Published online Dec 7, 2012. doi: 10.3748/wjg.v18.i45.6674
Revised: July 27, 2012
Accepted: August 3, 2012
Published online: December 7, 2012
Endoscopic intervention is less invasive than percutaneous or surgical approaches and should be considered the primary drainage procedure in most cases with obstructive jaundice. Recently, therapeutic endoscopic retrograde cholangiopancreatography (ERCP) using double-balloon enteroscopy (DBE) has been shown to be feasible and effective, even in patients with surgically altered anatomies. On the other hand, endoscopic partial stent-in-stent (PSIS) placement of self-expandable metallic stents (SEMSs) for malignant hilar biliary obstruction in conventional ERCP has also been shown to be feasible, safe and effective. We performed PSIS placement of SEMSs for malignant hilar biliary obstruction due to liver metastasis using a short DBE in a patient with Roux-en-Y anastomosis and achieved technical and clinical success. This procedure can result in quick relief from obstructive jaundice in a single session and with short-term hospitalization, even in patients with surgically altered anatomies.
- Citation: Tsutsumi K, Kato H, Tomoda T, Matsumoto K, Sakakihara I, Yamamoto N, Noma Y, Sonoyama T, Okada H, Yamamoto K. Partial stent-in-stent placement of biliary metallic stents using a short double-balloon enteroscopy. World J Gastroenterol 2012; 18(45): 6674-6676
- URL: https://www.wjgnet.com/1007-9327/full/v18/i45/6674.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i45.6674
Endoscopic intervention is less invasive than percutaneous or surgical approaches and should be considered the primary drainage procedure in most cases with obstructive jaundice. Recently therapeutic endoscopic retrograde cholangiopancreatography (ERCP) using double-balloon enteroscopy (DBE) has been shown to be safe and feasible, even in patients with surgically altered anatomies[1-4]. On the other hand, the placement of biliary stents is effective for the palliation of unresectable malignant hilar biliary obstruction in conventional ERCP[5-8]. In particular, as we previously described, endoscopic partial stent-in-stent (PSIS) placement of self-expandable metallic stents (SEMSs) for malignant hilar biliary obstruction has been shown to be feasible, safe and effective[7,8], but it can be technically challenging. We report a case of a postoperative surgical patient who was managed successfully with a PSIS placement of SEMSs for malignant hilar biliary obstruction using a short DBE.
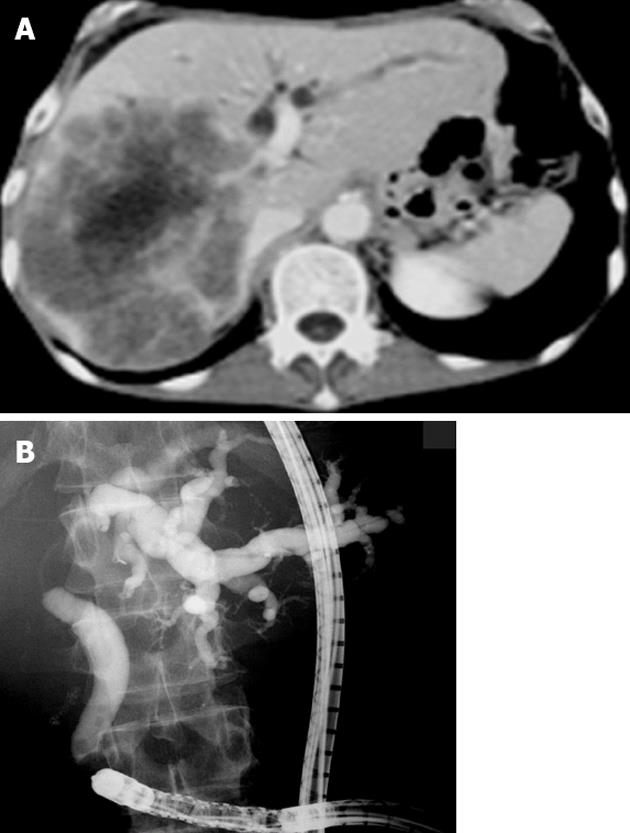
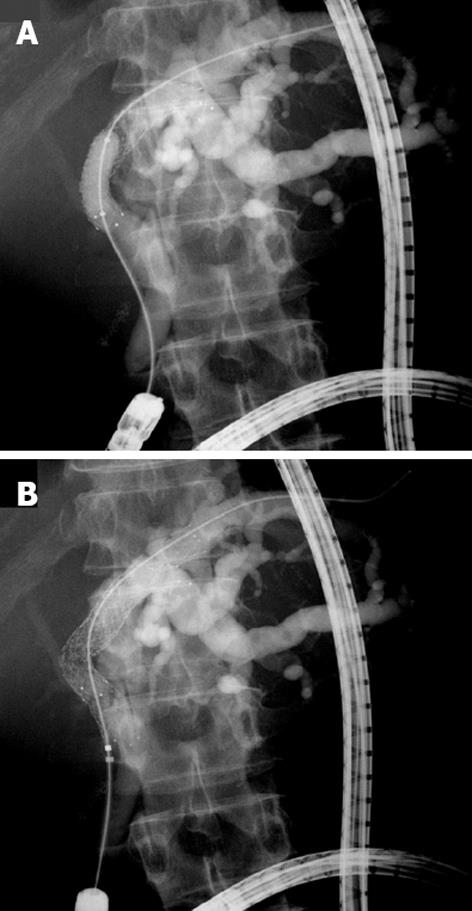
A 63-year-old male underwent total gastrectomy with Roux-en-Y reconstruction and sigmoidectomy due to simultaneous gastric and sigmoid colon cancer. Despite treatment with adjuvant chemotherapy, the patient’s liver and lymph node metastases increased and caused obstructive jaundice, but no cholangitis. Computed tomography imaging showed dilation of the left intrahepatic bile duct due to liver metastasis, which occupied the right lobe (Figure 1A). For endoscopic biliary drainage, endoscopic retrograde cholangiography with a short DBE, EC-450BI5 (Fujifilm, Tokyo, Japan), was performed. The cholangiography revealed hilar biliary obstruction and a dilated left intrahepatic bile duct with tumor invasion extending to the bifurcation of the left lateral sectional bile duct branches (Figure 1B). After needle-knife sphincterotomy, a 0.035-inch guidewire was passed selectively into the left lateral superior bile duct branch (B3). The first uncovered SEMS (Zeostent 10 mm × 80 mm; Zeon Medical Inc., Tokyo, Japan) was deployed, with the proximal end in B3 and the distal end in the common bile duct. The guidewire remained in place, and the delivery system was removed. Subsequently, the wire was passed by catheter into the left lateral inferior bile duct branch (B2) through the mesh of the initial SEMS. Following balloon dilation (8 mm) at the stricture (Figure 2A), the second uncovered SEMS (Zeostent 10 mm × 100 mm) was smoothly deployed, with the proximal end in B2 through the mesh of the initial SEMS, forming a PSIS (Figure 2B). The patient was immediately relieved of jaundice and left our hospital in 7 d. He recovered enough to receive another round of chemotherapy on an outpatient basis.
In patients with surgically altered anatomy and long afferent limbs, ERCP by gastroenteroscopy, colonoscopy, or standard duodenoscopy is technically challenging and often unsuccessful because of an inability to reach the papilla or bilioenteric anastomosis. Recently, the use of a DBE or single-balloon enteroscopy has made therapeutic ERCP-including sphincterotomy, stone extraction, dilation of bilioenteric anastomotic stricture, and biliary stent placement-feasible and effective, even in patients with surgically altered anatomies[1-4].
According to a recent report on endoscopic intervention for the relief of malignant hilar biliary obstruction, the placement of SEMSs offers advantages over plastic endoprostheses in terms of stent patency and the number of reinterventions needed[5]. In addition, endoscopic PSIS placement of SEMSs for malignant hilar biliary obstruction has been shown to be feasible, safe and effective in conventional ERCP[5-8]. We previously reported that this procedure is safe and effective even in cancer patients receiving chemotherapy[8].
Therefore, in this case of a cancer patient with Roux-en-Y anastomosis, we used a short DBE to perform PSIS placement of SEMSs for malignant hilar biliary obstruction and achieved technical and clinical success. Almost all conventional accessories, including uncovered SEMS, were available, as we used a short DBE with a working channel of 2.8 mm in diameter and a 152 cm in length.
Percutaneous stent insertion for malignant obstructive jaundice had significantly higher 30-d mortality than the endoscopic method (33% vs 15%, P = 0.016) in a randomized trial[9]. Complications related with percutaneous transhepatic biliary drainage (PTBD), including intraperitrial hemorrhage, hemobilia, bile leakage, and pleural complications, can be avoided by using endoscopic drainage[10]. In our cases, 2 PTBD routes would have been required for the placement of 2 SEMSs at B2 and B3, respectively. In addition, 2 sessions would have been required for the placement of the SEMSs, that is, the SEMSs are usually placed one week after the initial PTBD. The endoscopic procedure could protect our patient from the risks associated with more invasive drainage procedures, such as PTBD and surgical drainage, the latter of which is associated with high morbidity and mortality rates. Furthermore, the patient needed no further long-term hospitalization for the treatment of obstructive jaundice for the duration of his life. We think that this procedure is also indicated for patients in whom PTBD cannot be performed for various reasons, such as patients with severe coagulopathy, thrombocytopenia, a large amount of ascites, or an anatomically inaccessible location, e.g., patients with Chilaiditi syndrome.
In conclusion, endoscopic PSIS placement of SEMSs for the treatment of malignant hilar biliary obstruction using a short DBE was proved to be feasible and effective in a patient with Roux-en-Y anastomosis. This procedure can result in quick relief from obstructive jaundice in a single session and with short-term hospitalization, even in patients with surgically altered anatomies.
Peer reviewers: Dr. Herwig R Cerwenka, Professor, Department of Surgery, Medical University of Graz, Auenbruggerplatz 29, A-8036 Graz, Austria; Atsushi Nakajima, Professor, Division of Gastroenterology, Yokohama City University Graduate School of Medicine, 3-9 Fuku-ura, Kanazawa-ku, Yokohama 236-0004, Japan
S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 158] [Cited by in F6Publishing: 170] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 2. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 160] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 3. | Mönkemüller K, Fry LC, Bellutti M, Neumann H, Malfertheiner P. ERCP with the double balloon enteroscope in patients with Roux-en-Y anastomosis. Surg Endosc. 2009;23:1961-1967. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Gerges C, Schumacher B, Terheggen G, Neuhaus H. Expandable metal stents for malignant hilar biliary obstruction. Gastrointest Endosc Clin N Am. 2011;21:481-497, ix. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Chahal P, Baron TH. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest Endosc. 2010;71:195-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Kawamoto H, Tsutsumi K, Fujii M, Harada R, Kato H, Hirao K, Kurihara N, Nakanishi T, Mizuno O, Ishida E. Endoscopic 3-branched partial stent-in-stent deployment of metallic stents in high-grade malignant hilar biliary stricture (with videos). Gastrointest Endosc. 2007;66:1030-1037. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Kawamoto H, Tsutsumi K, Harada R, Fujii M, Kato H, Hirao K, Kurihara N, Nakanishi T, Mizuno O, Ishida E. Endoscopic deployment of multiple JOSTENT SelfX is effective and safe in treatment of malignant hilar biliary strictures. Clin Gastroenterol Hepatol. 2008;6:401-408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Speer AG, Cotton PB, Russell RC, Mason RR, Hatfield AR, Leung JW, MacRae KD, Houghton J, Lennon CA. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet. 1987;2:57-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 481] [Cited by in F6Publishing: 423] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 10. | Yee AC, Ho CS. Percutaneous transhepatic biliary drainage: a review. Crit Rev Diagn Imaging. 1990;30:247-279. [PubMed] [Cited in This Article: ] |