Published online Dec 7, 2015. doi: 10.3748/wjg.v21.i45.12882
Peer-review started: May 22, 2015
First decision: July 10, 2015
Revised: August 9, 2015
Accepted: September 30, 2015
Article in press: September 30, 2015
Published online: December 7, 2015
AIM: To compare the outcomes between the Stretta procedure and laparoscopic toupet fundoplication (LTF) in patients with gastroesophageal reflux disease (GERD)-related extra-esophageal symptoms.
METHODS: From January 2011 to February 2012, a total of 98 patients diagnosed with GERD-related extra-esophageal symptoms who met the inclusion criteria were enrolled in this study. All patients who either underwent the Stretta procedure or LTF treatment have now completed the 3-year follow-up. Primary outcome measures, including frequency and severity of extra-esophageal symptoms, proton pump inhibitor (PPI) use, satisfaction, and postoperative complications, were assessed. The results of the Stretta procedure and LTF therapy were analyzed and compared.
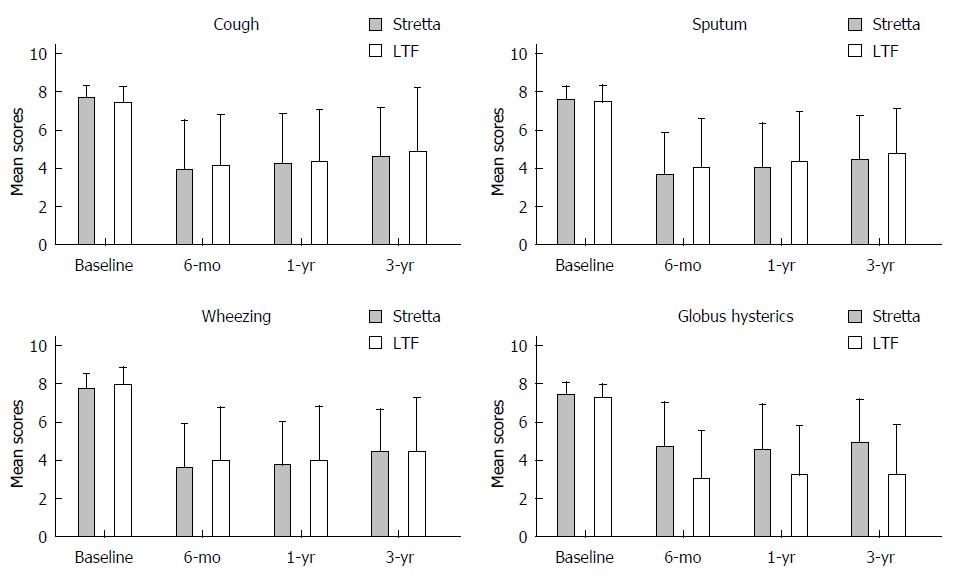
RESULTS: There were 47 patients in the Stretta group and 51 patients in the LTF group. Ninety patients were available at the 3-year follow-up. The total of the frequency and severity scores for every symptom improved in both groups (P < 0.05). Improvement in symptom scores of cough, sputum, and wheezing did not achieve statistical significance between the two groups (P > 0.05). However, the score for globus hysterics was different between the Stretta group and the LTF group (4.9 ± 2.24 vs 3.2 ± 2.63, P < 0.05). After the Stretta procedure and LTF treatment, 29 and 33 patients in each group achieved PPI therapy independence (61.7% vs 64.7%, P = 0.835). The patients in the LTF group were more satisfied with their quality of life than those in the Stretta procedure group (P < 0.05). Most complications resolved without intervention within two weeks; however, two patients in the LTF group still suffered from severe dysphagia 2 wk after the operation, and it improved after bougie dilation treatment in both patients.
CONCLUSION: The Stretta procedure and LTF were both safe and effective for the control of GERD-related extra-esophageal symptoms and the reduction of PPI use.
Core tip: Laparoscopic toupet fundoplication offers equivalent symptom relief and a significantly lower risk of postoperative dysphagia compared with laparoscopic Nissen fundoplication. The Stretta procedure and laparoscopic Toupet fundoplication have been demonstrated to be effective and safe in controlling gastroesophageal reflux disease-related symptoms as minimally invasive procedures. Few studies have been conducted to compare the outcome between laparoscopic Toupet fundoplication and the Stretta procedure. In this prospective study, we compared the outcomes of patients who underwent the Stretta procedure and laparoscopic Toupet fundoplication and evaluated the efficacy of the techniques in controlling gastroesophageal reflux disease-related extra-esophageal symptoms.
- Citation: Yan C, Liang WT, Wang ZG, Hu ZW, Wu JM, Zhang C, Chen MP. Comparison of Stretta procedure and toupet fundoplication for gastroesophageal reflux disease-related extra-esophageal symptoms. World J Gastroenterol 2015; 21(45): 12882-12887
- URL: https://www.wjgnet.com/1007-9327/full/v21/i45/12882.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i45.12882
Gastroesophageal reflux disease (GERD) is a condition that develops when the reflux of stomach contents causes troublesome symptoms and/or complications[1]. The typical symptoms of GERD are heartburn and regurgitation. The prevalences of extra-esophageal symptoms, including pneumonia, asthma, bronchitis, laryngitis, pharyngitis, chronic cough, wheezing, oral ulcers, and snoring, are significantly increased in symptomatic gastroesophageal reflux patients[2]. GERD has been confirmed to be one of the three main causes of chronic cough, accounting for approximately 20% of all cases[3].
Several randomized controlled trials strongly support antireflux surgery as an effective alternative for patients with disease that is not controlled well by medical therapy[4,5]. Laparoscopic Toupet fundoplication (LTF) offers equivalent symptom relief and has a significantly lower risk of postoperative complications compared with laparoscopic Nissen fundoplication (LNF)[6,7]. The earliest endoluminal technique for GERD, radiofrequency energy delivery to the gastroesophageal junction (Stretta), was introduced in 2000. Some studies on the Stretta procedure have confirmed not only an improvement in GERD symptoms and quality of life but also greater efficacy and safety compared with other surgical techniques[8].
LTF and the Stretta procedure have been used to treat selected patients with GERD-related extra-esophageal symptoms. This study compared the efficacy and safety of these two procedures, which were performed to control extra-esophageal symptoms in GERD patients.
From January 2011 to February 2012, we clinically treated a total of 98 patients with the Stretta procedure and LTF who suffered from extra-esophageal symptoms and completed 3 years of follow-up. All patients failed to respond to medical treatment or opted for surgery despite effective medical management.
The inclusion criteria were as follows: (1) GERD diagnosed by endoscopic evidence of esophagitis or abnormal esophageal pH, a DeMeester score ≥ 14.7 with symptom correlation of ≥ 50%, and/or > 73 reflux episodes during 24-h ambulatory impedance monitoring; (2) lower than normal lower esophageal sphincter (LES) pressure detected by esophageal manometry; (3) endoscopically confirmed Los Angeles grade A or B esophagitis; (4) non-hiatal hernia or small (< 2 cm) hiatal hernia; and (5) age ≥ 18 years. Patients with central nervous system diseases, connective tissue diseases, previous esophageal or gastric surgery, esophageal stricture, shortened esophagus, impaired distal esophageal peristalsis, Barrett’s esophagus, autoimmune diseases, collagen vascular diseases, and/or coagulation disorders were excluded.
LTF was performed with five ports under general anesthesia. After dissecting the gastro-hepatic ligament with a harmonic scalpel, a window was created behind the lower esophagus. Then, the diaphragmatic crura were carefully dissected, and approximately 5 cm of the distal esophagus was mobilized, while the mediastinal structures, including the pleura, pericardium, vagus nerves, and aorta, were identified and preserved. In all cases, the gastric fundus was dissected by dividing the short gastric vessels. The diaphragmatic crura were sewed behind the esophagus with 1-2 non-absorbable sutures, and a posterior 270° and 2-cm-long fundoplication was constructed with 5-6 interrupted non-absorbable sutures.
For the Stretta procedure, after the patient was sedated with a combination of intravenously administered fentanyl and midazolam, the distance to the gastro-esophageal junction was measured under gastroscopy. Then, the endoscope was withdrawn, and a radiofrequency-delivering catheter, consisting of a flexible balloon-basket assembly with four electrode needle sheaths, was introduced orally using a guide wire. The balloon was inflated 2 cm proximal to the squamo-columnar junction, the electrode needles were deployed, and RF energy was delivered for 1 min. The needles were then withdrawn, the balloon was deflated, and the catheter was rotated 45°. This process was serially repeated every 0.5 cm inward to cover an area 2 cm above and 0.5 cm below the squamo-columnar junction.
The primary outcome measures of this study were frequency and severity of the extra-esophageal GERD symptoms, including cough, sputum, wheezing, and globus hysterics. Data on these outcome measures were collected through a standardized questionnaire using the 6-point Likert scale system. More specifically, the frequency was graded as 0 (none), 1 (less than once per week), 2 (once or twice per week), 3 (three or four times per week), 4 (five or six times per week), and 5 (more than six times per week); the severity was graded as 0 (none), 1 (slight), 2 (mild), 3 (moderate), 4 (severe), and 5 (extremely severe). The total of the frequency and severity scores for each outcome measure was designated as the symptom score. Other outcome measures included medication independence, satisfaction, and reoperation complications. The questionnaires were prepared in simplified Chinese and administered to the subjects before LTF or the Stretta procedure and at 6 months and 1 and 3 years post-treatment.
Data were analyzed with SPSS 17.0 software (SPSS Inc., Chicago, IL, United States) and are presented as the mean ± SD for continuous variables and as frequencies and proportions for categorical variables. For the statistical analyses, normality was assessed by the Kolmogorov-Smirnov test. For continuous outcomes measured by the questionnaire, we performed comparisons between the 0- and 6-mo values and the 1- and 3-year values using the paired t-test or the Wilcoxon matched pairs signed rank sum test, as appropriate. To assess differences in outcomes between the Stretta and LTF procedures, we performed comparisons by the independent-samples t-test or Wilcoxon Mann-Whitney test, as appropriate. Analyses of dichotomous data (e.g., medication independence) were performed using the chi-square statistic. A P value less than 0.05 was considered statistically significant.
A total of 47 patients were included in the Stretta group, and 51 patients were included in the LTF group. Ninety-six patients were available at the 1-year follow-up, and 90 patients were available at the 3-year follow-up. In the Stretta group, one patient underwent re-operation during the first postoperative year, and six patients underwent re-operation within 3 postoperative years. The mean duration of the Stretta procedure was 50 min, and the mean duration of the Toupet procedure was 100 min. The average hospitalization period of patients who underwent the Stretta procedure was 4.4 d, and that of patients who underwent the Toupet procedure was 5.3 d. The baseline symptom scores were similar between the two groups (Table 1).
| Characteristic/parameter | Stretta (n = 47) | LTF (n = 51) | P value |
| Age (yr) | 45.9 ± 10.7 | 49.7 ± 11.5 | 0.095 |
| Male ratio, n (%) | 19 (40.4) | 28 (54.9) | 0.163 |
| Symptom score1 | |||
| Cough | 7.7 ± 0.57 (20/47) | 7.4 ± 0.82 (25/51) | 0.110 |
| Sputum | 7.5 ± 0.70 (19/47) | 7.4 ± 0.90 (19/51) | 0.560 |
| Wheezing | 7.7 ± 0.81 (29/47) | 7.9 ± 0.93 (33/51) | 0.181 |
| Globus hysterics | 7.4 ± 0.64 (27/47) | 7.2 ± 0.73 (28/51) | 0.171 |
There were no differences in the pre-treatment symptom scores between patients in the Stretta and LTF groups. The extra-esophageal symptom scores for cough, sputum, wheezing, and globus hysterics improved in both groups. Evaluation at the 3-year follow-up demonstrated a statistically significant improvement in all extra-esophageal symptoms of GERD (Figure 1). Differences in the improvement of symptom scores for cough, sputum, and wheezing between the two groups were not statistically significant. However, the score for globus hysterics in the Stretta group decreased to 4.9 ± 2.24, while that in the LTF group decreased to 3.2 ± 2.63 (P < 0.05) (Table 2).
From baseline to the 3-year follow-up, the mean patient satisfaction score improved from 28.19 to 51.49 in the Stretta group and from 31.76 to 69.80 in the Toupet group. Patients were more satisfied with their quality of life after undergoing LTF than after undergoing the Stretta procedure (P < 0.05) (Table 3).
| Characteristic/parameter value | 6-mo follow-up | 1-yr follow-up | 3-yr follow-up | ||||||
| Stretta (n = 47) | LTF (n = 51) | P value | Stretta (n = 47) | LTF (n = 51) | P value | Stretta (n = 47) | LTF (n = 51) | P value | |
| Symptom score | |||||||||
| cough | 3.9 ± 2.55 | 4.1 ± 2.65 | 0.780 | 4.2 ± 2.59 | 4.3 ± 2.72 | 0.921 | 4.6 ± 2.52 | 4.8 ± 2.36 | 0.785 |
| Sputum | 3.6 ± 2.24 | 4.0 ± 2.54 | 0.638 | 4.0 ± 2.32 | 4.3 ± 2.60 | 0.695 | 4.4 ± 2.29 | 4.7 ± 2.35 | 0.628 |
| Wheezing | 3.6 ± 2.26 | 3.9 ± 2.83 | 0.635 | 3.7 ± 2.28 | 3.9 ± 2.86 | 0.784 | 4.4 ± 2.23 | 4.4 ± 2.83 | 0.982 |
| Globus hysterics | 4.7 ± 2.30 | 3.0 ± 2.53 | 0.015 | 4.5 ± 2.38 | 3.2 ± 2.58 | 0.040 | 4.9 ± 2.24 | 3.2 ± 2.63 | 0.013 |
| PPI independence, n (%) | 32 (68.1) | 38 (74.5) | 0.510 | 31 (66.0) | 36 (70.6) | 0.668 | 29 (61.7) | 33 (64.7) | 0.835 |
| Satisfaction | 59.26 ± 34.80 | 72.55 ± 28.50 | 0.041 | 56.49 ± 34.78 | 72.16 ± 28.68 | 0.016 | 51.49 ± 32.77 | 69.80 ± 28.44 | 0.004 |
At baseline, 100% of the patients were on daily proton pump inhibitor (PPI) therapy. The rate of medication use decreased significantly from baseline following surgical intervention. PPI independence was defined as the complete elimination of PPI use or PPI use less than once weekly. There were no significant differences in any parameters measured between the different follow-up time points. After the Stretta and LTF procedures, 29 (61.7%) and 33 (64.7%) patients in each group achieved PPI therapy independence (61.7% vs 64.7%, P = 0.835).
No patients experienced perforation, infection, or death. The recorded complications after therapy included fever, pharyngeal pain, retrosternal discomfort, diarrhea, abdominal distention, and dysphagia. Most complications resolved without intervention within two weeks (Table 3). However, two patients still suffered from severe dysphagia at 2 wk post-operation in the LTF group, and it improved after bougie dilation treatment in both patients.
GERD is considered a significant public health problem. According to a population-based survey, the prevalence of symptom-defined GERD in China is 3.1%[9]. PPI therapy is the main option for the treatment of GERD-related extra-esophageal symptoms. A follow-up study showed that most GERD patients with chronic cough showed an improvement in that symptom after 2 years of medical treatment[10]. However, clinical experience shows that 20%-30% of patients with GERD continue to have persistent reflux symptoms even while taking a PPI daily[11]. Therefore, surgical and Stretta therapy should be considered in patients whose disease has failed to respond to medical management and in patients who are unwilling to consent to lifelong medicine intake or have extra-esophageal manifestations.
This prospective study investigated the efficacy and safety of the Stretta procedure and LTF surgical therapy in patients with extra-esophageal symptoms and compared the outcomes following these two therapeutic methods. Oelschlager et al[12] demonstrated that laparoscopic anti-reflux surgery improved atypical symptoms, such as cough and hoarseness. Our previous study showed that the Stretta procedure improves GERD-related respiratory symptoms[13]. In this study, both procedures effectively decreased the frequency and severity of GERD-associated extra-esophageal symptoms. We compared the clinical efficacy of the two therapeutic methods. No significant differences in the improvement of extra-esophageal symptoms, such as cough, sputum, or wheezing, and no difference in the frequency of PPI independence were observed between the two groups. However, LTF surgical therapy was more effective in improving globus hysterics.
Dr. Zhonggao Wang hypothesized four phases through which GERD insults the airway: (1) gastroesophageal phase, the generator; (2) pharyngeal phase, the reactor; (3) naso-oral phase, the effector; and (4) laryngotracheal phase, the asthmatic or laryngotracheal irritation/spasm stimulator[14]. The Stretta procedure is thought to improve the reflux barrier of the LES and to reduce transient LES relaxations that occur due to ablation or demodulation of vagal afferent fibers in the vicinity of the sphincter[15], while fundoplication is thought to significantly decrease acid exposure and significantly increase LES pressure[16]. In our previous study, laparoscopic LNF and Stretta RF were shown to be capable of effectively and safely controlling GERD symptoms in selected patients, but LNF showed a greater improvement of symptoms than Stretta RF[17]. In the current study, we compared LTF with Stretta RF to evaluate whether these different methods have similar abilities to control the different phases of GERD to provide a reference for clinical treatment.
This was an uncontrolled, nonrandomized study that did not include pH or motility outcomes. Regarding the medication requirement of GERD patients, the rate of PPI medication usage decreased significantly from baseline following surgical intervention. However, changes in respiratory drug use were not examined. In future research, we will include a larger study population and will evaluate changes in respiratory drug use.
In summary, through this 3-year prospective observational study, we demonstrated that LTF and the Stretta procedure were both effective in controlling GERD extra-esophageal symptoms and reducing PPI use. However, LTF achieved a greater symptom improvement and resulted in greater patient satisfaction.
Laparoscopic Toupet fundoplication (LTF) is a major anti-reflux surgical procedure for gastroesophageal reflux disease (GERD). The endoluminal technique for GERD (Stretta) was introduced in 2000. These two techniques are both minimally invasive treatments.
Although LTF and the Stretta procedure have been used to treat selected patients with GERD-related extra-esophageal symptoms as minimally invasive procedures, few studies have been conducted to compare the efficacy and safety of these two procedures.
To the authors’ knowledge, the study was the first to compare the efficacy and safety of these two procedures to determine which procedure is optimal for the treatment of GERD-related extra-esophageal symptoms.
This research showed that LTF and the Stretta procedure were both effective in controlling GERD-related extra-esophageal symptoms and reducing PPI use. LTF yielded a greater improvement of symptoms and resulted in greater patient satisfaction.
The results are worth to be published. Authors have to apply sample size analysis in order to justify their results in each of the primary outcomes (two means t-test for independent samples).
P- Reviewer: Sgourakis G S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Liu XM
| 1. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900-1920; quiz 1943. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 2. | Wang JH, Luo JY, Dong L, Gong J, Tong M. Epidemiology of gastroesophageal reflux disease: a general population-based study in Xi’an of Northwest China. World J Gastroenterol. 2004;10:1647-1651. [PubMed] [Cited in This Article: ] |
| 3. | Tsoukali E, Sifrim D. Investigation of extraesophageal gastroesophageal reflux disease. Ann Gastroenterol. 2013;26:290-295. [PubMed] [Cited in This Article: ] |
| 4. | Ciovica R, Gadenstätter M, Klingler A, Lechner W, Riedl O, Schwab GP. Quality of life in GERD patients: medical treatment versus antireflux surgery. J Gastrointest Surg. 2006;10:934-939. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Lundell L, Miettinen P, Myrvold HE, Hatlebakk JG, Wallin L, Malm A, Sutherland I, Walan A; Nordic GORD Study Group. Seven-year follow-up of a randomized clinical trial comparing proton-pump inhibition with surgical therapy for reflux oesophagitis. Br J Surg. 2007;94:198-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Velanovich V. Commentary on the SAGES Guidelines for Surgical Treatment of Gastroesophageal Reflux Disease. Surg Endosc. 2010;24:2645-2646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Shan CX, Zhang W, Zheng XM, Jiang DZ, Liu S, Qiu M. Evidence-based appraisal in laparoscopic Nissen and Toupet fundoplications for gastroesophageal reflux disease. World J Gastroenterol. 2010;16:3063-3071. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 40] [Cited by in F6Publishing: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Noar M, Squires P, Noar E, Lee M. Long-term maintenance effect of radiofrequency energy delivery for refractory GERD: a decade later. Surg Endosc. 2014;28:2323-2333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | He J, Ma X, Zhao Y, Wang R, Yan X, Yan H, Yin P, Kang X, Fang J, Hao Y. A population-based survey of the epidemiology of symptom-defined gastroesophageal reflux disease: the Systematic Investigation of Gastrointestinal Diseases in China. BMC Gastroenterol. 2010;10:94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Jaspersen D, Labenz J, Willich SN, Kulig M, Nocon M, Leodolter A, Lind T, Meyer-Sabellek W, Vieth M, Stolte M. Long-term clinical course of extra-oesophageal manifestations in patients with gastro-oesophageal reflux disease. A prospective follow-up analysis based on the ProGERD study. Dig Liver Dis. 2006;38:233-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Fass R. Proton-pump inhibitor therapy in patients with gastro-oesophageal reflux disease: putative mechanisms of failure. Drugs. 2007;67:1521-1530. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Oelschlager BK, Quiroga E, Parra JD, Cahill M, Polissar N, Pellegrini CA. Long-term outcomes after laparoscopic antireflux surgery. Am J Gastroenterol. 2008;103:280-287; quiz 288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Liang WT, Wu JM, Wang F, Hu ZW, Wang ZG. Stretta radiofrequency for gastroesophageal reflux disease-related respiratory symptoms: a prospective 5-year study. Minerva Chir. 2014;69:293-299. [PubMed] [Cited in This Article: ] |
| 14. | Wang ZG, Wu JM, Liu JJ, Wang LY, Lai YG, Ibrahim IM, Wang XJ, Dardik H. Respiratory distress resulting from gastroesophageal reflux is not asthma, but laryngotracheal irritation, spasm, even suffocation. Chin Med Sci J. 2009;24:130-132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Dughera L, Navino M, Cassolino P, De Cento M, Cacciotella L, Cisarò F, Chiaverina M. Long-Term Results of Radiofrequency Energy Delivery for the Treatment of GERD: Results of a Prospective 48-Month Study. Diagn Ther Endosc. 2011;2011:507157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD; SAGES Guidelines Committee. Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc. 2010;24:2647-2669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 299] [Cited by in F6Publishing: 318] [Article Influence: 22.7] [Reference Citation Analysis (1)] |
| 17. | Liang WT, Wu JN, Wang F, Hu ZW, Wang ZG, Ji T, Zhan XL, Zhang C. Five-year follow-up of a prospective study comparing laparoscopic Nissen fundoplication with Stretta radiofrequency for gastroesophageal reflux disease. Minerva Chir. 2014;69:217-223. [PubMed] [Cited in This Article: ] |