Published online Jun 28, 2010. doi: 10.3748/wjg.v16.i24.3040
Revised: March 22, 2010
Accepted: March 29, 2010
Published online: June 28, 2010
AIM: To evaluate the predisposing factors for peritoneal perforation and intrabiliary rupture and the effects of these complications on surgical outcome in liver hydatid disease.
METHODS: A total of 372 patients with liver hydatid cysts who had undergone surgical treatment were evaluated retrospectively. Twenty eight patients with peritoneal perforation, 93 patients with spontaneous intrabiliary perforation, and 251 patients with noncomplicated hydatid cysts were treated in our clinics.
RESULTS: When the predisposing factors for complications were evaluated, younger age, superficial position, and larger cyst dimensions (P < 0.05; range, 0.001-0.017) increased peritoneal perforation rates. It was shown that older age increased cyst dimensions, and presence of multiple and bilobar cysts increased intrabiliary rupture rates (P < 0.05; range, 0.001-0.028). Partial pericystectomy and drainage was the most frequent surgical procedure in all groups (71.6%). The incidence of post-operative complications in the peritoneal perforated group, in the intrabiliary ruptured group, and in the noncomplicated group was 25%, 16.1% and 5.5%, respectively. When compared, complication rates were significantly different (P = 0.002). When length of hospital stay was compared, there was no significant difference between the groups (P > 0.05). The overall recurrence rate was 3.8% (14 patients), but there was not any statistical difference among the patient groups (P = 0.13). The early postoperative mortality rate was 1.1%.
CONCLUSION: In peritoneally perforated and intrabiliary ruptured cases, the most important steps are irrigation of the peritoneal cavity and clearance of the cystic material from the biliary tree.
- Citation: Akcan A, Sozuer E, Akyildiz H, Ozturk A, Atalay A, Yilmaz Z. Predisposing factors and surgical outcome of complicated liver hydatid cysts. World J Gastroenterol 2010; 16(24): 3040-3048
- URL: https://www.wjgnet.com/1007-9327/full/v16/i24/3040.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i24.3040
Echinococcosis is a zoonosis transmitted by dogs that accidentally infects humans. Both sheep and humans are intermediate hosts. Developing countries with poor hygiene where sheep and cattle are raised are high-risk areas for acquiring cystic echinococcosis. Endemic regions of human cystic disease include South America; the Mediterranean region, including North Africa, Spain, Portugal, and Turkey; the Middle East; central Asia; and many regions in China[1,2]. The prevalence of the disease increased in Europe and North America in recent years. In the United States and Europe, most infections are seen in immigrants from endemic areas[3].
In humans, 50% to 75% of hydatid cysts occur in the liver, 25% are found in the lungs, and 5% to 10% are distributed along the arterial system[4]. The majority of the patients have single-organ involvement (87%) and a solitary cyst (72%) at the right part of the liver[5]. If the cyst ruptures, scolices can grow in the peritoneum, pleura, bronchial tree, and bile ducts[5-7]. Cyst sizes range from 1 to 30 cm, and cyst growth varies from 1 to 30 mm per year[6,8].
The clinical picture can be severe, and complications may occur, making the already difficult treatment even more so[9,10]. Complications are observed in one third of patients with liver hydatid cysts. In large series, incidences of peritoneal perforation were reported at between 10% and 16%[11,12], and communications between the cyst and the biliary tree are seen in 9% to 25% of cases[13-15]. Without treatment, cysts grow and eventually may form fistulas into the peritoneal cavity or intrabiliary rupture, requiring emergency surgery[2,9,10]. Operative treatments vary from complete resection to minimal invasive procedures, but the ideal treatment is still controversial[16,17]. The choice of therapy depends on several factors: number and localization of the cysts, surgeon expertise, and presence of complications.
Only a few studies have reported the management and outcome of patients with complicated liver hydatid disease[13,18]. Surgery is the mainstay of treatment, although there is no consensus on the respective advantages of conservative and radical methods. Besides, in the treatment of peritoneal perforated cases, profuse peritoneal lavage with hypertonic solutions appears to be more necessary; in the setting of intrabiliary rupture, T-tube drainage, sphincteroplasty, and choledochoduodenostomy are appropriate treatment strategies to reduce the pressure in the biliary tree. In this study, we aimed to evaluate the predisposing factors for peritoneal perforation and intrabiliary rupture and the effects of these complications on morbidity, length of hospital stay (LOS), mortality, and recurrence in hydatid disease.
We retrospectively evaluated medical records of 372 patients with liver hydatid cysts who were admitted to the Department of General Surgery, Faculty of Medicine, Erciyes University, between June 1990 and January 2008. In this period, 28 patients with peritoneal perforation (group I), 93 patients with spontaneous intrabiliary perforation (group II), and 251 patients with noncomplicated hydatid cysts (group III) were treated in our clinics. The ratios of intrabiliary rupture and peritoneal perforation cases to noncomplicated cases were 37% and 11.1%, respectively.
Patient age and sex, initial complaints, physical findings, cyst characteristics, imaging results, surgical procedures, reasons for peritoneal perforation and intrabiliary rupture, morbidity, LOS, recurrence rates, and mortality were evaluated. The patients with extrahepatic organ involvement were excluded.
The preoperative evaluation included blood tests (complete blood count, blood type, liver function tests), chest radiography, abdominal ultrasonography (US), and computed tomography (CT). Chest and abdominal radiography and abdominal US were performed in all patients at admission. The most important indications for CT were a need for additional anatomical and cystic details, the presence of multiple hydatid cysts, findings of a solid appearance, and findings of cyst infection. If intrabiliary rupture was suspected, magnetic resonance imaging (MRI) cholangiography was performed. Intraoperative ultrasound (IOUS) was used for identification of intraparenchimal cyst localization and selection of the best approach sight.
In all cases of liver hydatid cysts, the area around the cyst was covered with packs soaked in 3% hypertonic saline solution to prevent the further spread of the parasite during evacuation of the cyst. Cyst contents were aspirated from a suitable surface with a needle, which opened a nearly 1-2 cm incision; this was examined carefully for bile content. Subsequently, an aspirator was inserted into the cystic cavity to empty the remaining fluid, and then the incision was widened. The germinative membrane and daughter cysts were removed with forceps or spoons. With the roof excision of the redundant part of the cyst, an excellent exposure was obtained. After evacuation of the cyst, the cyst cavity was irrigated with 3% hypertonic saline for 10-15 min. Any orifices of bile ducts observed on the inner surface of the cavity were sutured with nonabsorbable sutures. To prevent peritoneal spreading in peritoneally perforated cases, the abdominal cavity was irrigated with 3% hypertonic saline or with povidone-iodine. Next, a surgical procedure, such as partial pericystectomy (PP) and capitonnage, PP and omentoplasty, PP and drainage, or PP and intraflexion, was performed. For pericystectomy, the hepatic pedicle was prepared for the Pringle maneuver. The cyst was then dissected along its boundary with healthy liver tissue. Blood vessels and small biliary structures passing through the plane between normal liver tissue and the cyst were clamped and divided. If the patient was fit and the cysts were away from the hepatic veins, large bile ducts, or major branches of the portal vein and hepatic artery, pericystectomy was performed. Liver resections were performed only if multiple cysts were localized in one lobe and peripherally.
If the preoperative evaluation suggested a probability of a connection between the cyst and the biliary duct, or this was suspected during surgery, choledochotomy, placement of a T-tube, and an intraoperative cholangiographic and/or choledochoscopic evaluation were performed. In the case of any doubt about free biliary drainage, biliodigestive anastomosis or sphincteroplasty was added.
Since 1993, medical treatment for hydatidosis has consisted of albendazole 10 mg/kg per day (Andazol, Biofarma, Istanbul, Turkey), beginning after surgery and continuing for 3 mo. Until 5 years ago, the therapy was performed over 3 mo and included 20 d of drug administration and 10 d drug free intervals. Over the last 5 years, the drug has been administered continuously with monthly blood liver function tests and complete blood count controls.
During follow-up, US was performed twice a year for 2 years, and then annually. CT scans were performed as needed.
Differences among categorical variables were compared using χ2 tests, and Kruskal-Wallis tests were used for age, diameter, and number of cysts and LOS. Multinominal logistic regression analysis was performed to analyze the effects of variables (age; sex; previous hydatid disease surgery; location, number, position, and presence of cyst infection) influencing peritoneal perforation or biliary rupture. Data were analyzed with the SPSS software package (version 13.0; SPSS, Inc., Chicago, IL). Significance was set at P < 0.05.
The mean age (mean ± SD) of peritoneal perforated and intrabiliary ruptured patients was 36.32 ± 11.86 and 50.26 ± 13.88, respectively. When calculated, it was 45.62 ± 16.01 in the noncomplicated group. The mean age factor in the peritoneal perforation group was significantly different from others (P = 0.001). The sex ratio of the patients was not statistically different among the groups (P = 0.95, Table 1).
| Characteristic | Group I (n = 28) | Group II (n = 93) | Group III (n = 251) | P |
| Age1 (yr) | 0.001b | |||
| mean ± SD | 36.32 ± 11.86 | 50.26 ± 13.88 | 45.62 ± 16.01 | |
| Median (range) | 37.0 (17-76) | 53.0 (23-76) | 43.0 (18-79) | |
| Sex | 0.950 | |||
| Male | 15 (53) | 51 (55) | 141 (56) | |
| Female | 13 (47) | 42 (45) | 110 (44) | |
| Previous hydatid disease surgery | 0.204 | |||
| No | 24 (86) | 74 (80) | 219 (87) | |
| Yes | 4 (14) | 19 (20) | 32 (13) | |
| Localization | 0.109 | |||
| Right lobe | 17 (61) | 54 (58) | 178 (71) | |
| Left lobe | 5 (18) | 25 (26) | 48 (19) | |
| Bilateral | 6 (21) | 14 (16) | 25 (10) | |
| No. of cysts1 | 0.284 | |||
| 1 | 22 (78) | 61 (66) | 193 (77) | |
| 2 | 4 (14) | 17 (18) | 39 (16) | |
| 3 | 1 (4) | 7 (8) | 16 (6) | |
| 4 | 1 (4) | 5 (5) | 3 (1) | |
| 5 | - | 3 (3) | - | |
| Cyst diameter1 (cm) | 9.5 (4-24) | 10 (6-29) | 7 (3-31) | 0.001b |
| Position | 0.017b | |||
| Superficial | 24 (86) | 52 (56) | 155 (62) | |
| Deep | 4 (14) | 41 (44) | 96 (38) | |
| Cyst infection | 0.683 | |||
| Negative | 26 (93) | 89 (95) | 234 (93) | |
| Positive | 2 (7) | 4 (5) | 17 (7) | |
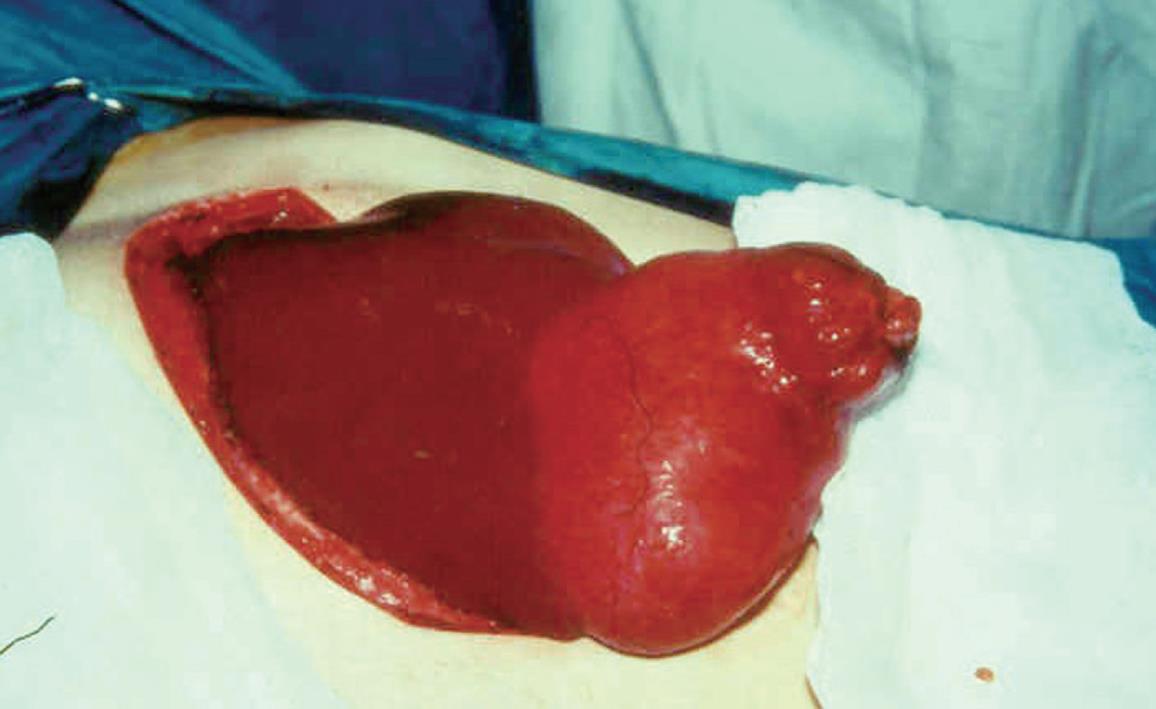
Previous hydatid disease surgery, cyst localization, number of cysts, and presence of infection were not statistically different among groups (P > 0.5; range, 0.109-0.683), whereas the differences in cyst diameters and positions (superficial or deep) were significant (P = 0.001 and 0.017, respectively; Table 1). Macroscopic appearance of an hydatid cyst that originates in the right lobe of the liver was seen in Figure 1.
The most common complaint was abdominal pain in all groups (67%). Other common complaints were nausea, vomiting, abdominal distension, and allergenic reactions in peritoneally perforated cases, jaundice (21%) in intrabiliary ruptured cases, and abdominal swelling (41%) in noncomplicated hydatid cysts. The most common physical examination findings were abdominal sensitivity and guarding (100%), acute abdomen findings (39%), distension (22%) in peritoneally perforated cases, hepatomegaly (28%) and jaundice (21%) in intrabiliary ruptured cysts, and finally, hepatomegaly (27%) in noncomplicated patients. In 49 (13%) patients, diagnosis was made incidentally by abdominal US or CT during a medical checkup or after a trauma.
When the predisposing factors for complications were evaluated, younger age, superficial position, and larger cyst dimensions increased peritoneal perforation rates. It has been seen that older age, increased cyst dimensions, and presence of multiple and bilobar cysts increases intrabiliary rupture rates. Sex, primary or recurrent disease, and cyst infection were not as effective variables in both logistic models (Table 2).
| Factor | Group I vs group III | Group II vs group III | ||
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Sex | ||||
| Male | 1.00 | 1.00 | ||
| Female | 1.61 | 0.68-3.77 | 1.10 | 0.65-1.87 |
| Age | 0.59 | 0.41-0.84 | 1.30 | 1.07-1.57 |
| Occurrence type | ||||
| Primary occurrence | 1.00 | 1.00 | ||
| Recurrence | 0.81 | 0.23-2.77 | 1.33 | 0.66-2.65 |
| Localization | ||||
| Unilobar | 1.00 | 1.00 | ||
| Bilateral | 1.48 | 0.86-2.55 | 1.54 | 1.07-2.21 |
| No. of cysts | 1.21 | 0.65-2.23 | 1.80 | 1.30-2.50 |
| Cyst diameter (cm) | 1.11 | 1.04-1.19 | 1.12 | 1.07-1.57 |
| Position | ||||
| Superficial | 1.00 | 1.00 | ||
| Deep | 0.27 | 0.09-0.84 | 1.40 | 0.18-4.33 |
| Cyst infection | ||||
| Positive | 1.00 | 1.00 | ||
| Negative | 1.02 | 0.20-5.11 | 0.58 | 0.17-2.01 |
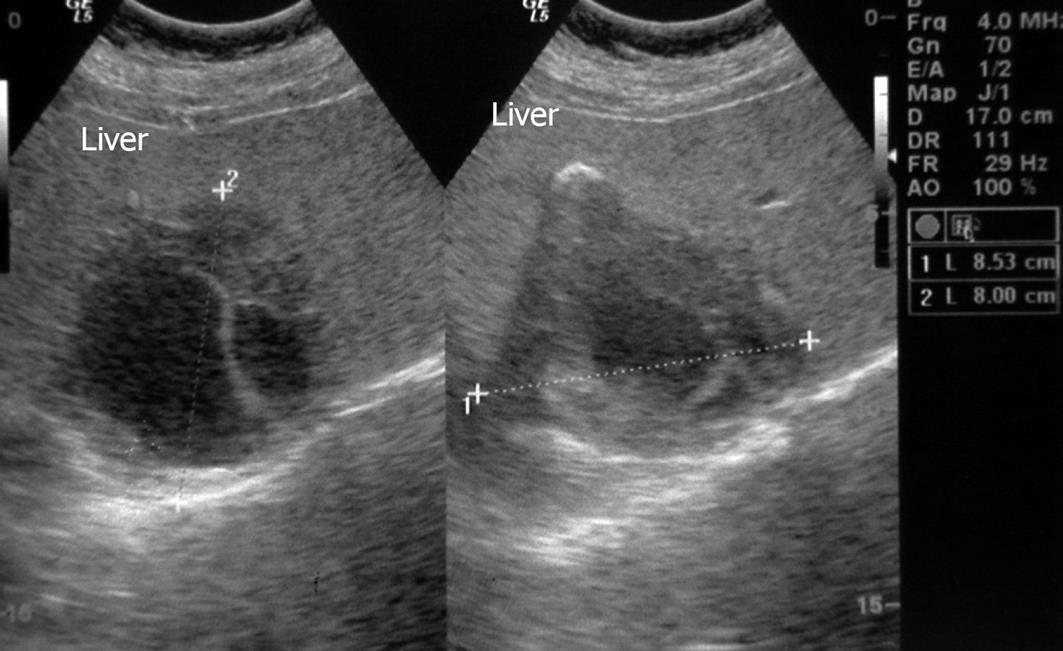
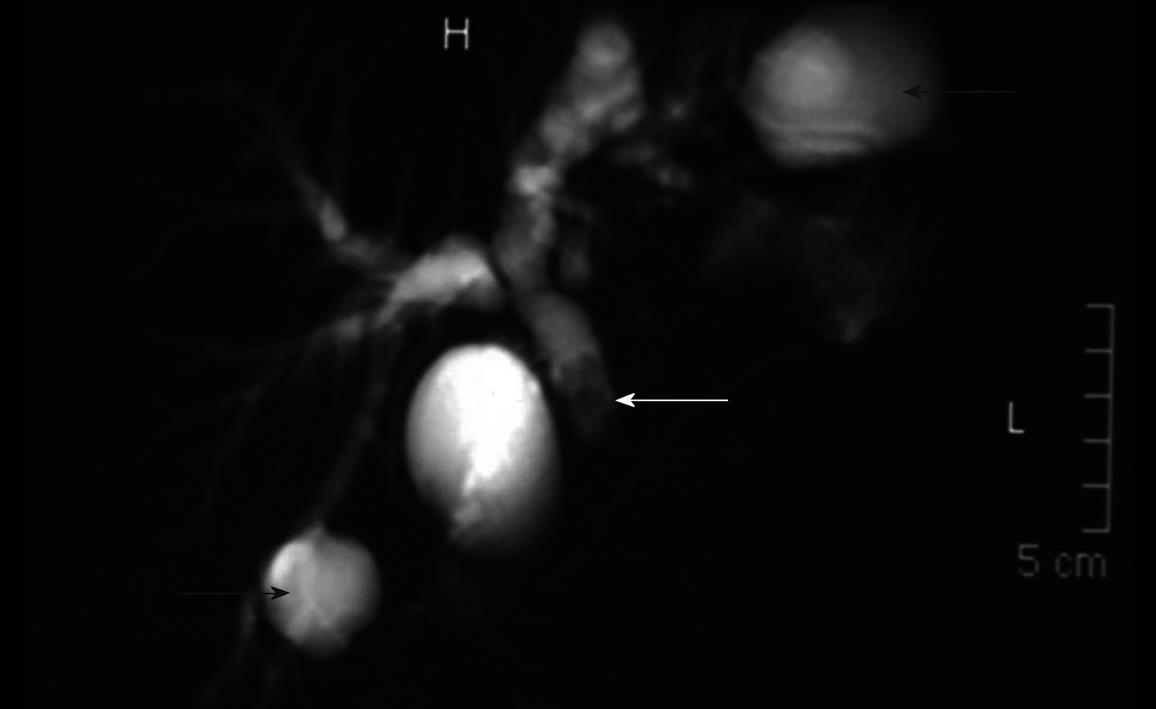
Abdominal US was done in 326 (87.6%) patients and demonstrated hepatic cysts with 96.7% sensitivity (Figure 2). CT was used as the second most frequent (n = 148, 46%) diagnostic modality, with 96.5% sensitivity. In 24 (6.5%) patients with intraparenchymal cysts, IOUS was performed for identification of cyst localization and selection of the best approach sight. MRI cholangiography was performed after 1996 to assess the spread of disease to the biliary tree but was not used routinely and was done in 37 patients (9.9%) (Figure 3). The indications for MRI cholangiography are the presence of jaundice seen during the physical examination, elevation of serum bilirubin and alkaline phosphatase levels, and other obstructive jaundice symptoms and demonstrated 98% sensitivity.
Surgical procedures used for the cysts of the 372 patients are shown in Table 3. Partial pericystectomy and drainage was the most frequent surgical procedure in all groups. Three of 4 jaundiced patients underwent cholecystectomy plus T-tube drainage, and the other patient underwent cholecystectomy plus sphincteroplasty in the peritoneal perforation group. In all intrabiliary rupture cases, cholecystectomy and common bile duct exploration were performed. Intraoperative cholangiography was performed in all patients, and choledochoscopy was also performed in 62 (66.6%) patients. Cyst remnants and daughter vesicles in the bile ducts were evacuated with Dormia forceps or a Fogarty catheter in 16 (17.2%) patients. A T-tube drainage was performed in 72 (77.4%) patients, choledochoduodenostomy was performed in 15 (16.1%) patients, and sphincteroplasty was performed in 6 (6.4%) patients.
| Surgical procedure | No. of cysts (%) | ||
| Group I (n = 28) | Group II (n = 93) | Group III (n = 251) | |
| Main surgical procedure | |||
| PP and drainage | 26 (70.3) | 101 (67.8) | 231 (73.5) |
| PP and omentoplasty | 2 (5.4) | 13 (8.7) | 26 (8.3) |
| PP and capitonnage | 2 (5.4) | 11 (7.4) | 20 (6.4) |
| PP and intraflexion | - | 3 (2.0) | 8 (2.6) |
| Pericystectomy | 5 (13.5) | 14 (9.4) | 19 (6.0) |
| Liver resection | 2 (5.4) | 7 (4.7) | 10 (3.2) |
| Total No. of cysts | 37 | 149 | 314 |
| Additional surgical procedure | |||
| Choledochotomy and T-tube | 3 (10.7) | 77 (82.8) | 7 (2.7) |
| Choledochotomy and choledochoduodenostomy or sphincteroplasty | 1 (3.5) | 16 (17.2) | 2 (0.8) |
The most frequent postoperative complications were wound infection (5.6%) and pulmonary complications (2.9%). In the peritoneal perforation group, 10 surgical complications occurred in 7 (25%) patients; in the intrabiliary rupture group, 18 complications occurred in 15 (16.1%) patients; and in the noncomplicated group, 16 complications occurred in 14 (5.5%) patients. When compared, complication rates were significantly different (P = 0.002, Table 4). When compared according to Dindo & Clavien Classification of Surgical Complications[19], the differences between grade I, grade IVa and grade IVb surgical complications were not significant (P > 0.05, range, 0.08-0.57), however differences between grade II, grade IIIa and grade IIIb complications were statistically significant (P < 0.05; range, 0.003-0.036).
| Group I (n = 28) | Group II (n = 93) | Group III (n = 251) | P | |
| Medical complications1 | 0.163 | |||
| Cardiac | 1 (3.6) | 1 (1.1) | 3 (1.2) | |
| Respiratory | 2 (7.2) | 3 (3.2) | 6 (2.4) | |
| Other | 1 (3.6) | 2 (2.2) | 4 (1.6) | |
| Surgical complications | ||||
| Wound infection | 6 (21.4) | 6 (6.5) | 9 (3.5) | 0.001b |
| Biliary fistula | 1 (3.6) | 9 (9.7) | 2 (0.8) | 0.001b |
| Intra-abdominal abscess | - | 1 (1.1) | 2 (0.8) | 0.855 |
| Incisional hernia | 2 (7.2) | 2 (2.2) | 3 (1.2) | 0.087 |
| Gastrocutaneous fistula | 1 (3.6) | - | - | 0.002b |
| Recurrence | 3 (10.7) | 3 (3.2) | 8 (3.2) | 0.132 |
| Mortality | - | 1 (1.1) | 3 (1.2) | 0.844 |
Median postoperative LOS in the peritoneal perforation group, intrabiliary ruptured group, and noncomplicated group were 12 (range, 5-21), 13 (range, 5-37), and 9 (range, 4-19) d, respectively. When LOS was compared, there was no significant difference between the groups (P > 0.05). According to the additional surgical procedures, the median LOS was 8 (range, 4-19) d in patients on which choledochotomy had not been performed, compared to 15 (range, 11-37) d in the choledochotomy with T-tube group and 10 (range, 6-13) d in the bilioenteric anastomosis group. There was a significant difference in LOS between the groups with choledochotomy with T-tube and without choledochotomy (P < 0.05). In contrast, no difference between the groups with biliodigestive anastomosis and without choledochotomy was seen (P > 0.05).
The follow-up data were complete for 28 (100%) of the peritoneal perforated group, 76 (82%) of the intrabiliary ruptured group, and 198 (79%) of the noncomplicated group. The mean follow-up periods were 37.3 ± 26.3 (range, 2-144) mo. The overall recurrence rate was 3.8% (14 patients), but there was not any statistical difference among the patient groups (P = 0.13, Table 4). The early postoperative mortality rate was 1.1% (n = 4). The causes of death were pulmonary embolism in one patient, myocardial infarct in one patient, and postoperative hemorrhage in two patients (Table 4). These causes were identified clinically, without necropsy.
Peritoneal perforation into the abdominal cavity and the spontaneous intrabiliary rupture of liver hydatid disease are not rare complications and cause serious problems. In our study, the ratios of peritoneal perforation and intrabiliary rupture cases to noncomplicated cases were 11.1% and 37%, respectively. The most common complication is rupture of the cyst, either internally or externally, followed by anaphylactic reaction and jaundice[5,9,10]. Systemic anaphylactic reactions have been reported in 1% to 12.5% of patients with intraperitoneal perforation, and these reactions may be life threatening[9,10]. Jaundice is the most important sign of intrabiliary rupture within a range of 9% to 30%[20,21]. In patients with peritoneal perforation and intrabiliary rupture, specific management has not been evaluated sufficiently. The presence of complications must be considered in the surgical treatment.
One third of 372 patients (32.5%) who underwent an operation for liver hydatid disease presented with complications. When compared, sex factor was not statistically different among groups (P = 0.95), but the mean age in the peritoneal perforated group was significantly different (P = 0.001, Table 1). Trauma is the most frequent etiological cause of perforation[9,22]. No patients in the current series experienced spontaneous peritoneal rupture. Hydatidosis is endemic in Turkey and the frequency of traffic accidents there is high[23]. Traffic accidents generally affect younger individuals, and the age risk factor found in our study may relate to this phenomenon. In superficial and bigger cysts, lack of normal liver tissue around the cyst to protect against trauma may be a cause of frequent rupture.
The differences in factors such as previous hydatid disease surgery, cyst localization, cyst number, and cyst infection were not significant among groups (P > 0.05, range, 0.109-0.683). Besides age, cyst diameter and cyst position (superficial or deep) were also significantly different factors (P = 0.001 and 0.017, respectively; Table 1). When compared to the same parameters with multinominal logistic regression analyses, young age, superficial position, and large diameter are significant predisposing factors for peritoneal perforation (Table 2). The hydatid cyst wall consists of an inner germinal layer and an outer laminated membrane. Surrounding the wall is the pericyst, which has an outer zone of compressed liver cells. A lack of presence of normal liver tissue around superficial cysts plays a role in relatively higher perforation rates. Similarly, an increase in cyst diameter may increase perforation risk either by becoming more superficial during growth or by increasing intracystic pressure.
Additionally, liver hydatid cysts at the dome of the liver grow progressively and have a tendency to erode the diaphragm[24]. In our study, it has been shown that older age, bigger dimensions, multiplicity of the cysts, and bilobar cysts are predisposing factors for intrabiliary rupture. The relationship between older age and intrabiliary rupture probably depends on cyst age. Hydatid disease is a slowly growing disease, and in early times, most of the cysts produce no symptoms. In advanced cases, the intracystic pressure may cause tension on cyst walls and thinner wall formations. The communications between the cysts and the biliary tree usually involve small cholangioles, and direct extension into major bile ducts is rare[25,26]. The most probable theory may be the fenestration of the cyst and minor bile ducts, which have low pressure in the surrounding liver tissue. In the case of multiple and bilobar cysts, this communication rate may increase. Factors such as sex, primary or recurrent disease, or infection did not show effectiveness in both logistic models (Table 2).
Cyst dimension and age (younger age for peritoneal perforation and older age for intrabiliary rupture) have been determined as significant predisposing factors for the two complications. We do not believe a direct relationship exists between the two complications, but we can speculate that risk of peritoneal perforation risk may decrease in intrabiliary ruptured cysts because of the lower intracystic pressure probability. In our study the ratio of intrabiliary ruptured cysts was 97 out of 372 (26%), whereas intrabiliary rupture was 4 out of 28 (14.3%) peritoneally perforated cases, but this was not statistically significant.
The principles of hydatid surgery are (1) removal of all infective cyst parts; (2) inactivation of the cyst cavity; (3) avoidance of intra-abdominal spillage of cyst contents; and (4) management of the residual cavity. A lot of surgical techniques have been proposed for liver hydatid disease during the last three decades. Some authors suggest that obliteration procedures, such as capitonnage, intraflexion, or omentoplasty, are simple and safe methods[27]. In the past, obliteration procedures such as omentoplasty, capitonnage, and intraflexion were used for most patients in our clinic. However, in the last 10 years use of these management options decreased gradually and for the last 5 years we have not shown a preference for them. Recently, some authors have favoured the use of pericystectomy and liver resections because complete surgical resection is the ideal treatment for hydatid disease[18]. In our study, liver resections were performed only if multiple cysts were localized in one lobe, located peripherally, and were pedunculated, and pericystectomy was performed if the cysts were away from the major vascular and biliary structures of the liver. The most important advantages of these resections are that no dead space is left behind and that all the cyst wall is removed, which prevents liver regeneration. The need for sufficient technical infrastructure and surgical experience in the field of hepatic surgery limit these treatments in small centers, especially in developing countries. Relatively small-sized subcapsular cysts can be managed by nonanatomic resection of the cysts with a rim of healthy hepatic tissue but routine application of pericystectomy and liver resection may increase the operative complications, such as bleeding and postoperative morbidity and mortality.
For almost 15 years, our preferred surgical technique for treatment of liver hydatid cysts has been PP and drainage, which has been performed in 70% of the patients (Table 3). Leaving the cyst cavity open, the peritoneum has more support in recent years[13]. After controlling the relation between the biliary tree, it has been stated that this procedure does not increase recurrence or cause adhesion. The most important superior aspect of this technique is its applicability to every cyst at every localization. Other advantages of the procedure are the simplicity, no requirement of advanced experience, effectiveness, and a shorter operation time. The most important detail of this procedure in our experience is to perform the partial pericystectomy as widely as possible, and the drainage procedure should be added after the cyst contents are removed completely. After the cyst management, in peritoneal perforated cysts, the most important step is irrigation of the peritoneal cavity with a sufficient amount of scolicidal agents and removal of all cystic content, and in intrabiliary ruptured cases, clearance of the cystic material from the biliary tree is most important; also, the restoration of normal bile flow should be performed. The fistula was large enough to allow daughter cysts and debris to migrate into the biliary tree. For this reason introperative cholangiography was performed in all patients who presented with abnormal liver function tests preoperatively, bile-stained cyst fluid, and bile leak from the cyst wall. During the introperative cholangiography, visible bile fistulas must be sutured by using late absorbable suture materials.
After the intervention to the cyst, the most important step is irrigation of the cyst cavity with a sufficient amount of scolicidal agents and careful removal of all cystic content from the patient. Numerous solutions, such as hypertonic saline solutions (15%-30%), have been used as scolicidal agents for the purpose of inactivation[5,28]. The concentration of hypertonic saline solutions has diminished gradually. Now we use only 3% concentrations. Gargouri et al[29] used 3%-5% saline and stated that the application time is more important than the concentration. Although Derici et al[30] reported that hypertonic saline is not appropriate because it may damage the peritoneal surfaces and may cause hypernatremia, we have not encountered any significant complications with the use of this solution. Additionally, we believe that profuse peritoneal lavage with hypertonic sodium chloride is mandatory for preventing intra-abdominal recurrence of intraperitoneal ruptured hydatid disease.
The most effective surgical procedures following the cleaning of hydatid material from the biliary tree remain controversial. Some authors prefer T-tube[13-15]; in contrast, some reported that wide choledochoduodenostomy decreases morbidity and mortality[31]. In our study, complication rates in patients with bilioenteric anastomosis and T-tube were 21% and 27%, respectively.
In the literature, reported complication rates are between 6% and 47%; recurrence rates are 8% to 15%[32]. In this study, the overall postoperative complication and recurrence rates were 18% and 3.8%, respectively. Most often, surgical complications were wound infection (n = 21) and biliary fistulas (n = 12); the difference between groups was significant (P = 0.001, Table 4). The important causes of higher wound infection rates in the peritoneal perforation group were coinjuries, which were seen in 10 patients. There were small intestine and colon perforations in five cases; in addition, splenic, pancreatic, and renal injuries were each seen in one patient. Retroperitoneal hematoma was seen in the remaining two coinjured patients. External biliary fistulas did not develop in 68 of the T-tube patients and in none of the biliodigestive anastomosis or sphincteroplasty patients in the intrabiliary rupture group. T-tubes were removed after a control cholangiography, which was done after a mean period of 12 d postoperatively. External biliary fistulas developed in 9 (9.7%) patients. If the fistulas did not close with conservative follow-up, endoscopic sphincterotomy was performed after a mean period of 19 d. The causes of fistulas were remnant germinal vesicles and debris in the distal common bile duct in 5 patients and papillary stenosis in 4. In the peritoneally perforated and noncomplicated groups, biliary fistulas developed in 3 patients who had hepatic resections, and the problem was resolved with endoscopic sphincterotomy. Endoscopic procedures have been used not only for diagnostic purposes, but for treatment as well. Dumas et al[33] treated 7 of 28 patients with cholangitis due to cystic material with ERCP. Tekant et al[34] and Vignote et al[35] reported that endoscopic sphincterotomy achieved closure of fistulas within 5-7 d. In our series, fistulas closed in all external biliary fistula patients within a mean time of 7 d (range, 3-17). At our center, intraoperative cholangiography with or without subsequent duct exploration remains the method of choice to prevent or decrease incidence of associated injuries and external biliary fistula. Several authors have advocated pre-operative or post-operative ERCP[33-35]. If performed in conjunction with a sphincterotomy, an ERCP may be used to clear the biliary tree as a planned procedure, thereby avoiding the need for an intraoperative cholangiography and bile duct exploration.
Recurrence occurred in 14 nonperforation cases (3.8%). When compared with the reported rates, the recurrence of our study is low. The cause of this may be the routine use of albendazol for 3 mo postoperatively. Recurrence rates were not significantly higher in peritoneal perforation and intrabiliary rupture cases when compared with noncomplicated cases (P = 0.132, Table 4). Recurrences of hydatid disease are usually due to inadequate cystic content removal, spillage of cystic liquid intraoperatively, undetected cysts, and satellite lesions and reinfestations. Readmissions in our series due to recurrent disease were generally after a long time and mostly from rural areas. Another clinical finding that suggests reinfestation is the presence of hydatid cyst at the same localisation which seen was 4 of 14 recurrent cases. For these reasons, the probability of reinfestation is high in endemic countries like Turkey. When compared with the literature, in our study the recurrence rate was low. Albendazole treatment may play an important role in this low rate. Although the efficacy of perioperative prophylaxis with albendazole has been controversial, recent studies suggest that medical treatment is effective in the prevention of recurrence after surgery[36,37]. To diminish recurrence and potential spread of the organism, we believe that medical treatment should apply as an adjuvant therapy to surgery when complete removal of the cyst is impossible or when the cyst contents threaten to disseminate due to peritoneal rupture. It is indicated in patients who are at high risk for surgery, and in the presence of bilateral multiple small cysts. Those with small cysts (< 4 cm) and cysts with thin walls are the best group for effective medical treatment. In addition, exogenous vesiculations have been pronounced in hydatid cyst recurrences[38]. The importance of medical treatment which is mainly effective on small cysts, may indicate the usefulness of the effect on recurrence.
Although there is insufficient published evidence to support a clear recommendation for the use of albendazole preoperatively[39], we highly recommend this treatment for one week before surgical exploration. Pre-operative therapy may reduce the risk of intraperitoneal seeding of infection that develops via cyst rupture and spillage occurring spontaneously or during surgery. In our study no correlation was found between recurrence of cysts and albendazole use.
Serology detect specific serum antibodies or circulating antigen by a variety of immunodiagnostic methods. Of these, the enzyme immunosorbent assay (ELISA) employing hydatid fluid antigen for detection of echinococcal antibodies (IgG) in the serum is the most widely used. Serological tests are of little clinical use in monitoring patients after operation for cystic echinococcosis or patients on chemotherapy. The antibody titers rise following surgical treatment. The titers start falling at 3 mo and become negative in a period of 12-24 mo. False positive tests can occur in normal persons from endemic areas and in those with other parasitic infections[16]. In our study, 86 (58.9%) of 146 (42.4%) serologically evaluated patients of group II and III were positive, and 41 (28%) of these were also serologically positive 2 years after surgery. However, recurrence occurred in only 1 of the patients that was serologically positive for a long term. We think that the value of serological screening in areas endemic for cystic echinococcosis is enhanced by combining it with abdominal US.
Mortality rates of the study groups were not statistically different (P = 0.814, Table 4). Liver resections were performed in two mortality cases that were due to intraoperative and postoperative bleeding. One of the patients who had PP and drainage died because of myocardial infarct, and one patient had PP and omentoplasty cases of pulmonary thromboembolism. When compared, mortality rates were significantly different among groups (P < 0.001). This result requires discussion of the controversial radical methods in hydatid disease. Chautems et al[38] recommended complete resection of hepatic hydatid cysts. In contrast, Daali et al[40] preferred conservative procedures. We think that radical methods should not be performed routinely for such a slowly growing benign pathology. It is wise to reserve radical surgery for peripheral, easily accessible cysts and for unilober multiple cysts.
LOS did not differ between the cases of peritoneal perforation and intrabiliary rupture when compared with noncomplicated cases (P > 0.05), whereas, according to the additional surgical procedures, there was a significant difference in LOS between choledochotomy with T-tube and procedures without choledochotomy (P < 0.05). An external biliary fistula formation and T-tube procedure, wherein the T-tube may be taken out after approximately 7-10 d, may affect LOS. In contrast, there was no difference between the groups with biliodigestive anastomosis and without choledochotomy (P > 0.05). Biliodigestive anastomosis may be a good alternative surgical procedure to T-tubes, with lower complication rates and shorter LOS.
According to this study’s multinominal logistic regression analysis, peritoneal perforation risk increases with younger age, superficial localization, and larger dimensions of cysts, and older age, multiple and larger cysts, and bilobar localization are established as predisposing factors for intrabiliary rupture. Morbidity rates significantly increased in peritoneally perforated and intrabiliary ruptured cases, but there was no difference in recurrence rates and hospital stay times. Our preferred surgical technique for liver hydatid cysts is partial pericystectomy and drainage because the rate of postoperative complications and recurrence, and the duration of hospital stay are satisfactory. We believe that radical methods should not be performed routinely for such a benign pathology. The localization and number of cysts, relation to blood vessels and bile ducts, and general status of the patient are parameters influencing the choice of surgical procedure. In peritoneal perforated and intrabiliary ruptured cysts, the most important steps are irrigation of the peritoneal cavity with a sufficient amount of scolicidal agents, removal of all cystic contents from the peritoneum, and clearance of the cystic material from the biliary tree. However, randomized controlled studies are needed to establish the best surgical management for peritoneal perforated and intrabiliary ruptured liver hydatid cysts.
The development of hydatid disease associated with Echinococcus granulosus is still an important health problem. The clinical picture can be severe, and complications may occur, making the already difficult treatment even more so. Complications are observed in one third of patients with liver hydatid cysts. The most common complication is rupture of the cyst, either internally or externally.
Only a few studies have reported the management and outcome of patients with complicated liver hydatid disease. Surgery is the mainstay of treatment, although there is no consensus on the respective advantages of conservative and radical methods. In this study, the authors evaluated the predisposing factors for peritoneal perforation and intrabiliary rupture and the effects of these complications on morbidity, length of hospital stay, mortality, and recurrence in hydatid disease.
According to this study’s multinominal logistic regression analysis, peritoneal perforation risk increases with younger age, superficial localization, and larger dimensions of cysts, and older age, multiple and larger cysts, and bilobar localization are established as predisposing factors for intrabiliary rupture. Morbidity rates significantly increased in peritoneally perforated and intrabiliary ruptured cases, but there was no difference in recurrence rates and hospital stay times.
In peritoneal perforated and intrabiliary ruptured cysts, the most important steps are irrigation of the peritoneal cavity with a sufficient amount of scolicidal agents, removal of all cystic contents from the peritoneum, and clearance of the cystic material from the biliary tree. However, randomized controlled studies are needed to establish the best surgical management for peritoneal perforated and intrabiliary ruptured liver hydatid cysts.
Echinococcus granulosus is a parasitic tapeworm that lives in the bowels of dogs. Humans contract the disease through enteral exposure and become accidental intermediate hosts.
Alper Akcan et al, evaluate the predisposing factors for peritoneal perforation and intrabiliary rupture and the effects of these complications on surgical outcome in liver hydatid disease. This is one of the largest and well treated series of patients that had been publish. The structure and methodology followed by the authors is correct in my opinion and the techniques they applied for the treatment of these complex patients are modern and correct.
Peer reviewers: Hussein M Atta, MD, PhD, Department of Surgery, Faculty of Medicine, Minia University, Mir-Aswan Road, El-Minia 61519, Egypt; Eduardo de Santibañes, MD, PhD, Professor, Department of Surgery, Hospital Italiano de Buenos Aires, Gascón 450, Buenos Aires, 1181, Argentina; Christopher Christophi, Professor and Head of The University of Melbourne Department of Surgery, Austin Hospital, Melbourne, 145 Studley Road, Victoria 3084, Australia
S- Editor Tian L L- Editor O’Neill M E- Editor Ma WH
| 1. | Arambulo P 3rd. Public health importance of cystic echinococcosis in Latin America. Acta Trop. 1997;67:113-124. [Cited in This Article: ] |
| 2. | Altintaş N. Cystic and alveolar echinococcosis in Turkey. Ann Trop Med Parasitol. 1998;92:637-642. [Cited in This Article: ] |
| 3. | Eckert J, Thompson RC. Echinococcus strains in Europe: a review. Trop Med Parasitol. 1988;39:1-8. [Cited in This Article: ] |
| 4. | Barnes SA, Lillemoe KD. Liver abscess and hydatid cyst disease. Maingot’s Abdominal Operations. 10th ed. Stamford, Conn: Appleton & Lange 1997; 1513-1545. [Cited in This Article: ] |
| 5. | Kammerer WS, Schantz PM. Echinococcal disease. Infect Dis Clin North Am. 1993;7:605-618. [Cited in This Article: ] |
| 6. | Frider B, Larrieu E, Odriozola M. Long-term outcome of asymptomatic liver hydatidosis. J Hepatol. 1999;30:228-231. [Cited in This Article: ] |
| 7. | Elton C, Lewis M, Jourdan MH. Unusual site of hydatid disease. Lancet. 2000;355:2132. [Cited in This Article: ] |
| 8. | Ammann RW, Eckert J. Cestodes. Echinococcus. Gastroenterol Clin North Am. 1996;25:655-689. [Cited in This Article: ] |
| 9. | Gunay K, Taviloglu K, Berber E, Ertekin C. Traumatic rupture of hydatid cysts: a 12-year experience from an endemic region. J Trauma. 1999;46:164-167. [Cited in This Article: ] |
| 10. | Saenz de San Pedro B, Cazaña JL, Cobo J, Serrano CL, Quiralte J, Contreras J, Martinez F. Anaphylactic shock by rupture of hydatid hepatic cyst. Follow-up by specific IgE serum antibodies. Allergy. 1992;47:568-570. [Cited in This Article: ] |
| 11. | Magistrelli P, Masetti R, Coppola R, Messia A, Nuzzo G, Picciocchi A. Surgical treatment of hydatid disease of the liver. A 20-year experience. Arch Surg. 1991;126:518-522; discussion 523. [Cited in This Article: ] |
| 12. | Karavias DD, Vagianos CE, Kakkos SK, Panagopoulos CM, Androulakis JA. Peritoneal echinococcosis. World J Surg. 1996;20:337-340. [Cited in This Article: ] |
| 13. | Bedirli A, Sakrak O, Sozuer EM, Kerek M, Ince O. Surgical management of spontaneous intrabiliary rupture of hydatid liver cysts. Surg Today. 2002;32:594-597. [Cited in This Article: ] |
| 14. | Paksoy M, Karahasanoglu T, Carkman S, Giray S, Senturk H, Ozcelik F, Erguney S. Rupture of the hydatid disease of the liver into the biliary tracts. Dig Surg. 1998;15:25-29. [Cited in This Article: ] |
| 15. | Kornaros SE, Aboul-Nour TA. Frank intrabiliary rupture of hydatid hepatic cyst: diagnosis and treatment. J Am Coll Surg. 1996;183:466-470. [Cited in This Article: ] |
| 16. | Khuroo MS, Wani NA, Javid G, Khan BA, Yattoo GN, Shah AH, Jeelani SG. Percutaneous drainage compared with surgery for hepatic hydatid cysts. N Engl J Med. 1997;337:881-887. [Cited in This Article: ] |
| 17. | Alfieri S, Doglietto GB, Pacelli F, Costamagna G, Carriero C, Mutignani M, Liberatori M, Crucitti F. Radical surgery for liver hydatid disease: a study of 89 consecutive patients. Hepatogastroenterology. 1997;44:496-500. [Cited in This Article: ] |
| 18. | Chautems R, Bühler LH, Gold B, Giostra E, Poletti P, Chilcott M, Morel P, Mentha G. Surgical management and long-term outcome of complicated liver hydatid cysts caused by Echinococcus granulosus. Surgery. 2005;137:312-316. [Cited in This Article: ] |
| 19. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [Cited in This Article: ] |
| 20. | Ergüney S, Tortum O, Taspinar AH, Ertem M, Gazioğlu E. [Complicated hydatid cysts of the liver]. Ann Chir. 1991;45:584-589. [Cited in This Article: ] |
| 21. | Köksal N, Müftüoglu T, Günerhan Y, Uzun MA, Kurt R. Management of intrabiliary ruptured hydatid disease of the liver. Hepatogastroenterology. 2001;48:1094-1096. [Cited in This Article: ] |
| 22. | Leviav S, Weissberg D. Traumatic rupture of hydatid cysts. Can J Surg. 1996;39:293-296. [Cited in This Article: ] |
| 23. | Sözüer M, Yildirim C, Senol V, Unalan D, Naçar M, Günay O. [Risk factors in traffic accidents]. Ulus Travma Derg. 2000;6:237-240. [Cited in This Article: ] |
| 24. | Kilani T, El Hammami S, Horchani H, Ben Miled-Mrad K, Hantous S, Mestiri I, Sellami M. Hydatid disease of the liver with thoracic involvement. World J Surg. 2001;25:40-45. [Cited in This Article: ] |
| 25. | Martí-Bonmatí L, Menor F, Ballesta A. Hydatid cyst of the liver: rupture into the biliary tree. AJR Am J Roentgenol. 1988;150:1051-1053. [Cited in This Article: ] |
| 26. | Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20:795-817. [Cited in This Article: ] |
| 27. | Akgun Y, Yilmaz G. Efficiency of obliteration procedures in the surgical treatment of hydatid cyst of the liver. ANZ J Surg. 2004;74:968-973. [Cited in This Article: ] |
| 28. | Sonişik M, Korkmaz A, Besim H, Karayalçin K, Hamamci O. Efficacy of cetrimide-chlorhexidine combination in surgery for hydatid cyst. Br J Surg. 1998;85:1277. [Cited in This Article: ] |
| 29. | Gargouri M, Ben Amor N, Ben Chehida F, Hammou A, Gharbi HA, Ben Cheikh M, Kchouk H, Ayachi K, Golvan JY. Percutaneous treatment of hydatid cysts (Echinococcus granulosus). Cardiovasc Intervent Radiol. 1990;13:169-173. [Cited in This Article: ] |
| 30. | Derici H, Tansug T, Reyhan E, Bozdag AD, Nazli O. Acute intraperitoneal rupture of hydatid cysts. World J Surg. 2006;30:1879-1883; discussion 1884-1885. [Cited in This Article: ] |
| 31. | Alper A, Ariogul O, Emre A, Uras A, Okten A. Choledochoduodenostomy for intrabiliary rupture of hydatid cysts of liver. Br J Surg. 1987;74:243-245. [Cited in This Article: ] |
| 32. | Little JM, Hollands MJ, Ekberg H. Recurrence of hydatid disease. World J Surg. 1988;12:700-704. [Cited in This Article: ] |
| 33. | Dumas R, Le Gall P, Hastier P, Buckley MJ, Conio M, Delmont JP. The role of endoscopic retrograde cholangiopancreatography in the management of hepatic hydatid disease. Endoscopy. 1999;31:242-247. [Cited in This Article: ] |
| 34. | Tekant Y, Bilge O, Acarli K, Alper A, Emre A, Arioğul O. Endoscopic sphincterotomy in the treatment of postoperative biliary fistulas of hepatic hydatid disease. Surg Endosc. 1996;10:909-911. [Cited in This Article: ] |
| 35. | Vignote ML, Miño G, de la Mata M, de Dios JF, Gomez F. Endoscopic sphincterotomy in hepatic hydatid disease open to the biliary tree. Br J Surg. 1990;77:30-31. [Cited in This Article: ] |
| 36. | Horton RJ. Albendazole in treatment of human cystic echinococcosis: 12 years of experience. Acta Trop. 1997;64:79-93. [Cited in This Article: ] |
| 37. | Schantz PM. Editorial response: Treatment of cystic echinococcosis--improving but still limited. Clin Infect Dis. 1999;29:310-311. [Cited in This Article: ] |
| 38. | Chautems R, Buhler L, Gold B, Chilcott M, Morel P, Mentha G. Long term results after complete or incomplete surgical resection of liver hydatid disease. Swiss Med Wkly. 2003;133:258-262. [Cited in This Article: ] |
| 39. | Prousalidis J, Kosmidis C, Anthimidis G, Fachantidis E, Harlaftis N, Aletras H. Forty-four years’ experience (1963-2006) in the management of primarily infected hydatid cyst of the liver. HPB (Oxford). 2008;10:18-24. [Cited in This Article: ] |