Stimuli-Responsive Aliphatic Polycarbonate Nanocarriers for Tumor-Targeted Drug Delivery
Abstract
:1. Introduction
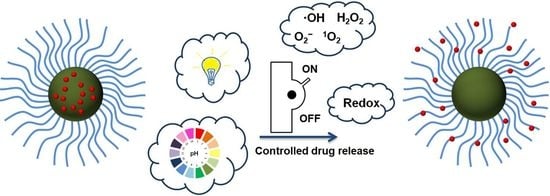
2. Application of Endogenous/Exogenous Stimulus-Responsive APC Nanocarriers
2.1. pH-Responsive APC Nanocarriers
2.2. Redox-Responsive APC Nanocarriers
2.3. ROS-Responsive APC Nanocarriers
2.4. Light-Responsive APC Nanocarriers
2.5. Dual/Multiple Stimuli-Responsive APC Nanocarriers
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Dang, H.; Wang, X.W. The significance of intertumor and intratumor heterogeneity in liver cancer. Exp. Mol. Med. 2018, 50, e416. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. The Hallmarks of Cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef] [Green Version]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [Green Version]
- Luo, J.; Solimini, N.L.; Elledge, S.J. Principles of Cancer Therapy: Oncogene and Non-oncogene Addiction. Cell 2009, 138, 823–837. [Google Scholar] [CrossRef] [Green Version]
- Mohme, M.; Riethdorf, S.; Pantel, K. Circulating and disseminated tumour cells—Mechanisms of immune surveillance and escape. Nat. Rev. Clin. Oncol. 2017, 14, 155–167. [Google Scholar] [CrossRef]
- Alizadeh, A.M.; Shiri, S.; Farsinejad, S. Metastasis review: From bench to bedside. Tumor Biol. 2014, 35, 8483–8523. [Google Scholar] [CrossRef]
- Brooks, S.A.; Lomax-Browne, H.J.; Carter, T.M.; Kinch, C.E.; Hall, D.M.S. Molecular interactions in cancer cell metastasis. Acta Histochem 2010, 112, 3–25. [Google Scholar] [CrossRef]
- Singh, S.; Hussain, A.; Aleti, R.R.; Nlooto, M.; Karpoormath, R. Chapter 8—Polycarbonate Nanoparticles as a Promising Tool for Anticancer Therapeutics. In Polymeric Nanoparticles as a Promising Tool for Anti-Cancer Therapeutics; Kesharwani, P., Paknikar, K.M., Gajbhiye, V., Eds.; Chapter 8; Academic Press: Cambridge, MA, USA, 2019; pp. 147–166. [Google Scholar] [CrossRef]
- Nicolas, J.; Mura, S.; Brambilla, D.; Mackiewicz, N.; Couvreur, P. Design, functionalization strategies and biomedical applications of targeted biodegradable/biocompatible polymer-based nanocarriers for drug delivery. Chem. Soc. Rev. 2013, 42, 1147–1235. [Google Scholar] [CrossRef]
- Wolinsky, J.B.; Colson, Y.L.; Grinstaff, M.W. Local drug delivery strategies for cancer treatment: Gels, nanoparticles, polymeric films, rods, and wafers. J. Control. Release 2012, 159, 14–26. [Google Scholar] [CrossRef] [Green Version]
- Krishna, R.; Mayer, L.D. Multidrug resistance (MDR) in cancer Mechanisms, reversal using modulators of MDR and the role of MDR modulators in influencing the pharmacokinetics of anticancer drugs. Eur. J. Pharm. Sci. 2000, 11, 265–283. [Google Scholar] [CrossRef]
- Danhier, F. To exploit the tumor microenvironment: Since the EPR effect fails in the clinic, what is the future of nanomedicine? J. Control. Release 2016, 244, 108–121. [Google Scholar] [CrossRef]
- Sindhwani, S.; Syed, A.M.; Ngai, J.; Kingston, B.R.; Maiorino, L.; Rothschild, J.; MacMillan, P.; Zhang, Y.; Rajesh, N.U.; Hoang, T.; et al. The entry of nanoparticles into solid tumours. Nat. Mater. 2020, 19, 566–575. [Google Scholar] [CrossRef]
- Du, J.; Lane, L.A.; Nie, S. Stimuli-Responsive Nanoparticles for Targeting the Tumor Microenvironment. J. Control. Release 2015, 219, 205–214. [Google Scholar] [CrossRef] [Green Version]
- Feng, L.; Dong, Z.; Tao, D.; Zhang, Y.; Liu, Z. The Acidic Tumor Microenvironment: A Target for Smart Cancer Nano-theranostics. Natl. Sci. Rev. 2018, 5, 269–286. [Google Scholar] [CrossRef] [Green Version]
- Leong, D.T.; Ng, K.W. Probing the relevance of 3D cancer models in nanomedicine research. Adv. Drug Deliv. Rev. 2014, 79–80, 95–106. [Google Scholar] [CrossRef]
- Hossen, S.; Hossain, M.K.; Basher, M.K.; Mia, M.N.H.; Rahman, M.T.; Uddin, M.J. Smart nanocarrier-based drug delivery systems for cancer therapy and toxicity studies: A review. J. Adv. Res. 2019, 15, 1–18. [Google Scholar] [CrossRef]
- Kobayashi, H.; Watanabe, R.; Choyke, P.L. Improving Conventional Enhanced Permeability and Retention (EPR) Effects; What Is the Appropriate Target? Theranostics 2014, 4, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Haume, K.; Rosa, S.; Grellet, S.; Smialek, M.A.; Butterworth, K.T.; Solov’yov, A.V.; Prise, K.M.; Mason, N.J. Gold nanoparticles for cancer radiotherapy: A review. Cancer Nanotechnol. 2016, 7, 8. [Google Scholar] [CrossRef] [Green Version]
- Kataoka, K.; Harada, A.; Nagasaki, Y. Block copolymer micelles for drug delivery: Design, characterization and biological significance. Adv. Drug Deliv. Rev. 2012, 64, 37–48. [Google Scholar] [CrossRef]
- Lee, J.S.; Feijen, J. Polymersomes for drug delivery: Design, formation and characterization. J. Control. Release 2012, 161, 473–483. [Google Scholar] [CrossRef]
- Rautio, J.; Kumpulainen, H.; Heimbach, T.; Oliyai, R.; Oh, D.; Jarvinen, T.; Savoleinen, J. Prodrugs: Design and clinical applications. Nat. Rev. Drug Discov. 2008, 7, 255–270. [Google Scholar] [CrossRef]
- Alven, S.; Nqoro, X.; Buyana, B.; Aderibigbe, B.A. Polymer-Drug Conjugate, a Potential Therapeutic to Combat Breast and Lung Cancer. Pharmaceutics 2020, 12, 406. [Google Scholar] [CrossRef]
- Bildstein, L.; Dubernet, C.; Couvre, P. Prodrug-based intracellular delivery of anticancer agents. Adv. Drug Deliv. Rev. 2011, 63, 3–23. [Google Scholar] [CrossRef]
- Cordato, D.J.; Mather, L.E.; Herkes, G.K. Stereochemistry in clinical medicine: A neurological Perspective. J. Clin. Neurosci. 2003, 10, 649–654. [Google Scholar] [CrossRef]
- Liu, Y.; Khan, A.R.; Du, X.; Zhai, Y.; Tan, H.; Zhai, G. Progress in the polymer-paclitaxel conjugate. J. Drug Deliv. Sci. Technol. 2019, 54, 101237. [Google Scholar] [CrossRef]
- Franks, M.E.; Macpherson, G.R.; Figg, W.D. Thalidomide. Lancet 2004, 363, 1802–1811. [Google Scholar] [CrossRef] [Green Version]
- Gong, J.; Neels, J.F.; Yu, X.; Kensler, T.W.; Peterson, L.A.; Sturla, S.J. Investigating the Role of Stereochemistry in the Activity of Anticancer Acylfulvenes: Synthesis, Reductase-Mediated Bioactivation, and Cellular Toxicity. J. Med. Chem. 2006, 49, 2593–2599. [Google Scholar] [CrossRef]
- Lu, H. Stereoselectivity in drug metabolism. Expert Opin. Drug Metab. Toxicol. 2007, 3, 149–158. [Google Scholar] [CrossRef]
- Aghebati-Maleki, A.; Dolati, S.; Ahmadi, M.; Baghbanzhadeh, A.; Asadi, M.; Fotouhi, A.; Yousefi, M.; Aghebati-Malek, L. Nanoparticles and cancer therapy: Perspectives for application of nanoparticles in the treatment of cancers. J. Cell. Physiol. 2019, 235, 1962–1972. [Google Scholar] [CrossRef]
- Mailander, V.; Landfester, K. Interaction of Nanoparticles with Cells. Biomacromolecules 2009, 10, 2379–2400. [Google Scholar] [CrossRef]
- Lin, W.; Yin, L.; Sun, T.; Wang, T.; Xie, Z.; Gu, J.; Jing, X. The Effect of Molecular Structure on Cytotoxicity and Antitumor Activity of PEGylated Nanomedicines. Biomacromolecules 2018, 19, 1625–1634. [Google Scholar] [CrossRef]
- Zhao, J.; Stenzel, M.H. Entry of nanoparticles into cells: The importance of nanoparticle properties. Polym. Chem. 2018, 9, 259–272. [Google Scholar] [CrossRef]
- Kumari, A.; Yadav, S.K.; Yadav, S.C. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf. B 2010, 75, 1–18. [Google Scholar] [CrossRef]
- Wang, J.; Li, S.; Han, Y.; Guan, J.; Chung, S.; Wang, C.; Li, D. Poly(Ethylene Glycol)–Polylactide Micelles for Cancer Therapy. Front. Pharmacol. 2018, 9, 202. [Google Scholar] [CrossRef] [Green Version]
- Essa, D.; Kondiah, P.P.D.; Choonara, Y.E.; Pillay, V. The Design of Poly(lactide-co-glycolide) Nanocarriers for Medical Applications. Front. Bioeng. Biotechnol. 2020, 8, 48. [Google Scholar] [CrossRef]
- Grossen, P.; Witzigmann, D.; Sieber, S.; Huwyler, J. PEG-PCL-based nanomedicines: A biodegradable drug delivery system and its application. J. Control. Release 2017, 260, 46–60. [Google Scholar] [CrossRef]
- Barouti, G.; Jaffredo, C.G.; Guillaume, S.M. Advances in drug delivery systems based on synthetic poly(hydroxybutyrate) (co)polymers. Prog. Polym. Sci. 2017, 73, 1–31. [Google Scholar] [CrossRef]
- Domiński, A.; Konieczny, T.; Zięba, M.; Klim, M.; Kurcok, P. Anionic Polymerization of β-Butyrolactone Initiated with Sodium Phenoxides. The Effect of the Initiator Basicity/Nucleophilicity on the ROP Mechanism. Polymers 2019, 11, 1221. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Meng, F.; Cheng, R.; Deng, C.; Feijen, J.; Zhong, Z. Advanced drug and gene delivery systems based on functional biodegradable polycarbonates and copolymers. J. Control. Release 2014, 190, 398–414. [Google Scholar] [CrossRef]
- Dai, Y.; Zhang, X. Recent development of functional aliphatic polycarbonates in the construction of amphiphilic polymers. Polym. Chem. 2017, 8, 7429–7437. [Google Scholar] [CrossRef]
- Garcia, K.P.; Zarschler, K.; Barbaro, L.; Barreto, J.A.; O’Malley, W.; Spiccia, L.; Stephan, H.; Graham, B. Zwitterionic-Coated “Stealth” Nanoparticles for Biomedical Applications: Recent Advances in Countering Biomolecular Corona Formation and Uptake by the Mononuclear Phagocyte System. Small 2014, 10, 2516–2529. [Google Scholar] [CrossRef]
- Geng, Y.; Discher, D.E. Visualization of degradable worm micelle breakdown in relation to drug release. Polymer 2006, 47, 2519–2525. [Google Scholar] [CrossRef]
- Chow, E.K.-H.; Ho, D. Cancer Nanomedicine: From Drug Delivery to Imaging. Sci. Trans. Med. 2013, 5, 216rv4. [Google Scholar] [CrossRef] [PubMed]
- Domiński, A.; Konieczny, T.; Kurcok, P. α-Cyclodextrin-Based Polypseudorotaxane Hydrogels. Materials 2020, 13, 133. [Google Scholar] [CrossRef] [Green Version]
- Kong, L.; Campbell, F.; Kros, A. DePEGylation strategies to increase cancer nanomedicine efficacy. Nanoscale Horiz. 2019, 4, 378–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barenholz, Y. Doxil®—The first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef]
- Feng, J.; Zhuo, R.-X.; Zhang, X.-Z. Construction of functional aliphatic polycarbonates for biomedical Applications. Prog. Polym. Sci. 2012, 37, 211–236. [Google Scholar] [CrossRef]
- Brannigan, R.P.; Dove, A.P. Synthesis, properties and biomedical applications of hydrolytically degradable materials based on aliphatic polyesters and polycarbonates. Biomater. Sci. 2017, 5, 9–21. [Google Scholar] [CrossRef]
- Tempelaar, S.; Mespouille, L.; Coulembier, O.; Dubois, P.; Dove, A.P. Synthesis and post-polymerisation modifications of aliphatic poly(carbonate)s prepared by ring-opening. Chem. Soc. Rev. 2013, 42, 1312–1336. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Feng, E.; Song, J. Renaissance of aliphatic polycarbonates: New techniques and biomedical Applications. J. Appl. Polym. Sci. 2014, 131, 39822. [Google Scholar] [CrossRef] [Green Version]
- Mespouille, L.; Coulembier, O.; Kawalec, M.; Dove, A.P.; Dubois, P. Implementation of metal-free ring-opening polymerization in the preparation of aliphatic polycarbonate materials. Prog. Polym. Sci. 2014, 39, 1144–1164. [Google Scholar] [CrossRef]
- Mura, S.; Nicolas, J.; Couvreur, P. Stimuli-Responsive Nanocarriers for Drug Delivery. Nat. Mater. 2013, 12, 991–1003. [Google Scholar] [CrossRef]
- Jin, Q.; Deng, Y.; Chen, X.; Ji, J. Rational Design of Cancer Nanomedicine for Simultaneous Stealth Surface and Enhanced Cellular Uptake. ACS Nano 2019, 13(2), 954–977. [Google Scholar] [CrossRef]
- Liu, M.; Du, H.; Zhang, W.; Zhai, G. Internal stimuli-responsive nanocarriers for drug delivery: Design strategies and applications. Mater. Sci. Eng. C 2017, 71, 1267–1280. [Google Scholar] [CrossRef]
- Cheng, R.; Meng, F.; Deng, C.; Zhong, Z. Bioresponsive polymeric nanotherapeutics for targeted cancer chemotherapy. Nanotoday 2015, 10, 656–670. [Google Scholar] [CrossRef]
- Deirram, N.; Zhang, C.; Kermaniyan, S.S.; Johnston, A.P.R.; Such, G.K. pH-Responsive Polymer Nanoparticles for Drug Delivery. Macromol. Rapid Commun. 2019, 40, 1800917. [Google Scholar] [CrossRef] [Green Version]
- Alsehli, M. Polymeric nanocarriers as stimuli-responsive systems for targeted tumor (cancer) therapy: Recent advances in drug delivery. Saudi Pharm. J. 2020, 28, 255–265. [Google Scholar] [CrossRef]
- Roma-Rodrigues, C.; Mendes, R.; Baptista, P.V.; Fernandes, A.R. Targeting Tumor Microenvironment for Cancer Therapy. Int. J. Mol. Sci. 2019, 20, 840. [Google Scholar] [CrossRef] [Green Version]
- Roma-Rodrigues, C.; Pombo, I.; Raposo, L.; Pedrosa, P.; Fernandes, A.R.; Baptista, P.V. Nanotheranostics Targeting the Tumor Microenvironment. Front. Bioeng. Biotechnol. 2019, 7, 197. [Google Scholar] [CrossRef] [Green Version]
- Thakkar, S.; Sharma, D.; Kalia, K.; Tekade, R.K. Tumor microenvironment targeted nanotherapeutics for cancer therapy and diagnosis: A review. Acta Biomater. 2020, 101, 43–68. [Google Scholar] [CrossRef]
- DeBerardinis, R.J.; Chandel, N.S. We need to talk about the Warburg effect. Nat. Metab. 2020, 2, 127–129. [Google Scholar] [CrossRef]
- Lu, J.; Tan, M.; Cai, Q. The Warburg effect in tumor progression: Mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett. Part A 2015, 356, 156–164. [Google Scholar] [CrossRef] [Green Version]
- Warburg, O. On the origin of cancer cells. Science 1956, 123, 309–314. [Google Scholar] [CrossRef]
- van der Heiden, M.G.; Cantley, L.C.; Thompson, C.B. Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation. Science 2009, 324, 1029–1033. [Google Scholar] [CrossRef] [Green Version]
- Krawczyk, M.; Pastuch-Gawołek, G.; Pluta, A.; Erfurt, K.; Domiński, A.; Kurcok, P. 8-Hydroxyquinoline Glycoconjugates: Modifications in the Linker Structure and Their Effect on the Cytotoxicity of the Obtained Compounds. Molecules 2019, 24, 4181. [Google Scholar] [CrossRef] [Green Version]
- Lecouvet, F.E.; Talbot, J.N.; Messiou, C.; Bourguet, P.; Liu, Y.; de Souza, N.M. EORTC Imaging Group. Monitoring the response of bone metastases to treatment with magnetic resonance imaging and nuclear medicine techniques: A review and position statement by the European Organisation for Research and Treatment of Cancer imaging group. Eur. J. Cancer. 2014, 50, 2519–2531. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Meng, F.; Li, F.; Ji, S.-J.; Zhong, Z. pH-Responsive Biodegradable Micelles Based on Acid-Labile Polycarbonate Hydrophobe: Synthesis and Triggered Drug Release. Biomacromolecules 2009, 10, 1727–1735. [Google Scholar] [CrossRef]
- Chen, W.; Meng, F.; Cheng, R.; Zhong, Z. pH-Sensitive degradable polymersomes for triggered release of anticancer drugs: A comparative study with micelles. J. Control. Release 2010, 142, 40–46. [Google Scholar] [CrossRef]
- Domiński, A.; Krawczyk, M.; Konieczny, T.; Kasprow, M.; Foryś, A.; Pastuch-Gawołek, G.; Kurcok, P. Biodegradable pH-responsive micelles loaded with 8-hydroxyquinoline glycoconjugates for Warburg effect based tumor targeting. Eur. J. Pharm. Biopharm. 2020, 154, 317–329. [Google Scholar] [CrossRef]
- Arno, M.C.; Brannigan, R.P.; Policastro, G.M.; Becker, M.L.; Dove, A.P. pH-Responsive, Functionalizable Spyrocyclic Polycarbonate: A Versatile Platform for Biocompatible Nanoparticles. Biomacromolecules 2018, 19, 3427–3434. [Google Scholar] [CrossRef]
- Wu, Y.; Chen, W.; Meng, F.; Wang, Z.; Cheng, R.; Deng, C.; Liu, H.; Zhong, Z. Core-crosslinked pH-sensitive degradable micelles: A promising approach to resolve the extracellular stability versus intracellular drug release dilemma. J. Control. Release 2012, 164, 338–345. [Google Scholar] [CrossRef]
- He, J.; Xia, Y.; Niu, Y.; Hu, D.; Xia, X.; Lu, Y.; Xu, W. pH-responsive core crosslinked polycarbonate micelles via thiol-acrylate Michael addition reaction. J. Appl. Polym. Sci. 2017, 134, 44421. [Google Scholar] [CrossRef]
- Wu, S.; Kuang, H.; Meng, F.; Wu, Y.; Li, X.; Jing, X.; Huang, Y. Facile preparation of core cross-linked micelles from catechol-containing amphiphilic triblock copolymer. J. Mater. Chem. 2012, 22, 15348–15356. [Google Scholar] [CrossRef]
- Zou, Y.; Song, Y.; Yang, W.; Meng, F.; Liu, H.; Zhong, Z. Galactose-installed photo-crosslinked pH-sensitive degradable micelles for active targeting chemotherapy of hepatocellular carcinoma in mice. J. Control. Release 2014, 193, 154–161. [Google Scholar] [CrossRef]
- Chen, W.; Meng, F.; Cheng, R.; Deng, C.; Feijen, J.; Zhong, Z. Facile construction of dual-bioresponsive biodegradable micelles with superior extracellular stability and activated intracellular drug release. J. Control. Release 2015, 210, 125–133. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, X.; Cheng, R.; Zhong, Z. A6 Peptide-Tagged Core-Disulfide-Cross-Linked Micelles for Targeted Delivery of Proteasome Inhibitor Carfilzomib to Multiple Myeloma in vivo. Biomacromolecules 2020, 21, 2049–2059. [Google Scholar] [CrossRef]
- Kuang, H.; Wu, S.; Meng, F.; Xie, Z.; Jinga, X.; Huang, Y. Core-crosslinked amphiphilic biodegradable copolymer based on the complementary multiple hydrogen bonds of nucleobases: Synthesis, self-assembly and in vitro drug delivery. J. Mater. Chem. 2012, 22, 24832–24840. [Google Scholar] [CrossRef]
- Kuang, H.; Wu, S.; Xie, Z.; Meng, F.; Jing, X.; Huang, Y. Biodegradable Amphiphilic Copolymer Containing Nucleobase: Synthesis, Self-Assembly in Aqueous Solutions, and Potential Use in Controlled Drug Delivery. Biomacromolecules 2012, 13, 3004–3012. [Google Scholar] [CrossRef]
- Cheng, D.-B.; Li, Y.-M.; Cheng, Y.-J.; Wu, Y.; Chang, X.-P.; He, F.; Zhuo, R.-X. Thymine-functionalized amphiphilic biodegradable copolymers for high-efficiency loading and controlled release of methotrexate. Colloids Surf. B 2015, 136, 618–624. [Google Scholar] [CrossRef]
- Li, Y.; Chen, S.; Chang, X.; He, F.; Zhuo, R. Efficient Co-delivery of Doxorubicin and Methotrexate by pH-Sensitive Dual-Functional Nanomicelles for Enhanced Synergistic Antitumor Efficacy. ACS Appl. Bio Mater. 2019, 2, 2271–2279. [Google Scholar] [CrossRef]
- Li, Y.-M.; Jiang, T.; Lv, Y.; Wu, Y.; He, F.; Zhuo, R.-X. Amphiphilic copolymers with pendent carboxyl groups for high-efficiency loading and controlled release of doxorubicin. Colloids Surf. B 2015, 132, 54–61. [Google Scholar] [CrossRef]
- Yu, L.; Lin, C.; Zheng, Z.; Li, Z.; Wang, X. Self-assembly of pH-responsive biodegradable mixed micelles based on anionic and cationic polycarbonates for doxorubicin delivery. Colloids Surf. B 2016, 145, 392–400. [Google Scholar] [CrossRef]
- Chan, J.M.W.; Tan, J.P.K.; Engler, A.C.; Ke, X.; Gao, S.; Yang, C.; Sardon, H.; Yang, Y.Y.; Hedrick, J.L. Organocatalytic Anticancer Drug Loading of Degradable Polymeric Mixed Micelles via a Biomimetic Mechanism. Macromolecules 2016, 49, 2013–2021. [Google Scholar] [CrossRef]
- Aguirre-Chagala, Y.E.; Santos, J.L.; Huang, Y.; Herrera-Alonso, M. Phenylboronic Acid-Installed Polycarbonates for the pH-Dependent Release of Diol-Containing Molecules. ACS Macro Lett. 2014, 3, 1249–1253. [Google Scholar] [CrossRef]
- Garcia, E.A.; Pessoa, D.; Herrera-Alonso, M. Oxidative instability of boronic acid-installed polycarbonate nanoparticles. Soft Matter 2020, 16, 2473–2479. [Google Scholar] [CrossRef]
- Liu, S.; Ono, R.J.; Yang, C.; Gao, S.; Tan, J.Y.M.; Hedrick, J.L.; Yang, Y.Y. Dual pH-Responsive Shell-Cleavable Polycarbonate Micellar Nanoparticles for in Vivo Anticancer Drug Delivery. ACS Appl. Mater. Interfaces 2018, 10, 19355–19364. [Google Scholar] [CrossRef]
- Tan, J.P.K.; Voo, Z.X.; Lima, S.; Venkataraman, S.; Ng, K.M.; Gao, S.; Hedrick, J.L.; Yang, Y.Y. Effective encapsulation of apomorphine into biodegradable polymeric nanoparticles through a reversible chemical bond for delivery across the blood–brain barrier. Nanomedicine 2019, 17, 236–245. [Google Scholar] [CrossRef]
- Sonawane, S.J.; Kalhapure, R.S.; Govender, T. Hydrazone linkages in pH responsive drug delivery systems. Eur. J. Pharm. Sci. 2017, 99, 45–65. [Google Scholar] [CrossRef]
- Ke, X.; Coady, D.J.; Yang, C.; Engler, A.C.; Hedrick, J.L.; Yang, Y.Y. pH-sensitive polycarbonate micelles for enhanced intracellular release of anticancer drugs: A strategy to circumvent multidrug resistance. Polym. Chem. 2014, 5, 2621–2628. [Google Scholar] [CrossRef]
- Wang, H.; Wang, Y.; Chen, Y.; Jin, Q.; Ji, J. A biomimic pH-sensitive polymeric prodrug based on polycarbonate for intracellular drug delivery. Polym. Chem. 2014, 5, 854–861. [Google Scholar] [CrossRef]
- Jiang, T.; Li, Y.-M.; Lv, Y.; Cheng, Y.-J.; He, F.; Zhuo, R.-X. Amphiphilic polycarbonate conjugates of doxorubicin with pH-sensitive hydrazone linker for controlled release. Colloids Surf. B 2013, 111, 542–548. [Google Scholar] [CrossRef]
- Ganivada, M.N.; Kumar, P.; Kanjilal, P.; Dinda, H.; Das Sarma, J.; Shunmugam, R. Polycarbonate Based Biodegradable Copolymers for Stimuli Responsive Targeted Drug Delivery. Polym. Chem. 2016, 7, 4237–4245. [Google Scholar] [CrossRef]
- Sun, J.; Fransen, S.; Yu, X.; Kuckling, D. Synthesis of pH-cleavable poly(trimethylene carbonate)-based block copolymers via ROP and RAFT polymerization. Polym. Chem. 2018, 9, 3287–3296. [Google Scholar] [CrossRef]
- Venkataraman, S.; Tan, J.P.K.; Ng, V.W.L.; Tan, E.W.P.; Hedrick, J.L.; Yang, Y.Y. Amphiphilic and Hydrophilic Block Copolymers from Aliphatic N-Substituted 8-Membered Cyclic Carbonates: A Versatile Macromolecular Platform for Biomedical Applications. Biomacromolecules 2017, 18, 178–188. [Google Scholar] [CrossRef]
- Su, W.; Wang, H.-F.; Feng, J.; Luo, X.-H.; Zhang, X.-Z.; Zhuo, R.-X. Novel cationic poly(ester-co-carbonate) materials functionalized with tertiary amine groups. J. Mater. Chem. 2011, 21, 6327–6336. [Google Scholar] [CrossRef]
- Wang, H.-F.; Luo, X.-H.; Liu, C.-W.; Feng, J.; Zhang, X.-Z.; Zhuo, R.-X. A smart micellar system with an amine-containing polycarbonate shell. Acta Biomater. 2012, 8, 589–598. [Google Scholar] [CrossRef]
- Wang, H.-F.; Jia, H.-Z.; Cheng, S.-X.; Feng, J.; Zhang, X.-Z.; Zhuo, R.-X. PEG-Stabilized Micellar System with Positively Charged Polyester Core for Fast pH-Responsive Drug Release. Pharm. Res. 2012, 29, 1582–1594. [Google Scholar] [CrossRef]
- Wang, H.-F.; Jia, H.-Z.; Zhu, J.-Y.; Chu, Y.-F.; Feng, J.; Zhang, X.-Z.; Zhuo, R.-X. One-Step Preparation and pH-Tunable Self-Aggregation of Amphoteric Aliphatic Polycarbonates Bearing Plenty of Amine and Carboxyl Groups. Macromol. Biosci. 2012, 12, 1689–1696. [Google Scholar] [CrossRef]
- Wang, H.-F.; Jia, H.-Z.; Chu, Y.-F.; Feng, J.; Zhang, X.-Z.; Zhuo, R.-X. Acidity-Promoted Cellular Uptake and Drug Release Mediated by Amine Functionalized Block Polycarbonates Prepared via One-Shot Ring-Opening Copolymerization. Macromol. Biosci. 2014, 14, 526–536. [Google Scholar] [CrossRef]
- Ray, P.; Confeld, M.; Borowicz, P.; Wang, T.; Mallik, S.; Quadir, M. PEG-b-poly(carbonate)-derived nanocarrier platform with pH-responsive properties for pancreatic cancer combination therapy. Colloids Surf. B 2019, 174, 126–135. [Google Scholar] [CrossRef]
- Zhang, P.; Wu, J.; Xiao, F.; Zhao, D.; Luan, Y. Disulfide bond based polymeric drug carriers for cancer chemotherapy and relevant redox environments in mammals. Med. Res. Rev. 2018, 38, 1485–1510. [Google Scholar] [CrossRef]
- Prior, R.L.; Cao, G. In vivo total antioxidant capacity: Comparision of different analytical methods. Free Radic. Biol. Med. 1999, 27, 1173–1181. [Google Scholar] [CrossRef]
- Kamaly, N.; Yameen, B.; Wu, J.; Farokhzad, O.C. Degradable Controlled-Release Polymers and Polymeric Nanoparticles: Mechanisms of Controlling Drug Release. Chem. Rev. 2016, 116, 2602–2663. [Google Scholar] [CrossRef] [Green Version]
- Ortega, A.L.; Mena, S.; Estrela, J.M. Glutathione in Cancer Cell Death. Cancers 2011, 3, 1285–1310. [Google Scholar] [CrossRef] [Green Version]
- Tormos, C.; Javier Chaves, F.; Garcia, M.J.; Garrido, F.; Jover, R.; O’Connor, J.E.; Iradi, A.; Oltra, A.; Oliva, M.R.; Saez, G.T. Role of glutathione in the induction of apoptosis and c-fos and c-jun mrnas by oxidative stress in tumor cells. Cancer Lett. 2004, 208, 103–113. [Google Scholar] [CrossRef]
- Schnelldorfer, T.; Gansauge, S.; Gansauge, F.; Schlosser, S.; Beger, H.G.; Nussler, A.K. Glutathione depletion causes cell growth inhibition and enhanced apoptosis in pancreatic cancer cells. Cancer 2000, 89, 1440–1447. [Google Scholar] [CrossRef]
- Lu, G.D.; Shen, H.M.; Chung, M.C.; Ong, C.N. Critical role of oxidative stress and sustained jnk activation in aloe-emodin-mediated apoptotic cell death in human hepatoma cells. Carcinogenesis 2007, 28, 1937–1945. [Google Scholar] [CrossRef]
- Mena, S.; Benlloch, M.; Ortega, A.; Carretero, J.; Obrador, E.; Asensi, M.; Petschen, I.; Brown, B.D.; Estrela, J.M. Bcl-2 and glutathione depletion sensitizes b16 melanoma to combination therapy and eliminates metastatic disease. Clin. Cancer Res. 2007, 13, 2658–2666. [Google Scholar] [CrossRef] [Green Version]
- Fleige, E.; Quadir, M.A.; Haag, R. Stimuli-responsive polymeric nanocarriers for the controlled transport of active compounds: Concepts and applications. Adv. Drug Deliv. Rev. 2012, 64, 866–884. [Google Scholar] [CrossRef]
- Yi, X.; Zhao, D.; Zhang, Q.; Xu, J.; Yuan, G.; Zhuo, R.; Li, F. A co-delivery system based on reduction-sensitive polymeric prodrug capable of loading hydrophilic and hydrophobic drugs for combination chemotherapy. Polym. Chem. 2016, 7, 5966–5977. [Google Scholar] [CrossRef]
- Chen, W.; Zou, Y.; Meng, F.; Cheng, R.; Deng, C.; Feijen, J.; Zhong, Z. Glyco-Nanoparticles with Sheddable Saccharide Shells: A Unique and Potent Platform for Hepatoma-Targeting Delivery of Anticancer Drugs. Biomacromolecules 2014, 15, 900–907. [Google Scholar] [CrossRef]
- Gajbhiye, K.R.; Gajbhiye, V.; Siddiqui, I.A.; Gajbhiye, J.M. cRGD functionalized nanocarriers for targeted delivery of bioactives. J. Drug Target. 2019, 27, 111–124. [Google Scholar] [CrossRef]
- Zou, Y.; Fang, Y.; Meng, H.; Meng, F.; Deng, C.; Zhang, J.; Zhong, Z. Self-Crosslinkable and Intracellularly Decrosslinkable Biodegradable Micellar Nanoparticles: A Robust, Simple and Multifunctional Nanoplatform for High-Efficiency Targeted Cancer Chemotherapy. J. Control. Release 2016, 244, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Zou, Y.; Zhong, P.; Meng, F.; Zhang, J.; Cheng, R.; Zhong, Z. A Smart Nano-Prodrug Platform with Reactive Drug Loading, Superb Stability, and Fast Responsive Drug Release for Targeted Cancer Therapy. Macromol. Biosci. 2017, 17, 1600518. [Google Scholar] [CrossRef] [Green Version]
- Bahrami, B.; Mohammadnia-Afrouzi, M.; Bakhshaei, P.; Yazdani, Y.; Ghalamfarsa, G.; Yousefi, M.; Sadreddini, S.; Jadidi-Niaragh, F.; Hojjat-Farsangi, M. Folate-conjugated nanoparticles as a potent therapeutic approach in targeted cancer therapy. Tumor Biol. 2015, 36, 5727–5742. [Google Scholar] [CrossRef]
- Lv, Y.; Yang, B.; Li, Y.-M.; He, F.; Zhuo, R.-X. Folate-conjugated amphiphilic block copolymer micelle for targeted and redox responsive delivery of doxorubicin. J. Biomater. Sci. Polym. Ed. 2018, 28, 92–106. [Google Scholar] [CrossRef]
- Gao, L.; Dong, B.; Zhang, J.; Chen, Y.; Qiao, H.; Liu, Z.; Chen, E.; Dong, Y.; Cao, C.; Huang, D.; et al. Functional Biodegradable Nitric Oxide Donor-Containing Polycarbonate-Based Micelles for Reduction-Triggered Drug Release and Overcoming Multidrug Resistance. ACS Macro Lett. 2019, 8, 1552–1558. [Google Scholar] [CrossRef]
- Engler, A.C.; Chan, J.M.W.; Fukushima, K.; Coady, D.J.; Yang, Y.Y.; Hedrick, J.L. Polycarbonate-Based Brush Polymers with Detachable Disulfide-Linked Side Chains. ACS Macro Lett. 2013, 2, 332–336. [Google Scholar] [CrossRef]
- Chen, W.; Zou, Y.; Jia, J.; Meng, F.; Cheng, R.; Deng, C.; Feijen, J.; Zhong, Z. Functional Poly(ε-caprolactone)s via Copolymerization of ε-Caprolactone and Pyridyl Disulfide Containing Cyclic Carbonate: Controlled Synthesis and Facile Access to Reduction-Sensitive Biodegradable Graft Copolymer Micelles. Macromolecules 2013, 46, 699–707. [Google Scholar] [CrossRef]
- Yan, L.; Wu, W.; Zhao, W.; Qi, R.; Cui, D.; Xie, Z.; Huang, Y.; Tong, T.; Jing, X. Reduction-sensitive core-cross-linked mPEG–poly(ester-carbonate) micelles for glutathione-triggered intracellular drug release. Polym. Chem. 2012, 3, 2403–2412. [Google Scholar] [CrossRef]
- Wang, Y.; Du, H.; Gao, L.; Ni, H.; Li, X.; Zhu, W.; Shen, Z. Reductively and hydrolytically dual degradable nanoparticles by “click” crosslinking of a multifunctional diblock copolymer. Polym. Chem. 2013, 4, 1657–1663. [Google Scholar] [CrossRef]
- Zhu, W.; Wang, Y.; Cai, X.; Zha, G.; Luo, Q.; Sun, R.; Li, X.; Shen, Z. Reduction-Triggered Release of Paclitaxel From In Situ Formed Biodegradable Core-Crosslinked Micelles. J. Mater. Chem. B 2015, 3, 3024–3031. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, H.; Fu, S.; Zhong, Z.; Zhuo, R. Redox-Responsive Micelles with Cores Crosslinked via Click Chemistry. Macromol. Rapid Commun. 2016, 37, 993–997. [Google Scholar] [CrossRef]
- Yi, X.; Zhang, Q.; Dong, H.; Zhao, D.; Xu, J.; Zhuo, R.; Li, F. One-pot synthesis of crosslinked amphiphilic polycarbonates as stable but reduction-sensitive carriers for doxorubicin delivery. Nanotechnology 2015, 26, 395602. [Google Scholar] [CrossRef]
- Xia, Y.; Wang, N.; Qin, Z.; Wu, J.; Wang, F.; Zhang, L.; Xia, X.; Li, J.; Lu, Y. Polycarbonate-based core-crosslinked redox-responsive nanoparticles for targeted delivery of anticancer drug. J. Mater. Chem. B 2018, 6, 3348–3357. [Google Scholar] [CrossRef]
- Xia, Y.; He, H.; Liu, X.; Hu, D.; Yin, L.; Lu, Y.; Xu, W. Redox-responsive core crosslinked degradable micelles for controlled drug release. Polym. Chem. 2016, 7, 6330–6339. [Google Scholar] [CrossRef]
- Zhu, C.; Zang, L.; Zheng, D.; Cao, H.; Liu, X. Small-sized copolymeric nanoparticles for tumor penetration and intracellular drug release. Chem. Commun. 2020, 56, 2000–2003. [Google Scholar] [CrossRef]
- Ovais, M.; Mukherjee, S.; Pramanik, A.; Das, D.; Mukherjee, A.; Raza, A.; Chen, C. Designing Stimuli-Responsive Upconversion Nanoparticles that Exploit the Tumor Microenvironment. Adv. Mater. 2020, 2000055. [Google Scholar] [CrossRef]
- Schumacker, P.T. Reactive Oxygen Species in Cancer: A Dance with the Devil. Cancer Cell 2015, 27, 156–157. [Google Scholar] [CrossRef] [Green Version]
- Ye, H.; Zhou, Y.; Liu, X.; Chen, Y.; Duan, S.; Zhu, R.; Liu, Y.; Yin, L. Recent Advances on Reactive Oxygen Species-Responsive Delivery and Diagnosis System. Biomacromolecules 2019, 20, 2441–2463. [Google Scholar] [CrossRef]
- Liu, J.; Li, Y.; Chen, S.; Lin, Y.; Lai, H.; Chen, B.; Chen, T. Biomedical Application of Reactive Oxygen Species–Responsive Nanocarriers in Cancer, Inflammation, and Neurodegenerative Diseases. Front. Chem. 2020, 8, 838. [Google Scholar] [CrossRef]
- Yan, B.; Zhang, Y.; Wei, C.; Xu, Y. Facile synthesis of ROS-responsive biodegradable main chain poly(carbonate-thioether) copolymers. Polym. Chem. 2018, 9, 904–911. [Google Scholar] [CrossRef]
- Wang, D.; Wang, S.; Xia, Y.; Liu, S.; Jia, R.; Xu, G.; Zhan, J.; Lu, Y. Preparation of ROS-responsive Core Crosslinked Polycarbonate Micelles with thioketal linkage. Colloids Surf. B 2020, 195, 111276. [Google Scholar] [CrossRef]
- Yang, X.-L.; Xing, X.; Li, J.; Liu, Y.-H.; Wang, N.; Yu, X.-Q. Enzymatic synthesis of selenium-containing amphiphilic aliphatic polycarbonate as an oxidation-responsive drug delivery vehicle. RSC Adv. 2019, 9, 6003–6010. [Google Scholar] [CrossRef] [Green Version]
- Yu, L.; Yang, Y.; Du, F.-S.; Li, Z.-C. ROS-Responsive Chalcogen-Containing Polycarbonates for Photodynamic Therapy. Biomacromolecules 2018, 19, 2182–2193. [Google Scholar] [CrossRef]
- Yu, L.; Ke, H.-L.; Du, F.-S.; Li, Z.-C. Redox-Responsive Fluorescent Polycarbonates Based on Selenide for Chemotherapy of Triple-Negative Breast Cancer. Biomacromolecules 2019, 20, 2809–2820. [Google Scholar] [CrossRef]
- Zhao, W.; Zhao, Y.; Wang, Q.; Liu, T.; Sun, J.; Zhang, R. Remote Light-Responsive Nanocarriers for Controlled Drug Delivery: Advances and Perspectives. Small 2019, 15, 1903060. [Google Scholar] [CrossRef]
- Delaney, G.; Jacob, S.; Featherstone, C.; Barton, M. The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer 2005, 104, 1129–1137. [Google Scholar] [CrossRef]
- Linsley, C.S.; Wu, B.M. Recent Advances in Light-Responsive on-demand Drug-Delivery Systems. Ther. Delivery 2017, 8, 89–107. [Google Scholar] [CrossRef] [Green Version]
- Raza, A.; Hayat, U.; Rasheed, T.; Bilal, M.; Iqbal, H.M.N. “Smart” materials-based nearinfrared light-responsive drug delivery systems for cancer treatment: A review. J. Mater. Res. Technol. 2019, 8, 1497–1509. [Google Scholar] [CrossRef]
- Hu, D.; Li, Y.; Niu, Y.; Li, L.; He, J.; Liu, X.; Xia, X.; Lu, Y.; Xiong, Y.; Xu, W. Photo-responsive reversible micelles based on azobenzene-modified poly(carbonate)s via azide–alkyne click chemistry. RSC Adv. 2014, 4, 47929–47936. [Google Scholar] [CrossRef]
- Hu, D.; Peng, H.; Niu, Y.; Li, Y.; Xia, Y.; Li, L.; He, J.; Liu, X.; Xia, X.; Lu, Y.; et al. Reversibly Light-Responsive Biodegradable Poly(carbonate)s Micelles Constructed Via CuAAC Reaction. J. Polym. Sci. Part A Polym. Chem 2015, 53, 750–760. [Google Scholar] [CrossRef]
- Shen, H.; Xia, Y.; Qin, Z.; Wu, J.; Zhang, L.; Lu, Y.; Xia, X.; Xu, W. Photoresponsive Biodegradable Poly(Carbonate)s with Pendent o-Nitrobenzyl Ester. J. Polym. Sci. Part A Polym. Chem. 2017, 55, 2770–2780. [Google Scholar] [CrossRef]
- Fang, J.-Y.; Lin, Y.-K.; Wang, S.-W.; Li, Y.-C.; Lee, R.-S. Synthesis and characterization of dual-stimuli-responsive micelles based on poly(N-isopropylacrylamide) and polycarbonate with photocleavable moieties. React. Funct. Polym. 2015, 95, 46–54. [Google Scholar] [CrossRef]
- Sun, J.; Birnbaum, W.; Anderski, J.; Picker, M.-T.; Mulac, D.; Langer, K.; Kuckling, D. Use of Light-Degradable Aliphatic Polycarbonate Nanoparticles As Drug Carrier for Photosensitizer. Biomacromolecules 2018, 19, 4677–4690. [Google Scholar] [CrossRef]
- Anderski, J.; Mahlert, L.; Sun, J.; Birnbaum, W.; Mulac, D.; Schreiber, S.; Herrmann, F.; Kuckling, D.; Langer, K. Light-responsive nanoparticles based on new polycarbonate polymers as innovative drug delivery systems for photosensitizers in PDT. Int. J. Pharm. 2019, 557, 182–191. [Google Scholar] [CrossRef]
- Sun, J.; Jung, D.; Schoppa, T.; Anderski, J.; Picker, M.-T.; Ren, Y.; Mulac, D.; Stein, N.; Langer, K.; Kuckling, D. Light-Responsive Serinol-Based Polycarbonate and Polyester as Degradable Scaffolds. ACS Appl. Bio Mater. 2019, 2, 3038–3051. [Google Scholar] [CrossRef]
- Sun, J.; Anderski, J.; Picker, M.-T.; Langer, K.; Kuckling, D. Preparation of Light-Responsive Aliphatic Polycarbonate via Versatile Polycondensation for Controlled Degradation. Macromol. Chem. Phys. 2019, 220, 1800539. [Google Scholar] [CrossRef]
- Mahlert, L.; Anderski, J.; Schoppa, T.; Mulac, D.; Sun, J.; Kuckling, D.; Langer, K. In vitro evaluation of innovative light-responsive nanoparticles for controlled drug release in intestinal PDT. Int. J. Pharm. 2019, 565, 199–208. [Google Scholar] [CrossRef]
- Müller, A.-K.; Jung, D.; Sun, J.; Kuckling, D. Synthesis and characterization of light-degradable bromocoumarin functionalized polycarbonates. Polym. Chem. 2020, 11, 721–733. [Google Scholar] [CrossRef]
- Grzywa, T.M.; Paskal, W.; Wlodarski, P.K. Intratumor and intertumor heterogeneity in melanoma. Transl. Oncol. 2017, 10, 956–975. [Google Scholar] [CrossRef]
- Chen, W.; Zhong, P.; Meng, F.; Cheng, R.; Deng, C.; Feijen, J.; Zhong, Z. Redox and pH-Responsive Degradable Micelles for Dually Activated Intracellular Anticancer Drug Release. J. Control. Release 2013, 169, 171–179. [Google Scholar] [CrossRef]
- Yi, X.-Q.; Zhang, Q.; Zhao, D.; Xu, J.-Q.; Zhong, Z.-L.; Zhuo, R.-X.; Li, F. Preparation of pH and redox dual-sensitive core crosslinked micelles for overcoming drug resistance of DOX. Polym. Chem. 2016, 7, 1719–1729. [Google Scholar] [CrossRef]
- Teo, J.Y.; Chin, W.; Ke, X.; Gao, S.; Liu, S.; Cheng, W.; Hedrick, J.L.; Yang, Y.Y. pH and redox dual-responsive biodegradable polymeric micelles with high drug loading for effective anticancer drug delivery. Nanomedicine 2017, 13, 431–442. [Google Scholar] [CrossRef]
- Hu, J.; Xu, Y.; Zhang, Y. Amphiphilic random polycarbonate self-assemble into GSH/pH dual responsive micelle-like aggregates in water. Chin. Chem. Lett. 2019, 30, 2039–2042. [Google Scholar] [CrossRef]
- Yu, L.; Tan, S.W.; Li, Z.; Zheng, Z.; Zhou, L.Z.; Su, Y.; Wang, X.L. Mixed polycarbonate prodrug nanoparticles with reduction/pH dualresponsive and charge conversional properties. React. Funct. Polym. 2017, 120, 74–82. [Google Scholar] [CrossRef]
- Leong, J.; Chin, W.; Ke, X.; Gao, S.; Kong, H.; Hedrick, J.L.; Yang, Y.Y. Disease-directed design of biodegradable polymers: Reactive oxygen species and pH-responsive micellar nanoparticles for anticancer drug delivery. Nanomedicine 2018, 14, 2666–2677. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, Y.; Wei, C.; Sun, C.; Yan, B.; Hua, J.; Lu, W. One-shot synthesis and solution properties of ROS/pH responsive Methoxy poly(ethylene glycol)-b-polycarbonate. Polym. Chem. 2019, 10, 2143–2151. [Google Scholar] [CrossRef]
- Yang, X.-L.; Li, J.; Wu, W.-X.; Liu, Y.-H.; Wang, N.; Yu, X.-Q. Preparation of fluorophore-tagged polymeric drug delivery vehicles with multiple biological stimuli-triggered drug release. Mater. Sci. Eng. C 2020, 108, 110358. [Google Scholar] [CrossRef]
- Xia, Y.; Zeng, Y.; Hu, D.; Shen, H.; Deng, J.; Lu, Y.; Xia, X.; Xu, W. Light and pH Dual-Sensitive Biodegradable Polymeric Nanoparticles for Controlled Release of Cargos. J. Polym. Sci. Part A Polym. Chem. 2017, 55, 1773–1783. [Google Scholar] [CrossRef]
- Xie, M.; Yu, L.; Li, Z.; Zheng, Z.; Wang, X. Synthesis and Character of Novel Polycarbonate for Constructing Biodegradable Multi-Stimuli Responsive Delivery System. J. Polym. Sci. Part A Polym. Chem. 2016, 54, 3583–3592. [Google Scholar] [CrossRef]
- Kalva, N.; Uthaman, S.; Augustine, R.; Jeon, S.H.; Huh, K.M.; Park, I.; Kim, I. Photo- and pH-Responsive Polycarbonate Block Copolymer Prodrug Nanomicelles for Controlled Release of Doxorubicin. Macromol. Biosci. 2020, 20, 2000118. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Sun, C.; Hu, J.; Huang, Y.; Lu, Y.; Zhang, Y. Ring Opening Copolymerization of ε-Caprolactone and Diselenic Macrolide Carbonate for Well-Defined Poly(ester-co-carbonate): Kinetic Evaluation and ROS/GSH Responsiveness. Polym. Chem. 2020, 11, 1597–1605. [Google Scholar] [CrossRef]
- Sun, C.; Wang, J.; Hu, J.; Lu, W.; Song, Z.; Zhang, Y. Facile synthesis of a well-defined heteroatomcontaining main chain polycarbonate for activated intracellular drug release. Mater. Chem. Front. 2020, 4, 2443–2451. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic. Bioeng. Transl. Med. 2016, 1, 10–29. [Google Scholar] [CrossRef]
- Mi, P.; Cabral, H.; Kataoka, K. Ligand-Installed Nanocarriers toward Precision Therapy. Adv. Mater. 2019, 1902604. [Google Scholar] [CrossRef]











Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domiński, A.; Konieczny, T.; Duale, K.; Krawczyk, M.; Pastuch-Gawołek, G.; Kurcok, P. Stimuli-Responsive Aliphatic Polycarbonate Nanocarriers for Tumor-Targeted Drug Delivery. Polymers 2020, 12, 2890. https://doi.org/10.3390/polym12122890
Domiński A, Konieczny T, Duale K, Krawczyk M, Pastuch-Gawołek G, Kurcok P. Stimuli-Responsive Aliphatic Polycarbonate Nanocarriers for Tumor-Targeted Drug Delivery. Polymers. 2020; 12(12):2890. https://doi.org/10.3390/polym12122890
Chicago/Turabian StyleDomiński, Adrian, Tomasz Konieczny, Khadar Duale, Monika Krawczyk, Gabriela Pastuch-Gawołek, and Piotr Kurcok. 2020. "Stimuli-Responsive Aliphatic Polycarbonate Nanocarriers for Tumor-Targeted Drug Delivery" Polymers 12, no. 12: 2890. https://doi.org/10.3390/polym12122890