Polymerized Albumin Receptor of Hepatitis B Virus for Evading the Reticuloendothelial System
Abstract
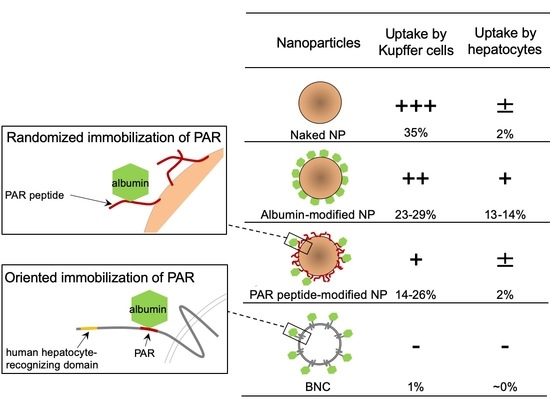
:1. Introduction
2. Results and Discussion
2.1. In Vivo Biodistribution of BNC-LP Complexes
2.2. Binding of BNCs to Various Albumins
2.3. Affinity of BNC-Derived Peptides to pHSA
2.4. Effect of BNC-Derived Peptides on Phagocytosis by Kupffer Cells
2.5. Effect of BNC-Derived Peptides on Circulation Time of NPs
2.6. Effect of BNC-Derived Peptides on Hepatotropic Properties of NPs
3. Materials and Methods
3.1. Bio-Nanocapsules (BNC), Liposomes (LPs), and BNC-LP Complexes
3.2. In Vivo Imaging
3.3. Pull-Down Assays with Albumin-Conjugated Resins
3.4. Pull-Down Assays with Peptide-Conjugated Resins
3.5. Quartz Crystal Microbalance (QCM) Analysis
3.6. Surface Modifications of 100-nm Polystyrene Microspheres
3.7. Phagocytosis Assay with Kupffer Cells
3.8. Measurement of Plasma Microsphere Concentrations
3.9. Hepatocyte Uptake Assay
3.10. Statistics
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Stolnik, S.; Illum, L.; Davis, S. Long circulating microparticulate drug carriers. Adv. Drug Deliv. Rev. 1995, 16, 195–214. [Google Scholar] [CrossRef]
- Vonarbourg, A.; Passirani, C.; Saulnier, P.; Benoit, J.-P. Parameters influencing the stealthiness of colloidal drug delivery systems. Biomaterials 2006, 27, 4356–4373. [Google Scholar] [CrossRef]
- Huang, Z.-Y.; Hunter, S.; Chien, P.; Kim, M.-K.; Han-Kim, T.-H.; Indik, Z.K.; Schreiber, A.D. Interaction of Two Phagocytic Host Defense Systems. J. Biol. Chem. 2011, 286, 160–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Furumoto, K.; Nagayama, S.; Ogawara, K.-I.; Takakura, Y.; Hashida, M.; Higaki, K.; Kimura, T. Hepatic uptake of negatively charged particles in rats: Possible involvement of serum proteins in recognition by scavenger receptor. J. Control. Release 2004, 97, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Owens, D.E.; Peppas, N.A. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int. J. Pharm. 2006, 307, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Passirani, C.; Barratt, G.; Devissaguet, J.P.; Labarre, D. Long-circulating nanoparticles bearing heparin or dextran covalently bound to poly(methyl methacrylate). Pharm. Res. 1998, 15, 1046–1050. [Google Scholar] [CrossRef]
- Allen, T.M.; Hansen, C.; Rutledge, J. Liposomes with prolonged circulation times: Factors affecting uptake by reticuloendothelial and other tissues. Biochim. Biophys. Acta (BBA) Biomembr. 1989, 981, 27–35. [Google Scholar] [CrossRef]
- Ishida, T.; Ichihara, M.; Wang, X.; Kiwada, H. Spleen plays an important role in the induction of accelerated blood clearance of PEGylated liposomes. J. Control. Release 2006, 115, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Bertholon, I.; Vauthier, C.; Labarre, D. Complement Activation by Core–Shell Poly(isobutylcyanoacrylate)–Polysaccharide Nanoparticles: Influences of Surface Morphology, Length, and Type of Polysaccharide. Pharm. Res. 2006, 23, 1313–1323. [Google Scholar] [CrossRef]
- Hong, R.L.; Huang, C.J.; Tseng, Y.L.; Pang, V.F.; Chen, S.T.; Liu, J.J.; Chang, F.H. Direct comparison of liposomal doxorubicin with or without polyethylene glycol coating in C-26 tumor-bearing mice: Is surface coating with polyethylene glycol beneficial? Clin. Cancer Res. 1999, 5, 3645–3652. [Google Scholar]
- Holland, J.W.; Hui, C.; Cullis, P.R.; Madden, T.D. Poly(ethylene glycol)−Lipid Conjugates Regulate the Calcium-Induced Fusion of Liposomes Composed of Phosphatidylethanolamine and Phosphatidylserine †. Biochemistry 1996, 35, 2618–2624. [Google Scholar] [CrossRef] [PubMed]
- Erbacher, P.; Bettinger, T.; Belguise-Valladier, P.; Zou, S.; Coll, J.L.; Behr, J.P.; Remy, J.S. Transfection and physical properties of various saccharide, poly(ethylene glycol), and antibody-derivatized polyethylenimines (PEI). J. Gene Med. 1999, 1, 210–222. [Google Scholar] [CrossRef]
- Yamada, T.; Iwasaki, Y.; Tada, H.; Iwabuki, H.; Chuah, M.K.L.; VandenDriessche, T.; Fukuda, H.; Kondo, A.; Ueda, M.; Seno, M.; et al. Nanoparticles for the delivery of genes and drugs to human hepatocytes. Nat. Biotechnol. 2003, 21, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Somiya, M.; Kuroda, S. Development of a virus-mimicking nanocarrier for drug delivery systems: The bio-nanocapsule. Adv. Drug Deliv. Rev. 2015, 95, 77–89. [Google Scholar] [CrossRef]
- Neurath, A.; Kent, S.; Strick, N.; Parker, K. Identification and chemical synthesis of a host cell receptor binding site on hepatitis B virus. Cell 1986, 46, 429–436. [Google Scholar] [CrossRef]
- Schulze, A.; Schieck, A.; Ni, Y.; Mier, W.; Urban, S. Fine Mapping of Pre-S Sequence Requirements for Hepatitis B Virus Large Envelope Protein-Mediated Receptor Interaction. J. Virol. 2009, 84, 1989–2000. [Google Scholar] [CrossRef] [Green Version]
- Yan, H.; Zhong, G.; Xu, G.; He, W.; Jing, Z.; Gao, Z.; Huang, Y.; Qi, Y.; Peng, B.; Wang, H.; et al. Sodium taurocholate cotransporting polypeptide is a functional receptor for human hepatitis B and D virus. eLife 2012, 1, e00049. [Google Scholar] [CrossRef]
- Machida, A.; Kishimoto, S.; Ohnuma, H.; Baba, K.; Ito, Y.; Miyamoto, H.; Funatsu, G.; Oda, K.; Usuda, S.; Togami, S. A polypep-tide containing 55 amino acid residues coded by the pre-S region of hepatitis B virus deoxyribonucleic acid bears the receptor for polymerized human as well as chimpanzee albumins. Gastroenterology 1984, 86, 910–918. [Google Scholar]
- Matsuura, Y.; Yagi, H.; Matsuda, S.; Itano, O.; Aiura, K.; Kuroda, S.; Ueda, M.; Kitagawa, Y. Human Liver-Specific Nanocarrier in a Novel Mouse Xenograft Model Bearing Noncancerous Human Liver Tissue. Eur. Surg. Res. 2011, 46, 65–72. [Google Scholar] [CrossRef]
- Ueda, M.; Iwasaki, Y.; Yamada, T.; Kondo, A.; Seno, M.; Tanizawa, K.; Kuroda, S.; Sakamoto, M.; Kitajima, M. Erratum: Gene therapy of liver tumors with human liver-specific nanoparticles. Cancer Gene Ther. 2007, 14, 440. [Google Scholar] [CrossRef]
- Kuroda, S.; Liu, Q.; Jung, J.; Iijima, M.; Yoshimoto, N.; Niimi, T.; Maturana, A.D.; Shin, S.H.; Jeong, S.-Y.; Choi, E.K.; et al. Virosomes of hepatitis B virus envelope L proteins containing doxorubicin: Synergistic enhancement of human liver-specific antitumor growth activity by radiotherapy. Int. J. Nanomed. 2015, 10, 4159–4172. [Google Scholar] [CrossRef] [Green Version]
- Ogawara, K.-I.; Furumoto, K.; Nagayama, S.; Minato, K.; Higaki, K.; Kai, T.; Kimura, T. Pre-coating with serum albumin reduces receptor-mediated hepatic disposition of polystyrene nanosphere: Implications for rational design of nanoparticles. J. Control. Release 2004, 100, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Elsadek, B.; Kratz, F. Impact of albumin on drug delivery—New applications on the horizon. J. Control. Release 2012, 157, 4–28. [Google Scholar] [CrossRef] [PubMed]
- Elzoghby, A.O.; Samy, W.M.; Elgindy, N.A. Albumin-based nanoparticles as potential controlled release drug delivery systems. J. Control. Release 2012, 157, 168–182. [Google Scholar] [CrossRef]
- Kasuya, T.; Jung, J.; Kinoshita, R.; Goh, Y.; Matsuzaki, T.; Iijima, M.; Yoshimoto, N.; Tanizawa, K.; Kuroda, S. Bio-Nanocapsule–Liposome Conjugates for In Vivo Pinpoint Drug and Gene Delivery. In Methods in Enzymology; Elsevier Inc.: Amsterdam, The Netherlands, 2009; Volume 464, pp. 147–166. ISBN 9780123749697. [Google Scholar]
- Tabor, E.; Buynak, E.; Smallwood, L.A.; Snoy, P.; Gerety, R.J. Inactivation of Hepatitis B Virus by Three Methods: Treatment With Pepsin, Urea, or Formalin. J. Med. Virol. 1983, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Milich, D.R.; Papas, E.D.; Bhatnagar, P.K.; Vyas, G.N. Interactions between polymerized human albumin, hepatitis B surface antigen, and complement: I. Binding of polyalbumin to Clq. J. Med. Virol. 1981, 7, 181–192. [Google Scholar] [CrossRef]
- Dash, S.; Rao, K.V.; Joshi, B.; Nayak, N.C.; Panda, S.K. Significance of natural polymerized albumin and its receptor in hepatitis B infection of hepatocytes. Hepatology 1991, 13, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Iwabuki, H.; Kanno, T.; Tanaka, H.; Kawai, T.; Fukuda, H.; Kondo, A.; Seno, M.; Tanizawa, K.; Kuroda, S. Physicochemical and immunological characterization of hepatitis B virus envelope particles exclusively consisting of the entire L (pre-S1+pre-S2+S) protein. Vaccine 2001, 19, 3154–3163. [Google Scholar] [CrossRef]
- Imai, M.; Yanase, Y.; Nojiri, T.; Miyakawa, Y.; Mayumi, M. A receptor for polymerized human and chimpanzee albumins on hepatitis B virus particles co-occurring with HBeAg. Gastroenterology 1979, 76, 242–247. [Google Scholar] [CrossRef]
- Itoh, Y.; Kuroda, S.; Miyazaki, T.; Otaka, S.; Fujisawa, Y. Identification of polymerized-albumin receptor domain in the pre-S2 region of hepatitis B virus surface antigen M protein. J. Biotechnol. 1992, 23, 71–82. [Google Scholar] [CrossRef]
- Bertrand, N.; Grenier, P.; Mahmoudi, M.; Lima, E.M.; Appel, E.A.; Dormont, F.; Lim, J.-M.; Karnik, R.; Langer, R.; Farokhzad, O.C. Mechanistic understanding of in vivo protein corona formation on polymeric nanoparticles and impact on pharmacokinetics. Nat. Commun. 2017, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tenzer, S.; Docter, D.; Kuharev, J.; Musyanovych, A.; Fetz, V.; Hecht, R.; Schlenk, F.; Fischer, D.; Kiouptsi, K.; Reinhardt, C.; et al. Rapid formation of plasma protein corona critically affects nanoparticle pathophysiology. Nat. Nanotechnol. 2013, 8, 772–781. [Google Scholar] [CrossRef] [PubMed]
- García-Álvarez, R.; Vallet-Regí, M. Hard and Soft Protein Corona of Nanomaterials: Analysis and Relevance. Nanomaterials 2021, 11, 888. [Google Scholar] [CrossRef] [PubMed]
- Takami, M.; Kasuya, I.; Tsunoo, H. Polymerized albumin receptor on rat liver cells. J. Biochem. 1992, 111, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Akilesh, S.; Christianson, G.J.; Roopenian, D.C.; Shaw, A.S. Neonatal FcR Expression in Bone Marrow-Derived Cells Functions to Protect Serum IgG from Catabolism. J. Immunol. 2007, 179, 4580–4588. [Google Scholar] [CrossRef] [Green Version]
- Stork, R.; Campigna, E.; Robert, B.; Müller, D.; Kontermann, R.E. Biodistribution of a Bispecific Single-chain Diabody and Its Half-life Extended Derivatives. J. Biol. Chem. 2009, 284, 25612–25619. [Google Scholar] [CrossRef] [Green Version]
- Chaudhury, C.; Brooks, C.L.; Carter, D.C.; Robinson, J.M.; Anderson, C.L. Albumin Binding to FcRn: Distinct from the FcRn−IgG Interaction. Biochemistry 2006, 45, 4983–4990. [Google Scholar] [CrossRef]
- Jung, J.; Iijima, M.; Yoshimoto, N.; Sasaki, M.; Niimi, T.; Tatematsu, K.; Jeong, S.-Y.; Choi, E.K.; Tanizawa, K.; Kuroda, S. Efficient and rapid purification of drug- and gene-carrying bio-nanocapsules, hepatitis B virus surface antigen L particles, from Saccharomyces cerevisiae. Protein Expr. Purif. 2011, 78, 149–155. [Google Scholar] [CrossRef]
- Kuroda, S.; Otaka, S.; Miyazaki, T.; Nakao, M.; Fujisawa, Y. Hepatitis B virus envelope L protein particles. Synthesis and assembly in Saccharomyces cerevisiae, purification and characterization. J. Biol. Chem. 1992, 267, 1953–1961. [Google Scholar] [CrossRef]
- Schreiber, R.; Taschler, U.; Wolinski, H.; Seper, A.; Tamegger, S.N.; Graf, M.; Kohlwein, S.D.; Haemmerle, G.; Zimmermann, R.; Zechner, R.; et al. Esterase 22 and beta-glucuronidase hydrolyze retinoids in mouse liver. J. Lipid Res. 2009, 50, 2514–2523. [Google Scholar] [CrossRef] [Green Version]
- Iijima, M.; Kadoya, H.; Hatahira, S.; Hiramatsu, S.; Jung, G.; Martin, A.; Quinn, J.; Jung, J.; Jeong, S.-Y.; Choi, E.K.; et al. Nanocapsules incorporating IgG Fc-binding domain derived from Staphylococcus aureus protein A for displaying IgGs on immunosensor chips. Biomaterials 2011, 32, 1455–1464. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Matsuo, H.; Yoshimoto, N.; Iijima, M.; Niimi, T.; Jung, J.; Jeong, S.-Y.; Choi, E.K.; Sewaki, T.; Arakawa, T. Engineered hepatitis B virus surface antigen L protein particles for in vivo active targeting of splenic dendritic cells. Int. J. Nanomed. 2012, 7, 3341–3350. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| Sample | Z-Average (nm) | PDI | ζ-Potential (mV) |
|---|---|---|---|
| LP | 151 | 0.318 | –74.8 |
| BNC | 70.8 | 0.186 | –15.6 |
| BNC-LP | 157 | 0.356 | –43.5 |
| Albumin | Albumin/L Protein (mol ratio) N = 4 | Albumin/BNC (mol ratio) * N = 3 |
|---|---|---|
| HSA | 0 | 0 |
| MSA | 0 | 0 |
| pHSA | 0.053 ± 0.017 | 5.820 ± 1.838 |
| pMSA | 0.011 ± 0.007 | 1.174 ± 0.741 |
| Microspheres | Z-Average (nm) | PDI | ζ-Potential (mV) |
|---|---|---|---|
| Naked | 81.0 | 0.019 | –53.6 |
| PEG | 95.2 | 0.186 | –45.9 |
| HSA | 120 | 0.120 | –31.3 |
| MSA | 102 | 0.019 | –29.3 |
| Peptide 2 | 78.0 | 0.010 | –54.7 |
| STI | 106 | 0.127 | –25.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takagi, K.; Somiya, M.; Jung, J.; Iijima, M.; Kuroda, S. Polymerized Albumin Receptor of Hepatitis B Virus for Evading the Reticuloendothelial System. Pharmaceuticals 2021, 14, 408. https://doi.org/10.3390/ph14050408
Takagi K, Somiya M, Jung J, Iijima M, Kuroda S. Polymerized Albumin Receptor of Hepatitis B Virus for Evading the Reticuloendothelial System. Pharmaceuticals. 2021; 14(5):408. https://doi.org/10.3390/ph14050408
Chicago/Turabian StyleTakagi, Kurumi, Masaharu Somiya, Joohee Jung, Masumi Iijima, and Shun’ichi Kuroda. 2021. "Polymerized Albumin Receptor of Hepatitis B Virus for Evading the Reticuloendothelial System" Pharmaceuticals 14, no. 5: 408. https://doi.org/10.3390/ph14050408