Construction of a Multifunctional Nano-Scale Metal-Organic Framework-Based Drug Delivery System for Targeted Cancer Therapy
Abstract
:1. Introduction
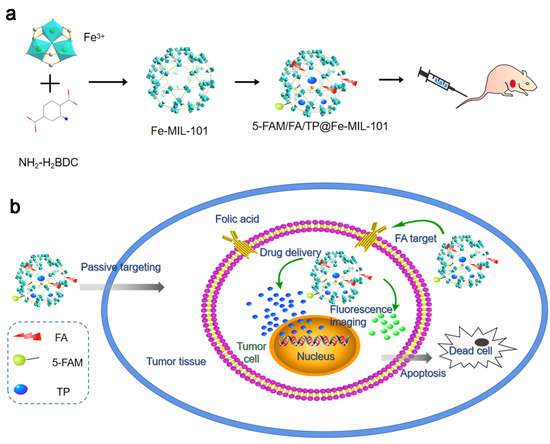
2. Materials and Methods
2.1. Synthesis MOFs
2.1.1. Synthesis of Fe-MIL-101
2.1.2. Synthesis of TP@Fe-MIL-101
2.1.3. Synthesis of 5-FAM/FA/TP@Fe-MIL-101
2.2. Characterizations of NPs
2.3. In Vitro Drug Release Study
2.4. Cell Culture
2.5. In Vitro Cytotoxicity Assay
2.6. Annexin V/PI Double-Staining Assay
2.6.1. Measurement of Intracellular ROS
2.6.2. Measurement of Mitochondrial Membrane Potential (MMP)
2.7. Cell Uptake Study
2.8. Western Blot Analysis
2.9. Animal and Tumor-Bearing Mouse Model
2.10. Distribution of Functionalized Nanoparticles In Vivo
2.11. Antitumor Effect of Functionalized Nanoparticles In Vivo
2.12. Safety Evaluation of Functionalized NPs In Vivo
2.13. Statistical Methods
3. Results
3.1. Preparation and Characterization of NPs
3.2. Study on the Drug Release of Functionalized Nanoparticles In Vitro
3.3. In Vitro Biological Evaluation of Functionalized NPs
3.3.1. In Vitro Cytotoxicity Assay
3.3.2. Cell Uptake Study
3.3.3. Western Blot Analysis
3.4. Distribution of Functionalized Nanoparticles In Vivo
3.5. Antitumor Effect of Functionalized Nanoparticles In Vivo
3.6. Safety Evaluation of Functionalized NPs In Vivo
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peng, M.; Darko, K.O.; Tao, T.; Huang, Y.J.; Su, Q.L.; He, C.M.; Yin, T.; Liu, Z.Q.; Yang, X.P. Combination of metformin with chemotherapeutic drugs via different molecular mechanisms. Cancer Treat. Rev. 2017, 54, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhao, J.; Hu, L.; Cao, Y.C.; Huang, B. Low dosages: New chemotherapeutic weapons on the battlefield of immune-related disease. Cell. Mol. Immunol. 2011, 8, 289–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lammers, T.; Kiessling, F.; Hennink, W.E.; Storm, G. Drug targeting to tumors: Principles, pitfalls and (pre-) clinical progress. J. Control. Release 2012, 161, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.C.; Xie, Z.X.; Li, D.D.; Kassymova, M.; Zang, S.Q.; Jiang, H.L. Nano-sized metal-organic frameworks: Synthesis and applications. Coord. Chem. Rev. 2020, 417, 213366. [Google Scholar] [CrossRef]
- Farha, O.K.; Hupp, J.T. Rational Design, Synthesis, Purification, and Activation of Metal-Organic Framework Materials. Acc. Chem. Res. 2010, 43, 1166–1175. [Google Scholar] [CrossRef] [Green Version]
- Luo, Z.D.; Fan, S.R.; Gu, C.Y.; Liu, W.C.; Chen, J.X.; Li, B.H.; Liu, J.A. Metal-Organic Framework (MOF)-based Nanomaterials for Biomedical Applications. Curr. Med. Chem. 2019, 26, 3341–3369. [Google Scholar] [CrossRef]
- Peikert, K.; McCormick, L.J.; Cattaneo, D.; Duncan, M.J.; Hoffmann, F.; Khan, A.H.; Bertmer, M.; Morris, R.E.; Froba, M. Tuning the nitric oxide release behavior of amino functionalized HKUST-1. Microporous Mesoporous Mater. 2015, 216, 118–126. [Google Scholar] [CrossRef]
- Rasheed, T.; Bilal, M.; Hassan, A.A.; Nabeel, F.; Bharagava, R.N.; Ferreira, L.F.R.; Tran, H.N.; Iqbal, H.M.N. Environmental threatening concern and efficient removal of pharmaceutically active compounds using metal-organic frameworks as adsorbents. Environ. Res. 2020, 185, 109436. [Google Scholar] [CrossRef]
- Fang, Y.X.; Ma, Y.W.; Zheng, M.F.; Yang, P.J.; Asiri, A.M.; Wang, X.C. Metal-organic frameworks for solar energy conversion by photoredox catalysis. Coord. Chem. Rev. 2018, 373, 83–115. [Google Scholar] [CrossRef]
- Hatami, Z.; Jalali, F.; Tabrizi, M.A.; Shamsipur, M. Application of metal-organic framework as redox probe in an electrochemical aptasensor for sensitive detection of MUC1. Biosens. Bioelectron. 2019, 141, 111433. [Google Scholar] [CrossRef]
- Shang, L.; Xu, J.; Nienhaus, G.U. Recent advances in synthesizing metal nanocluster-based nanocomposites for application in sensing, imaging and catalysis. Nano Today 2019, 28, 100767. [Google Scholar] [CrossRef]
- Park, H.J.; Suh, M.P. Enhanced isosteric heat of H-2 adsorption by inclusion of crown ethers in a porous metal-organic framework. Chem. Commun. 2012, 48, 3400–3402. [Google Scholar] [CrossRef]
- Ibrahim, M.; Sabouni, R.; Husseini, G.A. Anti-cancer Drug Delivery Using Metal Organic Frameworks (MOFs). Curr. Med. Chem. 2017, 24, 193–214. [Google Scholar] [CrossRef] [PubMed]
- Rojas, S.; Arenas-Vivo, A.; Horcajada, P. Metal-organic frameworks: A novel platform for combined advanced therapies. Coord. Chem. Rev. 2019, 388, 202–226. [Google Scholar] [CrossRef]
- Chen, X.R.; Tong, R.L.; Shi, Z.Q.; Yang, B.; Liu, H.; Ding, S.P.; Wang, X.; Lei, Q.F.; Wu, J.; Fang, W.J. MOF Nanoparticles with Encapsulated Autophagy Inhibitor in Controlled Drug Delivery System for Antitumor. ACS Appl. Mater. Interfaces 2018, 10, 2328–2337. [Google Scholar] [CrossRef]
- Zhang, L.; Lei, J.P.; Ma, F.J.; Ling, P.H.; Liu, J.T.; Ju, H.X. A porphyrin photosensitized metal-organic framework for cancer cell apoptosis and caspase responsive theranostics. Chem. Commun. 2015, 51, 10831–10834. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Tyagi, S.; Paul, A.K. Development of Biocompatible Iron-Carboxylate Metal Organic Frameworks for pH-Responsive Drug Delivery Application. J. Nanosci. Nanotechnol. 2019, 19, 646–654. [Google Scholar] [CrossRef]
- Gao, X.; Hai, X.; Baigude, H.; Guan, W.; Liu, Z. Fabrication of functional hollow microspheres constructed from MOF shells: Promising drug delivery systems with high loading capacity and targeted transport. Sci. Rep. 2016, 6, 37705. [Google Scholar] [CrossRef]
- Liu, Y.L.; Zhao, X.J.; Yang, X.X.; Li, Y.F. A nanosized metal-organic framework of Fe-MIL-88NH(2) as a novel peroxidase mimic used for colorimetric detection of glucose. Analyst 2013, 138, 4526–4531. [Google Scholar] [CrossRef]
- Ai, L.; Li, L.; Zhang, C.; Fu, J.; Jiang, J. MIL-53(Fe): A Metal-Organic Framework with Intrinsic Peroxidase-Like Catalytic Activity for Colorimetric Biosensing. Chem. Eur. J. 2013, 19, 15105–15108. [Google Scholar] [CrossRef]
- Bellido, E.; Hidalgo, T.; Lozano, M.V.; Guillevic, M.; Simon-Vazquez, R.; Santander-Ortega, M.J.; Gonzalez-Fernandez, A.; Serre, C.; Alonso, M.J.; Horcajada, P. Heparin-Engineered Mesoporous Iron Metal-Organic Framework Nanoparticles: Toward Stealth Drug Nanocarriers. Adv. Healthc. Mater. 2015, 4, 1246–1257. [Google Scholar] [CrossRef]
- Kamaly, N.; Kalber, T.; Thanou, M.; Bell, J.D.; Miller, A.D. Folate Receptor Targeted Bimodal Liposomes for Tumor Magnetic Resonance Imaging. Bioconjugate Chem. 2009, 20, 648–655. [Google Scholar] [CrossRef]
- Prabaharan, M.; Grailer, J.J.; Pilla, S.; Steeber, D.A.; Gong, S. Folate-conjugated amphiphilic hyperbranched block copolymers based on Boltorn (R) H40, poly(L-lactide) and poly(ethylene glycol) for tumor-targeted drug delivery. Biomaterials 2009, 30, 3009–3019. [Google Scholar] [CrossRef] [PubMed]
- Stella, B.; Arpicco, S.; Peracchia, M.T.; Desmaele, D.; Hoebeke, J.; Renoir, M.; D’Angelo, J.; Cattel, L.; Couvreur, P. Design of folic acid-conjugated nanoparticles for drug targeting. J. Pharm. Sci. 2000, 89, 1452–1464. [Google Scholar] [CrossRef]
- Yang, S.J.; Lin, F.H.; Tsai, K.C.; Wei, M.F.; Tsai, H.M.; Wong, J.M.; Shieh, M.J. Folic Acid-Conjugated Chitosan Nanoparticles Enhanced Protoporphyrin IX Accumulation in Colorectal Cancer Cells. Bioconjugate Chem. 2010, 21, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.C.; Lock, L.L.; Cheetham, A.G.; Cui, H.G. Enhanced Cellular Entry and Efficacy of Tat Conjugates by Rational Design of the Auxiliary Segment. Mol. Pharm. 2014, 11, 964–973. [Google Scholar] [CrossRef]
- Gao, X.C.; Cui, R.X.; Ji, G.F.; Liu, Z.L. Size and surface controllable metal-organic frameworks (MOFs) for fluorescence imaging and cancer therapy. Nanoscale 2018, 10, 6205–6211. [Google Scholar] [CrossRef]
- Wang, C.Y.; Bai, X.Y.; Wang, C.H. Traditional Chinese Medicine: A Treasured Natural Resource of Anticancer Drug Research and Development. Am. J. Chin. Med. 2014, 42, 543–559. [Google Scholar] [CrossRef]
- Song, C.; Wang, Y.; Cui, L.; Yan, F.; Shen, S. Triptolide attenuates lipopolysaccharide-induced inflammatory responses in human endothelial cells: Involvement of NF-kappa B pathway. BMC Complementary Altern. Med. 2019, 19, 198. [Google Scholar] [CrossRef] [Green Version]
- Hou, W.; Liu, B.; Xu, H. Triptolide: Medicinal chemistry, chemical biology and clinical progress. Eur. J. Med. Chem. 2019, 176, 378–392. [Google Scholar] [CrossRef]
- Westerheide, S.D.; Kawahara, T.L.A.; Orton, K.; Morimoto, R.I. Triptolide, an inhibitor of the human heat shock response that enhances stress-induced cell death. J. Biol. Chem. 2006, 281, 9616–9622. [Google Scholar] [CrossRef] [Green Version]
- Shamon, L.A.; Pezzuto, J.M.; Graves, J.M.; Mehta, R.R.; Wangcharoentrakul, S.; Sangsuwan, R.; Chaichana, S.; Tuchinda, P.; Cleason, P.; Reutrakul, V. Evaluation of the mutagenic, cytotoxic, and antitumor potential of triptolide, a highly oxygenated diterpene isolated from Tripterygium wilfordii. Cancer Lett. 1997, 112, 113–117. [Google Scholar] [CrossRef]
- Zhang, C.; Peng, F.; Liu, W.; Wan, J.; Wan, C.; Xu, H.; Lam, C.W.; Yang, X. Nanostructured lipid carriers as a novel oral delivery system for triptolide: Induced changes in pharmacokinetics profile associated with reduced toxicity in male rats. Int. J. Nanomed. 2014, 9, 1049–1063. [Google Scholar]
- You, L.; Dong, X.; Ni, B.; Fu, J.; Yang, C.; Yin, X.; Leng, X.; Ni, J. Triptolide Induces Apoptosis Through Fas Death and Mitochondrial Pathways in HepaRG Cell Line. Front. Pharmacol. 2018, 9, 813. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Tjiptoputro, A.K.; Ding, J.; Xue, J.M.; Zhu, Y. Pd-Ce nanoparticles supported on functional Fe-MIL-101-NH2: An efficient catalyst for selective glycerol oxidation. Catal. Today 2017, 279, 77–83. [Google Scholar] [CrossRef]
- Wang, D.; Li, Z. Bi-functional NH2-MIL-101(Fe) for one-pot tandem photo-oxidation/Knoevenagel condensation between aromatic alcohols and active methylene compounds. Catal. Sci. Technol. 2015, 5, 1623–1628. [Google Scholar] [CrossRef]
- Wang, T.; Song, X.; Luo, Q.; Yang, X.; Chong, S.; Zhang, J.; Ji, M. Acid-base bifunctional catalyst: Carboxyl ionic liquid immobilized on MIL-101-NH2 for rapid synthesis of propylene carbonate from CO2 and propylene oxide under facile solvent-free conditions. Microporous Mesoporous Mater. 2018, 267, 84–92. [Google Scholar] [CrossRef]
- Liu, Y.; Li, Z.; Zou, S.; Lu, C.; Xiao, Y.; Bai, H.; Zhang, X.; Mu, H.; Zhang, X.; Duan, J. Hyaluronic acid-coated ZIF-8 for the treatment of pneumonia caused by methicillin-resistant Staphylococcus aureus. Int. J. Biol. Macromol. 2020, 155, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Li, Q.; Liu, R.; Zhang, X.; Li, Z.; Luan, Y. A Versatile Prodrug Strategy to In Situ Encapsulate Drugs in MOF Nanocarriers: A Case of Cytarabine-IR820 Prodrug Encapsulated ZIF-8 toward Chemo-Photothermal Therapy. Adv. Funct. Mater. 2018, 28, 1802830. [Google Scholar] [CrossRef]
- Wang, X.-G.; Dong, Z.-Y.; Cheng, H.; Wan, S.-S.; Chen, W.-H.; Zou, M.-Z.; Huo, J.-W.; Deng, H.-X.; Zhang, X.-Z. A multifunctional metal-organic framework based tumor targeting drug delivery system for cancer therapy. Nanoscale 2015, 7, 16061–16070. [Google Scholar] [CrossRef]
- Zhang, L.; Kong, S.-Y.; Zheng, Z.-Q.; Meng, X.-X.; Feng, J.-L.; Tan, H.-S.; Lao, Y.-Z.; Xiao, L.-B.; Xu, H.-X. Nujiangexathone A, a Novel Compound Derived from Garcinia nujiangensis, Induces Caspase-Dependent Apoptosis in Cervical Cancer through the ROS/JNK Pathway. Molecules 2016, 21, 1360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, H.; Yang, G.-X.; Zhang, X.; Meng, X.-B.; Sheng, J.-L.; Sun, X.-J.; Feng, Y.-J.; Zhang, F.-M. Folic Acid Functionalized Zirconium-Based Metal-Organic Frameworks as Drug Carriers for Active Tumor-Targeted Drug Delivery. Chem. Eur. J. 2018, 24, 17148–17154. [Google Scholar] [CrossRef] [PubMed]
- Xiao, X.; Bai, P.; Nguyen, T.M.B.; Xiao, J.; Liu, S.; Yang, G.; Hu, L.; Chen, X.; Zhang, X.; Liu, J.; et al. The antitumoral effect of Paris Saponin I associated with the induction of apoptosis through the mitochondrial pathway. Mol. Cancer Ther. 2009, 8, 1179–1188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, X.; Shi, Z.; Peng, Z.; Zhao, C.; Zhang, Y.; Wang, Z.; Li, X.; Liu, G.; Li, X. Acetoacetate induces hepatocytes apoptosis by the ROS-mediated MAPKs pathway in ketotic cows. J. Cell. Physiol. 2017, 232, 3296–3308. [Google Scholar] [CrossRef]
- Tomek, M.; Akiyama, T.; Dass, C.R. Role of Bcl-2 in tumour cell survival and implications for pharmacotherapy. J. Pharm. Pharmacol. 2012, 64, 1695–1702. [Google Scholar] [CrossRef]
- Cherukuri, D.P.; Nelson, M.A. Role of reactive oxygen species (ROS) and JNKs in selenite-induced apoptosis in HepG2 cells. Cancer Biol. Ther. 2008, 7, 697–698. [Google Scholar] [CrossRef] [Green Version]
- Lavrik, I.N. Systems biology of apoptosis signaling networks. Curr. Opin. Biotechnol. 2010, 21, 551–555. [Google Scholar] [CrossRef]
- Jaracz, S.; Chen, J.; Kuznetsova, L.V.; Ojima, L. Recent advances in tumor-targeting anticancer drug conjugates. Bioorganic Med. Chem. 2005, 13, 5043–5054. [Google Scholar] [CrossRef]








Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cai, M.; Zeng, Y.; Liu, M.; You, L.; Huang, H.; Hao, Y.; Yin, X.; Qu, C.; Ni, J.; Dong, X. Construction of a Multifunctional Nano-Scale Metal-Organic Framework-Based Drug Delivery System for Targeted Cancer Therapy. Pharmaceutics 2021, 13, 1945. https://doi.org/10.3390/pharmaceutics13111945
Cai M, Zeng Y, Liu M, You L, Huang H, Hao Y, Yin X, Qu C, Ni J, Dong X. Construction of a Multifunctional Nano-Scale Metal-Organic Framework-Based Drug Delivery System for Targeted Cancer Therapy. Pharmaceutics. 2021; 13(11):1945. https://doi.org/10.3390/pharmaceutics13111945
Chicago/Turabian StyleCai, Mengru, Yawen Zeng, Manting Liu, Longtai You, Huating Huang, Yang Hao, Xingbin Yin, Changhai Qu, Jian Ni, and Xiaoxv Dong. 2021. "Construction of a Multifunctional Nano-Scale Metal-Organic Framework-Based Drug Delivery System for Targeted Cancer Therapy" Pharmaceutics 13, no. 11: 1945. https://doi.org/10.3390/pharmaceutics13111945