JOURNAL OF DENTISTRY AND ORAL SCIENCES
Orofacial Myofunctional Therapy Effectivity in Child's Anterior Open Bite
Harun Achmad1*, Ummi Wajdiyah2 and Lusy Damayanti1
1Department of Pediatric Dentistry, Faculty of Dentistry, Hasanuddin University, Makassar - Indonesia
2Pediatric Dentistry Residency Program, Faculty of Dentistry, Hasanuddin University, Makassar – Indonesia
*Corresponding Author: Harun Achmad, Department of Pediatric Dentistry, Faculty of Dentistry, Hasanuddin University, Makassar–Indonesia.
| ReceivedMay 10, 2022 | RevisedMay 15, 2022 | AcceptedMay 20, 2022 | PublishedMay 26, 2022 |
Abstract
Background: Anterior Open Bite (AOB) is a malocclusion condition characterized by the absence of contact between the upper and lower anterior teeth, resulting from oral bad habits for a long time or abnormalities in skeletal patterns. AOB leads a lack of confidence in children because of the difficulty for lip sealing and the unclear pronunciation function. AOB occurs in children and continues into adulthood so it needs to be treated early on at the age of growth and development. One method of treating AOB is Orofacial Myofunctional Therapy (OMT) which is a method to improve the stability of the stomatognatic system by involving the exercise of the facial and neck muscles.
Aim: Literature Review (LR) writing aims to find out the effectiveness of OMT in the case of AOB children, how the treatment is carried out and the problems that occur during OMT.
Mini-Review: OMT increases the activity of the masseter and buccinator muscles, and decreases the contraction of the lip muscles that the lips may seal. OMT is able to increase the ability to hold the tongue to stay in contact with the palate so there is no obstacle to the eruption of the lower insisivus tooth and AOB can be corrected. Results: Orofacial Myofunctional Therapy (OMT) is effective for the correction of a child's Anterior Open Bite (AOB) as a combination therapy with the use of orthodontic tools or myofunctional equipment, especially in children older than 12 years of age and craniofacial deformity has occurred.
Keywords
Orofacial myofunctional; Child;Growth and development; Anterior open bite
Introduction
In the era of globalization, the demands and services of orthodontic care for children continue to increase over time. Initially, they focused more on orthodontic curative action against malocclusion in children, but today more demand and services have shifted to prevention and early orthodontic care [1-4]. In the case of orthodontic services for children, it indicates different service patterns; both at the stages of preventive, interceptive, and orthodontic curative services [4]. In fact, the development of orthodontic in children, especially in preventive orthodontics and interception has been in line with government programs in the dental and oral health services in a tiered and integrated manner; however, its implemetation is still a complex problem [4-6]. The current orthodontic care system has delivered satisfactory results, but there are still difficult cases that are proven to be treated. There are still some bad habits that accompany myofunctional in a child, such as finger sucking, posture problems, and tongue placement when swallowing, and abnormal breathing patterns [7] included in the treatment of anterior open bite in children.
Anterior Open Bite is a malocclusion condition that often occurs in children. The prevalence of AOBis 16.52% in children and adolescents aged 2-16 years [8]. The prevalence of primary dentition AOBis 16.9% and mixed dentition is 11.3%. The habits of sucking, tongue thrusting, and oral breathing are the main risk of AOB in the firstborn teeth, in mixed dentition, the habits that often cause AOB are sucking pacifiers, sucking lips, tongue thrusting, and breathing with the mouth [9].
Treatment for AOB correction includes the use of removable, fixed, and functional appliance, which the aims are inhibiting mechanical factors (such as thumb sucking or sticking out the tongue) that cause open bites to continue to exist and limiting excessive vertical growth of the craniofacial skeleton [10-12]. The principle of the use of oral myofunctional therapy devices is highly recommended for use in the growth and development of children. Treatment that begins at the mixed dental stage can increase effectiveness, minimizing the need for orthodontic treatment with permanent tooth extraction ororthognatic surgery has been widely reported [13]. Some publications state that early interceptive treatment in AOB patients with a deviated and persistent swallowing pattern may use Orofacial Myofunctional Therapy(OMT) [14-17]. Other authors also state that the normal oral function is re-established after OMT in patients with myofunctional disorders such as tongue thrusting [18,19].
Although the use of tools is effective in making AOB corrections, including can eliminate oral bad habits, OMT remains a treatment option. This is based on cost efficiency considerations and gives a sense of comfort because it does not use tools in the mouth [20]. OMT can also provide effective results when done during desidui teeth and teeth mixed and become an adjunctive treatment [21,22].
The purpose of writing this literature review is to find out the effectiveness of OMT in the case of AOB children, how the treatment is carried out, and the problems that occur during OMT.
Literature Review
Anterior Open Bite (AOB) is a condition in the oral cavity, characterized by no contact or deficit of normal vertical contact between antagonistic teeth in the arch of the anterior tooth [23-25]. AOB causes a variety of aesthetic and functional changes that interfere with the grip and cutting of food. It also causes problems in articulating certain phonemes. These changes can lead to poor psychosocial conditions. Some clinical problems due to malocclusion are permanent insisivus tooth injury of the upper jaw during growth, periodontal damage, difficulty closing the lips normally, and social influences such as lack of confidence in the child.
Open bites are classified into skeletal open bites and dental open bites. Dental open bites are localized to the anterior teeth and the surrounding soft and hard tissues without showing bone defects in cephalometric radiography, while skeletal open bites exhibit vertical disharmony in cephalometric radiography [27,28].
A number of habits may lead to AOB [29,30] but if the habit is performed only until the period of primary or mixed dentition will not have a negative effect [31,32].AOB can develop in permanent dental periods [33-35].In the age range between 6-8 years, AOB is the dominant type of malocclusion [36].In the early days of mixed dentition, 39.1% of children did not have either contact between the upper and lower insisivus teeth or palatal gingiva, while 4.6% had no incisal overlap [37].
The habit of sucking fingers, nipple milk bottles, and tongue including the habit of tongue thrusting, as well as upper airway obstruction are the main cause of AOB [38-40]. All habits involving obstruction mechanisms can inhibit tooth eruption or allow continuous dental supra-eruption that causes less incisal contact, affect the tongue reducing pressure on the maxillary and can dilate the mandible. An imbalance between the tongue and perioral muscle pressure can lead to a cusp-to-cusp relationship, the mandible is in a clockwise rotational position and contact of the incisive tooth is obstructed. The habit of sucking fingers can cause negative pressure and worsen unwanted forces. However, muscles are thought to have a stronger influence. The habit of placing the tongue by pushing forward when swallowing also plays a role in causing AOB. When AOB is present, the habit of sucking produces pro alveolus that blocks the closure of the lips when swallowing and the placement of the tongue in an abnormal position, especially at rest. Dentalshifts in AOB often occur due to a lack of balance between the strength of the tongue muscle (centrifuge) and the lip and cheek muscles (centripetal). As the balance of muscle strength deteriorates, the shift of the tooth and the alveolus of the tooth causes anterior injury.The loss of balance is caused by a decrease or increase in the strength of muscle components or the result of reduced closure and increased overhang due to poor sucking habits. In Skeletal Anterior Open Bites (SAOB), when the vertical component of facial growth is disproportionately larger than the horizontal component, there is an increase in the angle of the Frankfurt-Mandibular Plane (FMPA). AOB arises from an eruption of labial teeth that cannot compensate for the increase in interoclusal distance. The resulting open bite will usually be symmetrical and, in most extreme situations, only the posterior molars will be in occlusion [43,44].
Orofacial Myofunctional Therapy (OMT) is re-education of muscle function to improve the function of suffocation, tongue, habit of breathing through the mouth and posture of lips, tongue and cheeks at rest [45]. OMT includes cervical and facial muscle exercises for proprioceptive, tone and movement enhancement, [46-50] including exercises that support the tightening and endurance of the mouth muscles [51,52]. OMT re-education trains normal and strong sucking skills, good sanctification using both sides of the jaw, normal swallowing, tongue in a normal position, and nasal breathing with lips in good contact at rest [53].
Method
Journal samples are determined by inclusion criteria, namely children in primary and mixed dentition, with Anterior Open Bite (AOB) or incompetence of the lips closure. Exclusion criterias are review articles and case reports.
Search method
Journal searching uses electronic databases through Pubmed, Science Direct, Wiley Online Libraryportal and manual searching.
Search details
Journal search using keywords: "anterior open bite" AND "myofunctionaltherapy" AND children.
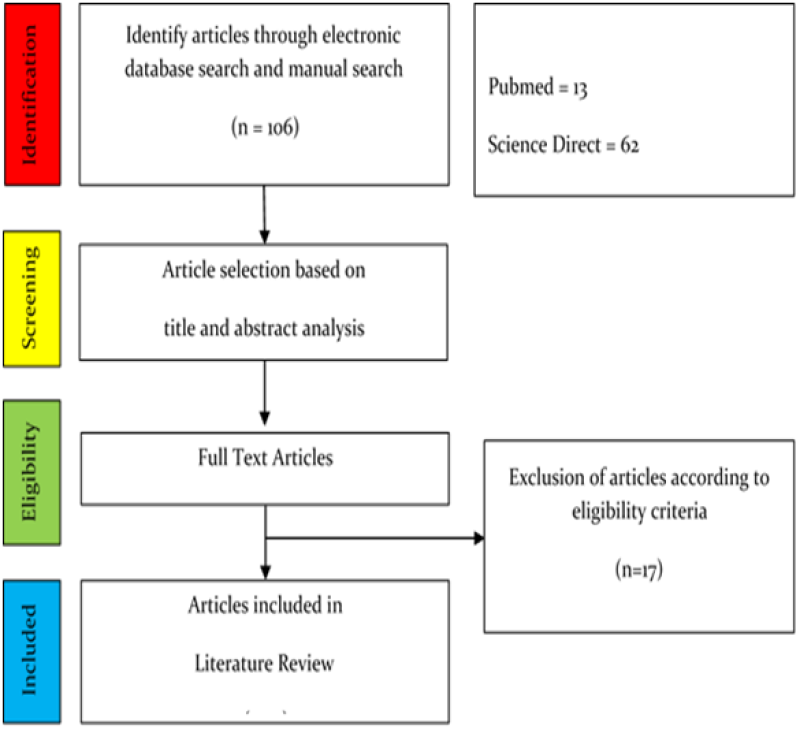
Figure 1: Completedatasearchprocessflowchart.
| NO. | AUTHOR | TITLE | INTERVENTION | RESULT | CONCLUSION |
| 1 | Daglio,
S., et. al., (1993) | Orthodontic
Changes in Oral Dyskinesia and Malocclusion under The Influence of
Myofunctional Therapy | Group A=undergoing
Myofunctional Therapy (MT)=13 children Group B=undergoing treatment with orthodonthic appliance and Myofunctional Therapy (MT)=15 children | Group
A: Reduction of overjet from 3.5 to 2.6 mm; the base angle of the mandible
decreased from 30° to 28.31°; The angle of ANB decreased from 4.4° to 2.7°;
statistically significant changes; better results with overbite correction, an
average of -2.46 to 3.06 mm Group B: Reduction of overjet from 6.6 to 2.6 mm; overbite increased from an average of -1.2 to +2.9 mm; the base angle of the mandible decreased from 31.2° to 27.8°;ANB angle reduced from 7.3° to 3.7° | Orofacial
dyskinesia can effectively be treated with a combination of orthodontic use and
myofunctional therapy rather than only being treated using myofunctional
therapy |
| 2 | Erbay
E, et. al., (1995) | The
Effects of Frankel's Function Regulator (FR-4) Therapy on the treatment of Angle Class I Skeletal Anterior Open bite Malocclusion | Group
1: control (without treatment)=20 children Group 2: lip-seal training and use of FR-4 appliance=20 children | AOB
closure in group 1(control)=from -3.5 mm to -2.1 mm (average increase of 1.4
mm) AOB closure in group 2=from -3.95 mm to 1.1 mm (average increase of 5 mm) | AOB
correction significantly occurs in the use of FR-4 and lip training through
rotation of the mandible up and forward |
| 3 | Lembrechts
D, et. al., (1999) | Effect
of a Logopedic Instruction Program after Adenoidectomy on Open Mouth Posture: A Single-Blind Study | Control
group: only undergoing adenoidectomy treatment=87 children Case group: undergoing adenoidectomy treatment and logopedic instruction program=72 children | In the
control group, spontaneous lip closure after adenoidectomy of 2 months by 14%
and after 1 year by 25% In the case group, lip closure occurred after adenoidectomy and logopedic instruction program by 2 months by 37% and after 1 year by 38%. | There
was a significant change in lip closure after 2 months of adenoidectomy and
logopedic instruction program. Children who can blow with their nose, do not have a habit of dripping saliva, do not have the habit of sucking thumbs or fingers, have a normal lower lip, are able to lift the tongue and are able to perform tongue control in good condition to start a logopedic instruction program and give better results than children who have bad mouth habits |
| 4 | Schievano
D, et. al., (1999) | The
13 children were divided into 4 groups, based on morphological evaluation of
the lower lip, chin, evaluation of respiration function, chewing and
swallowing. Each group is scored according to 4 levels of alteration (0-4
alteration=no alteration–severe alteration) Furthermore, Myofunctional Therapy (MT) is carried out by training the lips, tongue, chin area and chewer muscles, especially isometric procedures, facial massage especially in the chin area, and re-education of feeding (at least 30 minutes every week for 9 months) | There
is a significant RMS comparison between the position of the resting lip and the
closed lip before therapy (rate=1%), indicating an increase in the value of
muscle electrical activity (RMS). There was a statistically significant difference in electrical activity in the lips at rest and lips closed at a rate of 5%, suggesting that it required a decrease in muscle activity to close the lips before and after therapy. RMS values were similar in both situations analyzed, even when the muscles were not rehabilitated. There was a difference in electrical activity (significant at 5%) in the lips at rest and the lips closed earlier and after myofunctional therapy. Myofunctional therapy affects these muscles due to a decrease in muscle activity that is required to hold the lips together | There is a
significant RMS comparison between the position of the resting lip and the
closed lip before therapy (rate=1%), indicating an increase in the value of
muscle electrical activity (RMS). | MT
improves clinical and electromyographic outcomes significantly and shows a
positive influence of myofunctional therapy on the perioral muscles. This
therapy reduces the activity of the perioral muscles resulting in a lip closure
posture |
| 5 | Cayley
AS, et. al., (2000) | Electropalatographic
and Chepalometric Assessment of Myofunctional Therapy in Open-Bite Subjects | Tongue
Re-education Therapy in 4 sessions (each session=20 minutes) | 5
children with Anterior Open Bite (AOB)=0-6 mm; 2 AOB children have no change; 1
AOB child=5.5 mm -->5 children with AOB are correct, 3 children need
follow-up care | Treatment
has successfully improving tongue function during swallowing and lowers
anterior open bite (AOB). |
| 6 | Korbmacher
HM, et. al., (2004) | Evaluation
of A New Concept of Myofunctional Therapy in Children | MFT
group = conventional myofunctional therapy (speaking practice)=13 children Face Former Therapy (FFT) group=Tongue and lip traning using Flexible Silicone Appliance=15 children | There
was a very significant change in lip strength based on the length of therapy in
each group. However, there was no significant difference in lip strength
between the groups based on the duration of treatment. Within 6 months of observation, Face Former Therapy (FFT) showed success faster than Myofunctional Therapy (MFT). | Face
Former Therapy (FFT) achieves an increase in lip closure strength in a shorter
time than Myofunctional Therapy (MFT) |
| 7 | Degan
VV, and Puppin-Rontani RM. (2005) | Removal
of Sucking Habits and Myofunctional Therapy: Establishing Swallowing and Tongue Rest Position | Myofunctional
Therapy Group and Counseling (TMF)=10 children Modified Counseling Group (REM)=10 children | 60%
of TMF samples showed better resting tongue position at 3rd evaluation (180
days) than REM samples by 0% 80% of TMF samples showed normal swallowing patterns at evaluation to -3(180 days) rather than REM samples by 50% | Myofunctional
therapy (TMF) associated with eliminating the habit of sucking showed improved
swallowing patterns and better and faster tongue resting positions |
| 8 | Smithpeter
J, and Covell D (2010) | Relapse
of Anterior Open Bites Treated with Orthodontic Appliances with and without Orofacial Myofunctional Therapy | Experimental
group: received Orofacial Myofunctional Therapy (OMT) and orthodontic
treatment=27 children(before, during and after relapsing orthodontic treatment) Control group: history of orthodontic treatment with relaps anterior open bite (AOB)=49 children | There
was a significant difference in anterior open bite (AOB) relapsing between the
experimental group and the control group, where the experimental group occurred
relaps AOB=0.5 mm, while the control group=3.4 mm | The
combination of OMT and orthodontic treatment effectively maintains anterior
open bite closure versus single orthodontic treatment |
| 9 | Huang
B, et. al., (2015) | Influence
of Non-Orthodontic Intervention on Digit Sucking and Consequent Anterior Open Bite: A Preliminary Study | Experimental
group=Non-Orthodontic Intervention (NOI)/Stomahesive Wafer Spot + tongue
instruction=77 children Control group=14 children | From
77 children in the experimental group, the number of children with anterior
open bites (AOB) decreased from 37 (51.4%) to 12 (16.7%) at the end of NOI
treatment; Among 32 patients with a measured overjet, the average overjet decreased from 4.2 mm to 3.1 mm after NOI treatment; Children who received NOI were more likely to quit the habit of sucking fingers within a 4-month period and more likely to appear without an Anterior Open Bite (AOB) in a 4-month period | There
is clinical relevance to NOI in finger sucking habits, AOB closure and overjet
reduction |
Table 1: Synthesis Table.
Data Collection and Data Analysis
The author collected 106 articles through an electronic database and manual search according to the keywords. The author assessed the title and abstract of the journals resulting from the search. The relevant title and abstract were selected with the result that 28 articles were obtained. The author read the full-text article to determine that the study met the inclusion criteria. Studies that meet inclusion criteria then underwent quality assessment and data extraction. The author reviewed selecting 11 articles that included the synthesis table.
Discussion
This literature review discusses the effectiveness of Orofacial Myofunctional Therapy (OMT) in Anterior Open Bite (AOB) of children. From the 11 studies, 6 journals stated that correction of AOB can be performed through a combination of OMT with myofunctional appliance, orthodontic appliance and post adenoidectomy treatment. Four journals showed the effectiveness of OMT as a single therapy. One journal showed the use of myofunctional appliances was more effective than OMT in performing AOB corrections.
According to Daglioet. al., 1993 [43] malocclusion (open bite, anterior slit position and cross bite) can occur in neuromuscular disorders. Maloclusion can be treated with a combination of orthodontic use and myofunctional therapy compared to myofunctional therapy alone, by affecting the activity of the tongue muscles compared to the lip muscles, buccinators and facial muscles.
In Skeletal Anterior Open Bite (SAOB), the mandible grows and develops downward and backward. Erbayet. al., 1994 [44] showed that by using FR-4 and lip-seal training tools, the rotation of the mandible forward and upwards resulted in SAOB correction. Lip-seal training can activate and increase muscle tone, that the lips are able to close and mandible is held in the right position. Hong et. al., 2021 [45] show SAOB has an abnormal Orofacial Myofunctional Status (OMS) including distorted swallowing patterns and weak involuntary muscles, related to more than normal facial height and the presence of protrusive insisivus.
AOB may result from Obstructive Sleep Apnea (OSA). OSA causes children to tend to oral breathing that the lip posture is not able to close. The most common therapy is adenoidectomy. Lembrechtset. al., 1999 [46]stated that there was lip closure after 2 months of adenoidectomy and the administration of training instructions to close the lips and breathe with the nose (logopedic).
Smithpeter and Covell 2010 [47] stated that OMT is needed as an additional treatment after the use of orthodontic applaiance to prevent AOB relapsing. OMT is performed before, during and after using the appliance as an orofacial muscle therapy and eliminates oral bad habits.
OMT as a single therapy was performed by Cayley et. al., 2000 [48] and Van Dyck et. al., 2016 [49]. There is a downward trend of AOB and further eruption of upper and lower insisivus teeth after OMT is performed. Schievanoet. al., 1999 [50] showed that OMT can decrease perioral muscle activity so that the lips are able to close. Decreased muscle activity is seen from the clinical picture through electromyography. While Degan and Puppin 2005 [51] stated that eliminating oral bad habits shows a pattern of thickening and posture of the tongue at rest is better. Huang et. al., 2015 [52] showed that eliminating oral bad habits using Non-Orthodontic Intervention (NOI) effectively decreased AOB and reduced overjet. Reduced overjet implies backward movement, or rotation, of upper incisors. Due to the sensation of a foreign body, a stomahesive wafer placed attached to sharp papillae can cause the tip of the tongue to touch that spot, divert the subject from insertion of the thumb or other finger into the mouth, and stop oral bad habits.
Correction of AOB using combination treatments is indicated in neuromuscular disorders, SAOB, OSA and post-use stabilization of orthodontic devices. Effective combination treatment is performed in children up to the age of 18 years. Correction of AOB using a single OMT in children aged <10 years indicates early treatment of AOB in children of growing age is able to prevent maloclusion to reduce the need for orthodontic care in adolescence. The use of myofunctional equipment is considered effective in repairing AOB compared to OMT without tools because the use of an appliance is carried out for a longer duration than OMT and works directly on the orofacial muscle.
OMT has the effectiveness of correction of AOB by increasing the activity of the masseter and buccinator muscles, as well as decreasing the contraction of the lip muscles so that the lips are able to close. OMT is able to increase the ability to hold the tongue to stay in contact with the palate so that there is no obstacle to the eruption of the lower insisvus tooth and AOB can be corrected. AOB children have a wider pattern of tongue surface contact with palate because it involves the posterior and lateral sides of the tongue. In a normal swallowing pattern, only the tip of the tongue touches the palate behind the insisal papillae, while in AOB children the tongue is pushed into the open bite area so that contact occurs to the posterior and lateral parts of the tongue. In addition to AOB correction, OMT also has an effect on eliminating oral bad habits.
Based on these researches, it can be said that Orofacial Myofunctional Therapy (OMT) is effective in correcting a child's Anterior Open Bite (AOB) as an adjunct therapy or combined with the use of orthodontic or myofunctional appliance, especially in children over 12 years of age and craniofacial deformities have occurred. OMT is used as a single therapy when the child is still in the stage of growth and development.
Conclusion
Based on the analysis of literature reviews in related journals, it can be concluded that:
1. Orofacial Myofunctional Therapy (OMT) is effective for increasing facial muscle activity, decreasing perioral muscle contractions and improving tongue posture
2. OMT effectively eliminates bad mouth habits especially in relation to correction of Anterior Open Bite(AOB)
3. The effectiveness of OMT is used as a single therapy to eliminate children's bad habits and correction of AOB, especially while still in the stage of growth and development and there has been no craniofacial deformity
4. The effectiveness of OMT as an adjuvant therapy or combination with orthodontic treatment especially if there has been maloclusion or craniofacial deformity
Acknowledgment
The author is responsible for the content and writing of the paper. The author has read and approved the final manuscript of this literature review.The study did not receive any special grants from funding agencies in the public, commercial or nonprofit sectors.
Conflict of Interest
The author states that this manuscript has no conflict of interest.
Reference
1. Sutardjo IRS. Considerations and Problems of Early Use of Orthodontic Interseptic Devices in Developmental Children. J Stomatognatic. Jember University. 2011;8(1):1-10.
2. Araújo EA, Buschang PH. Recognizing and correcting developing malocclusions: a problem-oriented approach to orthodontics. John Wiley & Sons. 2016. CrossRef
3. Almeida MR, Almeida RR, Oltramari-Navarro PV, Conti AC, Navarro RD, Camacho JG. Early treatment of Class III malocclusion: 10-year clinical follow-up. J Appl Oral Sci. 2011;19(4):431-9. PubMed | CrossRef
4. Achmad H, Faizah N. M--Effect of Orthodontic Facemask as a Treatment for Children in Growth and Development Period: A Systematic Review.Ann Romanian Soc Cell Biol. 2021:1658-72.
5. Mandall N, Cousley R, DiBiase A, Dyer F, Littlewood S, Mattick R, et al. Early Class III protraction facemask treatment reduces the need for orthognathic surgery: a multi-centre, twoarm parallel randomized, controlled trial. J Orthod. 2016;43(3):164-75. PubMed | CrossRef
6. Nardoni DN, Siqueira DF, Cardoso MD, Capelozza Filho L. Cephalometric variables used to predict the success of interceptive treatment with rapid maxillary expansion and face mask. A longitudinal study. Dental Press J Orthod. 2015;20(1):85-96. PubMed | CrossRef
7. Achmad H, Tahir H, Adam M, Ramadhany YF. Increased overjet in growing child, problem solving in pediatric dentistry. J Int Dent Medical Res. 2017;10(2):374.
8. Avrella MT, Zimmermann DR, Andriani JS, Santos PS, Barasuol JC. Prevalence of anterior open bite in children and adolescents: a systematic review and meta-analysis. Eur Arch Paediatr Dent. 2021:1-0. PubMed | CrossRef
9. Urzal V, Braga AC, Ferreira AP. The prevalence of anterior open bite in Portuguese children during deciduous and mixed dentition–Correlations for a prevention strategy.Int Orthod. 2013;11(1):93-103. PubMed | CrossRef
10. Torres FC, Almeida RR, Almeida-Pedrin RR, Pedrin F, Paranhos LR. Dentoalveolar comparative study between removable and fixed cribs, associated to chincup, in anterior open bite treatment. J Appl Oral Sci. 2012;20(5):531-7. PubMed | CrossRef
11. De Menezes LM, Ritter DE, Locks A. Combining traditional techniques to correct anterior open bite and posterior crossbite. Am J Orthod Dentofacial Orthop. 2013;143(3):412-20. PubMed | CrossRef
12. Mucedero M, Franchi L, Giuntini V, Vangelisti A, McNamara Jr JA, Cozza P. Stability of quad-helix/crib therapy in dentoskeletal open bite: a long-term controlled study. Am J Orthod Dentofacial Orthop. 2013;143(5):695-703. PubMed | CrossRef
13. Achmad H, Mutmainnah N, Ramadhany YF. A Systematic Review of Oral Myofunctional Therapy, Methods and Development of Class II Skeletal Malocclusion Treatment in Children. Syst Rev Pharm. 2020;11(6):511-21.
14. Andrianopoulos MV, Hanson ML. Tongue-thrust and the stability of overjet correction. Angle Orthod. 1987;57(2):121-35. PubMed | CrossRef
15. Saccomanno S, Antonini G, D'Alatri L, D'Angeloantonio M, Fiorita A, Deli R. Case report of patients treated with an orthodontic and myofunctional protocol. Eur J Paediatr Dent. 2014;15:184–6. PubMed
16. Mason RM. A retrospective and prospective view of orofacial myology.Int J Orofacial Myology. 2008;34:5. PubMed
17. Takahashi O, Twasawa T. Integrating orthodontics and oral myofunctional therapy for patients with oral myofunctional disorders. Int J Orofacial Myology. 1995;21:66-72. PubMed | CrossRef
18. Takahashi S, Kuribayashi G, Ono T, Ishiwata Y, Kuroda T. Modulation of masticatory muscle activity by tongue position. Angle Orthod. 2005;75(1):35-9. PubMed | CrossRef
19. Benkert KK. The effectiveness of orofacial myofunctional therapy in improving dental occlusion. Int J Orofacial Myology. 1997;23(1):35-46. PubMed | CrossRef
20. Moschik CE, Pichelmayer M, Coulson S, Wendl B. Influence of Myofunctional Therapy on Upper Intercanine Distance. J Dent Oral DisordTher. 2015;3(1):1-7. CrossRef
21. Saccomanno S, Antonini G, D'Alatri L, D'Angeloantonio M, Fiorita A, Deli R. Case report of patients treated with an orthodontic and myofunctional protocol. Eur J Paediatr Dent. 2014;15:184-6. PubMed
22. Sugawara Y, Ishihara Y, Takano-Yamamoto T, Yamashiro T, Kamioka H. Orthodontic treatment of a patient with unilateral orofacial muscle dysfunction: The efficacy of myofunctional therapy on the treatment outcome. Am J Orthod Dentofacial Orthop. 2016;150(1):167-80. PubMed | CrossRef
23. Lin LH, Huang GW, Chen CS. Etiology and treatment modalities of anterior open bite malocclusion. J Exp Clin Med. 2013;5(1):1-4. CrossRef
24. Gutiérrez DA, Garzón JS, Franco JQ, Botero-Mariaca P. Anterior open bite and its relationship with dental arch dimensions and tongue position during swallowing and phonation in individuals aged 8–16 years: A retrospective case–control study. Int Orthod. 2021;19(1):107-16.
25. De Lima Mendes S, Ribeiro IL, de Castro RD, Filgueiras VM, Ramos TB, Lacerda RH. Risk factors for anterior open bite: A case–control study.Dent Res J. 2020;17(5):388. PubMed | CrossRef
26. Lentini‐Oliveira DA, Carvalho FR, Rodrigues CG, Ye Q, Hu R, Minami‐Sugaya H. Orthodontic and orthopaedic treatment for anterior open bite in children. Cochrane Database Syst Rev. 2014(9). PubMed | CrossRef
27. Daer AA, Abuaffan AH. Skeletal and dentoalveolar cephalometric features of anterior open bite among Yemeni adults. Scientifica (Ciaro). 2016;2016:3147972. PubMed | Crossref
28. English JD, Olfert KD. Masticatory muscle exercise as an adjunctive treatment for open bite malocclusions. Semin Orthod. 2005;11(3):164-69. CrossRef
29. Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36(5):386-94. PubMed | CrossRef
30. Doğramacı EJ, Rossi-Fedele G. Establishing the association between nonnutritive sucking behavior and malocclusions: A systematic review and meta-analysis. J Am Dent Assoc. 2016;147(12):926-34. PubMed | CrossRef
31. Moraes RB, Knorst JK, Pfeifer AB, Vargas‐Ferreira F, Ardenghi TM. Pathways to anterior open bite after changing of pacifier sucking habit in preschool children: A cohort study. Int J Paediatr Dent. 2021;31(2):278-84. PubMed | CrossRef
32. Nihi VSC, Maciel SM, Jarrus ME, Nihi FM, Salles CLF de, Pascotto RC. Pacifier-Sucking Habit Duration and Frequency on Occlusal and Myofunctional Alterations in Preschool Children. Braz Oral Res. 2015; 29: 1–7. PubMed | CrossRef
33. Rijpstra C, Lisson JA. Etiology of anterior open bite: a review.J OrofacOrthop. 2016;77(4):281-6. PubMed | CrossRef
34. Janson G, Rizzo M, Laranjeira V, Garib DG, Valarelli FP. Posterior teeth angulation in non-extraction and extraction treatment of anterior open-bite patients. Prog Orthod. 2017;18(1):1-7. PubMed | CrossRef
35. Garrett J, Araujo E, Baker C. Open-bite treatment with vertical control and tongue reeducation. Am J Orthod Dentofacial Orthop. 2016;149(2):269-76. PubMed | CrossRef
36. Tausche E, Luck O, Harzer W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. Eur J Orthod. 2004;26(3):237-44. PubMed | CrossRef
37. Keski-Nisula K, Lehto R, Lusa V, Keski-Nisula L, Varrela J. Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. Am J Orthod Dentofacial Orthop. 2003;124(6):631-8. PubMed | CrossRef
38. Dawson PE. Evaluation diagnosis and treatment of occlusal problems. CV Mosbv Co. Saint Louis. 1989;28-55.
39. Chen X, Xia B, Ge L. Effects of breast-feeding duration, bottle-feeding duration and non-nutritive sucking habits on the occlusal characteristics of primary dentition. BMC pediatr. 2015;15(1):1-9. PubMed | CrossRef
40. Urzal V, Braga AC, Ferreira AP. The prevalence of anterior open bite in Portuguese children during deciduous and mixed dentition–Correlations for a prevention strategy. Int Orthod. 2013;11(1):93-103. PubMed | CrossRef
41. Franco FCM, Araújo TM, F. Active Tips: A Resource for The Treatment of Anterior Bite Lingual Spurs: A Resource for The Treatment of Anterior Open Bite. Orthodon. Gauch. 2001;5(1):6-12.
42. Adair SM, Milano M, Lorenzo I, Russell C. Effects of current and former pacifier use on the dentition of 24-to 59-month old children. Pediatr Dent. 1995;17:437-44. PubMed
43. Sandler PJ, Madahar AK, Murra A. Anterior open bite: aetiology and management. Dent Update. 2011;38(8):522-32. PubMed | CrossRef
44. Tanny L, Huang B, Naung NY, Currie G. Non-orthodontic intervention and non-nutritive sucking behaviours: A literature review. Kaohsiung J Med Sci. 2018;34(4):215-22. CrossRef
45. Green SE. Confirmational study: a positive-based thumb and finger sucking elimination program. Int J Orofacial Myology. 2010;36:44-59. PubMed | CrossRef
46. Das UM, Beena JP. Effectiveness of circumoral muscle exercises in the developing dentofacial morphology in adenotonsillectomized children: an ultrasonographic evaluation. J Indian Soc PedodPrev Dent. 2009;27(2):94. PubMed | CrossRef
47. Maria de Felício C, De Oliveira Melchior M, LúciaPimenta Ferreira C, Rodrigues Da Silva MA. Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. Cranio. 2008;26(2):118-25. PubMed | CrossRef
48. Ruscello DM. Nonspeech oral motor treatment issues related to children with developmental speech sound disorders. Lang Speech Hear Serv Sch. 2008;39(3): 380–391. PubMed | CrossRef
49. Anupam Kumar T, Kuriakose S. Ultrasonographic evaluation of effectiveness of circumoral muscle exercises in adenotonsillectomized children. J Clin Pediatr Dent. 2004;29(1):49-55. PubMed | CrossRef
50. Mauclaire C, Vanpoulle F, Saint-Georges-Chaumet Y. Physiological correction of lingual dysfunction with the “Tongue Right Positioner”: Beneficial effects on the upper airways. Int Orthod. 2015;13(3):370-89. PubMed | CrossRef
51. Shah SS, Nankar MY, Bendgude VD, Shetty BR. Orofacial myofunctional therapy in tongue thrust habit: A narrative review. Int J Clin Pediatr Dent. 2021;14(2):298. PubMed | CrossRef
52. Achmad H, Huldani NH, Ramadhany Y. A Systematic Review of Oral Myofunctional Therapy for Future Treatment in Pediatric Obstructive Sleep Apnea (OSA). Syst Rev Pharm. 2020;11(6):522-8. CrossRef
53. Achmad H, Adam M, Oktawati S, Karim SR, Thahir H, Pratiwi R et. al. An overjet reduction of class II, division 1 malocclusion in twin block dentofacial orthopedic and fixed orthodontic treatment: Case report. J Int Dent Medical Res. 2017;10(3):1010-6.
54. Hong H, Zeng Y, Chen X, Peng C, Deng J, Zhang X et. al. Electromyographic features and efficacy of orofacial myofunctional treatment for skeletal anterior open bite in adolescents: an exploratory study. BMC Oral Health. 2021;21(1):1-3. PubMed | CrossRef
55. Lembrechts D, Verschueren D, Heulens H, Valkenburg HA, Feenstra L. Effect of a logopedic instruction program after adenoidectomy on open mouth posture: a single-blind study. Folia PhoniatrLogop. 1999;51(3):117-23. PubMed | CrossRef
56. Smithpeter J, Covell Jr D. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. American Journal of Orthodontics and Dentofacial Orthopedics. 2010;137(5):605-14. CrossRef
57. Cayley AS, Tindall AP, Sampson WJ, Butcher AR. Electropalatographic and cephalometric assessment of myofunctional therapy in open-bite subjects. Aust Orthod J. 2000;16(1):23-33. PubMed
58. Van Dyck C, Dekeyser A, Vantricht E, Manders E, Goeleven A, Fieuws S, Willems G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: a pilot study. Eur J Orthod. 2016;38(3):227-34.PubMed | CrossRef
59. Schievano D, Rontani RM, Berzin F. Influence of myofunctional therapy on the perioral muscles. Clinical and electromyographic evaluations. J Oral Rehabil. 1999;26(7):564-9. CrossRef
60. Degan VV, Puppin-Rontani RM. Removal of sucking habits and myofunctional therapy: establishing swallowing and tongue rest position. Pro Fono. 2005;17:375-82. PubMed | CrossRef
61. Huang B, Lejarraga C, Franco CS, Kang Y, Lee A, Abbott J, et. al. On P. Influence of non-orthodontic intervention on digit sucking and consequent anterior open bite: a preliminary study. Int Dent J. 2015;65(5):235-41. PubMed | CrossRef
Harun Achmad1*, Ummi Wajdiyah2 and Lusy Damayanti1
1Department of Pediatric Dentistry, Faculty of Dentistry, Hasanuddin University, Makassar - Indonesia
2Pediatric Dentistry Residency Program, Faculty of Dentistry, Hasanuddin University, Makassar – Indonesia
*Corresponding Author: Harun Achmad, Department of Pediatric Dentistry, Faculty of Dentistry, Hasanuddin University, Makassar–Indonesia.
Copyright© 2022 by Achmad H, et al. All rights reserved. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Achmad H, Wajdiyah U, Damayanti L. Orofacial Myofunctional Therapy Effectivity in Child's Anterior Open Bite. J Dent Oral Sci. 2022;4(2):1-16. DOI: https://doi.org/10.37191/Mapsci-2582-3736-4(2)-0125
