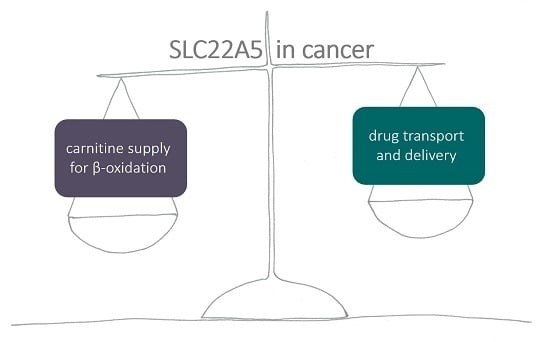
SLC22A5 (OCTN2) Carnitine Transporter—Indispensable for Cell Metabolism, a Jekyll and Hyde of Human Cancer
Abstract
:1. Introduction
2. Carnitine Transporters
3. SLC22A5 Regulation
4. SLC22A5 Pharmacological Implications
5. SLC22A5 and Fatty Acid Oxidation in the Brain
6. SLC22A5 and Fatty Acid Oxidation in Cancer
Author Contributions
Funding
Conflicts of Interest
References
- Tein, I. Disorders of fatty acid oxidation. Handb. Clin. Neurol. 2013, 113, 1675–1688. [Google Scholar] [PubMed]
- Wanders, R.J.; Waterham, H.R. Biochemistry of mammalian peroxisomes revisited. Annu. Rev. Biochem. 2006, 75, 295–332. [Google Scholar] [CrossRef] [PubMed]
- Theodoulou, F.L.; Holdsworth, M.; Baker, A. Peroxisomal ABC transporters. FEBS Lett. 2006, 580, 1139–1155. [Google Scholar] [CrossRef] [Green Version]
- Palmieri, L.; Rottensteiner, H.; Girzalsky, W.; Scarcia, P.; Palmieri, F.; Erdmann, R. Identification and functional reconstitution of the yeast peroxisomal adenine nucleotide transporter. EMBO J. 2001, 20, 5049–5059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Vinas, E.; Bentebibel, A.; Gurunathan, C.; Morillas, M.; de Arriaga, D.; Serra, D.; Asins, G.; Hegardt, F.G.; Gomez-Puertas, P. Definition by functional and structural analysis of two malonyl-CoA sites in carnitine palmitoyltransferase 1A. J. Biol. Chem. 2007, 282, 18212–18224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerner, J.; Hoppel, C. Fatty acid import into mitochondria. Biochim. Biophys. Acta 2000, 1486, 1–17. [Google Scholar] [CrossRef]
- Faye, A.; Esnous, C.; Price, N.T.; Onfray, M.A.; Girard, J. Prip-Buus C: Rat liver carnitine palmitoyltransferase 1 forms an oligomeric complex within the outer mitochondrial membrane. J. Biol. Chem. 2007, 282, 26908–26916. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.; Kerner, J.; Hoppel, C.L. Mitochondrial carnitine palmitoyltransferase 1a (CPT1a) is part of an outer membrane fatty acid transfer complex. J. Biol. Chem. 2011, 286, 25655–25662. [Google Scholar] [CrossRef] [Green Version]
- Indiveri, C.; Tonazzi, A.; Palmieri, F. Identification and purification of the carnitine carrier from rat liver mitochondria. Biochim. Biophys. Acta 1990, 1020, 81–86. [Google Scholar] [CrossRef]
- Indiveri, C.; Iacobazzi, V.; Tonazzi, A.; Giangregorio, N.; Infantino, V.; Convertini, P.; Console, L.; Palmieri, F. The mitochondrial carnitine/acylcarnitine carrier: Function, structure and physiopathology. Mol. Aspects. Med. 2011, 32, 223–233. [Google Scholar] [CrossRef]
- Ramsay, R.R. The role of the carnitine system in peroxisomal fatty acid oxidation. Am. J. Med. Sci. 1999, 318, 28–35. [Google Scholar] [CrossRef]
- Januszewicz, E.; Pajak, B.; Gajkowska, B.; Samluk, L.; Djavadian, R.L.; Hinton, B.T.; Nalecz, K.A. Organic cation/carnitine transporter OCTN3 is present in astrocytes and is up-regulated by peroxisome proliferators-activator receptor agonist. Int. J. Biochem. Cell Biol. 2009, 41, 2599–2609. [Google Scholar] [CrossRef] [PubMed]
- Vaz, F.M.; Wanders, R.J. Carnitine biosynthesis in mammals. Biochem. J. 2002, 361, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Van Vlies, N.; Wanders, R.J.; Vaz, F.M. Measurement of carnitine biosynthesis enzyme activities by tandem mass spectrometry: Differences between the mouse and the rat. Anal. Biochem. 2006, 354, 132–139. [Google Scholar] [CrossRef]
- Steiber, A.; Kerner, J.; Hoppel, C.L. Carnitine: A nutritional, biosynthetic, and functional perspective. Mol. Aspects Med. 2004, 25, 455–473. [Google Scholar] [CrossRef]
- Indiveri, C.; Giangregorio, N.; Iacobazzi, V.; Palmieri, F. Site-directed mutagenesis and chemical modification of the six native cysteine residues of the rat mitochondrial carnitine carrier: Implications for the role of cysteine-136. Biochemistry 2002, 41, 8649–8656. [Google Scholar] [CrossRef]
- Tamai, I.; Ohashi, R.; Nezu, J.I.; Sai, Y.; Kobayashi, D.; Oku, A.; Shimane, M.; Tsuji, A. Molecular and functional characterization of organic cation/carnitine transporter family in mice. J. Biol. Chem. 2000, 275, 40064–40072. [Google Scholar] [CrossRef] [Green Version]
- Lamhonwah, A.M.; Ackerley, C.A.; Tilups, A.; Edwards, V.D.; Wanders, R.J.; Tein, I. OCTN3 is a mammalian peroxisomal membrane carnitine transporter. Biochem. Biophy. Res. Co. 2005, 338, 1966–1972. [Google Scholar] [CrossRef]
- Lamhonwah, A.M.; Hawkins, C.E.; Tam, C.; Wong, J.; Mai, L.; Tein, I. Expression patterns of the organic cation/carnitine transporter family in adult murine brain. Brain Dev. 2008, 30, 31–42. [Google Scholar] [CrossRef]
- Enomoto, A.; Wempe, M.F.; Tsuchida, H.; Shin, H.J.; Cha, S.H.; Anzai, N.; Goto, A.; Sakamoto, A.; Niwa, T.; Kanai, Y.; et al. Molecular identification of a novel carnitine transporter specific to human testis. Insights into the mechanism of carnitine recognition. J. Biol. Chem. 2002, 277, 36262–36271. [Google Scholar] [CrossRef] [Green Version]
- Nakanishi, T.; Hatanaka, T.; Huang, W.; Prasad, P.D.; Leibach, F.H.; Ganapathy, M.E.; Ganapathy, V. Na+- and Cl--coupled active transport of carnitine by the amino acid transporter ATB(0,+) from mouse colon expressed in HRPE cells and Xenopus oocytes. J. Physiol. 2001, 532, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Tamai, I.; Ohashi, R.; Nezu, J.; Yabuuchi, H.; Oku, A.; Shimane, M.; Sai, Y.; Tsuji, A. Molecular and functional identification of sodium ion-dependent, high affinity human carnitine transporter OCTN2. J. Biol. Chem. 1998, 273, 20378–20382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.; Prasad, P.D.; Leibach, F.H.; Ganapathy, V. cDNA sequence, transport function, and genomic organization of human OCTN2, a new member of the organic cation transporter family. Biochem. Biophy. Res. Co. 1998, 246, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Januszewicz, E.; Bekisz, M.; Mozrzymas, J.W.; Nalecz, K.A. High affinity carnitine transporters from OCTN family in neural cells. Neurochem. Res. 2010, 35, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Indiveri, C.; Iacobazzi, V.; Giangregorio, N.; Palmieri, F. The mitochondrial carnitine carrier protein: cDNA cloning, primary structure and comparison with other mitochondrial transport proteins. Biochem. J. 1997, 321, 713–719. [Google Scholar] [CrossRef] [Green Version]
- Lamhonwah, A.M.; Skaug, J.; Scherer, S.W.; Tein, I. A third human carnitine/organic cation transporter (OCTN3) as a candidate for the 5q31 Crohn’s disease locus (IBD5). Biochem. Biophy. Res. Co. 2003, 301, 98–101. [Google Scholar] [CrossRef]
- Sloan, J.L.; Mager, S. Cloning and functional expression of a human Na(+) and Cl(-)-dependent neutral and cationic amino acid transporter B(0+). J. Biol. Chem. 1999, 274, 23740–23745. [Google Scholar] [CrossRef] [Green Version]
- Kido, Y.; Tamai, I.; Ohnari, A.; Sai, Y.; Kagami, T.; Nezu, J.; Nikaido, H.; Hashimoto, N.; Asano, M.; Tsuji, A. Functional relevance of carnitine transporter OCTN2 to brain distribution of l-carnitine and acetyl-l-carnitine across the blood- brain barrier. J. Neurochem. 2001, 79, 959–969. [Google Scholar] [CrossRef]
- Berezowski, V.; Miecz, D.; Marszalek, M.; Broer, A.; Broer, S.; Cecchelli, R.; Nalecz, K.A. Involvement of OCTN2 and B0,+ in the transport of carnitine through an in vitro model of the blood-brain barrier. J. Neurochem. 2004, 91, 860–872. [Google Scholar] [CrossRef]
- Michalec, K.; Mysiorek, C.; Kuntz, M.; Berezowski, V.; Szczepankiewicz, A.A.; Wilczynski, G.M.; Cecchelli, R.; Nalecz, K.A. Protein kinase C restricts transport of carnitine by amino acid transporter ATB(0,+) apically localized in the blood-brain barrier. Arch. Biochem. Biophys. 2014, 554, 28–35. [Google Scholar] [CrossRef]
- Wu, X.; Huang, W.; Prasad, P.D.; Seth, P.; Rajan, D.P.; Leibach, F.H.; Chen, J.; Conway, S.J.; Ganapathy, V. Functional characteristics and tissue distribution pattern of organic cation transporter 2 (OCTN2), an organic cation/carnitine transporter. J. Pharmacol. Exp. Ther. 1999, 290, 1482–1492. [Google Scholar] [PubMed]
- Nezu, J.; Tamai, I.; Oku, A.; Ohashi, R.; Yabuuchi, H.; Hashimoto, N.; Nikaido, H.; Sai, Y.; Koizumi, A.; Shoji, Y.; et al. Primary systemic carnitine deficiency is caused by mutations in a gene encoding sodium ion-dependent carnitine transporter. Nat. Genet. 1999, 21, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; George, R.L.; Huang, W.; Wang, H.; Conway, S.J.; Leibach, F.H.; Ganapathy, V. Structural and functional characteristics and tissue distribution pattern of rat OCTN1, an organic cation transporter, cloned from placenta. Biochim. Biophys. Acta 2000, 1466, 315–327. [Google Scholar] [CrossRef] [Green Version]
- Grundemann, D.; Harlfinger, S.; Golz, S.; Geerts, A.; Lazar, A.; Berkels, R.; Jung, N.; Rubbert, A.; Schomig, E. Discovery of the ergothioneine transporter. Proc. Natl. Acad. Sci. USA 2005, 102, 5256–5261. [Google Scholar] [CrossRef] [Green Version]
- Cahoy, J.D.; Emery, B.; Kaushal, A.; Foo, L.C.; Zamanian, J.L.; Christopherson, K.S.; Xing, Y.; Lubischer, J.L.; Krieg, P.A.; Krupenko, S.A.; et al. A transcriptome database for astrocytes, neurons, and oligodendrocytes: A new resource for understanding brain development and function. J. Neurosci. 2008, 28, 264–278. [Google Scholar] [CrossRef] [Green Version]
- Jernberg, J.N.; Bowman, C.E.; Wolfgang, M.J.; Scafidi, S. Developmental regulation and localization of carnitine palmitoyltransferases (CPTs) in rat brain. J. Neurochem. 2017, 142, 407–419. [Google Scholar] [CrossRef]
- Ingoglia, F.; Visigalli, R.; Rotoli, B.M.; Barilli, A.; Riccardi, B.; Puccini, P.; Milioli, M.; Di Lascia, M.; Bernuzzi, G.; Dall’Asta, V. Human macrophage differentiation induces OCTN2-mediated L-carnitine transport through stimulation of mTOR-STAT3 axis. J. Leukoc. Biol. 2017, 101, 665–674. [Google Scholar] [CrossRef]
- Wang, C.; Uray, I.P.; Mazumdar, A.; Mayer, J.A.; Brown, P.H. SLC22A5/OCTN2 expression in breast cancer is induced by estrogen via a novel intronic estrogen-response element (ERE). Breast Cancer Res. Treat. 2012, 134, 101–115. [Google Scholar] [CrossRef] [Green Version]
- Koch, A.; Konig, B.; Stangl, G.I.; Eder, K. PPAR alpha mediates transcriptional upregulation of novel organic cation transporters-2 and -3 and enzymes involved in hepatic carnitine synthesis. Exp. Biol. Med. 2008, 233, 356–365. [Google Scholar] [CrossRef]
- Eder, K.; Ringseis, R. The role of peroxisome proliferator-activated receptor alpha in transcriptional regulation of novel organic cation transporters. Eur. J. Pharmacol. 2010, 628, 1–5. [Google Scholar] [CrossRef]
- D’Argenio, G.; Petillo, O.; Margarucci, S.; Torpedine, A.; Calarco, A.; Koverech, A.; Boccia, A.; Paolella, G.; Peluso, G. Colon OCTN2 gene expression is up-regulated by peroxisome proliferator-activated receptor gamma in humans and mice and contributes to local and systemic carnitine homeostasis. J. Biol. Chem. 2010, 285, 27078–27087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, X.; Ringseis, R.; Wen, G.; Eder, K. Carnitine transporter OCTN2 and carnitine uptake in bovine kidney cells is regulated by peroxisome proliferator-activated receptor beta/delta. Acta Vet. Scand. 2014, 56, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, G.; Ringseis, R.; Eder, K. Mouse OCTN2 is directly regulated by peroxisome proliferator-activated receptor alpha (PPARalpha) via a PPRE located in the first intron. Biochem. Pharmacol. 2009, 79, 768–776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, H.; Zhang, Y.; Guo, H.; Zhang, L.; Li, X.; Ringseis, R.; Wen, G.; Hui, D.; Liang, A.; Eder, K.; et al. Transcriptional regulation of the human, porcine and bovine OCTN2 gene by PPARalpha via a conserved PPRE located in intron 1. BMC Genet. 2014, 15, 90. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.; Ringseis, R.; Wen, G.; Eder, K. The pro-inflammatory cytokine tumor necrosis factor alpha stimulates expression of the carnitine transporter OCTN2 (novel organic cation transporter 2) and carnitine uptake via nuclear factor-kappaB in Madin-Darby bovine kidney cells. J. Dairy Sci. 2015, 98, 3840–3848. [Google Scholar] [CrossRef]
- Nagai, K.; Takikawa, O.; Kawakami, N.; Fukao, M.; Soma, T.; Oda, A.; Nishiya, T.; Hayashi, M.; Lu, L.; Nakano, M.; et al. Cloning and functional characterization of a novel up-regulator, cartregulin, of carnitine transporter, OCTN2. Arch. Biochem. Biophys. 2006, 452, 29–37. [Google Scholar] [CrossRef] [Green Version]
- Filippo, C.A.; Ardon, O.; Longo, N. Glycosylation of the OCTN2 carnitine transporter: Study of natural mutations identified in patients with primary carnitine deficiency. Biochim. Biophys. Acta 2011, 1812, 312–320. [Google Scholar] [CrossRef] [Green Version]
- Czeredys, M.; Samluk, L.; Michalec, K.; Tulodziecka, K.; Skowronek, K.; Nalecz, K.A. Caveolin-1-a novel interacting partner of organic cation/carnitine transporter (octn2): Effect of protein kinase C on this interaction in rat astrocytes. PLoS ONE 2013, 8, e82105. [Google Scholar] [CrossRef]
- Rytting, E.; Audus, K.L. Contributions of phosphorylation to regulation of OCTN2 uptake of carnitine are minimal in BeWo cells. Biochem. Pharmacol. 2008, 75, 745–751. [Google Scholar] [CrossRef] [Green Version]
- Kato, Y.; Sai, Y.; Yoshida, K.; Watanabe, C.; Hirata, T.; Tsuji, A. PDZK1 directly regulates the function of organic cation/carnitine transporter OCTN2. Mol. Pharmacol. 2005, 67, 734–743. [Google Scholar] [CrossRef]
- Watanabe, C.; Kato, Y.; Sugiura, T.; Kubo, Y.; Wakayama, T.; Iseki, S.; Tsuji, A. PDZ adaptor protein PDZK2 stimulates transport activity of organic cation/carnitine transporter OCTN2 by modulating cell surface expression. Drug Metab. Dispos. 2006, 34, 1927–1934. [Google Scholar] [CrossRef] [PubMed]
- Juraszek, B.; Nalecz, K.A. Protein phosphatase PP2A-a novel interacting partner of carnitine transporter OCTN2 (SLC22A5) in rat astrocytes. J. Neurochem. 2016, 139, 537–551. [Google Scholar] [CrossRef] [PubMed]
- Jurkiewicz, D.; Michalec, K.; Skowronek, K.; Nałęcz, K.A. Tight junction protein ZO-1 controls organic cation/carnitine transporter OCTN2 (SLC22A5) in a protein kinase C-dependent way. Biochim. Biophys. Acta 2017, 1864, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Ye, F.; Zhang, M. Structures and target recognition modes of PDZ domains: Recurring themes and emerging pictures. Biochem. J. 2013, 455, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Hung, A.Y.; Sheng, M. PDZ domains: Structural modules for protein complex assembly. J. Biol. Chem. 2002, 277, 5699–5702. [Google Scholar] [CrossRef] [Green Version]
- Herve, J.C.; Derangeon, M.; Sarrouilhe, D.; Bourmeyster, N. Influence of the scaffolding protein Zonula Occludens (ZOs) on membrane channels. Biochim. Biophys. Acta 2014, 1838, 595–604. [Google Scholar] [CrossRef] [Green Version]
- Blumberg, P.M. Protein kinase C as the receptor for the phorbol ester tumor promoters: Sixth Rhoads memorial award lecture. Cancer Res. 1988, 48, 1–8. [Google Scholar]
- Seshacharyulu, P.; Pandey, P.; Datta, K.; Batra, S.K. Phosphatase: PP2A structural importance, regulation and its aberrant expression in cancer. Cancer Lett. 2013, 335, 9–18. [Google Scholar] [CrossRef] [Green Version]
- Wagner, C.A.; Lukewille, U.; Kaltenbach, S.; Moschen, I.; Broer, A.; Risler, T.; Broer, S.; Lang, F. Functional and pharmacological characterization of human Na(+)- carnitine cotransporter hOCTN2. Am. J. Physiol. Renal. Physiol. 2000, 279, 584–591. [Google Scholar] [CrossRef]
- Ohashi, R.; Tamai, I.; Nezu, J.I.; Nikaido, H.; Hashimoto, N.; Oku, A.; Sai, Y.; Shimane, M.; Tsuji, A. Molecular and physiological evidence for multifunctionality of carnitine/organic cation transporter OCTN2. Mol. Pharmacol. 2001, 59, 358–366. [Google Scholar] [CrossRef]
- Dos Santos Pereira, J.N.; Tadjerpisheh, S.; Abu Abed, M.; Saadatmand, A.R.; Weksler, B.; Romero, I.A.; Couraud, P.O.; Brockmoller, J.; Tzvetkov, M.V. The poorly membrane permeable antipsychotic drugs amisulpride and sulpiride are substrates of the organic cation transporters from the SLC22 family. AAPS J. 2014, 16, 1247–1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, C.; Lancaster, C.S.; Zuo, Z.; Hu, S.; Chen, Z.; Rubnitz, J.E.; Baker, S.D.; Sparreboom, A. Inhibition of OCTN2-mediated transport of carnitine by etoposide. Mol. Cancer Ther. 2012, 11, 921–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jong, N.N.; Nakanishi, T.; Liu, J.J.; Tamai, I.; McKeage, M.J. Oxaliplatin transport mediated by organic cation/carnitine transporters OCTN1 and OCTN2 in overexpressing human embryonic kidney 293 cells and rat dorsal root ganglion neurons. J. Pharmacol. Exp. Ther. 2011, 338, 537–547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, S.; Franke, R.M.; Filipski, K.K.; Hu, C.; Orwick, S.J.; de Bruijn, E.A.; Burger, H.; Baker, S.D.; Sparreboom, A. Interaction of imatinib with human organic ion carriers. Clin. Cancer Res. 2008, 14, 3141–3148. [Google Scholar] [CrossRef] [Green Version]
- Campone, M.; Berton-Rigaud, D.; Joly-Lobbedez, F.; Baurain, J.F.; Rolland, F.; Stenzl, A.; Fabbro, M.; van Dijk, M.; Pinkert, J.; Schmelter, T.; et al. A double-blind, randomized phase II study to evaluate the safety and efficacy of acetyl-L-carnitine in the prevention of sagopilone-induced peripheral neuropathy. Oncologist 2013, 18, 1190–1191. [Google Scholar] [CrossRef] [Green Version]
- Hershman, D.L.; Unger, J.M.; Crew, K.D.; Minasian, L.M.; Awad, D.; Moinpour, C.M.; Hansen, L.; Lew, D.L.; Greenlee, H.; Fehrenbacher, L.; et al. Randomized double-blind placebo-controlled trial of acetyl-l-carnitine for the prevention of taxane-induced neuropathy in women undergoing adjuvant breast cancer therapy. J. Clin. Oncol. 2013, 31, 2627–2633. [Google Scholar] [CrossRef] [Green Version]
- Visentin, M.; Gai, Z.; Torozi, A.; Hiller, C.; Kullak-Ublick, G.A. Colistin is substrate of the carnitine/organic cation transporter 2 (OCTN2, SLC22A5). Drug Metab. Dispos. 2017, 45, 1240–1244. [Google Scholar] [CrossRef] [Green Version]
- Grigat, S.; Fork, C.; Bach, M.; Golz, S.; Geerts, A.; Schomig, E.; Grundemann, D. The carnitine transporter SLC22A5 is not a general drug transporter, but it efficiently translocates mildronate. Drug Metab. Dispos. 2009, 37, 330–337. [Google Scholar] [CrossRef] [Green Version]
- Ganapathy, M.E.; Huang, W.; Rajan, D.P.; Carter, A.L.; Sugawara, M.; Iseki, K.; Leibach, F.H.; Ganapathy, V. Beta-lactam antibiotics as substrates for OCTN2, an organic cation/carnitine transporter. J. Biol. Chem. 2000, 275, 1699–1707. [Google Scholar] [CrossRef] [Green Version]
- Szabo, K.; Nagy, Z.; Juhasz, V.; Zolnerciks, J.K.; Csorba, A.; Timar, Z.; Molnar, E.; Padar, P.; Johnson, W.; Beery, E.; et al. Species specificity profiling of rat and human organic cation/carnitine transporter Slc22a5/SLC22A5 (Octn2/OCTN2). Drug Metab. Pharmacokinet 2017, 32, 165–171. [Google Scholar] [CrossRef]
- Grube, M.; Ameling, S.; Noutsias, M.; Kock, K.; Triebel, I.; Bonitz, K.; Meissner, K.; Jedlitschky, G.; Herda, L.R.; Reinthaler, M.; et al. Selective regulation of cardiac organic cation transporter novel type 2 (OCTN2) in dilated cardiomyopathy. Am. J. Pathol. 2011, 178, 2547–2559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Todesco, L.; Bur, D.; Brooks, H.; Torok, M.; Landmann, L.; Stieger, B.; Krahenbuhl, S. Pharmacological manipulation of L-carnitine transport into L6 cells with stable overexpression of human OCTN2. Cell Mol. Life Sci. 2008, 65, 1596–1608. [Google Scholar] [CrossRef] [PubMed]
- Grube, M.; Meyer zu Schwabedissen, H.E.; Prager, D.; Haney, J.; Moritz, K.U.; Meissner, K.; Rosskopf, D.; Eckel, L.; Bohm, M.; Jedlitschky, G.; et al. Uptake of cardiovascular drugs into the human heart: Expression, regulation, and function of the carnitine transporter OCTN2 (SLC22A5). Circulation 2006, 113, 1114–1122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elimrani, I.; Dionne, S.; Saragosti, D.; Qureshi, I.; Levy, E.; Delvin, E.; Seidman, E.G. Acetylcarnitine potentiates the anticarcinogenic effects of butyrate on SW480 colon cancer cells. Int. J. Oncol. 2015, 47, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, C.S.; Hu, C.; Franke, R.M.; Filipski, K.K.; Orwick, S.J.; Chen, Z.; Zuo, Z.; Loos, W.J.; Sparreboom, A. Cisplatin-induced downregulation of OCTN2 affects carnitine wasting. Clin. Cancer Res. 2010, 16, 4789–4799. [Google Scholar] [CrossRef] [Green Version]
- Johnston, R.A.; Rawling, T.; Chan, T.; Zhou, F.; Murray, M. Selective inhibition of human solute carrier transporters by multikinase inhibitors. Drug Metab. Dispos. 2014, 42, 1851–1857. [Google Scholar] [CrossRef] [Green Version]
- Zheng, J.; Chan, T.; Zhu, L.; Yan, X.; Cao, Z.; Wang, Y.; Zhou, F. The inhibitory effects of camptothecin (CPT) and its derivatives on the substrate uptakes mediated by human solute carrier transporters (SLCs). Xenobiotica 2016, 46, 831–840. [Google Scholar] [CrossRef]
- Nehlig, A.; Pereira de Vasconcelos, A. Glucose and ketone body utilization by the brain of neonatal rats. Prog. Neurobiol. 1993, 40, 163–221. [Google Scholar] [CrossRef]
- Patel, A.B.; Lai, J.C.; Chowdhury, G.M.; Hyder, F.; Rothman, D.L.; Shulman, R.G.; Behar, K.L. Direct evidence for activity-dependent glucose phosphorylation in neurons with implications for the astrocyte-to-neuron lactate shuttle. Proc. Natl. Acad. Sci. USA 2014, 111, 5385–5390. [Google Scholar] [CrossRef] [Green Version]
- Pellerin, L.; Magistretti, P.J. Neuroenergetics: Calling upon astrocytes to satisfy hungry neurons. Neuroscientist 2004, 10, 53–62. [Google Scholar] [CrossRef]
- Ebert, D.; Haller, R.G.; Walton, M.E. Energy contribution of octanoate to intact rat brain metabolism measured by 13C nuclear magnetic resonance spectroscopy. J. Neurosci. 2003, 23, 5928–5935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schonfeld, P.; Reiser, G. Why does brain metabolism not favor burning of fatty acids to provide energy? Reflections on disadvantages of the use of free fatty acids as fuel for brain. J. Cereb. Blood Flow Metab. 2013, 33, 1493–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, R.W.; Edmundson, C.L.; Miller, D.W.; Hatch, G.M. On the mechanism of oleate transport across human brain microvessel endothelial cells. J. Neurochem. 2009, 110, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.W.; On, N.H.; Del Bigio, M.R.; Miller, D.W.; Hatch, G.M. Fatty acid transport protein expression in human brain and potential role in fatty acid transport across human brain microvessel endothelial cells. J. Neurochem. 2011, 117, 735–746. [Google Scholar] [CrossRef] [PubMed]
- Lamhonwah, A.M.; Baric, I.; Lamhonwah, J.; Grubic, M.; Tein, I. Attention deficit/hyperactivity disorder as an associated feature in OCTN2 deficiency with novel deletion (p.T440-Y449). Clin. Case Rep. 2018, 6, 585–591. [Google Scholar] [CrossRef] [Green Version]
- Celestino-Soper, P.B.; Violante, S.; Crawford, E.L.; Luo, R.; Lionel, A.C.; Delaby, E.; Cai, G.; Sadikovic, B.; Lee, K.; Lo, C.; et al. A common X-linked inborn error of carnitine biosynthesis may be a risk factor for nondysmorphic autism. Proc. Natl. Acad. Sci. USA 2012, 109, 7974–7981. [Google Scholar] [CrossRef] [Green Version]
- Ziats, M.N.; Comeaux, M.S.; Yang, Y.; Scaglia, F.; Elsea, S.H.; Sun, Q.; Beaudet, A.L.; Schaaf, C.P. Improvement of regressive autism symptoms in a child with TMLHE deficiency following carnitine supplementation. Am. J. Med. Genet. A 2015, 167A, 2162–2167. [Google Scholar] [CrossRef]
- Lin, H.; Patel, S.; Affleck, V.S.; Wilson, I.; Turnbull, D.M.; Joshi, A.R.; Maxwell, R.; Stoll, E.A. Fatty acid oxidation is required for the respiration and proliferation of malignant glioma cells. Neuro. Oncol. 2017, 19, 43–54. [Google Scholar] [CrossRef] [Green Version]
- Fink, M.A.; Paland, H.; Herzog, S.; Grube, M.; Vogelgesang, S.; Weitmann, K.; Bialke, A.; Hoffmann, W.; Rauch, B.H.; Schroeder, H.W.S.; et al. L-Carnitine-Mediated Tumor Cell Protection and Poor Patient Survival Associated with OCTN2 Overexpression in Glioblastoma Multiforme. Clin. Cancer Res. 2019, 25, 2874–2886. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, T.; Seino, Y.; Fukumoto, H.; Koh, G.; Yano, H.; Inagaki, N.; Yamada, Y.; Inoue, K.; Manabe, T.; Imura, H. Over-expression of facilitative glucose transporter genes in human cancer. Biochem. Biophys. Res. Commun. 1990, 170, 223–230. [Google Scholar] [CrossRef]
- Yu, M.; Yongzhi, H.; Chen, S.; Luo, X.; Lin, Y.; Zhou, Y.; Jin, H.; Hou, B.; Deng, Y.; Tu, L.; et al. The prognostic value of GLUT1 in cancers: A systematic review and meta-analysis. Oncotarget 2017, 8, 43356–43367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carracedo, A.; Cantley, L.C.; Pandolfi, P.P. Cancer metabolism: Fatty acid oxidation in the limelight. Nat. Rev. Cancer 2013, 13, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Pike, L.S.; Smift, A.L.; Croteau, N.J.; Ferrick, D.A.; Wu, M. Inhibition of fatty acid oxidation by etomoxir impairs NADPH production and increases reactive oxygen species resulting in ATP depletion and cell death in human glioblastoma cells. Biochim. Biophys. Acta 2011, 1807, 726–734. [Google Scholar] [CrossRef] [Green Version]
- Schlaepfer, I.R.; Rider, L.; Rodrigues, L.U.; Gijon, M.A.; Pac, C.T.; Romero, L.; Cimic, A.; Sirintrapun, S.J.; Glode, L.M.; Eckel, R.H.; et al. Lipid catabolism via CPT1 as a therapeutic target for prostate cancer. Mol. Cancer Ther. 2014, 13, 2361–2371. [Google Scholar] [CrossRef] [Green Version]
- Harper, M.E.; Antoniou, A.; Villalobos-Menuey, E.; Russo, A.; Trauger, R.; Vendemelio, M.; George, A.; Bartholomew, R.; Carlo, D.; Shaikh, A.; et al. Characterization of a novel metabolic strategy used by drug-resistant tumor cells. FASEB J. 2002, 16, 1550–1557. [Google Scholar] [CrossRef] [Green Version]
- Torrano, V.; Valcarcel-Jimenez, L.; Cortazar, A.R.; Liu, X.; Urosevic, J.; Castillo-Martin, M.; Fernandez-Ruiz, S.; Morciano, G.; Caro-Maldonado, A.; Guiu, M.; et al. The metabolic co-regulator PGC1alpha suppresses prostate cancer metastasis. Nat. Cell Biol. 2016, 18, 645–656. [Google Scholar] [CrossRef] [Green Version]
- Valcarcel-Jimenez, L.; Macchia, A.; Crosas-Molist, E.; Schaub-Clerigue, A.; Camacho, L.; Martin-Martin, N.; Cicogna, P.; Viera-Bardon, C.; Fernandez-Ruiz, S.; Rodriguez-Hernandez, I.; et al. PGC1alpha suppresses prostate cancer cell invasion through ERRalpha transcriptional control. Cancer Res. 2019. [Google Scholar] [CrossRef] [Green Version]
- Mastropasqua, F.; Girolimetti, G.; Shoshan, M. PGC1alpha: Friend or Foe in Cancer? Genes (Basel) 2018, 9, 48. [Google Scholar] [CrossRef] [Green Version]
- Camarda, R.; Zhou, A.Y.; Kohnz, R.A.; Balakrishnan, S.; Mahieu, C.; Anderton, B.; Eyob, H.; Kajimura, S.; Tward, A.; Krings, G.; et al. Inhibition of fatty acid oxidation as a therapy for MYC-overexpressing triple-negative breast cancer. Nat. Med. 2016, 22, 427–432. [Google Scholar] [CrossRef]
- Holubarsch, C.J.; Rohrbach, M.; Karrasch, M.; Boehm, E.; Polonski, L.; Ponikowski, P.; Rhein, S. A double-blind randomized multicentre clinical trial to evaluate the efficacy and safety of two doses of etomoxir in comparison with placebo in patients with moderate congestive heart failure: The ERGO (etomoxir for the recovery of glucose oxidation) study. Clin. Sci. 2007, 113, 205–212. [Google Scholar] [PubMed]
- Scalise, M.; Galluccio, M.; Accardi, R.; Cornet, I.; Tommasino, M.; Indiveri, C. Human OCTN2 (SLC22A5) is down-regulated in virus- and nonvirus-mediated cancer. Cell Biochem. Funct. 2012, 30, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Elsnerova, K.; Mohelnikova-Duchonova, B.; Cerovska, E.; Ehrlichova, M.; Gut, I.; Rob, L.; Skapa, P.; Hruda, M.; Bartakova, A.; Bouda, J.; et al. Gene expression of membrane transporters: Importance for prognosis and progression of ovarian carcinoma. Oncol. Rep. 2016, 35, 2159–2170. [Google Scholar] [CrossRef] [PubMed]
- Cortazar, A.R.; Torrano, V.; Martin-Martin, N.; Caro-Maldonado, A.; Camacho, L.; Hermanova, I.; Guruceaga, E.; Lorenzo-Martin, L.F.; Caloto, R.; Gomis, R.R.; et al. CANCERTOOL: A Visualization and Representation Interface to Exploit Cancer Datasets. Cancer Res. 2018, 78, 6320–6328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.H.; Zhao, X.M.; Yoon, I.; Lee, J.Y.; Kwon, N.H.; Wang, Y.Y.; Lee, K.M.; Lee, M.J.; Kim, J.; Moon, H.G.; et al. Integrative analysis of mutational and transcriptional profiles reveals driver mutations of metastatic breast cancers. Cell Discov. 2016, 2, 16025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, X.; Lu, X.; Wang, Z.C.; Iglehart, J.D.; Zhang, X.; Richardson, A.L. Predicting features of breast cancer with gene expression patterns. Breast Cancer Res. Treat. 2008, 108, 191–201. [Google Scholar] [CrossRef]
- Kou, L.; Sun, R.; Ganapathy, V.; Yao, Q.; Chen, R. Recent advances in drug delivery via the organic cation/carnitine transporter 2 (OCTN2/SLC22A5). Expert Opin. Ther. Targets 2018, 22, 715–726. [Google Scholar] [CrossRef]
- 108 Kou, L.; Hou, Y.; Yao, Q.; Guo, W.; Wang, G.; Wang, M.; Fu, Q.; He, Z.; Ganapathy, V.; Sun, J. l-Carnitine-conjugated nanoparticles to promote permeation across blood-brain barrier and to target glioma cells for drug delivery via the novel organic cation/carnitine transporter OCTN2. Artif. Cell Nanomed. B. 2018, 46, 1605–1616. [Google Scholar]




| Name | Aliases | Type of Transport | Other Ions | Km (µM) | Cell Localization | Expression | Ref. |
|---|---|---|---|---|---|---|---|
| SLC25A20 | CAC, CACT | E, U | - | 10200# (in) | inner mitochondrial membrane | ubiquitous | [16] |
| 480# (out) | |||||||
| Slc22a21 * | Octn3 | U | - | 2.99 | peroxisomal membrane | testis, brain, fibroblasts | [12,17,18,19] |
| SLC22A16 | CT2/FLIPT2 | F | - | 20.3 | plasma membrane | testis, epididymis, endometrium | [20] |
| SLC6A14 | ATB0,+ | U | 2 Na+, 1 Cl− | 803 | plasma membrane | lung, trachea and salivary gland | [21] |
| SLC22A5 | OCTN2, CT1 | U | Na+ | 4.3 | plasma membrane | ubiquitous; kidney, skeletal muscle, heart, placenta, brain | [12,19,22,23,24] |
| Drug | Drug Target and Use | Conc. | Net Uptake | Time of Uptake | Type of Assay | Other Info | Ref. | |
|---|---|---|---|---|---|---|---|---|
| amisulpride | selective dopamine antagonist; antipsychotic drug, treatment of psychoses, schizophrenia and persistent depressive disorder | hOCTN2 | 5 µM | ≈13 ± 1.5 pmol/min/mg protein | 2 min | HPLC | Km 185.3 ± 68 µM | [61] |
| [14C]colistin | surface active agent which penetrates into and disrupts the bacterial cell membrane; antibiotic effective against most Gram-negative bacilli, particularly Pseudomonas aeruginosa | hOCTN2 | 1 µM | 2.4 pmol/mg protein | 10 min | radioactive | [67] | |
| [3H]etoposide | DNA topoisomerase II inhibitor; treatment of testicular cancer, small cell lung cancer, acute myeloid leukaemia, lymphoma, ovarian cancer | hOCTN2 | ND | 2.85 µL/mg/5min | 5 min | radioactive | independent of Na+; Km 150 ± 34.1 µM | [62] |
| mildronate | inhibitor of gamma-butyrobetaine dioxygenase, inhibits carnitine biosynthesis; anti-ischemia medication | hOCTN2 | 10 µM | ≈250 µL/min mg protein | 1 min | LC/MS/MS | [68] | |
| [14C]oxaliplatin | cross-links DNA, thus inhibiting DNA synthesis and transcription; treatment of colon and rectum advanced carcinoma | hOCTN2 | 1 µM | ≈1.5 µL/mg protein | 1 h | radioactive | [63] | |
| [14C]oxaliplatin | rOctn2 | 1 µM | ≈3.5 µL/mg protein | 1 h | radioactive | |||
| [3H]verapamil | calcium channel blocker; class IV anti-arrhythmia agent used to treat hypertension, angina (chest pain), and certain heart rhythm disorders | mOctn2 | 12 nM | 275 µL/mg protein | 5 min | radioactive | [60] | |
| [3H]pyrilamine | H1 receptor; antihistamine | 50 nM | 118 µL/mg protein | 5 min | radioactive | |||
| [3H]imatinib | Bcr-Abl tyrosine-kinase inhibitor; cancer treatment (chronic myelogenous leukemia (CML), acute lymphoblastic leukemia (ALL), gastrointestinal stromal tumors (GISTs) and other) | mOctn2 | 0.2 µM | 140% of control | ND | radioactive | [64] |
| Drug | Drug Target and Use | Concentration µM | Relative Uptake % of Control | Experimental System | Ref. | ||||
|---|---|---|---|---|---|---|---|---|---|
| hOCTN2 | rOctn2 | mOctn2 | hOCTN2 | rOctn2 | mOctn2 | ||||
| cephaloridine | disrupts the synthesis of the peptidoglycan layer of bacterial cell walls; experimental drug, withdrawn from clinical trials | 2500 | 10 | JAR; E | [69] | ||||
| 2500 | 2500 | 13 | 25 | HEK293; O | [69] | ||||
| cefepime | disrupts the synthesis of the peptidoglycan layer of bacterial cell walls; active against Gram+ and Gram− bacteria, for the treatment of pneumonia, urinary tract infections, skin infections | 2500 | 19 | JAR; E | [69] | ||||
| 2500 | 2500 | 27 | 28 | HEK293; O | [69] | ||||
| cefluprenam | disrupts the synthesis of the peptidoglycan layer of bacterial cell walls; | 2500 | 58 | JAR; E | [69] | ||||
| 2500 | 2500 | 74 | 76 | HEK293; O | [69] | ||||
| nelfinavir mesylate hydrate | HIV-1 protease inhibitor; antiviral drug used for treatment of HIV | 11.87 * | 3.138 * | 50 | 50 | CHO; O | [70] | ||
| ipratropium bromide | blocks muscarinic acetylcholine receptors; anticholinergic agent for treatment of chronic obstructive pulmonary disease (COPD) and asthma | 100 | 71.3 ± 2.3 | MDCKII; O | [71] | ||||
| 100/1000 | 38 ± 2/29 ± 2 | L6; O | [72] | ||||||
| nifedipine | calcium channel blocker; used to treat hypertension and chronic stable angina | 100/59.4 * | 69.6 ± 16.4/50 | MDCKII; O | [71] | ||||
| spironolactone | antagonist of the mineralocorticoid receptor; treatment of heart failure, hyperaldosteronism, adrenal hyperplasia, hypertension, and nephrotic syndrome | 100/36 * | 72.2 ± 12.0/50 | MDCKII; O | [71] | ||||
| 50 | 48 ± 3 | MDCKII; O | [73] | ||||||
| tetraethyl-ammonium (TEA) | blocks potassium and voltage-dependent channels; no approved use in humans | 448.4 * | 211.8 * | 50 | 50 | CHO; O | [70] | ||
| quinine | target not fully known; antimalarial drug | 26.94 * | 79.48 * | 50 | 50 | CHO; O | [70] | ||
| quinidine | blocker of voltage-gated sodium and potassium channels; class I antiarrhythmic agent | 17.44 * | 45.75 * | 50 | 50 | CHO; O | [70] | ||
| 500 | 6.1 ± 0.40 | HEK293; O | [60] | ||||||
| 500 | ≈36.4 | Nb2a; E | [24] | ||||||
| lidocaine | blocks sodium channels; local anesthetic, also class Ib antiarrhythmic agent | 500 | 57.1 ± 1.14 | HEK293; O | [60] | ||||
| 100 | 77.6 ± 7.8 | MDCKII; O | [71] | ||||||
| 50 | 69 ± 7 | MDCKII; O | [73] | ||||||
| amiodarone | blocker of voltage gated potassium and voltage gated calcium channels; antiarrhythmic drug | 100 | 66.3 ± 16.2 | MDCKII; O | [71] | ||||
| enalapril | angiotensin-converting enzyme (ACE) inhibitor; treatment of hypertension, heart failure, asymptomatic left ventricular dysfunction and diabetic nephropathy | 50 | 71 ± 4 | MDCKII; O | [73] | ||||
| verapamil | calcium channel blocker; class IV anti-arrhythmia agent used to treat hypertension, angina (chest pain), and certain heart rhythm disorders | 17.53 * | 46.66 * | 50 | 50 | CHO; O | [70] | ||
| 500 | 1.3 ± 0.12 | HEK293; O | [60] | ||||||
| 500 | ≈34 | Nb2a; E | [24] | ||||||
| 100/50.9 * | 66.5 ± 38.3/50 | MDCKII; O | [71] | ||||||
| 50 | 58 ± 2 | MDCKII; O | [73] | ||||||
| 100/1000 | 54 ± 1/28 ± 1 | L6; O | [72] | ||||||
| simvastatine | lipid-lowering drug; treatment of dyslipidemia and to lower the risk of cardiovascular disease | 8.457 * | 13.05 * | 50 | 50 | CHO; O | [70] | ||
| pyrilamine | H1 receptor; antihistamine | 500 | 15.4 ± 0.73 | HEK293; O | [60] | ||||
| 500 | ≈35 | SW480; E | [74] | ||||||
| 500 | ≈27.5 | SW480; E | [74] | ||||||
| diphenhydra-mine | H1 receptor; antihistamine, also used for tremor in parkinsonism and as antiemetic | 500 | 43.6 ± 1.74 | HEK293; O | [60] | ||||
| cortisone | naturally occurring glucocorticoid; used in replacement therapy for adrenal insufficiency and as an anti-inflammatory agent | 50 | 64 ± 3 | MDCKII; O | [73] | ||||
| mildronate | inhibitor of gamma-butyrobetaine dioxygenase, inhibits carnitine biosynthesis; anti-ischemia medication | 50 | 42 ± 7 | MDCKII; O | [73] | ||||
| rapamycin/sirolimus | bind the cytosolic protein FK-binding protein 12 (FKBP12) what inhibits the mTOR kinase and blocks activation of T and B cells; immunosuppressive agent indicated for the prevention of transplant rejection | 100 | 100 | 70.2 ± 5.7 | 75.2 ± 6.7 | HEK293; O | [62] | ||
| imatinib | Bcr-Abl tyrosine-kinase inhibitor; cancer treatment (chronic myelogenous leukemia (CML), acute lymphoblastic leukemia (ALL), gastrointestinal stromal tumors (GISTs) and other) | 30.99 * | 71.19 * | 50 | 50 | CHO; O | [70] | ||
| vincristine | binds tubulin and stops tubulin dimers from polymerizing to form microtubules; treatment of acute leukaemia, malignant lymphoma, Hodgkin’s disease, acute erythraemia, and acute panmyelosis. | 39 * | 16.26 * | 50 | 50 | CHO; O | [70] | ||
| 100 | 100 | 33.6 ± 0.1 | 101 ± 7.3 | HEK293; O | [62] | ||||
| paclitaxel | hyper-stabilizes structure of polymerized microtubules; treatment of ovarian cancer, breast cancer, non-small cell lung carcinoma, Kaposi sarcoma | 100 | 100 | 64.9 ± 1.8 | 29.3 ± 8.1 | HEK293; O | [62] | ||
| daunorubicin | intercalates DNA and inhibits topoisomerase II activity; treatment of acute nonlymphocytic leukemia (myelogenous, monocytic, erythroid) | 50 | 50 | 62.3 ± 4.5 | 57.8 ± 2.2 | HEK293; O | [62] | ||
| vinblastine | binds to the microtubular proteins of the mitotic spindle, preventing polymerisation; treatment of Hodgkin’s disease, lymphocytic lymphoma, advanced testicular cancer, Kaposi’s sarcoma, choriocarcinoma, breast cancer, melanoma | 100 | 100 | 58.4 ± 1.1 | 79.9 ± 10.4 | HEK293; O | [62] | ||
| sunitinib | multi-targeted receptor tyrosine kinase (RTK) inhibitor; treatment of renal cell carcinoma (RCC) and imatinib-resistant gastrointestinal stromal tumor (GIST) | 100 | 100 | 46.2 ± 1.4 | 63.6 ± 9.5 | HEK293; O | [62] | ||
| etoposide | DNA topoisomerase II inhibitor; treatment of testicular cancer, small cell lung cancer, acute myeloid leukaemia, lymphoma, ovarian cancer | 100/55 * | 100 | 41.2 ± 4.5/50 | 64.3 ± 4.1 | HEK293; O | [62] | ||
| vinorelbine | binds to tubulin and prevents formation of the mitotic spindle; treatment of advanced nonsmall cell lung cancer (NSCLC), metastatic breast cancer | 100 | 100 | 15.3 ± 1.3 | 65.6 ± 12.1 | HEK293; O | [62] | ||
| 60 | 60 | ≈20 | ≈65 | HEK293; O | [75] | ||||
| cisplatin | platinum-based chemotherapy drug that intercalates DNA; treatment of various types of cancers (e.g., small cell lung cancer, metastatic testicular and ovarian cancer, advanced bladder cancer, head and neck epithelial tumors | 100 | 100 | ≈90 | ≈65 | HEK293; O | [75] | ||
| oxaliplatin | cross-links DNA, thus inhibiting DNA synthesis and transcription; treatment of colon and rectum advanced carcinoma | 100 | 100 | ≈85 | ≈100 | HEK293; O | [75] | ||
| cediranib | Vascular endothelial growth factor receptor-2 inhibitor; in development, clinical trials for ovarian cancer, alveolar soft part sarcoma, cervical cancer, endometrial cancer, mesothelioma, prostate cancer and solid tumors | 2.49 * | 50 | HEK293; O | [76] | ||||
| camptothecin (CZ112) | selectively inhibits the nuclear enzyme DNA topoisomerase, type I; investigated for the treatment of cancer. | 10/4.5 ± 1.2 | 40/50 | HEK293; O | [77] | ||||
| valporate | not fully known; used to treat epilepsy and bipolar disorder and to prevent migraine headaches; has anti-proliferative effects and is the subject of many clinical trials in a variety of cancer types | 500 | ≈60 | SW480; E | [74] | ||||
| Cancer Patient Survival Analysis Correlated to SLC22A5 Expression | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cancer Type | Prognosis | p Value | % 5 Year Survival | n | FPKM Best Cut Off | FPKM Median | ||
| High | Low | High | Low | |||||
| glioma | unfavorable | 0.0046 | 6 * | 15 * | 105 | 48 | 1.21 | 1.51 |
| melanoma | unfavorable | 0.16 | 22 * | 53 * | 48 | 54 | 0.72 | 0.71 |
| thyroid cancer | unfavorable | 0.022 | 79 | 95 | 101 | 400 | 1.93 | 1.59 |
| liver cancer | unfavorable | 0.015 | 42 | 63 | 257 | 108 | 0.69 | 0.87 |
| prostate cancer | unfavorable | 0.035 | 97 | 99 | 283 | 211 | 3.07 | 3.27 |
| ovarian cancer | unfavorable | 0.051 | 29 | 35 | 176 | 197 | 1.21 | 1.18 |
| cervical cancer | unfavorable | 0.17 | 60 | 73 | 150 | 141 | 1.02 | 1.04 |
| breast cancer | --- | 0.39 | 86 | 77 | 600 | 475 | 2.54 | 2.73 |
| pancreatic cancer | favorable | 0.00074 | 61 | 18 | 43 | 133 | 1.7 | 1.29 |
| stomach cancer | favorable | 0.011 | 50 | 27 | 152 | 202 | 1.54 | 1.45 |
| renal cancer | favorable | 0.00084 | 72 | 61 | 599 | 278 | 5.25 | 7.12 |
| endometrial cancer | favorable | 2.9 × 10−5 | 81 | 63 | 405 | 136 | 1.28 | 1.85 |
| colorectal cancer | favorable | 0.022 | 67 | 51 | 411 | 188 | 1.49 | 1.78 |
| head & neck cancer | favorable | 0.12 | 52 | 41 | 208 | 291 | 0.81 | 0.75 |
| testis cancer | favorable | 0.03 | 100 | 94 | 84 | 50 | 0.6 | 0.74 |
| lung cancer | favorable | 0.092 | 45 | 45 | 647 | 347 | 0.92 | 1.06 |
| urothelial cancer | favorable | 0.012 | 47 | 33 | 250 | 156 | 1.02 | 1.28 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juraszek, B.; Nałęcz, K.A. SLC22A5 (OCTN2) Carnitine Transporter—Indispensable for Cell Metabolism, a Jekyll and Hyde of Human Cancer. Molecules 2020, 25, 14. https://doi.org/10.3390/molecules25010014
Juraszek B, Nałęcz KA. SLC22A5 (OCTN2) Carnitine Transporter—Indispensable for Cell Metabolism, a Jekyll and Hyde of Human Cancer. Molecules. 2020; 25(1):14. https://doi.org/10.3390/molecules25010014
Chicago/Turabian StyleJuraszek, Barbara, and Katarzyna A. Nałęcz. 2020. "SLC22A5 (OCTN2) Carnitine Transporter—Indispensable for Cell Metabolism, a Jekyll and Hyde of Human Cancer" Molecules 25, no. 1: 14. https://doi.org/10.3390/molecules25010014