Published online Aug 7, 2016. doi: 10.3748/wjg.v22.i29.6629
Peer-review started: March 16, 2016
First decision: March 31, 2016
Revised: April 17, 2016
Accepted: May 4, 2016
Article in press: May 4, 2016
Published online: August 7, 2016
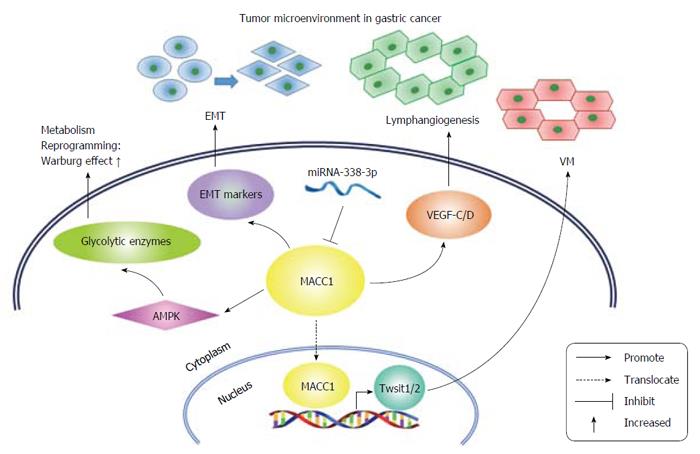
Metastasis-associated in colon cancer-1 (MACC1) is an oncogene that was first identified in colon cancer. The upstream and downstream of MACC1 form a delicate regulatory network that supports its tumorigenic role in cancers. Multiple functions of MACC1 have been discovered in many cancers. In gastric cancer (GC), MACC1 has been shown to be involved in oncogenesis and tumor progression. MACC1 overexpression adversely affects the clinical outcomes of GC patients. Regarding the mechanism of action of MACC1 in GC, studies have shown that it promotes the epithelial-to-mesenchymal transition and accelerates cancer metastasis. MACC1 is involved in many hallmarks of GC in addition to metastasis. MACC1 promotes vasculogenic mimicry (VM) via TWIST1/2, and VM increases the tumor blood supply, which is necessary for tumor progression. MACC1 also facilitates GC lymphangiogenesis by upregulating extracellular secretion of VEGF-C/D, indicating that MACC1 may be an important player in GC lymphatic dissemination. Additionally, MACC1 supports GC growth under metabolic stress by enhancing the Warburg effect. In conclusion, MACC1 participates in multiple biological processes inside and outside of GC cells, making it an important mediator of the tumor microenvironment.
Core tip: Metastasis-associated in colon cancer-1 (MACC1) is an oncogene that is involved in multiple aspects of gastric cancer (GC). Although MACC1 was first identified as a promoter of the epithelial-mesenchymal transition in GC, as in colon cancer, it has subsequently been found to have functions in GC far beyond metastasis, including vasculogenic mimicry, lymphangiogenesis and metabolic reprogramming. These features of tumorigenesis and tumor progression involve both GC cells and the surrounding tumor microenvironment, indicating that the tumor-promoting functions of MACC1 may hinge on its ability to mediate the tumor microenvironment.
- Citation: Wu ZZ, Chen LS, Zhou R, Bin JP, Liao YL, Liao WJ. Metastasis-associated in colon cancer-1 in gastric cancer: Beyond metastasis. World J Gastroenterol 2016; 22(29): 6629-6637
- URL: https://www.wjgnet.com/1007-9327/full/v22/i29/6629.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i29.6629
Metastasis-associated in colon cancer-1 (MACC1) is an oncogene. In 2009, Stein et al[1] first reported the identification and characterization of MACC1 as a tumor-promoting gene in colon cancer; they showed that it is involved in the HGF-MET pathway and promotes tumor growth and metastasis. Shortly thereafter, a wealth of research on MACC1 in several types of cancers was performed, and the results supported the oncogenic role of MACC1 in multiple hallmarks of cancer, including cell proliferation[1], epithelial-mesenchymal transition (EMT)[1,2], metabolic reprogramming[3], lymphogenesis[4] and angiogenesis[5].
MACC1 (GenBank gene ID: 346389, European Molecular Biology Laboratory (EMBL) data bank accession number AJ313524) was first referred to as Homo sapiens mRNA for putative binding protein 7a5, and the MACC1 full-length cDNA was characterized by Stein et al[1] in 2009. The MACC1 gene is located on human chromosome 7 (7p21.1) and contains seven exons and six introns. The coding cDNA of MACC1 contains 2559 nucleotides, and the MACC1 protein contains 852 amino acids. MACC1 was also referred to as SH3BP4L because it has 49.3% and 43.7% (nucleotide and amino acid, respectively) sequence identity to human SH3BP4[1].
MACC1 contains several motifs that allow it to participate in multiple biological processes in cancer cells; for example, MACC1 forms protein-protein interactions and has phosphorylation sites for tyrosine and serine-threonine kinases. MACC1 contains an SRC homology 3 (SH3) domain with the proline-rich consensus sequence that can bind to class I SH3 domain-containing proteins (R/KXXPXXP)[1]. SH3 domains have a conserved sequence, and they are located in the non-catalytic regions of many enzymes and cytoplasmic tyrosine kinases[6]. Several protein families contain SH3 domains, including the Src and Abl families, members of which are key components of pro-tumorigenic pathways[7,8]. Proteins with SH3 domains can act as tyrosine kinases or substrates of protein kinases involved in signaling pathways that regulate Ras protein, Src kinase and many other proteins[9]. Proteins with SH3 domains also regulate the activation of tyrosine kinases and are thought to increase the substrate specificity of some tyrosine kinases by binding to sites located far from their active sites[10]. It is reasonable to hypothesize that MACC1 functions as a signal transducer via its SH3 domain, either by acting as a kinase or boosting the efficiency of other kinases. Additionally, MACC1 has motifs that have been recognized as potential noncanonical class I SH3 domains, including SH2 domains, Eps15 homology domains, and clathrin and retinoblastoma protein interaction domains[1]. The MACC1 protein also has tyrosine phosphorylation sites at amino acids 665-673, 688-695 and 786-793, which allow for post-translational modifications[1].
In regards to gene polymorphism, three MACC1 single nucleotide polymorphisms (SNPs) have been genotyped in the coding region, including cg genotype (rs4721888, L31V), ct genotype (rs975263, S515L) and gc or cc genotype (rs3735615, R804T). These SNPs were not found to be associated with clinicopathological parameters or patient survival, but increased risk of shorter metastasis-free survival was observed with the ct genotype (rs975263) among stages I and II colon cancer patients less than 60 years old[11].
The publication by Stein et al[1] in 2009 established the tumor-promoting role of MACC1. In the next few years, several researchers made remarkable progress in determining the intricate regulatory network involving the upstream and downstream regions of MACC1. Because of this network, MACC1 is able to regulate multiple biological processes in many cancers. The MACC1 regulatory network is currently known to involve the HGF-MET pathway[1,12], transcriptional regulation[13] and epigenetic regulation[14-17]. Every element in this network helps MACC1 accelerate tumor progression in multiple ways, as reviewed in detail here.
First and foremost, the HGF-MET pathway is the first reported and most well-studied signaling pathway of MACC1. The HGF-MET pathway is widely accepted as one of the key pathways in cancer development and tumor progression[18]. In 2009, Stein et al[1] first identified the oncogenic role of MACC1, including control of MET expression, motility and proliferation, and its involvement in the HGF-MET pathway. First, they found that overexpression of MACC1 mRNA in colon cancer cells led to the upregulation of HGF receptor MET expression at both the mRNA and protein levels. Furthermore, underexpression of MACC1 mRNA through the introduction of a specific small interfering RNA (siRNA) decreased MET expression. In contrast, MACC1 expression was not altered in non-metastatic or metastatic colon cancer cells when MET expression was inhibited. In addition, chromatin immunoprecipitation (ChIP) and electrophoretic mobility shift assay (EMSA) data indicated that the MET gene is a transcriptional target of MACC1. Based on these results, Stein et al[1] inferred that MACC1 controls MET expression via direct transcriptional regulation. In regards to the tumor-promoting functions of MACC1, Stein et al[1] showed that MACC1 protein expression strongly induced cell migration, invasion and colony formation compared to the control. Additionally, MACC1 siRNA and MET siRNA both decreased cell motility and proliferation, but double knockdown of MACC1 and MET had no additional tumor-suppressing effects. Stein et al[1] verified these results through in vitro experiments in colon cancer tissues. Nuclear MACC1 expression and high MET expression were predominant in metastatic colon cancer tissues, while MACC1 was expressed in the cytoplasm with moderate MET expression in non-metastatic tumors. Taken together, MACC1 is an important mediator of the HGF-MET signaling pathway that acts by binding to the MET promoter. Galimi et al[19] conducted genetic and expression analyses of MET, MACC1, and HGF in metastatic colorectal cancer (mCRC) using patient xenografts treated with an MET inhibitor. They examined the correlation between MET inhibition and pathology in a cohort of 103 consecutive liver metastases from colorectal carcinomas[19]. They explored whether copy number variations of MET, MACC1, and HGF and overexpression of those genes can predict tumor response to MET-targeted therapies. They also assessed whether genomic or transcriptional deregulation of those genes was correlated with the pathologic and molecular parameters of aggressive disease. As was observed by Stein et al[1], Galimi et al[19] found that MACC1 controls MET level as an upstream regulator of MET transcription; genomic gain of MACC1 led to increased expression of MET, regardless of gains of MET copy number. However, neither MET genomic gain nor overexpression affected tumor growth of mCRC. Additionally, their pathologic correlations and bioinformatics analyses showed that MACC1 contributes to CRC progression via mechanisms other than MET transcriptional upregulation.
In 2013, Stein’s[1] study group, the group that first identified MACC1, identified the MACC1 promoter using a promoter luciferase construct that directs transcription of MACC1[13]. They generated 5’ truncated deletion constructs and transfected them into colorectal cancer cell lines to determine the essential domains within this promoter region. Their results showed that the region from -426 to -18 constitutes the core promoter and harbors functional motifs for the binding of AP-1, Sp1, and C/EBP transcription factors; this finding was validated by site-directed mutagenesis studies. Knockdown of these transcription factors remarkably reduced MACC1 expression and resulted in decreased cell migration, which was rescued by ectopic overexpression of MACC1. Additionally, the results of studies in human colorectal tumors verified the correlation between MACC1 and c-Jun and Sp1 expression levels.
MicroRNA (miRNA) is well-accepted as one of the most important epigenetic regulators of gene expression. MACC1 is regulated by many miRNAs, including miR-1[14], miR-143[15], miR-200a[16] and miR-338-3p[17]. These miRNAs bind directly to the 3’ untranslated region (UTR) of MACC1 mRNA and inhibit MACC1 protein expression. In CRC, miR-1 downregulation and MACC1 upregulation collectively promote MET overexpression[14]. Migliore et al[14] found that miR-1 was downregulated in 84.6% of tumors studied and was significantly correlated with MET overexpression, particularly in metastatic tumors. Concurrent MACC1 upregulation and miR-1 downregulation are required to achieve increased MET expression. miR-1 can suppress MET expression in colon cancer cells and inhibit MET-induced invasive growth. miR-143 also targets MACC1, resulting in inhibition of cell invasion and migration of colorectal cancer cells[15]. Zhang et al[15] reported that miR-143 directly targets MACC1 in CRC. In colorectal cancer cells, the same effect of MACC1 knockdown, significant inhibition of cell growth, migration and invasion, is achieved by restoration of miR-143. Concurrent miR-143 overexpression and MACC1 suppression enhance those inhibitory effects. Conversely, inhibition of miR-143 promotes cell growth, migration and invasion in colorectal cancer cells. Furthermore, miR-143 expression is inversely correlated with MACC1 mRNA expression in CRC tissues. In addition to being targeted by miR-1 and miR-143 in colorectal cancer, MACC1 is targeted by other miRNAs in other types of cancers, such as miR-200a and miR-338-3p. miR-200a suppresses cell growth and migration by targeting MACC1 and predicts prognosis in hepatocellular carcinoma (HCC)[16]. Researchers have shown that miR-200a is markedly downregulated in HCC and has suppressive effects on tumor cell growth and metastasis. They found that miR-200a suppresses tumor growth and metastasis by directly targeting MACC1. Additionally, miR-338-3p inhibits EMT in gastric cancer (GC) cells by targeting MACC1/MET/AKT signaling[17]. As a tumor-suppressing miRNA, miR-338-3p inhibits the migration and invasion of GC cells in vitro, and knockdown of miR-338-3p in GC cells leads to mesenchymal-like changes. miR-338-3p influences the expression of EMT-associated proteins by upregulating the epithelial marker E-cadherin and downregulating the mesenchymal markers N-cadherin, fibronectin, and vimentin. Conversely, reintroduction of MACC1 reverses miR-338-3p-induced EMT suppression. miR-338-3p represses the MET/AKT pathway by directly targeting MACC1.
When MACC1 was identified, it received its name because it was shown to be significantly associated with metastasis in colon cancer and inversely correlated with patient outcome. Further study of MACC1 has led to an increasing number of functions being reported, indicating the powerful oncogenic role of MACC1 in multiple cancers. Currently, MACC1 is being studied in an increasing number of solid tumor types.
After Stein et al[1] reported the tumor-promoting functions of MACC1 in colon cancer, researchers showed strong interest in exploring MACC1 in other cancers. Shortly thereafter, a few studies showed that MACC1 may also be a potential biomarker in lung cancer, hepatocellular carcinoma and ovarian cancer. In 2011, Chundong et al[20] reported that positive staining for MACC1 expression in resected specimens was associated with poor clinical prognosis in patients with lung adenocarcinoma following surgery. At the same time, Qiu et al[21] identified MACC1 as a novel prognostic marker in HCC. Their results showed that MACC1 is more highly expressed in HCC than in non-HCC tissues and that MACC1 expression is significantly increased in HCC tissues with high alpha fetoprotein (AFP) expression. MACC1 expression is also associated with overall survival (OS) and disease free survival (DFS). Meanwhile, Shirahata et al[22] discovered that MACC1 is more frequently expressed in vascular invasive HCC than in noninvasive HCC and may serve as a new parameter for the prognostic prediction of HCC. High MACC1 expression was also detected in ovarian cancer tissues by Zhang et al[23]. They knocked down MACC1 expression in the ovarian cancer cell line OVCAR-3 using specific small hairpin RNA (shRNA) and found that downregulation of MACC1 significantly inhibits cell proliferation, migration and invasion while significantly promoting apoptosis. As the number of studies of MACC1 conducted in multiple cancers has increased, the correlation of high MACC1 expression with poorer clinical outcome has been identified in an increasing number of cancer types, including GC[2], pancreatic cancer[24], glioma[25], breast cancer[26], nasopharyngeal carcinoma[27], gallbladder cancer[28], cervical cancer[29], esophageal cancer[30] and osteosarcoma[31].
Increasing evidence has suggested that MACC1 overexpression is associated with the development and progression of many cancer types. A meta-analysis assessed the relationship between MACC1 overexpression in solid tumors and patient survival[32]. The combined results suggested strong links between high MACC1 expression and poor OS, DFS and relapse-free survival (RFS). Another meta-analysis provided further evidence of the prognostic value of MACC1 expression in digestive system neoplasms: high MACC1 expression is significantly correlated with poorer OS and RFS in patients with digestive system neoplasms[33].
Even though MACC1 is a proven oncogene in solid tumors, as mentioned above, most studies have only reported the correlation between MACC1 overexpression and clinical parameters and have failed to further clarify the underlying mechanism of MACC1 in promoting tumor progression and metastasis; the exception to this is the studies conducted in CRC and GC. In CRC, Stein et al[1], the identifiers of MACC1, have made extraordinary efforts to clarify how MACC1 acts and is regulated. In GC, many aspects of the role of MACC1 in cancer biology have also been elucidated, and the regulatory network of MACC1 has been shown to include other cellular processes in addition to metastasis.
As GC is similar to CRC in terms of being a digestive system neoplasm, and MACC1 is a proven prominent oncogene in CRC, several researchers had great interest in identifying the tumorigenic potential of MACC1 in GC. MACC1 indeed plays an important role in the progression of GC and has many functions beyond metastasis promotion.
In the beginning of MACC1 research, Guo et al[34] reported the correlation of MACC1 protein expression and clinical features of GC. They performed an immunohistochemistry (IHC) assay to detect MACC1 protein expression in GC tissues. MACC1 and MET protein expression was positively correlated. In accordance with the metastasis-promoting properties of MACC1, MACC1 protein expression in GC tissues is significantly correlated with lymph node metastasis, peritoneal metastasis and hepatic metastasis, all of which contribute to a poor prognosis for GC patients. At nearly the same time, another publication confirmed the correlation between MACC1 and Met expression in GC and their correlation with clinical parameters and patient prognosis[35]. The results of that study also indicated that MACC1 and MET expression levels are highly increased and are significantly correlated in GC tissues. MACC1 and MET expression is associated with larger tumor size, deeper tumor invasion, lymph node metastasis, lymphatic involvement, venous invasion, distant metastasis and advanced clinical stage. Compared to patients with high levels of these proteins, patients harboring lower MACC1 and Met levels had a higher 5-year survival rate.
Those first two studies showed a correlation between high MACC1 expression and poor clinical outcome in GC patients, implying that MACC1 may be an independent prognostic indicator of GC. However, they both failed to explore the underlying mechanism through which MACC1 facilitates GC progression. However, Wang et al[2] managed to reveal important functions of MACC1 in GC. As with the first two studies, they first verified MACC1 expression in GC and its correlation with adverse clinical features. They studied fresh GC tissues from 361 GC patients (stages I-IV) by Western blot analysis of MACC1 and conducted a retrospective analysis of MACC1 protein expression by IHC. Then, they examined the correlation of MACC1 expression with the clinical parameters in GC patients. Consistent with previous studies, higher MACC1 expression was associated with higher frequencies of advanced disease, postoperative recurrence, metastases and a higher mortality rate. Clinical prognosis was significantly poorer for patients with tumors with high MACC1 expression. MACC1 overexpression significantly accelerated tumor proliferation, migration and invasion and facilitated metastasis of GC in vivo. Moreover, MACC1 mRNA expression was found to be significantly correlated with markers of EMT in patients with GC. MACC1 overexpression upregulated EMT factors and induced changes in the levels of EMT markers, and silencing of MACC1 reversed these changes. All these findings indicate that MACC1 modulates EMT in GC.
MACC1 also mediates acetylcholine-induced invasion and migration in GC. The neurotransmitter acetylcholine (ACh) is known to promote the growth and metastasis of several cancers by binding to M3 muscarinic receptors (M3Rs). By binding to M3Rs, ACh promotes GC cell invasion and migration and the expression of several markers of EMT. ACh upregulates MACC1 in GC cells, and MACC1 knockdown using siRNA attenuates the effects of ACh on GC cells. AMP-activated protein kinase (AMPK) serves as an intermediate signal between ACh and MACC1. MACC1 may mediate acetylcholine-induced invasion and migration in human GC cells by participating in the Ach/M3R/AMPK/MACC1 signaling pathway[36].
Considering that tumor metastasis requires a sufficient blood supply, which, in most cases, is achieved by neovascularization, angiogenesis is a well-recognized hallmark of cancer[37]. However, anti-angiogenesis therapy has no significant benefits for some cancer patients[37]. Hence researchers have focused on identifying alternative tumor blood supply sources independent of blood vessel endothelium, termed vasculogenic mimicry (VM)[38]. VM is formed by cancer cells and is strongly associated with EMT, TWIST1 activation and tumor progression.
Considering that MACC1 induces EMT and is associated with poor prognoses of patients with GC, Wang et al[5] aimed to determine whether MACC1 promotes VM and regulates the TWIST signaling pathway, which is closely related to the EMT process in GC. To prove this theory, they investigated MACC1 expression and VM by IHC in 88 patients with stage IV GC and investigated the role of TWIST1 and TWIST2 in MACC1-induced VM both in GC xenografts and in GC cell lines. As expected, the VM density was significantly increased in tumor tissues from patients who died of GC and was positively correlated with MACC1 immunoreactivity. Furthermore, the patients with high VM density had a significantly poorer survival rate. The nuclear expression of MACC1, TWIST1, and TWIST2 is upregulated in GC tissues compared with normal tissues, and overexpression of MACC1 increased TWIST1/2 expression and induced typical VM in GC xenografts and GC cell lines. Nuclear translocations of MACC1, TWIST1, and TWIST2 were induced by HGF, and an MET inhibitor reversed those effects. These findings indicate that MACC1 promotes VM in GC by regulating the HGF/MET-TWIST1/2 signaling pathway, allowing GC cells to gain an increased blood supply and grow and possibly migrate faster.
In addition to EMT, lymph node metastasis is another common feature of GC and is one of the major causes of GC death[39]. Lymphangiogenesis is the first and most critical step of lymph node metastasis[40]. According to the aforementioned studies, MACC1 expression is associated with lymph node metastasis. Sun et al[4] reported that MACC1 promotes lymphangiogenesis and that MACC1 and lymphangiogenesis are positively correlated both in vivo and in vitro. In that study, an indirect co-culture system was constructed to determine whether MACC1 promotes lymphangiogenesis. The study involved collecting supernatant from MACC1 overexpressed/knockdown GC cells and treating human lymphatic endothelial cells (HLECs) with the collected supernatant. The results showed that supernatant from MACC1 overexpressed GC cells enhanced the proliferative and migratory capacities of HLECs. Additionally, MACC1 overexpression in xenografts promoted lymphatic vessel formation. In regards to the underlying mechanism, MACC1 significantly increases the expression of VEGF-C/D, which are important factors in the regulation of lymphangiogenesis and the promotion of lymphatic metastasis in vivo and in vitro[41].
In addition to vascular supply, tumor metastasis relies on sufficient metabolic supply to a large extent. In cancer cells, glycometabolism is reprogrammed to better accommodate the increased energy demand. Unlike normal cells, the main metabolic process of cancer cells is glycolysis, known as the Warburg effect, and this allows cancer cells to better adapt to and resist metabolic stress[42]. MACC1 has been reported to be involved in metabolic reprogramming in GC. MACC1 expression is significantly upregulated via adenosine monophosphate-activated protein kinase (AMPK) signaling in response to glucose deprivation-induced metabolic stress[3]. The results of that study showed that MACC1 expression is positively correlated with the maximum standardized uptake value of 18F-deoxyglucose in GC patients and that MACC1 enhances 18F-deoxyglucose uptake in GC cells and xenografts. The underlying mechanism of this MACC1 effect is promotion of the Warburg effect through upregulation of the activities and expression of a series of glycolytic enzymes, including hexokinase, pyruvate dehydrogenase kinase and lactate dehydrogenase, in GC cells. This metabolic shift enhances cell viability and resistance to apoptosis by facilitating ATP generation, reducing reactive oxygen species production and stabilizing mitochondrial membrane potential. In contrast, MACC1 silencing, which blocks the Warburg effect, causes GC cells to be more vulnerable to metabolic stress.
MiRNAs are well-recognized as one of the key epigenetic regulators of the EMT process and are associated with metastasis in GC[43]. Huang et al[17] found that miR-338-3p directly binds to MACC1 3’ UTR to regulate MACC1 expression. Because miR-338-3p was previously reported to be aberrantly expressed in GC, it was the first miRNA that they examined via bioinformatics analysis as a potential MACC1 regulator. Then, they showed that miR-338-3p inhibited the migration and invasion of GC cells and that inhibition of miR-338-3p in GC cells resulted in mesenchymal-like changes. MiR-338-3p also upregulated the epithelial marker E-cadherin and downregulates the mesenchymal markers, N-cadherin, fibronectin, and vimentin. Furthermore, reintroduction of MACC1 reversed miR-338-3p-induced EMT inhibition. MACC1 was proven to be directly targeted by miR-338-3p, and the Met/Akt pathway was repressed by MACC1 inhibition. Consistently, the expression of miR-338-3p and MACC1 is inversely correlated in human GC tissue samples.
After determining the diagnostic and prognostic value of circulating MACC1 in CRC, the study group of Stein et al[1] conducted a prospective study of GC and found that circulating MACC1 is a diagnostic and prognostic biomarker for GC[44]. Compared to tumor-free volunteers, the levels of circulating MACC1 transcripts were increased in GC patients of all disease stages: tumor without metastasis, tumor with synchronous metastasis, and tumor with metachronous metastasis. Both the sensitivity and specificity of MACC1 as a diagnostic and prognostic biomarker for GC were statistically significant. Importantly, GC patients with high circulating plasma MACC1 transcript levels demonstrated significantly shorter survival compared to patients with low MACC1 levels. Furthermore, GC patients with high circulating plasma transcript levels of MACC1 and S100A4 had significantly shorter survival compared to patients with low levels of both biomarkers and patients with elevation of only one biomarker.
Taken together, we conclude that MACC1 plays an important role in many hallmarks of cancer in GC; MACC1 has crucial roles in GC in addition to metastasis promotion. These strong pro-tumorigenic properties of MACC1 have been observed since it was first discovered. The fact that MACC1 interacts with the HGF-MET pathway, a key tumor-promoting signaling pathway, to promote cell motility and metastasis establishes its oncogenic role. MACC1 contains an SH3 domain, which is a powerful signal transducing domain that may be responsible for the oncogenic nature of MACC1. With this domain, MACC1 is able to execute its signal transducing functions, and, as aforementioned, it is possible that MACC1 is involved in pathways other than the HGF-MET pathway, such as the MAPK pathway or apoptosis-associated pathway. It is also worth noting that MACC1 is located on chromosome 7, which also contains MET and HGF. If the copy number of chromosome 7 is increased, MET and HGF gene copy numbers will also be increased, and the copy number gain of MACC1 may result in increased expression of MET and HGF. Furthermore, the intricate MACC1 regulatory network formed by multiple signaling pathways, kinases, transcription factors, and miRNAs facilitates the tumor-promoting features of MACC1.
MACC1 aids GC progression through multiple means; it functions beyond metastasis promotion. MACC1 has a role in lymphogenesis, VM formation and metabolic reprogramming, which are also important hallmarks of cancer. EMT is the only hallmark of cancer among those mentioned above that is directly related to tumor metastasis. However, other hallmarks of cancer should not be considered independent of metastasis. In fact, lymphogenesis is the core process of lymph node metastasis, and VM formation contributes to the blood supply necessary for tumor growth. Additionally, metabolic reprogramming allows cancer cells to resist metabolic stress during metastasis formation. Thus, all of these hallmarks of cancer, not only EMT, act to promote metastasis and tumor progression. The regulation of these processes by MACC1 in GC is a relatively complete example of how oncogenes participate in multiple biological processes of cancer and promote tumor progression.
MACC1 participates in multiple biological processes both inside and outside GC cells, functioning as an important mediator of the tumor microenvironment (Figure 1). The tumor microenvironment is defined and well-recognized as the cellular environment in which the tumor exists, including the surrounding blood vessels, lymphocytes, signaling molecules and other key elements, including immune cells, fibroblasts, bone marrow-derived inflammatory cells and the extracellular matrix (ECM)[45]. These components of the tumor microenvironment interact with GC and neighboring cells. Because MACC1 promotes EMT, VM formation, lymphangiogenesis and the Warburg effect, the main aspects of which are inside GC cells or in the neighboring environment, MACC1 may mediate the tumor microenvironment in GC. MACC1 not only helps GC cells transition into mesenchymal form but also influences the surrounding blood supply and lymphangiogenesis by promoting VM formation and VEGF-C/D secretion. Furthermore, MACC1 enhances the Warburg effect and changes the metabolite composition of the inside and outside of GC cells, ultimately sustaining GC growth. All of these properties of MACC1 aid the metastasis of GC cells. Future studies of MACC1 functions should clearly focus on the tumor microenvironment. Increasing evidence of the role of MACC1 in the tumor microenvironment will expand our knowledge of the role MACC1 in cancer. Targeting MACC1 may disrupt the balance of the tumor microenvironment, resulting in tumor suppression.
Therefore, MACC1 is a noteworthy oncogene and a promising biomarker in GC. The metastasis-promoting properties of MACC1 allow it to serve as a prognostic biomarker in GC. High MACC1 expression indicates a poor clinical outcome of GC patients. Considering the involvement of MACC1 in multiple malignant biological behaviors, MACC1 may also be a promising target for the inhibition of GC, especially for patients with advanced disease. Furthermore, the involvement of MACC1 in mediation of the tumor microenvironment can lead to a more comprehensive understanding of GC. Simultaneous inhibition of MACC1 and relevant components of its regulatory network in the tumor microenvironment may help boost the efficacy of MACC1 inhibition. In the future, translational research should pay increased attention to MACC1 and its therapeutic potential for GC to improve treatment, which is currently limited, and accelerate the progress of research from bench to bedside.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Miyoshi N, Stein US S- Editor: Gong ZM L- Editor: A E- Editor: Ma S
| 1. | Stein U, Walther W, Arlt F, Schwabe H, Smith J, Fichtner I, Birchmeier W, Schlag PM. MACC1, a newly identified key regulator of HGF-MET signaling, predicts colon cancer metastasis. Nat Med. 2009;15:59-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 321] [Cited by in F6Publishing: 359] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 2. | Wang L, Wu Y, Lin L, Liu P, Huang H, Liao W, Zheng D, Zuo Q, Sun L, Huang N. Metastasis-associated in colon cancer-1 upregulation predicts a poor prognosis of gastric cancer, and promotes tumor cell proliferation and invasion. Int J Cancer. 2013;133:1419-1430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | Lin L, Huang H, Liao W, Ma H, Liu J, Wang L, Huang N, Liao Y, Liao W. MACC1 supports human gastric cancer growth under metabolic stress by enhancing the Warburg effect. Oncogene. 2015;34:2700-2710. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Sun L, Duan J, Jiang Y, Wang L, Huang N, Lin L, Liao Y, Liao W. Metastasis-associated in colon cancer-1 upregulates vascular endothelial growth factor-C/D to promote lymphangiogenesis in human gastric cancer. Cancer Lett. 2015;357:242-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Wang L, Lin L, Chen X, Sun L, Liao Y, Huang N, Liao W. Metastasis-associated in colon cancer-1 promotes vasculogenic mimicry in gastric cancer by upregulating TWIST1/2. Oncotarget. 2015;6:11492-11506. [PubMed] [Cited in This Article: ] |
| 6. | Mayer BJ, Baltimore D. Signalling through SH2 and SH3 domains. Trends Cell Biol. 1993;3:8-13. [PubMed] [Cited in This Article: ] |
| 7. | Roskoski R. Src protein-tyrosine kinase structure, mechanism, and small molecule inhibitors. Pharmacol Res. 2015;94:9-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 300] [Cited by in F6Publishing: 355] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 8. | Panjarian S, Iacob RE, Chen S, Engen JR, Smithgall TE. Structure and dynamic regulation of Abl kinases. J Biol Chem. 2013;288:5443-5450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Amata I, Maffei M, Pons M. Phosphorylation of unique domains of Src family kinases. Front Genet. 2014;5:181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Pagano MA, Tibaldi E, Palù G, Brunati AM. Viral proteins and Src family kinases: Mechanisms of pathogenicity from a “liaison dangereuse”. World J Virol. 2013;2:71-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Schmid F, Burock S, Klockmeier K, Schlag PM, Stein U. SNPs in the coding region of the metastasis-inducing gene MACC1 and clinical outcome in colorectal cancer. Mol Cancer. 2012;11:49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Stein U, Smith J, Walther W, Arlt F. MACC1 controls Met: what a difference an Sp1 site makes. Cell Cycle. 2009;8:2467-2469. [PubMed] [Cited in This Article: ] |
| 13. | Juneja M, Ilm K, Schlag PM, Stein U. Promoter identification and transcriptional regulation of the metastasis gene MACC1 in colorectal cancer. Mol Oncol. 2013;7:929-943. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Migliore C, Martin V, Leoni VP, Restivo A, Atzori L, Petrelli A, Isella C, Zorcolo L, Sarotto I, Casula G. MiR-1 downregulation cooperates with MACC1 in promoting MET overexpression in human colon cancer. Clin Cancer Res. 2012;18:737-747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Zhang Y, Wang Z, Chen M, Peng L, Wang X, Ma Q, Ma F, Jiang B. MicroRNA-143 targets MACC1 to inhibit cell invasion and migration in colorectal cancer. Mol Cancer. 2012;11:23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 16. | Feng J, Wang J, Chen M, Chen G, Wu Z, Ying L, Zhuo Q, Zhang J, Wang W. miR-200a suppresses cell growth and migration by targeting MACC1 and predicts prognosis in hepatocellular carcinoma. Oncol Rep. 2015;33:713-720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Huang N, Wu Z, Lin L, Zhou M, Wang L, Ma H, Xia J, Bin J, Liao Y, Liao W. MiR-338-3p inhibits epithelial-mesenchymal transition in gastric cancer cells by targeting ZEB2 and MACC1/Met/Akt signaling. Oncotarget. 2015;6:15222-15234. [PubMed] [Cited in This Article: ] |
| 18. | Lordick F. Targeting the HGF/MET pathway in gastric cancer. Lancet Oncol. 2014;15:914-916. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Galimi F, Torti D, Sassi F, Isella C, Corà D, Gastaldi S, Ribero D, Muratore A, Massucco P, Siatis D. Genetic and expression analysis of MET, MACC1, and HGF in metastatic colorectal cancer: response to met inhibition in patient xenografts and pathologic correlations. Clin Cancer Res. 2011;17:3146-3156. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 20. | Chundong G, Uramoto H, Onitsuka T, Shimokawa H, Iwanami T, Nakagawa M, Oyama T, Tanaka F. Molecular diagnosis of MACC1 status in lung adenocarcinoma by immunohistochemical analysis. Anticancer Res. 2011;31:1141-1145. [PubMed] [Cited in This Article: ] |
| 21. | Qiu J, Huang P, Liu Q, Hong J, Li B, Lu C, Wang L, Wang J, Yuan Y. Identification of MACC1 as a novel prognostic marker in hepatocellular carcinoma. J Transl Med. 2011;9:166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Shirahata A, Fan W, Sakuraba K, Yokomizo K, Goto T, Mizukami H, Saito M, Ishibashi K, Kigawa G, Nemoto H. MACC 1 as a marker for vascular invasive hepatocellular carcinoma. Anticancer Res. 2011;31:777-780. [PubMed] [Cited in This Article: ] |
| 23. | Zhang R, Shi H, Chen Z, Wu Q, Ren F, Huang H. Effects of metastasis-associated in colon cancer 1 inhibition by small hairpin RNA on ovarian carcinoma OVCAR-3 cells. J Exp Clin Cancer Res. 2011;30:83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Wang G, Kang MX, Lu WJ, Chen Y, Zhang B, Wu YL. MACC1: A potential molecule associated with pancreatic cancer metastasis and chemoresistance. Oncol Lett. 2012;4:783-791. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 25. | Hagemann C, Fuchs S, Monoranu CM, Herrmann P, Smith J, Hohmann T, Grabiec U, Kessler AF, Dehghani F, Löhr M. Impact of MACC1 on human malignant glioma progression and patients’ unfavorable prognosis. Neuro Oncol. 2013;15:1696-1709. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Huang Y, Zhang H, Cai J, Fang L, Wu J, Ye C, Zhu X, Li M. Overexpression of MACC1 and Its significance in human Breast Cancer Progression. Cell Biosci. 2013;3:16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 27. | Meng F, Li H, Shi H, Yang Q, Zhang F, Yang Y, Kang L, Zhen T, Dai S, Dong Y. MACC1 down-regulation inhibits proliferation and tumourigenicity of nasopharyngeal carcinoma cells through Akt/β-catenin signaling pathway. PLoS One. 2013;8:e60821. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Chen L, Wang J, Fu L, Zhang B, Zhang H, Ye B. Prognostic significance of metastasis associated in colon cancer 1 (MACC1) expression in patients with gallbladder cancer. J Cancer Res Ther. 2014;10:1052-1056. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Guo L, Lu W, Zhang X, Luo D, Zhang H. Metastasis-associated colon cancer-1 is a novel prognostic marker for cervical cancer. Int J Clin Exp Pathol. 2014;7:4150-4155. [PubMed] [Cited in This Article: ] |
| 30. | Zhu M, Xu Y, Mao X, Gao Y, Shao L, Yan F. Overexpression of metastasis-associated in colon cancer-1 associated with poor prognosis in patients with esophageal cancer. Pathol Oncol Res. 2013;19:749-753. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Zhang K, Zhang Y, Zhu H, Xue N, Liu J, Shan C, Zhu Q. High expression of MACC1 predicts poor prognosis in patients with osteosarcoma. Tumour Biol. 2014;35:1343-1350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Wang G, Fu Z, Li D. MACC1 overexpression and survival in solid tumors: a meta-analysis. Tumour Biol. 2015;36:1055-1065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Wu Z, Zhou R, Su Y, Sun L, Liao Y, Liao W. Prognostic Value of MACC1 in Digestive System Neoplasms: A Systematic Review and Meta-Analysis. Biomed Res Int. 2015;2015:252043. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Guo T, Yang J, Yao J, Zhang Y, Da M, Duan Y. Expression of MACC1 and c-Met in human gastric cancer and its clinical significance. Cancer Cell Int. 2013;13:121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 35. | Ma J, Ma J, Meng Q, Zhao ZS, Xu WJ. Prognostic value and clinical pathology of MACC-1 and c-MET expression in gastric carcinoma. Pathol Oncol Res. 2013;19:821-832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 36. | Yang T, He W, Cui F, Xia J, Zhou R, Wu Z, Zhao Y, Shi M. MACC1 mediates acetylcholine-induced invasion and migration by human gastric cancer cells. Oncotarget. 2016;7:18085-18094. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 37. | Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39812] [Cited by in F6Publishing: 42985] [Article Influence: 3306.5] [Reference Citation Analysis (4)] |
| 38. | Paulis YW, Soetekouw PM, Verheul HM, Tjan-Heijnen VC, Griffioen AW. Signalling pathways in vasculogenic mimicry. Biochim Biophys Acta. 2010;1806:18-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 39. | Deng JY, Liang H. Clinical significance of lymph node metastasis in gastric cancer. World J Gastroenterol. 2014;20:3967-3975. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 111] [Cited by in F6Publishing: 123] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 40. | Li S, Li Q. Cancer stem cells, lymphangiogenesis, and lymphatic metastasis. Cancer Lett. 2015;357:438-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 41. | Karnezis T, Shayan R, Caesar C, Roufail S, Harris NC, Ardipradja K, Zhang YF, Williams SP, Farnsworth RH, Chai MG. VEGF-D promotes tumor metastasis by regulating prostaglandins produced by the collecting lymphatic endothelium. Cancer Cell. 2012;21:181-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 205] [Cited by in F6Publishing: 199] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 42. | Lu J, Tan M, Cai Q. The Warburg effect in tumor progression: mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett. 2015;356:156-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 390] [Cited by in F6Publishing: 473] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 43. | Bouyssou JM, Manier S, Huynh D, Issa S, Roccaro AM, Ghobrial IM. Regulation of microRNAs in cancer metastasis. Biochim Biophys Acta. 2014;1845:255-265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 44. | Burock S, Herrmann P, Wendler I, Niederstrasser M, Wernecke KD, Stein U. Circulating Metastasis Associated in Colon Cancer 1 transcripts in gastric cancer patient plasma as diagnostic and prognostic biomarker. World J Gastroenterol. 2015;21:333-341. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 27] [Cited by in F6Publishing: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 45. | Joyce JA, Fearon DT. T cell exclusion, immune privilege, and the tumor microenvironment. Science. 2015;348:74-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1263] [Cited by in F6Publishing: 1436] [Article Influence: 159.6] [Reference Citation Analysis (0)] |