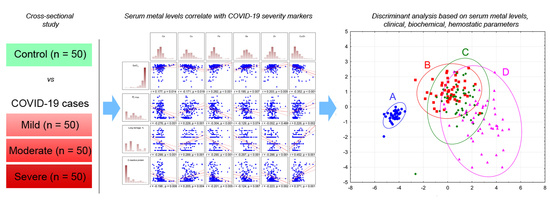
Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782. [Google Scholar] [CrossRef]
- Henderson, L.A.; Canna, S.W.; Schulert, G.S.; Volpi, S.; Lee, P.Y.; Kernan, K.F.; Caricchio, R.; Mahmud, S.; Hazen, M.M.; Halyabar, O.; et al. On the Alert for Cytokine Storm: Immunopathology in COVID-19. Arthritis Rheumatol. 2020, 72, 1059–1063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsatsakis, A.; Calina, D.; Falzone, L.; Petrakis, D.; Mitrut, R.; Siokas, V.; Pennisi, M.; Lanza, G.; Libra, M.; Doukas, S.G.; et al. SARS-CoV-2 pathophysiology and its clinical implications: An integrative overview of the pharmacotherapeutic management of COVID-19. Food Chem. Toxicol. 2020, 146, 111769. [Google Scholar] [CrossRef] [PubMed]
- Munblit, D.; Nekliudov, N.A.; Bugaeva, P.; Blyuss, O.; Kislova, M.; Listovskaya, E.; Gamirova, A.; Shikhaleva, A.; Belyaev, V.; Timashev, P.; et al. StopCOVID cohort: An observational study of 3,480 patients admitted to the Sechenov University hospital network in Moscow city for suspected COVID-19 infection. Clin. Infect. Dis. 2020, ciaa1535. [Google Scholar] [CrossRef] [PubMed]
- Petrakis, D.; Margină, D.; Tsarouhas, K.; Tekos, F.; Stan, M.; Nikitovic, D.; Kouretas, D.; Spandidos, D.A.; Tsatsakis, A. Obesity—A risk factor for increased COVID‑19 prevalence, severity and lethality (Review). Mol. Med. Rep. 2020, 22, 9–19. [Google Scholar] [CrossRef]
- Richardson, D.P.; Lovegrove, J.A. Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: A UK perspective. Br. J. Nutr. 2020, 20, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Im, J.H.; Je, Y.S.; Baek, J.; Chung, M.-H.; Kwon, H.Y.; Lee, J.-S. Nutritional status of patients with COVID-19. Int. J. Infect. Dis. 2020, 100, 390–393. [Google Scholar] [CrossRef]
- Velthuis, A.J.W.T.; Worm, S.H.E.V.D.; Sims, A.C.; Baric, R.S.; Snijder, E.J.; Van Hemert, M.J. Zn2+ Inhibits Coronavirus and Arterivirus RNA Polymerase Activity In Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture. PLoS Pathog. 2010, 6, e1001176. [Google Scholar] [CrossRef]
- Skalny, A.V.; Rink, L.; Ajsuvakova, O.P.; Aschner, M.; Gritsenko, V.A.; Alekseenko, S.I.; Svistunov, A.A.; Petrakis, D.; Spandidos, D.A.; Aaseth, J.; et al. Zinc and respiratory tract infections: Perspectives for COVID‑19 (Review). Int. J. Mol. Med. 2020, 46, 17–26. [Google Scholar] [CrossRef] [Green Version]
- Fooladi, S.; Matin, S.; Mahmoodpoor, A. Copper as a potential adjunct therapy for critically ill COVID-19 patients. Clin. Nutr. ESPEN 2020, 40, 90–91. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.; Tinkov, A.; Strand, T.A.; Alehagen, U.; Skalny, A.; Aaseth, J. Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19. Nutrients 2020, 12, 2358. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Huang, J.; Dai, D.; Feng, Y.; Liu, L.; Nie, S. Serum Iron Level as a Potential Predictor of Coronavirus Disease 2019 Severity and Mortality: A Retrospective Study. Open Forum Infect. Dis. 2020, 7, ofaa250. [Google Scholar] [CrossRef]
- Sonnweber, T.; Boehm, A.; Sahanic, S.; Pizzini, A.; Aichner, M.; Sonnweber, B.; Kurz, K.; Koppelstätter, S.; Haschka, D.; Petzer, V.; et al. Persisting alterations of iron homeostasis in COVID-19 are associated with non-resolving lung pathologies and poor patients’ performance: A prospective observational cohort study. Respir. Res. 2020, 21, 276. [Google Scholar] [CrossRef]
- Gonçalves, T.J.M.; Gonçalves, S.E.A.B.; Guarnieri, A.; Risegato, R.C.; Guimarães, M.P.; de Freitas, D.C.; Razuk-Filho, A.; Junior, P.B.B.; Parrillo, E.F. Association Between Low Zinc Levels and Severity of Acute Respiratory Distress Syndrome by New Coronavirus SARS-CoV-2. Nutr. Clin. Pr. 2021, 36, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Yasui, Y.; Yasui, H.; Suzuki, K.; Saitou, T.; Yamamoto, Y.; Ishizaka, T.; Nishida, K.; Yoshihara, S.; Gohma, I.; Ogawa, Y. Analysis of the predictive factors for a critical illness of COVID-19 during treatment—relationship between serum zinc level and critical illness of COVID-19-. Int. J. Infect. Dis. 2020, 100, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, A.; Heller, R.A.; Sun, Q.; Seelig, J.; Cherkezov, A.; Seibert, L.; Hackler, J.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Selenium Deficiency Is Associated with Mortality Risk from COVID-19. Nutrients 2020, 12, 2098. [Google Scholar] [CrossRef]
- Zhou, X.; Chen, D.; Wang, L.; Zhao, Y.; Wei, L.; Chen, Z.; Yang, B. Low serum calcium: A new, important indicator of COVID-19 patients from mild/moderate to severe/critical. Biosci. Rep. 2020, 40, 20202690. [Google Scholar] [CrossRef]
- Zhang, J.; Taylor, E.W.; Bennett, K.; Saad, R.; Rayman, M.P. Association between regional selenium status and reported outcome of COVID-19 cases in China. Am. J. Clin. Nutr. 2020, 111, 1297–1299. [Google Scholar] [CrossRef]
- Majeed, M.; Nagabhushanam, K.; Gowda, S.; Mundkur, L. An Exploratory Study of Selenium Status in Normal Subjects and COVID-19 Patients in South Indian population: Case for Adequate Selenium Status: Selenium Status in COVID-19 Patients. Nutrition 2020, 11, 111053. [Google Scholar] [CrossRef]
- Heller, R.A.; Sun, Q.; Hackler, J.; Seelig, J.; Seibert, L.; Cherkezov, A.; Minich, W.B.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker. Redox Biol. 2020, 38, 101764. [Google Scholar] [CrossRef]
- Bermano, G.; Méplan, C.; Mercer, D.K.; Hesketh, J.E. Selenium and viral infection: Are there lessons for COVID-19? Br. J. Nutr. 2021, 125, 618–627. [Google Scholar] [CrossRef]
- Hiffler, L.; Rakotoambinina, B. Selenium and RNA Virus Interactions: Potential Implications for SARS-CoV-2 Infection (COVID-19). Front. Nutr. 2020, 7, 164. [Google Scholar] [CrossRef] [PubMed]
- Bolondi, G.; Russo, E.; Gamberini, E.; Circelli, A.; Meca, M.C.C.; Brogi, E.; Viola, L.; Bissoni, L.; Poletti, V.; Agnoletti, V. Iron metabolism and lymphocyte characterisation during Covid-19 infection in ICU patients: An observational cohort study. World J. Emerg. Surg. 2020, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Chen, Y.; Ji, Y.; He, X.; Xue, D. Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19. Med. Sci. Monit. 2020, 26, 926178. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Frost, J.N.; Aaron, L.; Donovan, K.; Drakesmith, H.; Collaborators. Systemic hypoferremia and severity of hypoxemic respiratory failure in COVID-19. Crit. Care 2020, 24, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Jothimani, D.; Kailasam, E.; Danielraj, S.; Nallathambi, B.; Ramachandran, H.; Sekar, P.; Manoharan, S.; Ramani, V.; Narasimhan, G.; Kaliamoorthy, I.; et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int. J. Infect. Dis. 2020, 100, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Anuk, A.T.; Polat, N.; Akdas, S.; Erol, S.A.; Tanacan, A.; Biriken, D.; Keskin, H.L.; Tekin, O.M.; Yazihan, N.; Sahin, D. The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection during Pregnancy. Biol. Trace Element Res. 2020, 24, 1–10. [Google Scholar] [CrossRef]
- Wessels, I.; Rolles, B.; Rink, L. The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis. Front. Immunol. 2020, 11, 1712. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, P.M.; Ahuja, T.; Petrilli, C.; Rajagopalan, H.; Jones, S.; Rahimian, J. Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients. J. Med. Microbiol. 2020, 69, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.S.; Paguio, J.A.; Dee, E.C.; Tan, H.C.; Moulick, A.; Milazzo, C.; Jurado, J.; Della Penna, N.; Celi, L.A. The Minimal Effect of Zinc on the Survival of Hospitalized Patients With COVID-19: An Observational Study. Chest 2020, 22, 108–111. [Google Scholar] [CrossRef]
- Pal, A.; Squitti, R.; Picozza, M.; Pawar, A.; Rongioletti, M.; Dutta, A.K.; Sahoo, S.; Goswami, K.; Sharma, P.; Prasad, R. Zinc and COVID-19: Basis of Current Clinical Trials. Biol. Trace Elem. Res. 2020, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, F.; Brivio, R.; Casati, M.; Cavallero, A.; Contro, E.; Brambilla, P. Low levels of total and ionized calcium in blood of COVID-19 patients. Clin. Chem. Lab. Med. 2020, 58, e171–e173. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Han, P.; Wu, J.; Gong, J.; Tian, D. Prevalence and predictive value of hypocalcemia in severe COVID-19 patients. J. Infect. Public Health 2020, 13, 1224–1228. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, L.; Formenti, A.M.; Giustina, A. Hypocalcemia: The quest for the cause of a major biochemical feature of COVID-19. Endocrine 2020, 70, 463–464. [Google Scholar] [CrossRef]
- Torres, B.; Alcubilla, P.; González-Cordón, A.; Inciarte, A.; Chumbita, M.; Cardozo, C.; Meira, F.; Giménez, M.; de Hollanda, A.; Soriano, A. COVID19 Hospital Clínic Infectious Diseases research group. Impact of low serum calcium at hospital admission on SARS-CoV-2 infection outcome. Int. J. Infect. Dis. 2020, 2. [Google Scholar] [CrossRef]
- Yang, C.; Ma, X.; Wu, J.; Han, J.; Zheng, Z.; Duan, H.; Liu, Q.; Wu, C.; Dong, Y.; Dong, L. Low serum calcium and phosphorus and their clinical performance in detecting COVID-19 patients. J. Med. Virol. 2020, 93, 1639–1651. [Google Scholar] [CrossRef]
- Di Filippo, L.; Formenti, A.M.; Rovere-Querini, P.; Carlucci, M.; Conte, C.; Ciceri, F.; Zangrillo, A.; Giustina, A. Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19. Endocrine 2020, 68, 475–478. [Google Scholar] [CrossRef]
- Pereira, T.C.B.; Campos, M.M.; Bogo, M.R. Copper toxicology, oxidative stress and inflammation using zebrafish as experimental model. J. Appl. Toxicol. 2016, 36, 876–885. [Google Scholar] [CrossRef]
- Osredkar, J.; Sustar, N. Copper and Zinc, Biological Role and Significance of Copper/Zinc Imbalance. J. Clin. Toxicol. 2011, s3, 0495. [Google Scholar] [CrossRef] [Green Version]
- MalavoltaRobertina, M.; Giacconi, R.; Piacenza, F.; Santarelli, L.; Cipriano, C.; Costarelli, L.; Tesei, S.; Pierpaoli, S.; Basso, A.; Galeazzi, R.; et al. Plasma copper/zinc ratio: An inflammatory/nutritional biomarker as predictor of all-cause mortality in elderly population. Biogerontology 2010, 11, 309–319. [Google Scholar] [CrossRef]
- Laine, J.T.; Tuomainen, T.-P.; Salonen, J.T.; Virtanen, J.K. Serum copper-to-zinc-ratio and risk of incident infection in men: The Kuopio Ischaemic Heart Disease Risk Factor Study. Eur. J. Epidemiol. 2020, 35, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Temporary Methodologic Guidelines “Prophylaxis, Diagnosis, and Treatment of Novel Coronavirus Infection (COVID-19), v. 7 (03.06. 2020). Available online: http://edu.rosminzdrav.ru/fileadmin/user_upload/specialists/COVID-19/MR_COVID-19_v7.pdf (accessed on 24 August 2020).



| Parameter | Control | Mild | Moderate | Severe | Trend p |
|---|---|---|---|---|---|
| SatO2, % | 97.98 ± 0.83 | 95.43 ± 1.81 | 94.76 ± 2.15 1 | 86.98 ± 8.55 1,2,3 | <0.001 |
| HR, per min | 73.23 ± 6.22 | 83.02 ± 14.94 1 | 84.43 ± 10.64 1 | 86.94 ± 13.23 1 | <0.001 |
| RR, per min | 18 ± 1.54 | 19.74 ± 2.22 1 | 19.94 ± 2.29 1 | 22.15 ± 4.69 1,2,3 | <0.001 |
| Fever, t °Cmax | 36.6 ± 0.09 | 38.21 ± 0.68 1 | 38.12 ± 0.63 1 | 38.32 ± 0.8 1 | <0.001 |
| Lung damage, % | - | 26.22 ± 10.33 | 39.7 ± 16.15 2 | 57.9 ± 17.11 2,3 | <0.001 |
| CRP, mg/L | 1.95 ± 1.29 | 44.57 ± 65.28 1 | 67 ± 66.34 1,2 | 161.28 ± 88.61 1,2,3 | <0.001 |
| Parameter | Control | Mild | Moderate | Severe | Trend p |
|---|---|---|---|---|---|
| Total protein, g/L | 77.61 ± 3.87 | 71.66 ± 6.36 1 | 71.72 ± 7.2 1 | 66.21 ± 6.76 1,2,3 | <0.001 |
| Total bilirubin, µmol/L | 13.27 ± 6.46 | 10.15 ± 4.11 | 10.6 ± 6.81 | 10.4 ± 5.05 | 0.074 |
| Creatinine, µmol/L | 86.31 ± 10.18 | 99.57 ± 34.53 | 92.95 ± 20.30 | 99.11 ± 39.03 | 0.534 |
| Glucose, mmol/L | 5.4 ± 0.58 | 5.6 ± 1.06 | 5.79 ± 1.62 | 7.15 ± 3.48 1,2,3 | <0.001 |
| AST, U/L | 25.44 ± 7.37 | 39.69 ± 27.98 1 | 44.1 ± 38.96 1 | 51.54 ± 30.43 1,2 | <0.001 |
| ALT, U/L | 23.23 ± 9.12 | 47.56 ± 51.39 1 | 50.98 ± 61.56 1 | 54.34 ± 63.65 1 | <0.001 |
| INR | 0.97 ± 0.08 | 1.17 ± 0.09 1 | 1.19 ± 0.09 1 | 1.32 ± 0.23 1,2,3 | <0.001 |
| PT, s | 13.93 ± 1.06 | 13.06 ± 1.63 | 14.22 ± 8.18 | 14.37 ± 2.53 | 0.078 |
| Prothrombin, % | 101.02 ± 6.12 | 80.83 ± 8.08 1 | 76.71 ± 12.43 1 | 71.49 ± 14.83 1,2 | <0.001 |
| APTT, ratio | 1.02 ± 0.11 | 1.04 ± 0.14 | 1.06 ± 0.13 | 1.05 ± 0.2 | 0.722 |
| Fibrinogen, g/L | 2.67 ± 0.64 | 5.32 ± 2.15 1 | 5.62 ± 1.86 1 | 7.44 ± 2.9 1,2,3 | <0.001 |
| Parameter | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Ca | 0.110 | 0.090 | 0.017 | 0.765 | 0.014 | 0.789 |
| Cu | −0.911 | <0.001 * | −0.832 | <0.001 * | −0.602 | 0.001 * |
| Fe | 0.179 | 0.009 * | 0.081 | 0.177 | 0.103 | 0.068 |
| Se | 0.022 | 0.772 | −0.078 | 0.235 | −0.037 | 0.548 |
| Zn | 0.726 | <0.001 * | 0.707 | <0.001 * | 0.533 | <0.001 * |
| Cu/Zn | −1.378 | <0.001 * | −1.120 | <0.001 * | −0.789 | <0.001 * |
| Age | - | - | 0.005 | 0.930 | 0.043 | 0.427 |
| Gender | - | - | −0.330 | <0.001 * | −0.269 | <0.001 * |
| BMI | - | - | 0.038 | 0.504 | 0.103 | 0.055 |
| HR | - | - | −0.027 | 0.664 | −0.004 | 0.945 |
| RR | - | - | −0.055 | 0.380 | 0.012 | 0.838 |
| t °Cmax | - | - | −0.099 | 0.145 | −0.030 | 0.657 |
| Lung damage | - | - | −0.343 | <0.001 * | −0.223 | 0.006 * |
| CRP | - | - | - | - | −0.374 | <0.001 * |
| Total protein | - | - | - | - | −0.128 | 0.053 |
| Glucose | - | - | - | - | −0.069 | 0.212 |
| AST | - | - | - | - | −0.124 | 0.179 |
| ALT | - | - | - | - | 0.123 | 0.165 |
| INR | - | - | - | - | −0.114 | 0.133 |
| PT | - | - | - | - | 0.048 | 0.379 |
| Fibrinogen | - | - | - | - | 0.039 | 0.611 |
| Multiple R | 0.505 | 0.706 | 0.771 | |||
| Multiple R2 | 0.255 | 0.498 | 0.594 | |||
| Adjusted R2 | 0.231 | 0.462 | 0.544 | |||
| p for a model | <0.001 * | <0.001 * | <0.001 * | |||
| − | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Ca | −0.242 | <0.001 * | −0.116 | 0.029 * | −0.082 | 0.098 |
| Cu | −0.143 | 0.485 | 0.096 | 0.597 | 0.158 | 0.360 |
| Fe | −0.125 | 0.060 | 0.025 | 0.661 | 0.039 | 0.455 |
| Se | −0.114 | 0.125 | −0.117 | 0.057 | −0.121 | 0.033 * |
| Zn | 0.160 | 0.352 | −0.115 | 0.450 | −0.123 | 0.385 |
| Cu/Zn | 0.561 | 0.026 * | 0.040 | 0.860 | −0.042 | 0.844 |
| Age | - | - | −0.036 | 0.498 | −0.073 | 0.151 |
| Gender | - | - | −0.036 | 0.540 | −0.112 | 0.056 |
| BMI | - | - | 0.112 | 0.033 * | 0.058 | 0.247 |
| HR | - | - | 0.071 | 0.229 | 0.086 | 0.119 |
| RR | - | - | 0.137 | 0.019 * | 0.083 | 0.130 |
| t °Cmax | - | - | 0.251 | <0.001 * | 0.100 | 0.112 |
| SpO2 | - | - | −0.302 | <0.001 * | −0.193 | 0.006 * |
| CRP | - | - | - | - | 0.080 | 0.344 |
| Total protein | - | - | - | - | −0.174 | 0.004 * |
| Glucose | - | - | - | - | 0.064 | 0.214 |
| AST | - | - | - | - | −0.090 | 0.295 |
| ALT | - | - | - | - | 0.138 | 0.092 |
| INR | - | - | - | - | 0.231 | 0.001 * |
| PT | - | - | - | - | −0.012 | 0.806 |
| Fibrinogen | - | - | - | - | 0.031 | 0.671 |
| Multiple R | 0.553 | 0.747 | 0.805 | |||
| Multiple R2 | 0.306 | 0.559 | 0.648 | |||
| Adjusted R2 | 0.284 | 0.527 | 0.605 | |||
| p for a model | <0.001 * | <0.001 * | <0.001 * | |||
| Parameter | Control | Mild | Moderate | Severe |
|---|---|---|---|---|
| Age, y.o. | 55.67 ± 4.36 | 50.47 ± 15.91 | 54.22 ± 12.5 | 64.5 ± 15.49 |
| Height, cm | 1.72 ± 0.07 | 168.64 ± 8.75 | 171.12 ± 11.63 | 170.19 ± 8.54 |
| Weight, kg | 78.09 ± 9.01 | 85.52 ± 23.08 | 93.88 ± 19.5 | 88.82 ± 16.09 |
| BMI | 26.24 ± 2.29 | 30.06 ± 8.35 | 32.09 ± 5.96 | 30.31 ± 5.4 |
| Gender, m/f | 27/16 (63%/37%) | 25/25 (50%/50%) | 31/19 (62%/38%) | 25/25 (50%/50%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skalny, A.V.; Timashev, P.S.; Aschner, M.; Aaseth, J.; Chernova, L.N.; Belyaev, V.E.; Grabeklis, A.R.; Notova, S.V.; Lobinski, R.; Tsatsakis, A.; et al. Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers. Metabolites 2021, 11, 244. https://doi.org/10.3390/metabo11040244
Skalny AV, Timashev PS, Aschner M, Aaseth J, Chernova LN, Belyaev VE, Grabeklis AR, Notova SV, Lobinski R, Tsatsakis A, et al. Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers. Metabolites. 2021; 11(4):244. https://doi.org/10.3390/metabo11040244
Chicago/Turabian StyleSkalny, Anatoly V., Peter S. Timashev, Michael Aschner, Jan Aaseth, Lyubov N. Chernova, Vladimir E. Belyaev, Andrey R. Grabeklis, Svetlana V. Notova, Ryszard Lobinski, Aristides Tsatsakis, and et al. 2021. "Serum Zinc, Copper, and Other Biometals Are Associated with COVID-19 Severity Markers" Metabolites 11, no. 4: 244. https://doi.org/10.3390/metabo11040244