Association between Body Mass Index, Waist-to-Height Ratio and Adiposity in Children: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of the Studies
3.2. Quantitative Meta-Analysis
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| AUC | area under the curve |
| BF | body fat |
| %BF | body fat percentage |
| BMI | body mass index |
| DEXA | dual-energy X-ray absorptiometry |
| FMI | fat mass index |
| NHANES | national health and nutrition examination survey |
| r | correlation coefficient |
| R2 | coefficient of determination |
| WtHr | waist to height ratio |
| WC | waist circumference |
| 95% CI | 95% confidence interval |
References
- WHO. Obesity and Overweight. Fact Sheet. 2015. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 4 May 2016).
- Dietz, W.H. Health consequences of obesity in youth: Childhood predictors of adult disease. Pediatrics 1998, 101, 518–525. [Google Scholar] [PubMed]
- Gurnani, M.; Birken, C.; Hamilton, J. Childhood obesity: Causes, consequences, and management. Pediatr. Clin. N. Am. 2015, 62, 821–840. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.R. The consequences of childhood overweight and obesity. Future Child 2006, 16, 47–67. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.R.; Greer, F.R. Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics 2008, 122, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Deckelbaum, R.J.; Williams, C.L. Childhood obesity: The health issue. Obes. Res. 2001, 9, 239S–243S. [Google Scholar] [CrossRef] [PubMed]
- Twig, G.; Yaniv, G.; Levine, H.; Leiba, A.; Goldberger, N.; Derazne, E.; Ben-Ami, S.D.; Tzur, D.; Afek, A.; Shamiss, A.; et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 2016, 374, 2430–2440. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Hyder, M.L.; Poston, W.S. Childhood overweight: An expanding problem. Treat Endocrinol. 2003, 2, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Roberts, E.A. Non-alcoholic steatohepatitis in children. Clin. Liver Dis. 2007, 11, 155–172. [Google Scholar] [CrossRef] [PubMed]
- Shypailo, R.J.; Butte, N.F.; Ellis, K.J. DXA: Can it be used as a criterion reference for body fat measurements in children? Obesity 2008, 16, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Faith, M.S.; Allison, D.B.; Gallagher, D.; Chiumello, G.; Heymsfield, S.B. Body mass index as a measure of adiposity among children and adolescents: A validation study. J. Pediatr. 1998, 132, 204–210. [Google Scholar] [CrossRef]
- Jensen, N.S.; Camargo, T.F.; Bergamaschi, D.P. Comparison of methods to measure body fat in 7-to-10-year-old children: A systematic review. Public Health 2016, 133, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Field, A.E.; Laird, N.; Steinberg, E.; Fallon, E.; Semega-Janneh, M.; Yanovski, J.A. Which metric of relative weight best captures body fatness in children? Obes. Res. 2003, 11, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.R.; Jacobson, M.S.; McCrindle, B.W.; Eckel, R.H.; Sanner, B.M. American Heart Association Childhood Obesity Research Summit Report. Circulation 2009, 119, e489–e517. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Mei, Z.; Srinivasan, S.R.; Berenson, G.S.; Dietz, W.H. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J. Pediatr. 2007, 150, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Demerath, E.W.; Schubert, C.M.; Maynard, L.M.; Sun, S.S.; Chumlea, W.C.; Pickoff, A.; Czerwinski, S.A.; Towne, B.; Siervogel, R.M. Do changes in body mass index percentile reflect changes in body composition in children? Data from the Fels Longitudinal Study. Pediatrics 2006, 117, e487–e495. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Wang, J.; Maynard, L.M.; Thornton, J.C.; Mei, Z.; Pierson, R.N.; Dietz, W.H.; Horlick, M. Relation of BMI to fat and fat-free mass among children and adolescents. Int. J. Obes. 2005, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, P.; Bedogni, G.; Moreno, L.A.; Goran, M.I.; Gutin, B.; Fox, K.R.; Peters, D.M.; Barbeau, P.; de Simone, M.; Pietrobelli, A. Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children. Int. J. Obes. 2006, 30, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Despres, J.P.; Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 2006, 444, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Savva, S.C.; Tornaritis, M.; Savva, M.E.; Kourides, Y.; Panagi, A.; Silikiotou, N.; Georgiou, C.; Kafatos, A. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1453–1458. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, R.; Gheiratmand, R.; Ardalan, G.; Adeli, K.; Gouya, M.M.; Razaghi, E.M.; Majdzadeh, R.; Delavari, A.; Shariatinejad, K.; Motaghian, M.; et al. Association of anthropometric indices with cardiovascular disease risk factors among children and adolescents: CASPIAN Study. Int. J. Cardiol. 2007, 117, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Department of Preventive Medicine and Public Health. University of Navarre. Available online: http://www.unav.edu/departamento/preventiva/publicaciones (accessed on 16 May 2016).
- Welch, V.; Petticrew, M.; Petkovic, J.; Moher, D.; Waters, E.; White, H.; Tugwell, P. Extending the PRISMA statement to equity-focused systematic reviews (PRISMA-E 2012): Explanation and elaboration. Int. J. Equity Health 2015, 14, 92. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Rutjes, A.W.; Reitsma, J.B.; Bossuyt, P.M.; Kleijnen, J. The development of QUADAS: A tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med. Res. Methodol. 2003, 3, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karlsson, A.K.; Kullberg, J.; Stokland, E.; Allvin, K.; Gronowitz, E.; Svensson, P.A.; Dahlgren, J. Measurements of total and regional body composition in preschool children: A comparison of MRI, DXA, and anthropometric data. Obesity 2013, 21, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- De Miguel-Etayo, P.; Moreno, L.A.; Santabarbara, J.; Martin-Matillas, M.; Piqueras, M.J.; Rocha-Silva, D.; del Moral, A.M.; Campoy, C.; Marcos, A.; Garagorri, J.M. Anthropometric indices to assess body-fat changes during a multidisciplinary obesity treatment in adolescents: EVASYON Study. Clin. Nutr. 2015, 34, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Barreira, T.V.; Broyles, S.T.; Gupta, A.K.; Katzmarzyk, P.T. Relationship of anthropometric indices to abdominal and total body fat in youth: Sex and race differences. Obesity 2014, 22, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, P.; Bedogni, G.; Heo, M.; Pietrobelli, A. Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int. J. Obes. 2013, 37, 943–946. [Google Scholar] [CrossRef] [PubMed]
- Tuan, N.T.; Wang, Y. Adiposity assessments: Agreement between dual-energy X-ray absorptiometry and anthropometric measures in U.S. children. Obesity 2014, 22, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gomez, D.; Gomez-Martinez, S.; Puertollano, M.A.; Nova, E.; Warnberg, J.; Veiga, O.L.; Martí, A.; Campoy, C.; Garagorri, J.M.; Azcona, C.; et al. Design and evaluation of a treatment programme for Spanish adolescents with overweight and obesity. The EVASYON Study. BMC Public Health 2009, 9, 414. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Ogden, C.L.; Yanovski, J.A.; Freedman, D.S.; Shepherd, J.A.; Graubard, B.I.; Borrud, L.G. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am. J. Clin. Nutr. 2010, 91, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Puder, J.; Zahner, L.; Roth, R.; Meyer, U.; Bedogni, G. Estimation of percentage body fat in 6- to 13-year-old children by skinfold thickness, body mass index and waist circumference. Br. J. Nutr. 2010, 104, 1565–1572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedogni, G.; Iughetti, L.; Ferrari, M.; Malavolti, M.; Poli, M.; Bernasconi, S.; Battistini, N. Sensitivity and specificity of body mass index and skinfold thicknesses in detecting excess adiposity in children aged 8–12 years. Ann. Hum. Biol. 2003, 30, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.G.; Going, S.B. Body composition assessment for development of an international growth standard for preadolescent and adolescent children. Food Nutr. Bull. 2006, 27, S314–S325. [Google Scholar] [CrossRef] [PubMed]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Burch, J.; Llewellyn, A.; Griffiths, C.; Yang, H.; Owen, C.; Duffy, S.; Woolacott, N. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: A systematic review and meta-analysis. Health Technol. Assess. 2015, 19, 1–336. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Ogden, C.L.; Blanck, H.M.; Borrud, L.G.; Dietz, W.H. The abilities of body mass index and skinfold thicknesses to identify children with low or elevated levels of dual-energy X-ray absorptiometry-determined body fatness. J. Pediatr. 2013, 163, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Steinberger, J.; Jacobs, D.R.; Raatz, S.; Moran, A.; Hong, C.P.; Sinaiko, A.R. Comparison of body fatness measurements by BMI and skinfolds vs. dual energy X-ray absorptiometry and their relation to cardiovascular risk factors in adolescents. Int. J. Obes. 2005, 29, 1346–1352. [Google Scholar] [CrossRef] [PubMed]
- Kahn, H.S.; Imperatore, G.; Cheng, Y.J. A population-based comparison of BMI percentiles and waist-to-height ratio for identifying cardiovascular risk in youth. J. Pediatr. 2005, 146, 482–488. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, H.D.; Ashwell, M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message—‘Keep your waist circumference to less than half your height’. Int. J. Obes. 2006, 30, 988–992. [Google Scholar] [CrossRef] [PubMed]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [PubMed]
- Fujita, Y.; Kouda, K.; Nakamura, H.; Iki, M. Cut-off values of body mass index, waist circumference, and waist-to-height ratio to identify excess abdominal fat: Population-based screening of Japanese school children. J. Epidemiol. 2011, 21, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.W.; Williams, S.M.; Grant, A.M.; Taylor, B.J.; Goulding, A. Predictive ability of waist-to-height in relation to adiposity in children is not improved with age and sex-specific values. Obesity 2011, 19, 1062–1068. [Google Scholar] [CrossRef] [PubMed]
- Brannsether, B.; Roelants, M.; Bjerknes, R.; Juliusson, P.B. Waist circumference and waist-to-height ratio in Norwegian children 4–18 years of age: Reference values and cut-off levels. Acta Paediatr. 2011, 100, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Roswall, J.; Bergman, S.; Almqvist-Tangen, G.; Alm, B.; Niklasson, A.; Nierop, A.F.; Dahlgren, J. Population-based waist circumference and waist-to-height ratio reference values in preschool children. Acta Paediatr. 2009, 98, 1632–1636. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]




| Authors (Year) | Design | Simple Characteristics | Age (Years) | Mean %BF (SD) | Fat Mass Assessment | BMI or WtHr | Results * | Other Findings | ||
|---|---|---|---|---|---|---|---|---|---|---|
| R2 (95%CI) | Beta Coefficient | AUC | ||||||||
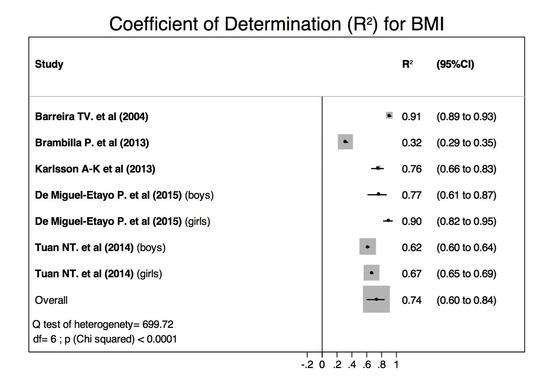
| Barreira, T.V., et al. (2014) [27] | Cross-sectional | N = 382; 180 boys (84 African Americans (AA) & 96 Whites) and 202 girls (118 AA & 84 Whites). | 5–18 | Boys: Whites: 24.0 (9.1) AA: 24.0 (10.0) Girls: Whites: 31.1 (8.4) AA: 31.8 (9.6) | Total fat mass (kg) | BMI | 0.91 (0.89–0.93) | Significant linear relationship | No significant interaction with race or sex. | |
| WtHr | 0.69 (0.64–0.74) | Significant linear relationship | Significant interaction race and sex. | |||||||
| Brambilla, P., et al. (2013) [28] | Cross-sectional (US-NHANES 2003–2004) | N= 2339; 1221 boys (326 Whites, 453 Blacks, 373 Mexicans, 69 other races) & 1118 girls (321 Whites, 387 Blacks, 348 Mexicans, 62 other races). | 8–18 | Whites: 29.0 (7.7) Blacks: 26.0 (8.3) Mexicans: 29.8 (7.7) Others: 28.3 (7.8) | %BF | BMI | 0.32 (0.29–0.35) (unadjusted) 0.68 (age & sex) 0.70 (age, sex & race) | Found no practical advantage to add the ethnic group as further predictor in the model. | ||
| WtHr | 0.64 (0.62–0.66) (unadjusted) 0.80 (age & sex) 0.80 (age, sex & race) | |||||||||
| Karlsson, A.-K., et al. (2013) [25] | Cross-sectional | N = 100; 55 boys and 45 girls, moderately preterm at birth. | 4.9–5.2 | Boys: 17 (6) Girls: 21 (6) | Total fat mass (kg) | BMI | 0.76 (0.66–0.83) | |||
| WtHr | 0.55 (0.41–0.67) | |||||||||
| De Miguel-Etayo, P., et al. (2015) [26] | Longitudinal (EVASYON treatment program) [30] | N = 83; 43 boys and 40 girls, overweight or obese [32] | 13–16 | Boys: 33.3 (31.5–35.1) Girls: 39.9 (37.9–41.9) | Changes in FMI. | Changes in BMI | Boys: 0.77 (0.61–0.87) Girls: 0.90 (0.82–0.95) | Boys: 0.68, Girls: 0.66 (unadjusted) Boys: 0.68, Girls: 0.66 (age) Boys: 0.68, Girls: 0.65 (age and Tanner) | ||
| Changes in WtHr | Boys: 0.50 (0.27–0.70) Girls: 0.49 (0.24–0.69) | Boys: 33.91, Girls: 19.04 (crude model) Boys: 33.57, Girls: 18.37 (age) Boys: 33.61, Girls: 18.53 (age and Tanner) | ||||||||
| Tuan, N.T., et al. (2014) [29] | Cross-sectional (US-NHANES 2001–2004) | N= 5355; 2792 boys (796 Whites, 962 Blacks, 818 Mexicans, 216 other races) & 2563 girls (742 Whites, 809 Blacks, 809 Mexicans, 203 other races). | 8–19 | Boys: Whites: 25.7 (0.5) Blacks: 22.8 (0.2) Mexican: 27.3 (0.3) Girls: Whites: 32.5 (0.4) Blacks: 31.5 (0.3) Mexican: 33.7 (0.3) | z-score of the %BF Obesity was defined as %BF by DEXA > 75th age & sex specific percentile (26%–33% in boys & 36%–38% in girls) [31]. | z-score of the BMI | Boys: 0.62 (0.60–0.64) Girls: 0.67 (0.65-0.69) | Boys: 0.79 Girls: 0.82 (z-BMI) (all races) | Boys: 0.91 Girls: 0.90 (all races) | Kappa + Boys: 0.59 Girls: 0.60 (all races) Sex and ethnicity-race variations. |
| z-score of the WtHr | Boys: 0.73 (0.71–0.75) Girls: 0.70 (0.68–0.72) | Boys: 0.86 Girls: 0.84 (z-WtHr) (all races) | Boys: 0.97 Girls: 0.94 (all races) | Kappa + Boys: 0.71 Girls: 0.64 (all races) Sex and ethnicity-race variations. | ||||||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin-Calvo, N.; Moreno-Galarraga, L.; Martinez-Gonzalez, M.A. Association between Body Mass Index, Waist-to-Height Ratio and Adiposity in Children: A Systematic Review and Meta-Analysis. Nutrients 2016, 8, 512. https://doi.org/10.3390/nu8080512
Martin-Calvo N, Moreno-Galarraga L, Martinez-Gonzalez MA. Association between Body Mass Index, Waist-to-Height Ratio and Adiposity in Children: A Systematic Review and Meta-Analysis. Nutrients. 2016; 8(8):512. https://doi.org/10.3390/nu8080512
Chicago/Turabian StyleMartin-Calvo, Nerea, Laura Moreno-Galarraga, and Miguel Angel Martinez-Gonzalez. 2016. "Association between Body Mass Index, Waist-to-Height Ratio and Adiposity in Children: A Systematic Review and Meta-Analysis" Nutrients 8, no. 8: 512. https://doi.org/10.3390/nu8080512