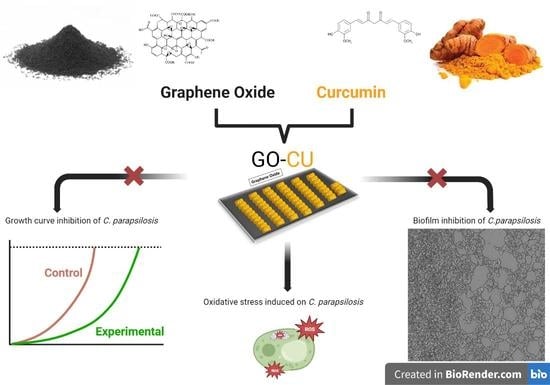
Curcumin-Functionalized Graphene Oxide Strongly Prevents Candida parapsilosis Adhesion and Biofilm Formation
Abstract
:1. Introduction
2. Results
2.1. Characterization of GO- and GO/CU-Coated Surfaces
2.2. Effect of GO and GO/CU on C. parapsilosis Planktonic Cells
2.2.1. Growth Curve
2.2.2. Reactive Oxygen Species Assay
2.3. Effect of GO and GO/CU Surfaces on C. parapsilosis Early Adhesion and Biofilm Formation
2.3.1. C. parapsilosis Coated Surface Adhesion
2.3.2. Crystal Violet Assay
2.3.3. Live and Dead Assay
2.4. Effect of GO and GO/CU Surfaces on C. parapsilosis Mature Biofilm Formation
2.4.1. Fluorescein Diacetate Assay (FDA)
2.4.2. EPS Staining
3. Discussion
4. Materials and Methods
4.1. GO and GO/CU Surface Preparation
4.2. Characterization of Samples
4.3. Clinical Strain
4.4. Growth Curve
4.5. ROS Assay
4.6. Adhesion Assay
4.7. Crystal Violet Biofilm Quantification Assay
4.8. LIVE and DEAD Assay
4.9. FDA
4.10. Biofilm Confocal Microscopy
4.11. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dadi, N.C.T.; Radochová, B.; Vargová, J.; Bujdáková, H. Impact of Healthcare-Associated Infections Connected to Medical Devices—An Update. Microorganisms 2021, 9, 2332. [Google Scholar] [CrossRef]
- Davey, M.E.; O’toole, G.A. Microbial Biofilms: From Ecology to Molecular Genetics. Microbiol. Mol. Biol. Rev. 2000, 64, 847–867. [Google Scholar] [CrossRef]
- Bugli, F.; Posteraro, B.; Papi, M.; Torelli, R.; Maiorana, A.; Sterbini, F.P.; Posteraro, P.; Sanguinetti, M.; de Spirito, M. In Vitro Interaction between Alginate Lyase and Amphotericin B against Aspergillus Fumigatus Biofilm Determined by Different Methods. Antimicrob. Agents Chemother. 2013, 57, 1275–1282. [Google Scholar] [CrossRef]
- Arciola, C.R.; Campoccia, D.; Montanaro, L. Implant Infections: Adhesion, Biofilm Formation and Immune Evasion. Nat. Rev. Microbiol. 2018, 16, 397–409. [Google Scholar] [CrossRef]
- Stoodley, P.; Sauer, K.; Davies, D.G.; Costerton, J.W. Biofilms as Complex Differentiated Communities. Annu. Rev. Microbiol. 2002, 56, 187–209. [Google Scholar] [CrossRef] [PubMed]
- Ciofu, O.; Moser, C.; Jensen, P.Ø.; Høiby, N. Tolerance and Resistance of Microbial Biofilms. Nat. Rev. Microbiol. 2022, 20, 621–635. [Google Scholar] [CrossRef] [PubMed]
- Alam, F.; Catlow, D.; di Maio, A.; Blair, J.M.A.; Hall, R.A. Candida Albicans Enhances Meropenem Tolerance of Pseudomonas Aeruginosa in a Dual-Species Biofilm. J. Antimicrob. Chemother. 2020, 75, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Cao, B.; Christophersen, L.; Thomsen, K.; Sønderholm, M.; Bjarnsholt, T.; Jensen, P.Ø.; Høiby, N.; Moser, C. Antibiotic Penetration and Bacterial Killing in a Pseudomonas Aeruginosa Biofilm Model. J. Antimicrob. Chemother. 2015, 70, 2057–2063. [Google Scholar] [CrossRef] [PubMed]
- Hrynyshyn, A.; Simões, M.; Borges, A. Biofilms in Surgical Site Infections: Recent Advances and Novel Prevention and Eradication Strategies. Antibiotics 2022, 11, 69. [Google Scholar] [CrossRef]
- Torelli, R.; Cacaci, M.; Papi, M.; Paroni Sterbini, F.; Martini, C.; Posteraro, B.; Palmieri, V.; de Spirito, M.; Sanguinetti, M.; Bugli, F. Different Effects of Matrix Degrading Enzymes towards Biofilms Formed by E. Faecalis and E. Faecium Clinical Isolates. Colloids Surf B Biointerfaces 2017, 158, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Molina-Santiago, C.; de Vicente, A.; Romero, D. Bacterial Extracellular Matrix as a Natural Source of Biotechnologically Multivalent Materials. Comput. Struct. Biotechnol. J. 2021, 19, 2796–2805. [Google Scholar] [CrossRef]
- Brandwein, M.; Steinberg, D.; Meshner, S. Microbial Biofilms and the Human Skin Microbiome. NPJ Biofilms Microbiomes. 2016, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Hardy, L.; Cerca, N.; Jespers, V.; Vaneechoutte, M.; Crucitti, T. Bacterial Biofilms in the Vagina. Res. Microbiol. 2017, 168, 865–874. [Google Scholar] [CrossRef] [PubMed]
- Motta, J.P.; Wallace, J.L.; Buret, A.G.; Deraison, C.; Vergnolle, N. Gastrointestinal Biofilms in Health and Disease. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 314–334. [Google Scholar] [CrossRef]
- Rodríguez-Merchán, E.C.; Davidson, D.J.; Liddle, A.D. Recent Strategies to Combat Infections from Biofilm-Forming Bacteria on Orthopaedic Implants. Int. J. Mol. Sci. 2021, 22, 10243. [Google Scholar] [CrossRef] [PubMed]
- Tumbarello, M.; Posteraro, B.; Trecarichi, E.M.; Fiori, B.; Rossi, M.; Porta, R.; Donati, K.D.G.; la Sorda, M.; Spanu, T.; Fadda, G.; et al. Biofilm Production by Candida Species and Inadequate Antifungal Therapy as Predictors of Mortality for Patients with Candidemia. J. Clin. Microbiol. 2007, 45, 1843–1850. [Google Scholar] [CrossRef]
- Quindós, G. Epidemiology of Candidaemia and Invasive Candidiasis. A Changing Face. Rev. Iberoam. Micol. 2014, 31, 42–48. [Google Scholar] [CrossRef]
- da Silva, E.M.; Sciuniti Benites Mansano, E.; de Souza Bonfim-Mendonça, P.; Olegário, R.; Tobaldini-Valério, F.; Fiorini, A.; Svidzinski, T.I.E. High Colonization by Candida Parapsilosis Sensu Stricto on Hands and Surfaces in an Adult Intensive Care Unit. J. Med. Mycol. 2021, 31, 101110. [Google Scholar] [CrossRef]
- Vera-González, N.; Shukla, A. Advances in Biomaterials for the Prevention and Disruption of Candida Biofilms. Front. Microbiol. 2020, 11, 538602. [Google Scholar] [CrossRef]
- Palmieri, V.; Bugli, F.; Lauriola, M.C.; Cacaci, M.; Torelli, R.; Ciasca, G.; Conti, C.; Sanguinetti, M.; Papi, M.; de Spirito, M. Bacteria Meet Graphene: Modulation of Graphene Oxide Nanosheet Interaction with Human Pathogens for Effective Antimicrobial Therapy. ACS Biomater. Sci. Eng. 2017, 3, 619–627. [Google Scholar] [CrossRef]
- Tricomi, J.; Cacaci, M.; Biagiotti, G.; Caselli, L.; Niccoli, L.; Torelli, R.; Gabbani, A.; di Vito, M.; Pineider, F.; Severi, M.; et al. Ball Milled Glyco-Graphene Oxide Conjugates Markedly Disrupted Pseudomonas Aeruginosa Biofilms. Nanoscale 2022, 14, 10190–10199. [Google Scholar] [CrossRef]
- Cacaci, M.; Martini, C.; Guarino, C.; Torelli, R.; Bugli, F.; Sanguinetti, M. Graphene Oxide Coatings as Tools to Prevent Microbial Biofilm Formation on Medical Device. Adv. Exp. Med. Biol. 2020, 1282, 21–35. [Google Scholar]
- Palmieri, V.; Lauriola, M.C.; Ciasca, G.; Conti, C.; de Spirito, M.; Papi, M. The Graphene Oxide Contradictory Effects against Human Pathogens. Nanotechnology 2017, 28, 152001. [Google Scholar] [CrossRef] [PubMed]
- Mangadlao, J.D.; Santos, C.M.; Felipe, M.J.L.; de Leon, A.C.C.; Rodrigues, D.F.; Advincula, R.C. On the Antibacterial Mechanism of Graphene Oxide (GO) Langmuir-Blodgett Films. Chem. Commun. 2015, 51, 2886–2889. [Google Scholar] [CrossRef] [PubMed]
- Martini, C.; Longo, F.; Castagnola, R.; Marigo, L.; Grande, N.M.; Cordaro, M.; Cacaci, M.; Papi, M.; Palmieri, V.; Bugli, F.; et al. Antimicrobial and Antibiofilm Properties of Graphene Oxide on Enterococcus Faecalis. Antibiotics 2020, 9, 692. [Google Scholar] [CrossRef] [PubMed]
- Papi, M.; Palmieri, V.; Bugli, F.; de Spirito, M.; Sanguinetti, M.; Ciancico, C.; Braidotti, M.C.; Gentilini, S.; Angelani, L.; Conti, C. Biomimetic Antimicrobial Cloak by Graphene-Oxide Agar Hydrogel. Sci. Rep. 2016, 6, 12. [Google Scholar] [CrossRef] [PubMed]
- Zheng, D.; Huang, C.; Huang, H.; Zhao, Y.; Khan, M.R.U.; Zhao, H.; Huang, L. Antibacterial Mechanism of Curcumin: A Review. Chem. Biodivers. 2020, 17, e2000171. [Google Scholar] [CrossRef] [PubMed]
- Zorofchian Moghadamtousi, S.; Abdul Kadir, H.; Hassandarvish, P.; Tajik, H.; Abubakar, S.; Zandi, K. A Review on Antibacterial, Antiviral, and Antifungal Activity of Curcumin. Biomed Res. Int. 2014, 2014, 186864. [Google Scholar] [CrossRef] [PubMed]
- Rai, D.; Singh, J.K.; Roy, N.; Panda, D. Curcumin Inhibits FtsZ Assembly: An Attractive Mechanism for Its Antibacterial Activity. Biochem. J. 2008, 410, 147–155. [Google Scholar] [CrossRef]
- Tyagi, P.; Singh, M.; Kumari, H.; Kumari, A.; Mukhopadhyay, K. Bactericidal Activity of Curcumin I Is Associated with Damaging of Bacterial Membrane. PLoS ONE 2015, 10, e0121313. [Google Scholar] [CrossRef]
- Bugli, F.; Cacaci, M.; Palmieri, V.; di Santo, R.; Torelli, R.; Ciasca, G.; di Vito, M.; Vitali, A.; Conti, C.; Sanguinetti, M.; et al. Curcumin-Loaded Graphene Oxide Flakes as an Effective Antibacterial System against Methicillin-Resistant Staphylococcus Aureus. Interface Focus 2018, 8, 20170059. [Google Scholar] [CrossRef] [Green Version]
- Oluwole, D.O.; Coleman, L.; Buchanan, W.; Chen, T.; la Ragione, R.M.; Liu, L.X. Antibiotics-Free Compounds for Chronic Wound Healing. Pharmaceutics 2022, 14, 1021. [Google Scholar] [CrossRef]
- Packiavathy, I.A.S.V.; Priya, S.; Pandian, S.K.; Ravi, A.V. Inhibition of Biofilm Development of Uropathogens by Curcumin—An Anti-Quorum Sensing Agent from Curcuma Longa. Food Chem. 2014, 148, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Gayani, B.; Dilhari, A.; Wijesinghe, G.K.; Kumarage, S.; Abayaweera, G.; Samarakoon, S.R.; Perera, I.C.; Kottegoda, N.; Weerasekera, M.M. Effect of Natural Curcuminoids-Intercalated Layered Double Hydroxide Nanohybrid against Staphylococcus Aureus, Pseudomonas Aeruginosa, and Enterococcus Faecalis: A Bactericidal, Antibiofilm, and Mechanistic Study. Microbiologyopen 2019, 8, e00723. [Google Scholar] [CrossRef]
- Azari, B.; Zahmatkesh Moghadam, S.; Zarrinfar, H.; Tasbandi, A.; Jamialahmadi, T.; Sahebkar, A. Antifungal Activity of Curcuminoids and Difluorinated Curcumin Against Clinical Isolates of Candida Species. Adv. Exp. Med. Biol. 2021, 1328, 123–129. [Google Scholar] [CrossRef]
- Karameşe, M.; Özgür, D. The Antibacterial and Antifungal Activities of Commonly Used Herbal Oils. J. Exp. Clin. Med. 2020, 37, 47–51. [Google Scholar] [CrossRef]
- Prasad, S.; Tyagi, A.K.; Aggarwal, B.B. Recent Developments in Delivery, Bioavailability, Absorption and Metabolism of Curcumin: The Golden Pigment from Golden Spice. Cancer Res. Treat. 2014, 46, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, V.; Bugli, F.; Cacaci, M.; Perini, G.; de Maio, F.; Delogu, G.; Torelli, R.; Conti, C.; Sanguinetti, M.; de Spirito, M.; et al. Graphene Oxide Coatings Prevent Candida Albicans Biofilm Formation with a Controlled Release of Curcumin-Loaded Nanocomposites. Nanomedicine 2018, 13, 2867–2879. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Hosseinipour, M.; Abdolvand, H.; Najafabadi, S.A.A.; Sahraneshin Samani, F. Improvement in Bioavailability of Curcumin within the Castor-Oil Based Polyurethane Nanocomposite through Its Conjugation on the Surface of Graphene Oxide Nanosheets. Polym. Adv. Technol. 2022, 33, 1126–1136. [Google Scholar] [CrossRef]
- Pourmadadi, M.; Abbasi, P.; Eshaghi, M.M.; Bakhshi, A.; Ezra Manicum, A.-L.; Rahdar, A.; Pandey, S.; Jadoun, S.; Díez-Pascual, A.M. Curcumin Delivery and Co-Delivery Based on Nanomaterials as an Effective Approach for Cancer Therapy. J. Drug Deliv. Sci Technol. 2022, 78, 103982. [Google Scholar] [CrossRef]
- Yan, H.; Li, P.; Jiang, X.; Wang, X.; Hu, Y.; Zhang, Y.; Su, R.; Su, W. Preparation of Graphene Oxide/Polydopamine-Curcumin Composite Nanomaterials and Its Antibacterial Effect against Staphylococcus Aureus Induced by White Light. Biomater. Adv. 2022, 139, 213040. [Google Scholar] [CrossRef] [PubMed]
- Esmaeili, Y.; Seyedhosseini Ghaheh, H.; Ghasemi, F.; Shariati, L.; Rafienia, M.; Bidram, E.; Zarrabi, A. Graphene Oxide Quantum Dot-Chitosan Nanotheranostic Platform as a PH-Responsive Carrier for Improving Curcumin Uptake Internalization: In Vitro & in Silico Study. Biomater. Adv. 2022, 139, 213017. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.; Singh, J.G.; Afzal, O.; Altamimi, A.S.A.; Alrobaian, M.; Haneef, J.; Barkat, M.A.; Almalki, W.H.; Handa, M.; Shukla, R.; et al. Preparation, Characterization, and Evaluation of Curcumin-Graphene Oxide Complex-Loaded Liposomes against Staphylococcus Aureus in Topical Disease. ACS Omega 2022, 7, 43499–43509. [Google Scholar] [CrossRef] [PubMed]
- Chiari, W.; Damayanti, R.; Harapan, H.; Puspita, K.; Saiful, S.; Rahmi, R.; Rizki, D.R.; Iqhrammullah, M. Trend of Polymer Research Related to COVID-19 Pandemic: Bibliometric Analysis. Polymers 2022, 14, 3297. [Google Scholar] [CrossRef] [PubMed]
- Biagiotti, G.; Salvatore, A.; Toniolo, G.; Caselli, L.; di Vito, M.; Cacaci, M.; Contiero, L.; Gori, T.; Maggini, M.; Sanguinetti, M.; et al. Metal-Free Antibacterial Additives Based on Graphene Materials and Salicylic Acid: From the Bench to Fabric Applications. ACS Appl Mater Interfaces 2021, 13, 26288–26298. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Yang, Y. Antimicrobial Activity of Wool Fabric Treated with Curcumin. Dye. Pigment. 2005, 64, 157–161. [Google Scholar] [CrossRef]
- Soldini, S.; Posteraro, B.; Vella, A.; de Carolis, E.; Borghi, E.; Falleni, M.; Losito, A.R.; Maiuro, G.; Trecarichi, E.M.; Sanguinetti, M.; et al. Microbiologic and Clinical Characteristics of Biofilm-Forming Candida Parapsilosis Isolates Associated with Fungaemia and Their Impact on Mortality. Clin. Microbiol. Infect. 2018, 24, 771–777. [Google Scholar] [CrossRef]
- Ching, Y.C.; Gunathilake, T.M.S.U.; Chuah, C.H.; Ching, K.Y.; Singh, R.; Liou, N.S. Curcumin/Tween 20-Incorporated Cellulose Nanoparticles with Enhanced Curcumin Solubility for Nano-Drug Delivery: Characterization and in Vitro Evaluation. Cellulose 2019, 26, 5467–5481. [Google Scholar] [CrossRef]
- Chen, X.; Zou, L.Q.; Niu, J.; Liu, W.; Peng, S.F.; Liu, C.M. The Stability, Sustained Release and Cellular Antioxidant Activity of Curcumin Nanoliposomes. Molecules 2015, 20, 14293–14311. [Google Scholar] [CrossRef]
- Ismail, E.H.; Sabry, D.Y.; Mahdy, H.; Khalil, M.M.H. Synthesis and Characterization of Some Ternary Metal Complexes of Curcumin with 1,10-Phenanthroline and Their Anticancer Applications. J. Sci. Res. 2014, 6, 509–519. [Google Scholar] [CrossRef]
- Banerjee, R. Inhibitory Effect of Curcumin-Cu(II) and Curcumin-Zn(II) Complexes on Amyloid-Beta Peptide Fibrillation. Bioinorg. Chem. Appl. 2014, 2014, 325873. [Google Scholar] [CrossRef] [Green Version]
- Hayyan, M.; Abo-Hamad, A.; AlSaadi, M.A.H.; Hashim, M.A. Functionalization of Graphene Using Deep Eutectic Solvents. Nanoscale Res. Lett. 2015, 10, 1004. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Jiang, J.; Zhu, Z.; Liao, Z.; Yao, X.; Yang, Y.; Cao, Y.; Jiang, Y. Lysine Enhances the Effect of Amphotericin B against Candida Albicans in Vitro. Acta Biochim. Biophys. Sin. 2016, 48, 182–193. [Google Scholar] [CrossRef]
- Elbasuney, S.; El-Sayyad, G.S. Silver Nanoparticles Coated Medical Fiber Synthesized by Surface Engineering with Bio-Inspired Mussel Powered Polydopamine: An Investigated Antimicrobial Potential with Bacterial Membrane Leakage Reaction Mechanism. Microb. Pathog. 2022, 169, 105680. [Google Scholar] [CrossRef] [PubMed]
- Yun, D.G.; Lee, D.G. Antibacterial Activity of Curcumin via Apoptosis-like Response in Escherichia Coli. Appl. Microbiol. Biotechnol. 2016, 100, 5505–5514. [Google Scholar] [CrossRef]
- Martins, C.V.B.; da Silva, D.L.; Neres, A.T.M.; Magalhães, T.F.F.; Watanabe, G.A.; Modolo, L.; Sabino, A.A.; de Fátima, Â.; de Resende, M.A. Curcumin as a Promising Antifungal of Clinical Interest. J. Antimicrob. Chemother. 2009, 63, 337–339. [Google Scholar] [CrossRef]
- Sharma, M.; Manoharlal, R.; Puri, N.; Prasad, R. Antifungal Curcumin Induces Reactive Oxygen Species and Triggers an Early Apoptosis but Prevents Hyphae Development by Targeting the Global Repressor TUP1 in Candida Albicans. Biosci. Rep. 2010, 30, 391–404. [Google Scholar] [CrossRef] [PubMed]
- Peeters, E.; Nelis, H.J.; Coenye, T. Comparison of Multiple Methods for Quantification of Microbial Biofilms Grown in Microtiter Plates. J. Microbiol. Methods 2008, 72, 157–165. [Google Scholar] [CrossRef]
- Yadav, N.; Dubey, A.; Shukla, S.; Saini, C.P.; Gupta, G.; Priyadarshini, R.; Lochab, B. Graphene Oxide-Coated Surface: Inhibition of Bacterial Biofilm Formation Due to Specific Surface-Interface Interactions. ACS Omega 2017, 2, 3070–3082. [Google Scholar] [CrossRef]
- Song, C.; Yang, C.M.; Sun, X.F.; Xia, P.F.; Qin, J.; Guo, B.B.; Wang, S.G. Influences of Graphene Oxide on Biofilm Formation of Gram-Negative and Gram-Positive Bacteria. Environ. Sci. Pollut. Res. Int. 2018, 25, 2853–2860. [Google Scholar] [CrossRef]
- Mihu, M.R.; Cabral, V.; Pattabhi, R.; Tar, M.T.; Davies, K.P.; Friedman, A.J.; Martinez, L.R.; Nosanchuk, J.D. Sustained Nitric Oxide-Releasing Nanoparticles Interfere with Methicillinresistant Staphylococcus Aureus Adhesion and Biofilm Formation in a Rat Central Venous Catheter Model. Antimicrob. Agents Chemother. 2017, 61, e02020-16. [Google Scholar] [CrossRef] [Green Version]
- Ramasamy, M.; Nanda, S.S.; Lee, J.H.; Lee, J. Construction of Alizarin Conjugated Graphene Oxide Composites for Inhibition of Candida Albicans Biofilms. Biomolecules 2020, 10, 565. [Google Scholar] [CrossRef] [PubMed]
- Pahlevanzadeh, F.; Setayeshmehr, M.; Bakhsheshi-Rad, H.R.; Emadi, R.; Kharaziha, M.; Poursamar, S.A.; Ismail, A.F.; Sharif, S.; Chen, X.; Berto, F. A Review on Antibacterial Biomaterials in Biomedical Applications: From Materials Perspective to Bioinks Design. Polymers 2022, 14, 2238. [Google Scholar] [CrossRef] [PubMed]
- Alalwan, H.; Rajendran, R.; Lappin, D.F.; Combet, E.; Shahzad, M.; Robertson, D.; Nile, C.J.; Williams, C.; Ramage, G. The Anti-Adhesive Effect of Curcumin on Candida Albicans Biofilms on Denture Materials. Front. Microbiol. 2017, 8, 659. [Google Scholar] [CrossRef] [PubMed]
- Kaur, S.; Modi, N.H.; Panda, D.; Roy, N. Probing the Binding Site of Curcumin in Escherichia Coli and Bacillus Subtilis FtsZ--a Structural Insight to Unveil Antibacterial Activity of Curcumin. Eur. J. Med. Chem. 2010, 45, 4209–4214. [Google Scholar] [CrossRef]
- Bellio, P.; Brisdelli, F.; Perilli, M.; Sabatini, A.; Bottoni, C.; Segatore, B.; Setacci, D.; Amicosante, G.; Celenza, G. Curcumin Inhibits the SOS Response Induced by Levofloxacin in Escherichia Coli. Phytomedicine 2014, 21, 430–434. [Google Scholar] [CrossRef]
- Langvad, F. A Rapid and Efficient Method for Growth Measurement of Filamentous Fungi. J. Microbiol. Methods 1999, 37, 97–100. [Google Scholar] [CrossRef]
- Shahina, Z.; Ndlovu, E.; Persaud, O.; Sultana, T.; Dahms, T.E.S. Candida Albicans Reactive Oxygen Species (ROS)-Dependent Lethality and ROS-Independent Hyphal and Biofilm Inhibition by Eugenol and Citral. Microbiol. Spectr. 2022, 10, e03183-22. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Liao, K.; Hang, C.; Wang, D. Honokiol Induces Reactive Oxygen Species-Mediated Apoptosis in Candida Albicans through Mitochondrial Dysfunction. PLoS ONE 2017, 12, e0172228. [Google Scholar] [CrossRef] [Green Version]










Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cacaci, M.; Squitieri, D.; Palmieri, V.; Torelli, R.; Perini, G.; Campolo, M.; Di Vito, M.; Papi, M.; Posteraro, B.; Sanguinetti, M.; et al. Curcumin-Functionalized Graphene Oxide Strongly Prevents Candida parapsilosis Adhesion and Biofilm Formation. Pharmaceuticals 2023, 16, 275. https://doi.org/10.3390/ph16020275
Cacaci M, Squitieri D, Palmieri V, Torelli R, Perini G, Campolo M, Di Vito M, Papi M, Posteraro B, Sanguinetti M, et al. Curcumin-Functionalized Graphene Oxide Strongly Prevents Candida parapsilosis Adhesion and Biofilm Formation. Pharmaceuticals. 2023; 16(2):275. https://doi.org/10.3390/ph16020275
Chicago/Turabian StyleCacaci, Margherita, Damiano Squitieri, Valentina Palmieri, Riccardo Torelli, Giordano Perini, Michela Campolo, Maura Di Vito, Massimiliano Papi, Brunella Posteraro, Maurizio Sanguinetti, and et al. 2023. "Curcumin-Functionalized Graphene Oxide Strongly Prevents Candida parapsilosis Adhesion and Biofilm Formation" Pharmaceuticals 16, no. 2: 275. https://doi.org/10.3390/ph16020275