Inhalable Formulations to Treat Non-Small Cell Lung Cancer (NSCLC): Recent Therapies and Developments
Abstract
:1. Introduction
2. Advantages and Challenges of Inhalable Anticancer Therapy
3. Physicochemical Properties
3.1. Size of Nanoparticles
3.2. Surface Properties
3.3. Lipophilicity
3.4. Nanoparticle Surface Modifications
4. Inhalable Formulations
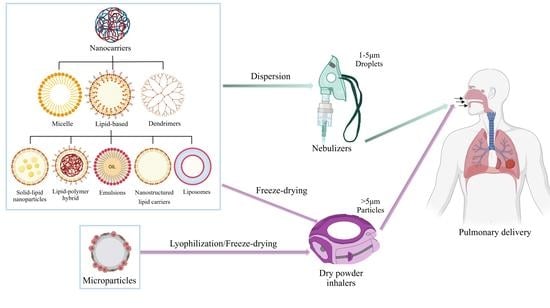
4.1. Nanocarriers
4.1.1. Polymeric Nanoparticles
4.1.2. Dendrimers
4.1.3. Lipid-Based Nanocarriers
Liposomes
Nanoemulsions
Solid Lipid Nanocarriers
Nanostructured Lipid Carriers
Lipid–Polymer Hybrid Nanocarriers
| Drug | Lipid-Based Carrier | Composition | Key Outcome | Refs. |
|---|---|---|---|---|
| 9-Nitrocamptothecin (9NC) | Liposome | Dilauroylphosphatidylcholine (DLPC) | The dose of aerosolized L-9NC was 3–20 times lower than the intramuscular and intravenous doses of 9NC. | [111] |
| Camptothecin (CPT) | Liposome | Dilauroylphosphatidylcholine (DLPC) | The highest drug concentrations in the lungs were obtained with the inhalable CPT liposome aerosol. | [112] |
| Paclitaxel | Liposome in bacteria | Soybean lecithin and cholesterol, E. coli | Highest anticancer effect, with VEGF and HIF-1 downregulation and improved cancer cell apoptosis. | [113] |
| Paclitaxel | Liposome | Dilauroylphosphatidylcholine (DLPC) | The AUC in the aerosol group was 26 times higher than the IV injection group. | [71] |
| Curcumin | Liposome | Poloxamer 188, 2-hydroxypropyl—cyclodextrin, lecithin, cholesterol, stearylamine | Liposome formulation outperformed curcumin powder in terms of rate and extent of lung tissue absorption, as well as mean residence time within lung tissues. | [114] |
| Curcumin | Liposome | Soybean lecithin and cholesterol | Liposomal curcumin dry powder demonstrated superior anticancer activity and selectivity over free curcumin. | [68] |
| Doxorubicin | Transferrin-conjugated liposome | DSPC, DSPE-PEG2000, DSPE-PEG-COOH, and cholesterol | The group of animals treated with TF-liposomes lived longer than those in the other treatment regimens, and tumor size was reduced. | [115] |
| Vincristine | Liposome | Soy phosphatidylcholine and cholesterol | In comparison to the free drug, the developed formulation had improved pharmacokinetic behavior, with increased maximum concentration and systemic exposure and decreased elimination half-life. | [116] |
| Docetaxel | Nano emulsion | Lauric fatty acids. Myristic fatty acids, PKOE, lecithin, Tween 85®, Span 85®, and glycerol | Good inhalable formulation for administration of docetaxel. Human lung carcinoma cell (A549) is more selective than normal cell (MRC-5). | [90] |
| Docetaxel and Curcumin | Nano emulsion | PKOE, lauric FA, myristic FA, lecithin, Tween 85®, Span 85®, and glycerol | Docetaxel and curcumin had a synergistic anticancer effect, and the nanoemulsion had desirable physicochemical and aerodynamic properties for pulmonary delivery. | [117] |
| Blank formulation | SLN | Lipid mixture (Softisan® and Phospholipon® 90G) and Solutol® HS15 as surfactant. | Blank SLNs are adequate for pulmonary delivery of drugs, intratracheally. There are no side effects or indicators of cell death or inflammation. | [97] |
| Erlotinib | SLN | Compritol 888 ATO®, Tween 80®, poloxamer 407®. | The created erlotinib loaded SLNs outperformed free erlotinib in terms of cumulative drug release profile and anticancer activity. | [118] |
| Myricetin | SLN | Gelucires (G 39/01, 50/13, 44/14) and compritol | The use of gelucire-based SLNs was proven to improve the drug’s physiochemical properties, release, and anticancer effects. | [119] |
| Paclitaxel | NLC | Precirol ATO 5®, squalene, Tween 80® | Inhaled NLCs had the highest drug concentration in the mice’s lungs, with no signs of systematic cytotoxicity when contrasted to the IV route. | [120] |
| Paclitaxel | NLC | Stearic acid (or glyceryl monostearate) oleic acid, Tween 80®, Tween 20®, or Tween 40® | When compared to free drug treatment, inhaled paclitaxel-NLCs demonstrated favorable organ distribution and superior anticancer effect. | [121] |
| Celecoxib combined with IV docetaxel | NLC | Compritol®, miglyol®, and sodium taurocholate | The synergistic effects of celecoxib-NLCs inhalation and IV docetaxel were demonstrated in vivo. | [122] |
| siRNA | LPHNs | Poly(lactic-co-glycolic) acid and Dipalmitoylphosphatidylcholine | Inhibition of ENaC protein expression in A549 cell lines for an extended period of time was observed. In vitro aerosol performance was found to be optimal after using a vibrating mesh nebulizer for delivery. | [123] |
| Gemcitabine and cisplatin | Niosomes | Tween 65®, Span 60®, cholesterol, sodium dodecyl sulfate (SDS), glycerol | Developed NGCs had a lower cytotoxicity effect against MRC5 as compared to the free drug. | [124] |
4.1.4. Gelatin-Based Nanocarriers
4.1.5. Inorganic Nanocarriers
4.1.6. Micelles
4.1.7. Aptamers
4.2. Microparticles
4.3. Nanocomposites and Nanoaggregates
4.3.1. Nanocomposites
4.3.2. Nanoaggregates
5. Toxicity Concerns
5.1. Toxicity Concerns Related to Inhalable Formulations
5.2. Toxicity and Safety Concerns as per NIOSH Guidelines
- Drug potency and its toxicity;
- Route of exposure;
- Drug’s physical and chemical properties;
- Type of drug formulation (such as liquid, powder, capsule, or pre-filled syringe).
6. Devices Used for Pulmonary Delivery
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NSCLC | Non-small cell lung cancer |
| SCLC | Small-cell lung carcinoma |
| DPIs | Dry-powder inhalers |
| Dae | Aerodynamic diameter |
| EPR | Enhanced permeability and retention |
| PLGA | Polylactic-co-glycolic |
| PEG | Polyethylene glycol |
| CD-RES NP | Resveratrol-cyclodextrin nanoparticles |
| SF | Sorafenib |
| PLA | Poly-L-arginine |
| DOX | Doxorubicin |
| AQ | Amodiaquine |
| HPH | High-pressure homogenization |
| BSA | Bovine serum albumin |
| PEI | Polyethyleneimine |
| Cs | Chitosan |
| F | Fucoidan |
| HTCC | N-[(2-hydroxy-3- trimethylammonium)propyl] chitosan chloride |
| SLNs | Solid lipid nanoparticles |
| LPN | Lipid–polymer hybrid nanoparticles |
| NLCs | Nanostructured lipid carriers |
| SD | Sprague–Dawley |
| PFD | Pirfenidone |
| PTX | Paclitaxel |
| DLPC | Dilauroylphosphatidyl choline |
| CLH | Hydroxycamptothecin |
| 5-ALA | 5-aminolevulinic acid |
| 5-FU | 5-Fluorouracil |
| DPPC | Dipalmitoyl phosphatidylcholine |
| DPPG | Dipalmitoyl phosphatidylglycerol |
| DPPA | Dipalmitoyl phosphatidic acid |
| NEs | Nanoemulsions |
| PDI | Polydispersity index |
| LDH | Lactate dehydrogenase |
| CU | Curcumin |
| DOTAP | (N-[1-(2,3-dioleoyloxy)propyl]-N,N,N-trimethylammonium) or 1, 2-dioleoyl-3-trimethylammonium propane |
| LPHNs | Lipid–polymer hybrid nanoparticles |
| DLPC | Dilauroylphosphatidylcholine |
| 9NC | 9-Nitrocamptothecin |
| GPs | Gelatin nanoparticles |
| MNPs | Magnetic nanoparticles |
| MSNs | Mesoporous silica NPs |
| ZnO-NPs | Zinc oxide nanoparticles |
| Cp | Cisplatin |
| Sb-GNPs | Gemcitabine (Gem) silibinin-loaded gold nanoparticles |
| CMC | Critical micellar concentration |
| DTX | Docetaxel |
| pMDIs | Pressurized metered-dose inhalers |
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Horn, L.; Lovly, C.M. Neoplasms of the Lung. In Harrison’s Principles of Internal Medicine, 20th ed.; Jameson, J.L., Fauci, A.S., Kasper, D.L., Hauser, S.L., Longo, D.L., Loscalzo, J., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- PDQ Adult Treatment Editorial Board. Small Cell Lung Cancer Treatment (PDQ®): Health Professional Version; National Cancer Institute: Bethesda, MD, USA, 2002. [Google Scholar]
- Chang, A. Chemotherapy, Chemoresistance and the Changing Treatment Landscape for NSCLC. Lung Cancer 2011, 71, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Postmus, P.E.; Kerr, K.M.; Oudkerk, M.; Senan, S.; Waller, D.A.; Vansteenkiste, J.; Escriu, C.; Peters, S. Early and Locally Advanced Non-Small-Cell Lung Cancer (NSCLC): ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Yadav, K.S.; Upadhya, A.; Misra, A. Targeted Drug Therapy in Nonsmall Cell Lung Cancer: Clinical Significance and Possible Solutions-Part II (Role of Nanocarriers). Expert Opin. Drug Deliv. 2021, 18, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Nurgali, K.; Jagoe, R.T.; Abalo, R. Editorial: Adverse Effects of Cancer Chemotherapy: Anything New to Improve Tolerance and Reduce Sequelae? Front. Pharmacol. 2018, 9, 245. [Google Scholar] [CrossRef] [Green Version]
- Gonciar, D.; Mocan, T.; Matea, C.T.; Zdrehus, C.; Mosteanu, O.; Mocan, L.; Pop, T. Nanotechnology in Metastatic Cancer Treatment: Current Achievements and Future Research Trends. J. Cancer 2019, 10, 1358–1369. [Google Scholar] [CrossRef]
- Loira-Pastoriza, C.; Todoroff, J.; Vanbever, R. Delivery Strategies for Sustained Drug Release in the Lungs. Adv. Drug Deliv. Rev. 2014, 75, 81–91. [Google Scholar] [CrossRef]
- Patton, J.S.; Byron, P.R. Inhaling Medicines: Delivering Drugs to the Body through the Lungs. Nat. Rev. Drug Discov. 2007, 6, 67–74. [Google Scholar] [CrossRef]
- Lee, W.H.; Loo, C.Y.; Traini, D.; Young, P.M. Nano- and Micro-Based Inhaled Drug Delivery Systems for Targeting Alveolar Macrophages. Expert Opin. Drug Deliv. 2015, 12, 1009–1026. [Google Scholar] [CrossRef]
- Gagnadoux, F.; Hureaux, J.; Vecellio, L.; Urban, T.; Le Pape, A.; Valo, I.; Montharu, J.; Leblond, V.; Boisdron-Celle, M.; Lerondel, S.; et al. Aerosolized Chemotherapy. J. Aerosol Med. Pulm. Drug Deliv. 2008, 21, 61–70. [Google Scholar] [CrossRef]
- Mangal, S.; Gao, W.; Li, T.; Zhou, Q.T. Pulmonary Delivery of Nanoparticle Chemotherapy for the Treatment of Lung Cancers: Challenges and Opportunities. Acta Pharmacol. Sin. 2017, 38, 782–797. [Google Scholar] [CrossRef]
- Gill, S.; Löbenberg, R.; Ku, T.; Azarmi, S.; Roa, W.; Prenner, E.J. Nanoparticles: Characteristics, Mechanisms of Action, and Toxicity in Pulmonary Drug Delivery—A Review. J. Biomed. Nanotechnol. 2007, 3, 107–119. [Google Scholar] [CrossRef]
- Was, H.; Borkowska, A.; Bagues, A.; Tu, L.; Liu, J.Y.H.; Lu, Z.; Rudd, J.A.; Nurgali, K.; Abalo, R. Mechanisms of Chemotherapy-Induced Neurotoxicity. Front. Pharmacol. 2022, 13, 750507. [Google Scholar] [CrossRef]
- Rapoport, B.L. Delayed Chemotherapy-Induced Nausea and Vomiting: Pathogenesis, Incidence, and Current Management. Front. Pharmacol. 2017, 8, 19. [Google Scholar] [CrossRef]
- Rosière, R.; Amighi, K.; Wauthoz, N. Nanomedicine-Based Inhalation Treatments for Lung Cancer. In Nanotechnology-Based Targeted Drug Delivery Systems for Lung Cancer; Academic Press: Cambrigde, MA, USA, 2019; pp. 249–268. [Google Scholar]
- Todoroff, J.; Vanbever, R. Fate of Nanomedicines in the Lungs. Curr. Opin. Colloid Interface Sci. 2011, 16, 246–254. [Google Scholar] [CrossRef]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Hasanzadeh Davarani, F.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M.R. Impact of Particle Size and Polydispersity Index on the Clinical Applications of Lipidic Nanocarrier Systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef] [Green Version]
- Shen, Y.B.; Du, Z.; Tang, C.; Guan, Y.X.; Yao, S.J. Formulation of Insulin-Loaded N-Trimethyl Chitosan Microparticles with Improved Efficacy for Inhalation by Supercritical Fluid Assisted Atomization. Int. J. Pharm. 2016, 505, 223–233. [Google Scholar] [CrossRef]
- Zanen, P.; Go, L.T.; Lammers, J.W.J. The Optimal Particle Size for β-Adrenergic Aerosols in Mild Asthmatics. Int. J. Pharm. 1994, 107, 211–217. [Google Scholar] [CrossRef]
- Wauthoz, N.; Amighi, K. Phospholipids in Pulmonary Drug Delivery. Eur. J. Lipid Sci. Technol. 2014, 116, 1114–1128. [Google Scholar] [CrossRef]
- Champion, J.A.; Mitragotri, S. Shape Induced Inhibition of Phagocytosis of Polymer Particles. Pharm. Res. 2009, 26, 244–249. [Google Scholar] [CrossRef]
- Depreter, F.; Pilcer, G.; Amighi, K. Inhaled Proteins: Challenges and Perspectives. Int. J. Pharm. 2013, 447, 251–280. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.H.; Loo, C.Y.; Young, P.M.; Traini, D.; Mason, R.S.; Rohanizadeh, R. Recent Advances in Curcumin Nanoformulation for Cancer Therapy. Expert Opin. Drug Deliv. 2014, 11, 1183–1201. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.E.; Chen, Z.; Shin, D.M. Nanoparticle Therapeutics: An Emerging Treatment Modality for Cancer. Nat. Rev. Drug Discov. 2008, 7, 771–782. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Ashitate, Y.; Lee, J.H.; Kim, S.H.; Matsui, A.; Insin, N.; Bawendi, M.G.; Semmler-Behnke, M.; Frangioni, J.V.; Tsuda, A. Rapid Translocation of Nanoparticles from the Lung Airspaces to the Body. Nat. Biotechnol. 2010, 28, 1300–1303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, M.; Jha, A.; Bharti, K.; Parmar, G.; Mishra, B. Advances in Lipid-Based Pulmonary Nanomedicine for the Management of Inflammatory Lung Disorders. Nanomedicine 2022, 17, 913–934. [Google Scholar] [CrossRef]
- Carvalho, T.C.; Carvalho, S.R.; McConville, J.T. Formulations for Pulmonary Administration of Anticancer Agents to Treat Lung Malignancies. J. Aerosol Med. Pulm. Drug Deliv. 2011, 24, 61–80. [Google Scholar] [CrossRef]
- Abdelaziz, H.M.; Gaber, M.; Abd-Elwakil, M.M.; Mabrouk, M.T.; Elgohary, M.M.; Kamel, N.M.; Kabary, D.M.; Freag, M.S.; Samaha, M.W.; Mortada, S.M.; et al. Inhalable Particulate Drug Delivery Systems for Lung Cancer Therapy: Nanoparticles, Microparticles, Nanocomposites and Nanoaggregates. J. Control. Release 2018, 269, 374–392. [Google Scholar] [CrossRef]
- Kuzmov, A.; Minko, T. Nanotechnology Approaches for Inhalation Treatment of Lung Diseases. J. Control. Release 2015, 219, 500–518. [Google Scholar] [CrossRef] [Green Version]
- Lai, S.K.; Wang, Y.Y.; Hanes, J. Mucus-Penetrating Nanoparticles for Drug and Gene Delivery to Mucosal Tissues. Adv. Drug Deliv. Rev. 2009, 61, 158–171. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Parvathaneni, V.; Shukla, S.K.; Kulkarni, N.S.; Muth, A.; Kunda, N.K.; Gupta, V. Inhalable Resveratrol-Cyclodextrin Complex Loaded Biodegradable Nanoparticles for Enhanced Efficacy against Non-Small Cell Lung Cancer. Int. J. Biol. Macromol. 2020, 164, 638–650. [Google Scholar] [CrossRef]
- Shukla, S.K.; Kulkarni, N.S.; Farrales, P.; Kanabar, D.D.; Parvathaneni, V.; Kunda, N.K.; Muth, A.; Gupta, V. Sorafenib Loaded Inhalable Polymeric Nanocarriers against Non-Small Cell Lung Cancer. Pharm. Res. 2020, 37, 1–19. [Google Scholar]
- Ak, G. Covalently Coupling Doxorubicin to Polymeric Nanoparticles as Potential Inhaler Therapy: In Vitro Studies. Pharm. Dev. Technol. 2021, 26, 890–898. [Google Scholar] [CrossRef]
- Parvathaneni, V.; Kulkarni, N.S.; Chauhan, G.; Shukla, S.K.; Elbatanony, R.; Patel, B.K.; Kunda, N.K.; Muth, A.; Gupta, V. Development of Pharmaceutically Scalable Inhaled Anti-Cancer Nanotherapy—Repurposing Amodiaquine for Non-Small Cell Lung Cancer (NSCLC). Mater. Sci. Eng. C 2020, 115, 111139. [Google Scholar] [CrossRef]
- Vaidya, B.; Kulkarni, N.S.; Shukla, S.K.; Parvathaneni, V.; Chauhan, G.; Damon, J.K.; Sarode, A.; Garcia, J.V.; Kunda, N.; Mitragotri, S.; et al. Development of Inhalable Quinacrine Loaded Bovine Serum Albumin Modified Cationic Nanoparticles: Repurposing Quinacrine for Lung Cancer Therapeutics. Int. J. Pharm. 2020, 577, 118995. [Google Scholar] [CrossRef]
- Gombotz, W.R.; Wee, S.F. Protein Release from Alginate Matrices. Adv. Drug Deliv. Rev. 1998, 31, 267–285. [Google Scholar] [CrossRef]
- Lemoine, D.; Wauters, F.; Bouchend’Homme, S.; Préat, V. Preparation and Characterization of Alginate Microspheres Containing a Model Antigen. Int. J. Pharm. 1998, 176, 9–19. [Google Scholar] [CrossRef]
- Chan, L.W.; Lee, H.Y.; Heng, P.W.S. Production of Alginate Microspheres by Internal Gelation Using an Emulsification Method. Int. J. Pharm. 2002, 242, 259–262. [Google Scholar] [CrossRef]
- Al-Kassas, R.S.; Al-Gohary, O.M.N.; Al-Faadhel, M.M. Controlling of Systemic Absorption of Gliclazide through Incorporation into Alginate Beads. Int. J. Pharm. 2007, 341, 230–237. [Google Scholar] [CrossRef]
- Rastogi, R.; Sultana, Y.; Aqil, M.; Ali, A.; Kumar, S.; Chuttani, K.; Mishra, A.K. Alginate Microspheres of Isoniazid for Oral Sustained Drug Delivery. Int. J. Pharm. 2007, 334, 71–77. [Google Scholar] [CrossRef]
- Chandy, T.; Sharma’, C.P. Chitosan—As a Biomaterial. Biomater. Artif. Cells Artif. Organs 1990, 18, 1–24. [Google Scholar] [CrossRef]
- Alipour, S.; Montaseri, H.; Tafaghodi, M. Preparation and Characterization of Biodegradable Paclitaxel Loaded Alginate Microparticles for Pulmonary Delivery. Colloids Surf. B Biointerfaces 2010, 81, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Shukla, S.K.; Mishra, A.K.; Arotiba, O.A.; Mamba, B.B. Chitosan-Based Nanomaterials: A State-of-the-Art Review. Int. J. Biol. Macromol. 2013, 59, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.J.; Lohade, A.A.; Parmar, J.J.; Hegde, D.D.; Soni, P.; Samad, A.; Menon, M.D. Development of Chitosan-Based Dry Powder Inhalation System of Cisplatin for Lung Cancer. Indian J. Pharm. Sci. 2012, 74, 521–526. [Google Scholar] [PubMed] [Green Version]
- Rosière, R.; Van Woensel, M.; Gelbcke, M.; Mathieu, V.; Hecq, J.; Mathivet, T.; Vermeersch, M.; Van Antwerpen, P.; Amighi, K.; Wauthoz, N. New Folate-Grafted Chitosan Derivative to Improve Delivery of Paclitaxel-Loaded Solid Lipid Nanoparticles for Lung Tumor Therapy by Inhalation. Mol. Pharm. 2018, 15, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Citkowska, A.; Szekalska, M.; Winnicka, K. Possibilities of Fucoidan Utilization in the Development of Pharmaceutical Dosage Forms. Mar. Drugs 2019, 17, 458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, N.; Zhang, Q.; Song, J. Toxicological Evaluation of Fucoidan Extracted from Laminaria Japonica in Wistar Rats. Food Chem. Toxicol. 2005, 43, 421–426. [Google Scholar] [CrossRef]
- Hsu, H.Y.; Lin, T.Y.; Wu, Y.C.; Tsao, S.M.; Hwang, P.A.; Shih, Y.W.; Hsu, J. Fucoidan Inhibition of Lung Cancer in Vivo and in Vitro: Role of the Smurf2-Dependent Ubiquitin Proteasome Pathway in TGFβ Receptor Degradation. Oncotarget 2014, 5, 7870–7885. [Google Scholar] [CrossRef] [Green Version]
- Bonacucina, G.; Cespi, M.; Misici-Falzi, M.; Palmieri, G.F. Colloidal Soft Matter as Drug Delivery System. J. Pharm. Sci. 2009, 98, 1–42. [Google Scholar] [CrossRef]
- Kaminskas, L.M.; McLeod, V.M.; Ryan, G.M.; Kelly, B.D.; Haynes, J.M.; Williamson, M.; Thienthong, N.; Owen, D.J.; Porter, C.J.H. Pulmonary Administration of a Doxorubicin-Conjugated Dendrimer Enhances Drug Exposure to Lung Metastases and Improves Cancer Therapy. J. Control. Release 2014, 183, 18–26. [Google Scholar] [CrossRef]
- Bai, S.; Ahsan, F. Synthesis and Evaluation of Pegylated Dendrimeric Nanocarrier for Pulmonary Delivery of Low Molecular Weight Heparin. Pharm. Res. 2009, 26, 539–548. [Google Scholar] [CrossRef]
- Mignani, S.; El Kazzouli, S.; Bousmina, M.; Majoral, J.P. Expand Classical Drug Administration Ways by Emerging Routes Using Dendrimer Drug Delivery Systems: A Concise Overview. Adv. Drug Deliv. Rev. 2013, 65, 1316–1330. [Google Scholar] [CrossRef]
- Kumar, R. Lipid-Based Nanoparticles for Drug-Delivery Systems. In Nanocarriers for Drug Delivery: Nanoscience and Nanotechnology in Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2018; pp. 249–284. ISBN 9780128140345. [Google Scholar]
- Narvekar, M.; Xue, H.Y.; Eoh, J.Y.; Wong, H.L. Nanocarrier for Poorly Water-Soluble Anticancer Drugs—Barriers of Translation and Solutions. AAPS PharmSciTech 2014, 15, 822–833. [Google Scholar] [CrossRef]
- Salvi, V.R.; Pawar, P. Nanostructured Lipid Carriers (NLC) System: A Novel Drug Targeting Carrier. J. Drug Deliv. Sci. Technol. 2019, 51, 255–267. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, Preparation, and Applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef] [Green Version]
- Rahimpour, Y.; Hamishehkar, H. Liposomes in Cosmeceutics. Expert Opin. Drug Deliv. 2012, 9, 443–455. [Google Scholar] [CrossRef]
- Talluri, S.V.; Kuppusamy, G.; Karri, V.V.S.R.; Tummala, S.; Madhunapantula, S.R.V. Lipid-Based Nanocarriers for Breast Cancer Treatment—Comprehensive Review. Drug Deliv. 2016, 23, 1291–1305. [Google Scholar] [CrossRef]
- Daraee, H.; Etemadi, A.; Kouhi, M.; Alimirzalu, S.; Akbarzadeh, A. Application of Liposomes in Medicine and Drug Delivery. Artif. Cells Nanomed. Biotechnol. 2016, 44, 381–391. [Google Scholar] [CrossRef]
- Minko, T.; Khandare, J.J.; Vetcher, A.A.; Soldatenkov, V.A.; Garbuzenko, O.B.; Saad, M.; Pozharov, V.P. Multifunctional Nanotherapeutics for Cancer; Springer: New York, NY, USA, 2008; pp. 309–336. [Google Scholar]
- Din, F.U.; Aman, W.; Ullah, I.; Qureshi, O.S.; Mustapha, O.; Shafique, S.; Zeb, A. Effective Use of Nanocarriers as Drug Delivery Systems for the Treatment of Selected Tumors. Int. J. Nanomed. 2017, 12, 7291–7309. [Google Scholar] [CrossRef] [Green Version]
- Gaber, M.; Medhat, W.; Hany, M.; Saher, N.; Fang, J.Y.; Elzoghby, A. Protein-Lipid Nanohybrids as Emerging Platforms for Drug and Gene Delivery: Challenges and Outcomes. J. Control. Release 2017, 254, 75–91. [Google Scholar] [CrossRef]
- Misra, A.; Jinturkar, K.; Patel, D.; Lalani, J.; Chougule, M. Recent Advances in Liposomal Dry Powder Formulations: Preparation and Evaluation. Expert Opin. Drug Deliv. 2009, 6, 71–89. [Google Scholar] [CrossRef]
- Tang, Y.; Zhang, H.; Lu, X.; Jiang, L.; Xi, X.; Liu, J.; Zhu, J. Development and Evaluation of a Dry Powder Formulation of Liposome-Encapsulated Oseltamivir Phosphate for Inhalation. Drug Deliv. 2015, 22, 608–618. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, A.; McElvaney, N.G.; Cryan, S.A. A Dry Powder Formulation of Liposome-Encapsulated Recombinant Secretory Leukocyte Protease Inhibitor (RSLPI) for Inhalation: Preparation and Characterisation. AAPS PharmSciTech 2010, 11, 1411–1421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, T.; Chen, Y.; Ge, Y.; Hu, Y.; Li, M.; Jin, Y. Inhalation Treatment of Primary Lung Cancer Using Liposomal Curcumin Dry Powder Inhalers. Acta Pharm. Sin. B 2018, 8, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Parvathaneni, V.; Kulkarni, N.S.; Shukla, S.K.; Farrales, P.T.; Kunda, N.K.; Muth, A.; Gupta, V. Systematic Development and Optimization of Inhalable Pirfenidone Liposomes for Non-Small Cell Lung Cancer Treatment. Pharmaceutics 2020, 12, 206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghosh, S.; Lalani, R.; Maiti, K.; Banerjee, S.; Bhatt, H.; Bobde, Y.S.; Patel, V.; Biswas, S.; Bhowmick, S.; Misra, A. Synergistic Co-Loading of Vincristine Improved Chemotherapeutic Potential of Pegylated Liposomal Doxorubicin against Triple Negative Breast Cancer and Non-Small Cell Lung Cancer. Nanomed. Nanotechnol. Biol. Med. 2021, 31, 102320. [Google Scholar] [CrossRef]
- Koshkina, N.V.; Waldrep, J.C.; Roberts, L.E.; Golunski, E.; Melton, S.; Knight, V. Paclitaxel Liposome Aerosol Treatment Induces Inhibition of Pulmonary Metastases in Murine Renal Carcinoma Model. Clin. Cancer Res. 2001, 7, 3258–3262. [Google Scholar]
- Xiao, Z.; Zhuang, B.; Zhang, G.; Li, M.; Jin, Y. Pulmonary Delivery of Cationic Liposomal Hydroxycamptothecin and 5-Aminolevulinic Acid for Chemo-Sonodynamic Therapy of Metastatic Lung Cancer. Int. J. Pharm. 2021, 601, 120572. [Google Scholar] [CrossRef]
- Hitzman, C.J.; Elmquist, W.F.; Wattenberg, L.W.; Wiedmann, T.S. Development of a Respirable, Sustained Release Microcarrier for 5-Fluorouracil I: In Vitro Assessment of Liposomes, Microspheres, and Lipid Coated Nanoparticles. J. Pharm. Sci. 2006, 95, 1114–1126. [Google Scholar] [CrossRef]
- Robins, M.M.; Watson, A.D.; Wilde, P.J. Emulsions—Creaming and Rheology. Curr. Opin. Colloid Interface Sci. 2002, 7, 419–425. [Google Scholar] [CrossRef]
- Maphosa, Y.; Jideani, V.A. Factors Affecting the Stability of Emulsions Stabilised by Biopolymers. In Science and Technology Behind Nanoemulsions; IntechOpen: Rjeka, Croatia, 2018; ISBN 978-1-78923-571-5. [Google Scholar]
- Gorain, B.; Choudhury, H.; Kundu, A.; Sarkar, L.; Karmakar, S.; Jaisankar, P.; Pal, T.K. Nanoemulsion Strategy for Olmesartan Medoxomil Improves Oral Absorption and Extended Antihypertensive Activity in Hypertensive Rats. Colloids Surf. B Biointerfaces 2014, 115, 286–294. [Google Scholar] [CrossRef]
- Gorain, B.; Choudhury, H.; Biswas, E.; Barik, A.; Jaisankar, P.; Pal, T.K. A Novel Approach for Nanoemulsion Components Screening and Nanoemulsion Assay of Olmesartan Medoxomil through a Developed and Validated HPLC Method. RSC Adv. 2013, 3, 10887–10893. [Google Scholar] [CrossRef]
- Ngan, C.L.; Asmawi, A.A. Lipid-Based Pulmonary Delivery System: A Review and Future Considerations of Formulation Strategies and Limitations. Drug Deliv. Transl. Res. 2018, 8, 1527–1544. [Google Scholar] [CrossRef]
- Pavoni, L.; Perinelli, D.R.; Bonacucina, G.; Cespi, M.; Palmieri, G.F. An Overview of Micro-and Nanoemulsions as Vehicles for Essential Oils: Formulation, Preparation and Stability. Nanomaterials 2020, 10, 135. [Google Scholar] [CrossRef] [Green Version]
- Lovelyn, C.; Attama, A.A. Current State of Nanoemulsions in Drug Delivery. J. Biomater. Nanobiotechnol. 2011, 2, 626–639. [Google Scholar] [CrossRef] [Green Version]
- Salcido, A. Equilibrium Properties of the Cellular Automata Models for Traffic Flow in a Single Lane. In Cellular Automata—Simplicity Behind Complexity; IntechOpen: Rjeka, Croatia, 2011. [Google Scholar]
- Choudhury, H.; Pandey, M.; Gorain, B.; Chatterjee, B.; Madheswaran, T.; Md, S.; Mak, K.-K.; Tambuwala, M.; Chourasia, M.K.; Kesharwani, P. Nanoemulsions as Effective Carriers for the Treatment of Lung Cancer. In Nanotechnology-Based Targeted Drug Delivery Systems for Lung Cancer; Elsevier: Amsterdam, The Netherlands, 2019; pp. 217–247. [Google Scholar]
- Kamali, H.; Abbasi, S.; Amini, M.A.; Amani, A. Investigation of Factors Affecting Aerodynamic Performance of Nebulized Nanoemulsion. Iran. J. Pharm. Res. IJPR 2016, 15, 687–693. [Google Scholar]
- Amani, A.; York, P.; Chrystyn, H.; Clark, B.J. Evaluation of a Nanoemulsion-Based Formulation for Respiratory Delivery of Budesonide by Nebulizers. AAPS PharmSciTech 2010, 11, 1147–1151. [Google Scholar] [CrossRef] [Green Version]
- Qi, K.; Al-Haideri, M.; Seo, T.; Carpentier, Y.A.; Deckelbaum, R.J. Effects of Particle Size on Blood Clearance and Tissue Uptake of Lipid Emulsions with Different Triglyceride Compositions. J. Parenter. Enter. Nutr. 2003, 27, 58–64. [Google Scholar] [CrossRef]
- Davis, W.W.; Pfeiffer, R.R.; Quay, J.F. Normal and Promoted Gastrointestinal Absorption of Water-soluble Substances I: Induced Rapidly Reversible Hyperabsorptive State in the Canine Fundic Stomach Pouch. J. Pharm. Sci. 1970, 59, 960–963. [Google Scholar] [CrossRef]
- Kaur, P.; Garg, T.; Rath, G.; Murthy, R.S.R.; Goyal, A.K. Surfactant-Based Drug Delivery Systems for Treating Drug-Resistant Lung Cancer. Drug Deliv. 2016, 23, 727–738. [Google Scholar] [CrossRef]
- Dammak, I.; do Amaral Sobral, P.J.; Aquino, A.; das Neves, M.A.; Conte-Junior, C.A. Nanoemulsions: Using Emulsifiers from Natural Sources Replacing Synthetic Ones—A Review. Compr. Rev. Food Sci. Food Saf. 2020, 19, 2721–2746. [Google Scholar] [CrossRef]
- Said-Elbahr, R.; Nasr, M.; Alhnan, M.A.; Taha, I.; Sammour, O. Simultaneous Pulmonary Administration of Celecoxib and Naringin Using a Nebulization-Friendly Nanoemulsion: A Device-Targeted Delivery for Treatment of Lung Cancer. Expert Opin. Drug Deliv. 2022, 19, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Asmawi, A.A.; Salim, N.; Ngan, C.L.; Ahmad, H.; Abdulmalek, E.; Masarudin, M.J.; Abdul Rahman, M.B. Excipient Selection and Aerodynamic Characterization of Nebulized Lipid-Based Nanoemulsion Loaded with Docetaxel for Lung Cancer Treatment. Drug Deliv. Transl. Res. 2019, 9, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Jardim, K.V.; Siqueira, J.L.N.; Báo, S.N.; Sousa, M.H.; Parize, A.L. The Role of the Lecithin Addition in the Properties and Cytotoxic Activity of Chitosan and Chondroitin Sulfate Nanoparticles Containing Curcumin. Carbohydr. Polym. 2020, 227, 115351. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, W.; Mäder, K. Solid Lipid Nanoparticles: Production, Characterization and Applications. Adv. Drug Deliv. Rev. 2001, 47, 165–196. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.; Sarmento, B.; Ferreira, D.C.; Souto, E.B. Lipid-Based Colloidal Carriers for Peptide and Protein Delivery—Liposomes versus Lipid Nanoparticles. Int. J. Nanomed. 2007, 2, 595–607. [Google Scholar]
- Subedi, R.K.; Kang, K.W.; Choi, H.K. Preparation and Characterization of Solid Lipid Nanoparticles Loaded with Doxorubicin. Eur. J. Pharm. Sci. 2009, 37, 508–513. [Google Scholar] [CrossRef]
- Haque, S.; Whittaker, M.; McIntosh, M.P.; Pouton, C.W.; Phipps, S.; Kaminskas, L.M. A Comparison of the Lung Clearance Kinetics of Solid Lipid Nanoparticles and Liposomes by Following the 3H-Labelled Structural Lipids after Pulmonary Delivery in Rats. Eur. J. Pharm. Biopharm. 2018, 125, 1–12. [Google Scholar] [CrossRef]
- Huang, Z.; Huang, Y.; Wang, W.; Fu, F.; Wang, W.; Dang, S.; Li, C.; Ma, C.; Zhang, X.; Zhao, Z.; et al. Relationship between Particle Size and Lung Retention Time of Intact Solid Lipid Nanoparticle Suspensions after Pulmonary Delivery. J. Control. Release 2020, 325, 206–222. [Google Scholar] [CrossRef]
- Nassimi, M.; Schleh, C.; Lauenstein, H.D.; Hussein, R.; Hoymann, H.G.; Koch, W.; Pohlmann, G.; Krug, N.; Sewald, K.; Rittinghausen, S.; et al. A Toxicological Evaluation of Inhaled Solid Lipid Nanoparticles Used as a Potential Drug Delivery System for the Lung. Eur. J. Pharm. Biopharm. 2010, 75, 107–116. [Google Scholar] [CrossRef]
- Hu, L.; Jia, Y. WenDing Preparation and Characterization of Solid Lipid Nanoparticles Loaded with Epirubicin for Pulmonary Delivery. Pharmazie 2010, 65, 585–587. [Google Scholar]
- Pi, C.; Zhao, W.; Zeng, M.; Yuan, J.; Shen, H.; Li, K.; Su, Z.; Liu, Z.; Wen, J.; Song, X.; et al. Anti-Lung Cancer Effect of Paclitaxel Solid Lipid Nanoparticles Delivery System with Curcumin as Co-Loading Partner in Vitro and in Vivo. Drug Deliv. 2022, 29, 1878–1891. [Google Scholar] [CrossRef]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Nanostructured Lipid Matrices for Improved Microencapsulation of Drugs. Int. J. Pharm. 2002, 242, 121–128. [Google Scholar] [CrossRef]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Solid Lipid Nanoparticles (SLN) and Nanostructured Lipid Carriers (NLC) in Cosmetic and Dermatological Preparations. Adv. Drug Deliv. Rev. 2002, 54, S131–S135. [Google Scholar] [CrossRef]
- Jenning, V.; Mäder, K.; Gohla, S.H. Solid Lipid Nanoparticles (SLN(TM)) Based on Binary Mixtures of Liquid and Solid Lipids: A 1H-NMR Study. Int. J. Pharm. 2000, 205, 15–21. [Google Scholar] [CrossRef]
- Jenning, V.; Thünemann, A.F.; Gohla, S.H. Characterisation of a Novel Solid Lipid Nanoparticle Carrier System Based on Binary Mixtures of Liquid and Solid Lipids. Int. J. Pharm. 2000, 199, 167–177. [Google Scholar] [CrossRef]
- Jaiswal, P.; Gidwani, B.; Vyas, A. Nanostructured Lipid Carriers and Their Current Application in Targeted Drug Delivery. Artif. Cells Nanomed. Biotechnol. 2016, 44, 27–40. [Google Scholar] [CrossRef]
- Garbuzenko, O.B.; Kbah, N.; Kuzmov, A.; Pogrebnyak, N.; Pozharov, V.; Minko, T. Inhalation Treatment of Cystic Fibrosis with Lumacaftor and Ivacaftor Co-Delivered by Nanostructured Lipid Carriers. J. Control. Release 2019, 296, 225–231. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, H.; Hao, J.; Li, B.; Li, M.; Xiuwen, W. Lung Cancer Combination Therapy: Co-Delivery of Paclitaxel and Doxorubicin by Nanostructured Lipid Carriers for Synergistic Effect. Drug Deliv. 2016, 23, 1398–1403. [Google Scholar] [CrossRef]
- Dave, V.; Tak, K.; Sohgaura, A.; Gupta, A.; Sadhu, V.; Reddy, K.R. Lipid-Polymer Hybrid Nanoparticles: Synthesis Strategies and Biomedical Applications. J. Microbiol. Methods 2019, 160, 130–142. [Google Scholar] [CrossRef]
- Hadinoto, K.; Sundaresan, A.; Cheow, W.S. Lipid-Polymer Hybrid Nanoparticles as a New Generation Therapeutic Delivery Platform: A Review. Eur. J. Pharm. Biopharm. 2013, 85, 427–443. [Google Scholar] [CrossRef]
- Yang, Y.; Cheow, W.S.; Hadinoto, K. Dry Powder Inhaler Formulation of Lipid–Polymer Hybrid Nanoparticles via Electrostatically-Driven Nanoparticle Assembly onto Microscale Carrier Particles. Int. J. Pharm. 2012, 434, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Bardoliwala, D.; Patel, V.; Misra, A.; Sawant, K. Systematic Development and Characterization of Inhalable Dry Powder Containing Polymeric Lipid Hybrid Nanocarriers Co-Loaded with ABCB1 ShRNA and Docetaxel Using QbD Approach. J. Drug Deliv. Sci. Technol. 2021, 66, 102903. [Google Scholar] [CrossRef]
- Knight, V.; Kleinerman, E.S.; Waldrep, C.; Giovanella, B.C.; Gilbert, B.E.; Koshkina, N.V. 9-Nitrocamptothecin Liposome Aerosol Treatment of Human Cancer Subcutaneous Xenografts and Pulmonary Cancer Metastases in Mice. In Proceedings of the Annals of the New York Academy of Sciences; New York Academy of Sciences: New York, NY, USA, 2000; Volume 922, pp. 151–163. [Google Scholar]
- Koshkina, N.V.; Waldrep, J.C.; Seryshev, A.; Knight, V.; Gilbert, B.E. Distribution of Camptothecin after Delivery as a Liposome Aerosol or Following Intramuscular Injection in Mice. Cancer Chemother. Pharmacol. 1999, 44, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Li, M.; Du, L.; Zeng, J.; Yao, T.; Jin, Y. Paclitaxel-in-Liposome-in-Bacteria for Inhalation Treatment of Primary Lung Cancer. Int. J. Pharm. 2020, 578, 119177. [Google Scholar] [CrossRef] [PubMed]
- Adel, I.M.; Elmeligy, M.F.; Abdelrahim, M.E.A.; Maged, A.; Abdelkhalek, A.A.; Abdelmoteleb, A.M.M.; Elkasabgy, N.A. Design and Characterization of Spray-Dried Proliposomes for the Pulmonary Delivery of Curcumin. Int. J. Nanomed. 2021, 16, 2667–2687. [Google Scholar] [CrossRef]
- Gaspar, M.M.; Radomska, A.; Gobbo, O.L.; Bakowsky, U.; Radomski, M.W.; Ehrhardt, C. Targeted Delivery of Transferrin-Conjugated Liposomes to an Orthotopic Model of Lung Cancer in Nude Rats. J. Aerosol Med. Pulm. Drug Deliv. 2012, 25, 310–318. [Google Scholar] [CrossRef]
- Xu, J.; Lu, X.; Zhu, X.; Yang, Y.; Liu, Q.; Zhao, D.; Lu, Y.; Wen, J.; Chen, X.; Li, N. Formulation and Characterization of Spray-Dried Powders Containing Vincristine-Liposomes for Pulmonary Delivery and Its Pharmacokinetic Evaluation From In Vitro and In Vivo. J. Pharm. Sci. 2019, 108, 3348–3358. [Google Scholar] [CrossRef]
- Asmawi, A.A.; Salim, N.; Abdulmalek, E.; Rahman, M.B.A. Modeling the Effect of Composition on Formation of Aerosolized Nanoemulsion System Encapsulating Docetaxel and Curcumin Using D-Optimal Mixture Experimental Design. Int. J. Mol. Sci. 2020, 21, 4357. [Google Scholar] [CrossRef]
- Bakhtiary, Z.; Barar, J.; Aghanejad, A.; Saei, A.A.; Nemati, E.; Ezzati Nazhad Dolatabadi, J.; Omidi, Y. Microparticles Containing Erlotinib-Loaded Solid Lipid Nanoparticles for Treatment of Non-Small Cell Lung Cancer. Drug Dev. Ind. Pharm. 2017, 43, 1244–1253. [Google Scholar] [CrossRef]
- Nafee, N.; Gaber, D.M.; Elzoghby, A.O.; Helmy, M.W.; Abdallah, O.Y. Promoted Antitumor Activity of Myricetin against Lung Carcinoma Via Nanoencapsulated Phospholipid Complex in Respirable Microparticles. Pharm. Res. 2020, 37, 82. [Google Scholar] [CrossRef]
- Garbuzenko, O.B.; Kuzmov, A.; Taratula, O.; Pine, S.R.; Minko, T. Strategy to Enhance Lung Cancer Treatment by Five Essential Elements: Inhalation Delivery, Nanotechnology, Tumor-Receptor Targeting, Chemo- and Gene Therapy. Theranostics 2019, 9, 8362–8376. [Google Scholar] [CrossRef]
- Kaur, P.; Garg, T.; Rath, G.; Murthy, R.S.R.; Goyal, A.K. Development, Optimization and Evaluation of Surfactant-Based Pulmonary Nanolipid Carrier System of Paclitaxel for the Management of Drug Resistance Lung Cancer Using Box-Behnken Design. Drug Deliv. 2016, 23, 1912–1925. [Google Scholar] [CrossRef]
- Patel, A.R.; Chougule, M.B.; Townley, I.; Patlolla, R.; Wang, G.; Singh, M. Efficacy of Aerosolized Celecoxib Encapsulated Nanostructured Lipid Carrier in Non-Small Cell Lung Cancer in Combination with Docetaxel. Pharm. Res. 2013, 30, 1435–1446. [Google Scholar] [CrossRef] [Green Version]
- D’Angelo, I.; Costabile, G.; Durantie, E.; Brocca, P.; Rondelli, V.; Russo, A.; Russo, G.; Miro, A.; Quaglia, F.; Petri-Fink, A.; et al. Hybrid Lipid/Polymer Nanoparticles for Pulmonary Delivery of SiRNA: Development and Fate upon in Vitro Deposition on the Human Epithelial Airway Barrier. J. Aerosol Med. Pulm. Drug Deliv. 2018, 31, 170–181. [Google Scholar] [CrossRef] [Green Version]
- Saimi, N.I.M.; Salim, N.; Ahmad, N.; Abdulmalek, E.; Rahman, M.B.A. Aerosolized Niosome Formulation Containing Gemcitabine and Cisplatin for Lung Cancer Treatment: Optimization, Characterization and in Vitro Evaluation. Pharmaceutics 2021, 13, 59. [Google Scholar] [CrossRef]
- Vandervoort, J.; Ludwig, A. Preparation and Evaluation of Drug-Loaded Gelatin Nanoparticles for Topical Ophthalmic Use. Eur. J. Pharm. Biopharm. 2004, 57, 251–261. [Google Scholar] [CrossRef]
- Tseng, C.L.; Wu, S.Y.H.; Wang, W.H.; Peng, C.L.; Lin, F.H.; Lin, C.C.; Young, T.H.; Shieh, M.J. Targeting Efficiency and Biodistribution of Biotinylated-EGF-Conjugated Gelatin Nanoparticles Administered via Aerosol Delivery in Nude Mice with Lung Cancer. Biomaterials 2008, 29, 3014–3022. [Google Scholar] [CrossRef]
- Morimoto, K.; Katsumata, H.; Yabuta, T.; Iwanaga, K.; Kakemi, M.; Tabata, Y.; Ikada, Y. Gelatin Microspheres as a Pulmonary Delivery System: Evaluation of Salmon Calcitonin Absorption. J. Pharm. Pharmacol. 2010, 52, 611–617. [Google Scholar] [CrossRef]
- Deaton, A.T.; Jones, L.T.D.; Dunbar, C.A.; Hickey, A.J.; Williams, D.M. Generation of Gelatin Aerosol Particles from Nebulized Solutions as Model Drug Carrier Systems. Pharm. Dev. Technol. 2002, 7, 147–153. [Google Scholar] [CrossRef]
- Tseng, C.L.; Su, W.Y.; Yen, K.C.; Yang, K.C.; Lin, F.H. The Use of Biotinylated-EGF-Modified Gelatin Nanoparticle Carrier to Enhance Cisplatin Accumulation in Cancerous Lungs via Inhalation. Biomaterials 2009, 30, 3476–3485. [Google Scholar] [CrossRef]
- Upadhyay, D.; Scalia, S.; Vogel, R.; Wheate, N.; Salama, R.O.; Young, P.M.; Traini, D.; Chrzanowski, W. Magnetised Thermo Responsive Lipid Vehicles for Targeted and Controlled Lung Drug Delivery. Pharm. Res. 2012, 29, 2456–2467. [Google Scholar] [CrossRef] [PubMed]
- Pankhurst, Q.A.; Thanh, N.K.T.; Jones, S.K.; Dobson, J. Progress in Applications of Magnetic Nanoparticles in Biomedicine. J. Phys. D Appl. Phys. 2009, 42, 224001. [Google Scholar] [CrossRef] [Green Version]
- Bharti, C.; Gulati, N.; Nagaich, U.; Pal, A. Mesoporous Silica Nanoparticles in Target Drug Delivery System: A Review. Int. J. Pharm. Investig. 2015, 5, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vivero-Escoto, J.L.; Slowing, I.I.; Lin, V.S.Y.; Trewyn, B.G. Mesoporous Silica Nanoparticles for Intracellular Controlled Drug Delivery. Small 2010, 6, 1952–1967. [Google Scholar] [CrossRef] [PubMed]
- Taratula, O.; Garbuzenko, O.B.; Chen, A.M.; Minko, T. Innovative Strategy for Treatment of Lung Cancer: Targeted Nanotechnology-Based Inhalation Co-Delivery of Anticancer Drugs and SiRNA. J. Drug Target. 2011, 19, 900–914. [Google Scholar] [CrossRef]
- Hu, C.; Du, W. Zinc Oxide Nanoparticles (ZnO NPs) Combined with Cisplatin and Gemcitabine Inhibits Tumor Activity of NSCLC Cells. Aging 2020, 12, 25767–25777. [Google Scholar] [CrossRef]
- Ravi, R.; Zeyaullah, M.; Ghosh, S.; Khan Warsi, M.; Baweja, R.; AlShahrani, A.M.; Mishra, A.; Ahmad, R. Use of Gold Nanoparticle-Silibinin Conjugates: A Novel Approach against Lung Cancer Cells. Front. Chem. 2022, 10, 1018759. [Google Scholar] [CrossRef]
- Umamaheswari, A.; Prabu, S.L.; John, S.A.; Puratchikody, A. Green Synthesis of Zinc Oxide Nanoparticles Using Leaf Extracts of Raphanus Sativus Var. Longipinnatus and Evaluation of Their Anticancer Property in A549 Cell Lines. Biotechnol. Rep. 2021, 29, e00595. [Google Scholar] [CrossRef]
- Mateen, S.; Raina, K.; Agarwal, R. Chemopreventive and Anti-Cancer Efficacy of Silibinin against Growth and Progression of Lung Cancer. Nutr. Cancer 2013, 65, 3–11. [Google Scholar] [CrossRef]
- Abenavoli, L.; Izzo, A.A.; Milić, N.; Cicala, C.; Santini, A.; Capasso, R. Milk Thistle (Silybum marianum): A Concise Overview on Its Chemistry, Pharmacological, and Nutraceutical Uses in Liver Diseases. Phyther. Res. 2018, 32, 2202–2213. [Google Scholar] [CrossRef]
- Vera-Nuñez, L.D.C.; Cornejo-Ruiz, J.O.; Arenas-Chávez, C.A.; de Hollanda, L.M.; Alvarez-Risco, A.; Del-Aguila-Arcentales, S.; Davies, N.M.; Yáñez, J.A.; Vera-Gonzales, C. Green Synthesis of a Novel Silver Nanoparticle Conjugated with Thelypteris Glandulosolanosa (Raqui-Raqui): Preliminary Characterization and Anticancer Activity. Processes 2022, 10, 1308. [Google Scholar] [CrossRef]
- He, Y.; Du, Z.; Ma, S.; Liu, Y.; Li, D.; Huang, H.; Jiang, S.; Cheng, S.; Wu, W.; Zhang, K. Effects of green-synthesized silver nanoparticles on lung cancer cells in vitro and grown as xenograft tumors in vivo. Int. J. Nanomed. 2016, 11, 1879–1887. [Google Scholar]
- Reczyńska, K.; Marszałek, M.; Zarzycki, A.; Reczyński, W.; Kornaus, K.; Pamuła, E.; Chrzanowski, W. Superparamagnetic Iron Oxide Nanoparticles Modified with Silica Layers as Potential Agents for Lung Cancer Treatment. Nanomaterials 2020, 10, 1076. [Google Scholar] [CrossRef]
- Sadhukha, T.; Wiedmann, T.S.; Panyam, J. Inhalable Magnetic Nanoparticles for Targeted Hyperthermia in Lung Cancer Therapy. Biomaterials 2013, 34, 5163–5171. [Google Scholar] [CrossRef] [Green Version]
- Torchilin, V.P. Micellar Nanocarriers: Pharmaceutical Perspectives. Pharm. Res. 2007, 24, 1–16. [Google Scholar] [CrossRef]
- Torchilin, V. Lipid-Core Micelles for Targeted Drug Delivery. Curr. Drug Deliv. 2005, 2, 319–327. [Google Scholar] [CrossRef]
- Torchilin, V.P. Targeted Polymeric Micelles for Delivery of Poorly Soluble Drugs. Cell. Mol. Life Sci. 2004, 61, 2549–2559. [Google Scholar] [CrossRef]
- Cabral, H.; Kataoka, K. Progress of Drug-Loaded Polymeric Micelles into Clinical Studies. J. Control. Release 2014, 190, 465–476. [Google Scholar] [CrossRef] [Green Version]
- Rezazadeh, M.; Davatsaz, Z.; Emami, J.; Hasanzadeh, F.; Jahanian-Najafabadi, A. Preparation and Characterization of Spray-Dried Inhalable Powders Containing Polymeric Micelles for Pulmonary Delivery of Paclitaxel in Lung Cancer. J. Pharm. Pharm. Sci. 2018, 21, 200s–214s. [Google Scholar] [CrossRef] [Green Version]
- Xie, F.Y.; Xu, W.H.; Yin, C.; Zhang, G.Q.; Zhong, Y.Q.; Gao, J. Nanomedicine Strategies for Sustained, Controlled, and Targeted Treatment of Cancer Stem Cells of the Digestive System. World J. Gastrointest. Oncol. 2016, 8, 735–744. [Google Scholar] [CrossRef]
- Wieleba, I.; Wojas-Krawczyk, K.; Krawczyk, P. Aptamers in Non-Small Cell Lung Cancer Treatment. Molecules 2020, 25, 3138. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Zhuang, H.; Zhuang, Z.; Lu, Y.; Xia, R.; Gan, L.; Wu, Y. Development of Docetaxel Liposome Surface Modified with CD133 Aptamers for Lung Cancer Targeting. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1864–1871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shigdar, S.; Qiao, L.; Zhou, S.F.; Xiang, D.; Wang, T.; Li, Y.; Lim, L.Y.; Kong, L.; Li, L.; Duan, W. RNA Aptamers Targeting Cancer Stem Cell Marker CD133. Cancer Lett. 2013, 330, 84–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertolini, G.; Roz, L.; Perego, P.; Tortoreto, M.; Fontanella, E.; Gatti, L.; Pratesi, G.; Fabbri, A.; Andriani, F.; Tinelli, S.; et al. Highly Tumorigenic Lung Cancer CD133+ Cells Display Stem-like Features and Are Spared by Cisplatin Treatment. Proc. Natl. Acad. Sci. USA 2009, 106, 16281–16286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, R.; Zhang, Z.; Wang, B.; Chen, G.; Zhang, Y.; Deng, H.; Tang, Z.; Mao, J.; Wang, L. Combination Chemotherapy of Lung Cancer—Co-Delivery of Docetaxel Prodrug and Cisplatin Using Aptamer-Decorated Lipid–Polymer Hybrid Nanoparticles. Drug Des. Devel. Ther. 2020, 14, 2249–2261. [Google Scholar] [CrossRef]
- Goel, A.; Sahni, J.; Ali, J.; Baboota, S. Exploring Targeted Pulmonary Delivery for Treatment of Lung Cancer. Int. J. Pharm. Investig. 2013, 3, 8–14. [Google Scholar] [CrossRef]
- Edwards, D.A.; Hanes, J.; Caponetti, G.; Hrkach, J.; Ben-Jebria, A.; Eskew, M.L.; Mintzes, J.; Deaver, D.; Lotan, N.; Langer, R. Large Porous Particles for Pulmonary Drug Delivery. Science 1997, 276, 1868–1871. [Google Scholar] [CrossRef] [Green Version]
- French, D.L.; Edwards, D.A.; Niven, R.W. The Influence of Formulation on Emission, Deaggregation and Deposition of Dry Powders for Inhalation. J. Aerosol Sci. 1996, 27, 769–783. [Google Scholar] [CrossRef]
- Vanbever, R.; Mintzes, J.D.; Wang, J.; Nice, J.; Chen, D.; Batycky, R.; Langer, R.; Edwards, D.A. Formulation and Physical Characterization of Large Porous Particles for Inhalation. Pharm. Res. 1999, 16, 1735–1742. [Google Scholar] [CrossRef]
- Ben-Jebria, A.; Chen, D.; Eskew, M.L.; Vanbever, R.; Langer, R.; Edwards, D.A. Large Porous Particles for Sustained Protection from Carbachol-Induced Bronchoconstriction in Guinea Pigs. Pharm. Res. 1999, 16, 555–561. [Google Scholar] [CrossRef]
- Mezzena, M.; Scalia, S.; Young, P.M.; Traini, D. Solid Lipid Budesonide Microparticles for Controlled Release Inhalation Therapy. AAPS J. 2009, 11, 771–778. [Google Scholar] [CrossRef] [Green Version]
- Möbus, K.; Siepmann, J.; Bodmeier, R. Zinc-Alginate Microparticles for Controlled Pulmonary Delivery of Proteins Prepared by Spray-Drying. Eur. J. Pharm. Biopharm. 2012, 81, 121–130. [Google Scholar] [CrossRef]
- Scalia, S.; Haghi, M.; Losi, V.; Trotta, V.; Young, P.M.; Traini, D. Quercetin Solid Lipid Microparticles: A Flavonoid for Inhalation Lung Delivery. Eur. J. Pharm. Sci. 2013, 49, 278–285. [Google Scholar] [CrossRef]
- Tawfeek, H.; Khidr, S.; Samy, E.; Ahmed, S.; Murphy, M.; Mohammed, A.; Shabir, A.; Hutcheon, G.; Saleem, I. Poly(Glycerol Adipate-Co-Ω-Pentadecalactone) Spray-Dried Microparticles as Sustained Release Carriers for Pulmonary Delivery. Pharm. Res. 2011, 28, 2086–2097. [Google Scholar] [CrossRef] [Green Version]
- Jaspart, S.; Bertholet, P.; Piel, G.; Dogné, J.M.; Delattre, L.; Evrard, B. Solid Lipid Microparticles as a Sustained Release System for Pulmonary Drug Delivery. Eur. J. Pharm. Biopharm. 2007, 65, 47–56. [Google Scholar] [CrossRef]
- El-Sherbiny, I.M.; McGill, S.; Smyth, H.D.C. Swellable Microparticles as Carriers for Sustained Pulmonary Drug Delivery. J. Pharm. Sci. 2010, 99, 2343–2356. [Google Scholar] [CrossRef]
- Shepard, K.B.; Vodak, D.T.; Kuehl, P.J.; Revelli, D.; Zhou, Y.; Pluntze, A.M.; Adam, M.S.; Oddo, J.C.; Switala, L.; Cape, J.L.; et al. Local Treatment of Non-Small Cell Lung Cancer with a Spray-Dried Bevacizumab Formulation. AAPS PharmSciTech 2021, 22, 230. [Google Scholar] [CrossRef]
- Haslam, S.; Chrisp, P. Bevacizumab: The Evidence for Its Clinical Potential in the Treatment of Nonsmall Cell Lung Cancer. Core Evid. 2007, 2, 31–49. [Google Scholar]
- Al-Hallak, M.K.; Sarfraz, M.K.; Azarmi, S.; Roa, W.H.; Finlay, W.H.; Löbenberg, R. Pulmonary Delivery of Inhalable Nanoparticles: Dry Powder Inhalers. Ther. Deliv. 2011, 2, 1313–1324. [Google Scholar] [CrossRef]
- Tomoda, K.; Ohkoshi, T.; Kawai, Y.; Nishiwaki, M.; Nakajima, T.; Makino, K. Preparation and Properties of Inhalable Nanocomposite Particles: Effects of the Temperature at a Spray-Dryer Inlet upon the Properties of Particles. Colloids Surf. B Biointerfaces 2008, 61, 138–144. [Google Scholar] [CrossRef]
- Ali, M.E.; Lamprecht, A. Spray Freeze Drying for Dry Powder Inhalation of Nanoparticles. Eur. J. Pharm. Biopharm. 2014, 87, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, J.; Akhter, S.; Rizwanullah, M.; Amin, S.; Rahman, M.; Ahmad, M.Z.; Rizvi, M.A.; Kamal, M.A.; Ahmad, F.J. Nanotechnology-Based Inhalation Treatments for Lung Cancer: State of the Art. Nanotechnol. Sci. Appl. 2015, 8, 55–66. [Google Scholar] [PubMed] [Green Version]
- Moghimi, S.M.; Hunter, A.C.; Murray, J.C. Nanomedicine: Current Status and Future Prospects. FASEB J. 2005, 19, 311–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bermudez, E.; Mangum, J.B.; Wong, B.A.; Asgharian, B.; Hext, P.M.; Warheit, D.B.; Everitt, J.I. Pulmonary Responses of Mice, Rats, and Hamsters to Subchronic Inhalation of Ultrafine Titanium Dioxide Particles. Toxicol. Sci. 2004, 77, 347–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elder, A.; Gelein, R.; Finkelstein, J.N.; Driscoll, K.E.; Harkema, J.; Oberdörster, G. Effects of Subchronically Inhaled Carbon Black in Three Species. I. Retention Kinetics, Lung Inflammation, and Histopathology. Toxicol. Sci. 2005, 88, 614–629. [Google Scholar] [CrossRef] [Green Version]
- Warheit, D.B.; Webb, T.R.; Reed, K.L. Pulmonary Toxicity Screening Studies in Male Rats with TiO2 Particulates Substantially Encapsulated with Pyrogenically Deposited, Amorphous Silica. Part. Fibre Toxicol. 2006, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Q.T.; Tang, P.; Leung, S.S.Y.; Chan, J.G.Y.; Chan, H.K. Emerging Inhalation Aerosol Devices and Strategies: Where Are We Headed? Adv. Drug Deliv. Rev. 2014, 75, 3–17. [Google Scholar] [CrossRef]
- Zhong, Q.; Da Rocha, S.R.P. Poly(Amidoamine) Dendrimer-Doxorubicin Conjugates: In Vitro Characteristics and Pseudosolution Formulation in Pressurized Metered-Dose Inhalers. Mol. Pharm. 2016, 13, 1058–1072. [Google Scholar] [CrossRef]
- Garrastazu Pereira, G.; Lawson, A.J.; Buttini, F.; Sonvico, F. Loco-Regional Administration of Nanomedicines for the Treatment of Lung Cancer. Drug Deliv. 2016, 23, 2881–2896. [Google Scholar] [CrossRef]
- Zarogoulidis, P.; Chatzaki, E.; Porpodis, K.; Domvri, K.; Hohenforst-Schmidt, W.; Goldberg, E.P.; Karamanos, N.; Zarogoulidis, K. Inhaled Chemotherapy in Lung Cancer: Future Concept of Nanomedicine. Int. J. Nanomed. 2012, 7, 1551–1572. [Google Scholar] [CrossRef] [Green Version]
- Longest, W.; Spence, B.; Hindle, M. Devices for Improved Delivery of Nebulized Pharmaceutical Aerosols to the Lungs. J. Aerosol Med. Pulm. Drug Deliv. 2019, 32, 317–339. [Google Scholar] [CrossRef]
- Wittgen, B.P.H.; Kunst, P.W.A.; Van Der Born, K.; Van Wijk, A.W.; Perkins, W.; Pilkiewicz, F.G.; Perez-Soler, R.; Nicholson, S.; Peters, G.J.; Postmus, P.E. Phase I Study of Aerosolized SLIT Cisplatin in the Treatment of Patients with Carcinoma of the Lung. Clin. Cancer Res. 2007, 13, 2414–2421. [Google Scholar] [CrossRef] [Green Version]
- Labiris, N.R.; Dolovich, M.B. Pulmonary Drug Delivery. Part I: Physiological Factors Affecting Therapeutic Effectiveness of Aerosolized Medications. Br. J. Clin. Pharmacol. 2003, 56, 588–599. [Google Scholar] [CrossRef]
- Lemarie, E.; Vecellio, L.; Hureaux, J.; Prunier, C.; Valat, C.; Grimbert, D.; Boidron-Celle, M.; Giraudeau, B.; Le Pape, A.; Pichon, E.; et al. Aerosolized Gemcitabine in Patients with Carcinoma of the Lung: Feasibility and Safety Study. J. Aerosol Med. Pulm. Drug Deliv. 2011, 24, 261–270. [Google Scholar] [CrossRef]
- Hureaux, J.; Lagarce, F.; Gagnadoux, F.; Vecellio, L.; Clavreul, A.; Roger, E.; Kempf, M.; Racineux, J.L.; Diot, P.; Benoit, J.P.; et al. Lipid Nanocapsules: Ready-to-Use Nanovectors for the Aerosol Delivery of Paclitaxel. Eur. J. Pharm. Biopharm. 2009, 73, 239–246. [Google Scholar] [CrossRef] [Green Version]
- Cipolla, D.; Gonda, I.; Chan, H.K. Liposomal Formulations for Inhalation. Ther. Deliv. 2013, 4, 1047–1072. [Google Scholar] [CrossRef]
- Wauthoz, N.; Rosière, R.; Amighi, K. Inhaled Cytotoxic Chemotherapy: Clinical Challenges, Recent Developments, and Future Prospects. Expert Opin. Drug Deliv. 2021, 18, 333–354. [Google Scholar] [CrossRef]
- Levet, V.; Rosière, R.; Merlos, R.; Fusaro, L.; Berger, G.; Amighi, K.; Wauthoz, N. Development of Controlled-Release Cisplatin Dry Powders for Inhalation against Lung Cancers. Int. J. Pharm. 2016, 515, 209–220. [Google Scholar] [CrossRef]
- Meenach, S.A.; Anderson, K.W.; Zach Hilt, J.; McGarry, R.C.; Mansour, H.M. Characterization and Aerosol Dispersion Performance of Advanced Spray-Dried Chemotherapeutic PEGylated Phospholipid Particles for Dry Powder Inhalation Delivery in Lung Cancer. Eur. J. Pharm. Sci. 2013, 49, 699–711. [Google Scholar] [CrossRef] [Green Version]
- El-Gendy, N.; Berkland, C. Combination Chemotherapeutic Dry Powder Aerosols via Controlled Nanoparticle Agglomeration. Pharm. Res. 2009, 26, 1752–1763. [Google Scholar] [CrossRef] [Green Version]
- Wauthoz, N.; Deleuze, P.; Saumet, A.; Duret, C.; Kiss, R.; Amighi, K. Temozolomide-Based Dry Powder Formulations for Lung Tumor-Related Inhalation Treatment. Pharm. Res. 2011, 28, 762–775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, T.; Lin, S.; Niu, B.; Wang, X.; Huang, Y.; Zhang, X.; Li, G.; Pan, X.; Wu, C. Influence of Physical Properties of Carrier on the Performance of Dry Powder Inhalers. Acta Pharm. Sin. B 2016, 6, 308–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deb, P.K.; Abed, S.N.; Jaber, A.M.Y.; Tekade, R.K. Particulate Level Properties and Its Implications on Product Performance and Processing. In Dosage Form Design Parameters; Academic Press: Cambridge, MA, USA, 2018; Volume 2, pp. 155–220. ISBN 9780128144220. [Google Scholar]
- Pilcer, G.; Amighi, K. Formulation Strategy and Use of Excipients in Pulmonary Drug Delivery. Int. J. Pharm. 2010, 392, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Pilcer, G.; Wauthoz, N.; Amighi, K. Lactose Characteristics and the Generation of the Aerosol. Adv. Drug Deliv. Rev. 2012, 64, 233–256. [Google Scholar] [CrossRef]









| Lung Clearance Mechanism | Strategy | Reference |
|---|---|---|
| Mucociliary Clearance | Dae = 1.8–2.8 μm Increase mucus penetration with PEG-based formulation | [20,21,22] |
| Alveolar Phagocytosis | Dae = 1–1.5 μm Vary particle size: nanoparticles, microparticlesVary geometric shape—worm-like-shaped particles | [23] |
| Dissolution | Micro and nanoparticles (lipid-, polymer-based) Liposomes | [22,24] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gupta, C.; Jaipuria, A.; Gupta, N. Inhalable Formulations to Treat Non-Small Cell Lung Cancer (NSCLC): Recent Therapies and Developments. Pharmaceutics 2023, 15, 139. https://doi.org/10.3390/pharmaceutics15010139
Gupta C, Jaipuria A, Gupta N. Inhalable Formulations to Treat Non-Small Cell Lung Cancer (NSCLC): Recent Therapies and Developments. Pharmaceutics. 2023; 15(1):139. https://doi.org/10.3390/pharmaceutics15010139
Chicago/Turabian StyleGupta, Chetna, Aadya Jaipuria, and Nikesh Gupta. 2023. "Inhalable Formulations to Treat Non-Small Cell Lung Cancer (NSCLC): Recent Therapies and Developments" Pharmaceutics 15, no. 1: 139. https://doi.org/10.3390/pharmaceutics15010139