a residual tumor has to be left. In fact, a GTR did not seem affect the tumor recurrence but is associated to a worsening of the neurological function in most of the cases. Moreover, the Ki67 (MIB-1) should be always evaluated because it seems strongly associated with the tumor recurrence. Further studies should clarify the role of adjuvant RT.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agarwal S, Sharma MC, Sarkar C, Suri V, Jain A, Sharma MS. Extraventricular neurocytomas: A morphological and histogenetic consideration. A study of six cases. Pathology. 2011. 43: 327-34
2. Ashkan K, Casey AT, D’Arrigo C, Harkness WF, Thomas DG. Benign central neurocytoma. Cancer. 2000. 89: 1111-20
3. Coca S, Moreno M, Martos JA, Rodriguez J, Barcena A, Vaquero J. Neurocytoma of spinal cord. Acta Neuropathol. 1994. 87: 537-40
4. Do-Dai DD, Brooks MK, Goldkamp A, Erbay S, Bhadelia RA. Magnetic resonance imaging of intramedullary spinal cord lesions: A pictorial review. Curr Probl Diagn Radiol. 2010. 39: 160-85
5. Gokhan GA, Gurer IE, Akyuz M, Tuncer R. A case of extraventricular neurocytoma of the spinal cord. Neuropathology. 2008. 28: 322-5
6. Han L, Niu H, Wang J, Wan F, Shu K, Ke C. Extraventricular neurocytoma in pediatric populations: A case report and review of the literature. Oncol Lett. 2013. 6: 1397-405
7. Hassoun J, Gambarelli D, Grisoli F, Pellet W, Salamon G, Pellissier JF. Central neurocytoma. An electron-microscopic study of two cases. Acta Neuropathol. 1982. 56: 151-6
8. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007. 114: 97-109
9. Martin AJ, Sharr MM, Teddy PJ, Gardner BP, Robinson SF. Neurocytoma of the thoracic spinal cord. Acta Neurochir (Wien). 2002. 144: 823-8
10. Marucci G, Barbanera A, Serchi E, Andreoli A. Ganglioneurocytoma of the spinal cord: Report of a case and review of literature. Eur Spine J. 2009. 18: 183-5
11. Patil AS, Menon G, Easwer HV, Nair S. Extraventricular neurocytoma, a comprehensive review. Acta Neurochir (Wien). 2014. 156: 349-54
12. Polli FM, Salvati M, Miscusi M, Delfini R, Giangaspero F. Neurocytoma of the spinal cord: Report of three cases and review of the literature. Acta Neurochir (Wien). 2009. 151: 569-74
13. Sharma S, Sarkar C, Gaikwad S, Suri A, Sharma MC. Primary neurocytoma of the spinal cord: A case report and review of literature. J Neurooncol. 2005. 74: 47-52
14. Stapleton SR, David KM, Harkness WF, Harding BN. Central neurocytoma of the cervical spinal cord. J Neurol Neurosurg Psychiatry. 1997. 63: 119-
15. Stephan CL, Kepes JJ, Arnold P, Green KD, Chamberlin F. Neurocytoma of the cauda equina. Case report. J Neurosurg. 1999. 90: 247-51
16. Sun Z, Yuan D, Cui Z, Sun Y, Yang J, Yan P. Intramedullary neurocytomas in the craniocervical spinal cord: A report of two cases and a literature review. Oncol Lett. 2015. 9: 86-90
17. Tatter SB, Borges LF, Louis DN. Central neurocytomas of the cervical spinal cord. Report of two cases. J Neurosurg. 1994. 81: 288-93
18. Tsai CY, Tsai TH, Lin CH, Cheng YH, Lieu AS. Unusual exophytic neurocytoma of thoracic spine mimicking meningioma: A case report and review of the literature. Eur Spine J. 2011. 20: S239-42
19. Wu L, Deng X, Yang C, Zhao L, Yang T, Xu Y. Primary spinal neurocytoma involving the medulla oblongata: Two case reports and a literature review. Neurol Med Chir (Tokyo). 2014. 54: 417-22