Utilization of a 3D Printed Orthodontic Distalizer for Tooth-Borne Hybrid Treatment in Class II Unilateral Malocclusions
Abstract
:1. Introduction
- patient compliance can be improved with aesthetical and comfortable devices;
- combination of CAT and fixed orthodontic devices can result in optimized patient adherence to therapy, reducing the time required to wear Class II elastics;
- treatment effectivity can be improved by the employment of a fixed appliance.
2. Materials and Methods
2.1. Digital Workflow for Personalized 3D Design and Printing
2.2. Patients—Selection Criteria
- Patients must be adults;
- Unilateral Class II occlusion measurable on molars and canines with a class I relationship on the opposite side and no skeletal Class II values (Figure 4);
- Skeletal cephalometric values of SNA = 81 ± 3°, SNB = 78 ± 3°, ANB = 3 ± 2°;
- Target of planned linear distance of the frontal cusp of upper molar translation (distalization and distorotation) had to be between 2.5 and 6 mm (Figure 5);
- Patients were compliant with dental monitoring on a weekly basis;
- Patients had a distalizer combined with CAT (all patients were using an Invisalign type of appliance).
2.3. Materials, Handling, 3D Printing and Post-Printing Protocols
Post-Processing after 3D Printing
2.4. 3D Printing and Costs
2.5. Method of Digital Design of the Personalized Orthodontic Distalizer
- The first step is to register an intraoral situation with a digital intraoral scan and exporting it in a common 3D format. For example, the STL file format is suitable and can be processed in various simple 3D modelling programs like Meshmixer (from Autodesk).
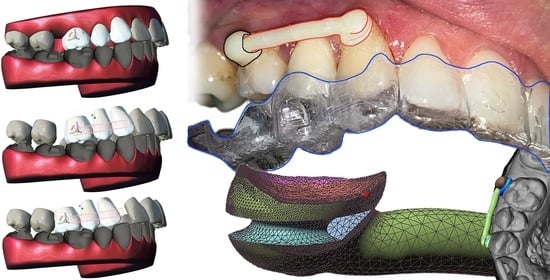
- The second step is to coordinate the distalizer and CAT planned effects and plan the placement of distalizer in harmony with CAT. In this research, all CAT were performed using Invisalign appliances (Figure 6).
- The third step was to design the body of the distalizer, including movable joints and individual bases on the terminal pads of the distalizer.
- The fourth step was clinical application and distalizer activation followed by weeks of movement Dental monitoring.
- The fifth step was performed after achieving planned occlusal correction. Removal of the distalizer was followed by stabilization of the result.
Elastic Bands Attachment and Distalizer Activation
2.6. Practical Aspects of Post-Prints Handling
2.7. Method of Clinical Application
3. Results
- A total of seven failures consisted of four debonding incidents and three breaks of material;
- Only in two patients did double failure happen (one debonding and one breaking);
- Both patients with double failures preferred the same material in the final question;
- Another three failures were separate incidents in separate patients.
4. Discussion
- reduce strictness of clinical conditions like I. skeletal class patients or bilateral distalization situations;
- or prolong the research for more years.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3D | Three-Dimensional |
| AM | Additive Manufacturing |
| CAT | Clear Aligner Therapy |
| CDA | Carriere Distalizer Appliance |
| CMA | Carriere Motion 3D Appliance (Another name for CDA. Table of used abbreviations in alphabetical order.) |
| STL | Standard Tessellation Language, describes only the surface geometry of a three-dimensional object without any representation of colour or texture |
References
- Huang, H.-M. Medical Application of Polymer-Based Composites. Polymers 2020, 12, 2560. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Vallittu, P.K.; Özcan, M. Fiber-Reinforced Composites for Dental Applications. BioMed Res. Int. 2018, 2018, 4734986. [Google Scholar] [CrossRef] [PubMed]
- Burgard, N.; Kienitz, M.; Jourdan, C.; Rüttermann, S. The Influence of Modified Experimental Dental Resin Composites on the Initial in Situ Biofilm—A Triple-Blinded, Randomized, Controlled Split-Mouth Trial. Polymers 2021, 13, 2814. [Google Scholar] [CrossRef] [PubMed]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and Machinable Dental Restorative Composites for CAD/CAM Application—Comparison of Mechanical Properties, Fractographic, Texture and Fractal Dimension Analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.-J.; Park, J.-M.; Kim, T.-H.; Ahn, J.-S.; Cha, H.-S.; Lee, J.-H. 3D Printing of Resin Material for Denture Artificial Teeth: Chipping and Indirect Tensile Fracture Resistance. Materials 2018, 11, 1798. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Vallittu, P.K.; Lassila, L.V.J.; Viola, A.; Gandini, P.; Scribante, A. Glass Fiber Reinforced Composite Orthodontic Retainer: In Vitro Effect of Tooth Brushing on the Surface Wear and Mechanical Properties. Materials 2020, 13, 1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Yang, J.; Jia, Y.-G.; Lu, B.; Ren, L. A Study of 3D-Printable Reinforced Composite Resin: PMMA Modified with Silver Nanoparticles Loaded Cellulose Nanocrystal. Materials 2018, 11, 2444. [Google Scholar] [CrossRef] [Green Version]
- Tappa, K.; Jammalamadaka, U. Novel Biomaterials Used in Medical 3D Printing Techniques. J. Funct. Biomater. 2018, 9, 17. [Google Scholar] [CrossRef] [Green Version]
- Melo, M.A. Bacterial Interactions with Dental and Medical Materials. J. Funct. Biomater. 2020, 11, 83. [Google Scholar] [CrossRef]
- Mai, H.-N.; Hyun, D.C.; Park, J.H.; Kim, D.-Y.; Lee, S.M.; Lee, D.-H. Antibacterial Drug-Release Polydimethylsiloxane Coating for 3D-Printing Dental Polymer: Surface Alterations and Antimicrobial Effects. Pharmaceuticals 2020, 13, 304. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Bajaj, D.; Siena, F.L.; Breedon, P. Effects of post-curing conditions on mechanical properties of 3D printed clear dental aligners. Rapid Prototyp. J. 2020, 26, 1337–1344. [Google Scholar] [CrossRef]
- Vasques, M.T.; Mori, M.; Laganá, D.C. Three-dimensional printing of occlusal devices for temporomandibular disorders by using a free CAD software program: A technical report. J. Prosthet. Dent. 2020, 123, 232–235. [Google Scholar] [CrossRef]
- Milovanović, A.; Sedmak, A.; Golubović, Z.; Mihajlović, K.Z.; Žurkić, A.; Trajković, I.; Milošević, M. The effect of time on mechanical properties of biocompatible photopolymer resins used for fabrication of clear dental aligners. J. Mech. Behav. Biomed. Mater. 2021, 119, 104494. [Google Scholar] [CrossRef]
- Scribante, A.; Gallo, S.; Turcato, B.; Trovati, F.; Gandini, P.; Sfondrini, M.F. Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial. Polymers 2020, 12, 963. [Google Scholar] [CrossRef] [Green Version]
- Sfondrini, M.F.; Gallo, S.; Turcato, B.; Montasser, M.A.; Albelasy, N.F.; Vallittu, P.K.; Gandini, P.; Scribante, A. Universal Adhesive for Fixed Retainer Bonding: In Vitro Evaluation and Randomized Clinical Trial. Materials 2021, 14, 1341. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Moray, L.J. Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the NHANES III survey. Int. J. Adult Orthod. Orthognath. Surg. 1998, 13, 97–106. [Google Scholar] [PubMed]
- Ke, Y.; Zhu, Y.; Zhu, M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth move-ment: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef] [Green Version]
- Nanda, R.; Garino, F.; Ojima, K.; Castroflorio, T.; Parrini, S. Chapter 12: The hybrid approach in Class II malocclusions treatment. In Principles and Biomechanics of Aligner Treatment—E-Book, 1st ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2021; Volume 1, pp. 149–160. ISBN 9780323683838. [Google Scholar]
- Bolla, E.; Muratore, F.; Carano, A.; Bowman, S.J. Evaluation of maxillary molar distalization with the distal jet a comparison with other contemporary methods. Angle Orthod. 2002, 72, 481–494. [Google Scholar]
- Grec, R.H.; Janson, G.; Branco, N.C.; Moura-Grec, P.G.; Patel, M.P.; Henriques, J.F.C. Intraoral distalizer effects with conventional and skeletal anchorage a meta-analysis. Am. J. Orthod. Dentofacial Orthop. 2013, 143, 602–615. [Google Scholar] [CrossRef]
- Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; Deregibus, A. Maxillary molar distalization with aligners in adult patients a multicenter retrospective study. Prog. Orthod. 2016, 17, 12. [Google Scholar] [CrossRef] [Green Version]
- Barakat, D.; Bakdach, W.M.; Youssef, M. Treatment effects of Carriere Motion Appliance on patients with Class II malocclusion: A systematic review and meta-analysis. Int. Orthod. 2021, 19, 353–364. [Google Scholar] [CrossRef]
- Scribante, A.; Gallo, S.; Bertino, K.; Meles, S.; Gandini, P.; Sfondrini, M.F. The Effect of Chairside Verbal Instructions Matched with Instagram Social Media on Oral Hygiene of Young Orthodontic Patients: A Randomized Clinical Trial. Appl. Sci. 2021, 11, 706. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Deregibus, A.; Castroflorio, T. Controlling orthodontic tooth movement with clear aligners. An updated systematic review regarding efficacy and efficiency. J. Aligner Orthod. 2017, 1, 7–20. [Google Scholar]
- Garino, F.; Castroflorio, T.; Daher, S.; Ravera, S.; Rossini, G.; Cugliari, G.; Deregibus, A. Effectiveness of composite attachments in controlling upper-molar movement with aligners. J. Clin. Orthod. 2016, 50, 341–347. [Google Scholar]
- Richter, D.D.; Nanda, R.S.; Sinha, P.K.; Smith, D.W. Effect of behavior modification on patient compliance in orthodontics. Angle Orthod. 1998, 68, 123–132. [Google Scholar]
- Lombardo, L.; Colonna, A.; Carlucci, A.; Oliverio, T.; Siciliani, G. Class II subdivision correction with clear aligners using intermaxilary elastics. Prog. Orthod. 2018, 1, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Nedwed, V.; Miethke, R.R. Motivation, acceptance and problems of invisalign patients. J. Orofac. Orthop. 2005, 66, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 276.e1–276.e12. [Google Scholar] [CrossRef] [PubMed]
- Shah, N. Compliance with removable orthodontic appliances. Evid. Based Dent. 2017, 18, 105–106. [Google Scholar] [CrossRef] [PubMed]
- Carano, A.; Testa, M. The distal jet for upper molar distalization. J. Clin. Orthod. 1996, 30, 374–380. [Google Scholar]
- Antonarakis, G.S.; Kiliaridis, S. Maxillary molar distalization with noncompliance intramaxillary appliances in Class II malocclusion a systematic review. Angle Orthod. 2008, 78, 1133–1140. [Google Scholar] [CrossRef] [Green Version]
- Carano, A.; Testa, M.; Siciliani, G. The lingual distalizer system. Eur. J. Orthod. 1996, 18, 445–448. [Google Scholar] [CrossRef]
- Hilgers, J.J. The pendulum appliance for Class II noncompliance therapy. J. Clin. Orthod. 1992, 26, 706–714. [Google Scholar]
- Marure, P.S.; Patil, R.U.; Reddy, S.; Prakash, A.; Kshetrimayum, N.; Shukla, R. The effectiveness of pendulum, K-loop, and distal jet distalization techniques in growing children and its effects on anchor unit a comparative study. J. Indian Soc. Pedod. Prev. Dent. 2016, 34, 331–340. [Google Scholar]
- Byloff, F.K.; Darendeliler, M.A.; Clar, E.; Darendeliler, A. Distal molar movement using the pendulum appliance. Part 2 the effects of maxillary molar root uprighting bends. Angle Orthod. 1997, 67, 261–270. [Google Scholar]
- Chaqués-Asensi, J.; Kalra, V. Effects of the pendulum appliance on the dentofacial complex. J. Clin. Orthod. 2001, 35, 254–257. [Google Scholar]
- Byloff, F.K.; Darendeliler, M.A. Distal molar movement using the pendulum appliance. Part 1 clinical and radiological evaluation. Angle Orthod. 1997, 67, 249–260. [Google Scholar]
- Ghosh, J.; Nanda, R.S. Evaluation of an intraoral maxillary molar distalization technique. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 639–646. [Google Scholar] [CrossRef]
- Carrière, L. A new Class II distalizer. J. Clin. Orthod. 2004, 38, 224–231. [Google Scholar]
- Martel, D. The Carriere distalizer simple and efficient. Int. J. Orthod. 2012, 23, 63–66. [Google Scholar]
- Rodríguez, H.L. Unilateral application of the Carriere distalizer. J. Clin. Orthod. 2011, 45, 177–180. [Google Scholar]
- Sandifer, C.L.; English, J.D.; Colville, C.D.; Gallerano, R.L.; Akyalcin, S. Treatment effects of the Carrière distalizer using lingual arch and full fixed appliances. J. World Fed. Orthod. 2014, 3, e49–e54. [Google Scholar] [CrossRef]
- Nanda, R. Biomechanics in Clinical Orthodontics; WB Saunders: Philadelphia, PA, USA, 1997. [Google Scholar]
- Yin, K.; Han, E.; Guo, J.; Yasumura, T.; Grauer, D.; Sameshima, G. Evaluating the treatment effectiveness and efficiency of Carriere Distalizer: A cephalometric and study model comparison of Class II appliances. Prog. Orthod. 2019, 20, 24. [Google Scholar] [CrossRef] [PubMed]
- Kim-Berman, H.; McNamara, J.A., Jr.; Lints, J.P.; McMullen, C.; Franchi, L. Treatment effects of the Carriere® Motion 3D™ appliance for the correction of Class II malocclusion in adolescents. Angle Orthod. 2019, 89, 839–846. [Google Scholar] [CrossRef] [Green Version]
- Khosravi, R.; Cohanim, B.; Hujoel, P.; Daher, S.; Neal, M.; Liu, W.; Huang, G. Management of overbite with the Invisalign appliance. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 691–699. [Google Scholar] [CrossRef]
- Mantovani, E.; Parrini, S.; Coda, E.; Cugliari, G.; Scotti, N.; Pasqualini, D.; Deregibus, A.; Castroflorio, T. Micro computed tomography evaluation of Invisalign aligner thickness homogeneity. Angle Orthod. 2021, 91, 343–348. [Google Scholar] [CrossRef]
- Kinzinger, G.S.; Wehrbein, H.; Gross, U.; Diedrich, P.R. Molar distalization with pendulum appliances in the mixed dentition effects on the position of unerupted canines and premolars. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 407–417. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, B. Class II Correction Prior to Orthodontics with the Carriere Distalizer. Int. J. Orthod. 2013, 24, 35–36. [Google Scholar]
- Ahmed, S.H. Three dimensional assessment of the long-term treatment stability after maxillary first molar distalization with Carriere distalizer appliance. Life Sci. J. 2020, 17, 83–90. Available online: http://www.lifesciencesite.com/lsj/lsj170220/12_36058lsj170220_83_90.pdf (accessed on 10 October 2021). [CrossRef]
- Wilson, B.; Konstantoni, N.; Kim, K.B.; Foley, P.; Ueno, H. Three-dimensional cone-beam computed tomography comparison of shorty and standard Class II Carriere Motion appliance. Angle Orthod. 2021, 91, 423–432. [Google Scholar] [CrossRef]
- Hamilton, C.F.; Saltaji, H.; Preston, C.B.; Flores-Mir, C.; Tabbaa, S. Adolescent patients’ experience with the Carriere distalizer appliance. Eur. J. Paediatr. Dent. 2013, 14, 219–224. [Google Scholar]
- Areepong, D.; Kim, K.B.; Oliver, D.R.; Ueno, H. The Class II Carriere Motion appliance: A 3D CBCT evaluation of the effects on the dentition. Angle Orthod. 2020, 90, 491–499. [Google Scholar] [CrossRef] [Green Version]
- Gupta, D.K.; Tuli, A.; Jain, A. 3D printed material application in orthodontics. Mater. Today Proc. 2020, 28 Pt 3, 1635–1642. [Google Scholar] [CrossRef]
- Eliades, T.; Zinelis, S. Three-dimensional printing and in-house appliance fabrication: Between innovation and stepping into the unknown. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, F.D.F.; Briso, A.L.F.; Ramos, F.d.S.e.S.; Esteves, L.M.B.; Omoto, É.M.; Sundfeld, R.H.; Fagundes, T.C. Use of auxiliary devices during retreatment of direct resin composite veneers. PLoS ONE 2021, 16, e0252171. [Google Scholar] [CrossRef]
- Technical Data Sheet—Dental LT Clear (V2). Available online: https://formlabs-media.formlabs.com/datasheets/2001429-TDS-ENUS-0.pdf (accessed on 10 October 2021).
- Formlabs Denture Resins—PKG-RS-F2-DT. Available online: https://dental.formlabs.com/store/denture-teeth-resin-1l/ (accessed on 10 October 2021).
- Form Cure Time and Temperature Settings. Available online: https://s3.amazonaws.com/servicecloudassets.formlabs.com/media/Finishing/Post-Curing/115001414464-Form%20Cure%20Time%20and%20Temperature%20Settings/FormCurePost-CureSettings.pdf (accessed on 10 October 2021).
- Safety Data Sheet—Dental LT Clear (V2). Available online: https://formlabs-media.formlabs.com/datasheets/2001421-SDS-ENEU-0.pdf (accessed on 10 October 2021).
- Safety Data Sheet—Denture Teeth. Available online: https://formlabs-media.formlabs.com/datasheets/1902185-SDS-ENEU-0.pdf (accessed on 10 October 2021).
- Technical Data Sheet—Denture Base and Teeth. Available online: https://dental-media.formlabs.com/datasheets/1802131-TDS-ENEU-0.pdf (accessed on 10 October 2021).
- Form 2—3D Printer Technical Data Sheet—Online. Available online: https://formlabs.com/3d-printers/form-2 (accessed on 10 October 2021).
- Cha, H.S.; Park, J.M.; Kim, T.H.; Lee, J.H. Wear Resistance of 3D-Printed Denture Tooth Resin Opposing Zirconia and Metal Antagonists. J. Prosthet. Dent. 2020, 124, 387–394. [Google Scholar] [CrossRef]
- Espinar-Escalona, E.; Barrera-Mora, J.M.; Llamas-Carreras, J.M.; Solano-Reina, E.; Rodríguez, D.; Gil, F.J. Improvement in adhesion of the brackets to the tooth by sandblasting treatment. J. Mater. Sci. Mater. Med. 2012, 23, 605–611. [Google Scholar] [CrossRef]
- Goracci, C.; Cacciatore, G. Early treatment of a severe Class II malocclusion with the Forsus fatigue resistant device. Eur. J. Paediatr. Dent. 2017, 18, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Graf, S.; Vasudavan, S.; Wilmes, B. CAD/CAM Metallic Printing of a Skeletally Anchored Upper Molar Distalizer. J. Clin. Orthod. 2020, 54, 140–150. [Google Scholar] [PubMed]
- Thurzo, A.; Kočiš, F.; Novák, B.; Czako, L.; Varga, I. Three-Dimensional Modeling and 3D Printing of Biocompatible Orthodontic Power-Arm Design with Clinical Application. Appl. Sci. 2021, 11, 9693. [Google Scholar] [CrossRef]
- Tamaya, N.; Kawamura, J.; Yanagi, Y. Tooth Movement Efficacy of Retraction Spring Made of a New Low Elastic Modulus Material, Gum Metal, Evaluated by the Finite Element Method. Materials 2021, 14, 2934. [Google Scholar] [CrossRef]
- Thurzo, A.; Kosnáčová, H.S.; Kurilová, V.; Kosmeľ, S.; Beňuš, R.; Moravanský, N.; Kováč, P.; Kuracinová, K.M.; Palkovič, M.; Varga, I. Use of Advanced Artificial Intelligence in Forensic Medicine, Forensic Anthropology and Clinical Anatomy. Healthcare 2021, 9, 1545. [Google Scholar] [CrossRef]
- Dalessandri, D.; Sangalli, L.; Tonni, I.; Laffranchi, L.; Bonetti, S.; Visconti, L.; Signoroni, A.; Paganelli, C. Attitude towards Telemonitoring in Orthodontists and Orthodontic Patients. Dent. J. 2021, 9, 47. [Google Scholar] [CrossRef]
- Federici Canova, F.; Oliva, G.; Beretta, M.; Dalessandri, D. Digital (R)Evolution: Open-Source Softwares for Orthodontics. Appl. Sci. 2021, 11, 6033. [Google Scholar] [CrossRef]
- Zinelis, S.; Panayi, N.; Polychronis, G.; Papageorgiou, S.N.; Eliades, T. Comparative analysis of mechanical properties of orthodontic aligners produced by different contemporary 3D printers. Orthod. Craniofacial Res. 2021, 1–6. [Google Scholar] [CrossRef]
- Urbanova, W.; Klimova, I.; Brudnicki, A.; Polackova, P.; Kroupova, D.; Dubovska, I.; Rachwalski, M.; Fudalej, P.S. The Slav-Cleft: A Three-Center Study of the Outcome of Treatment of Cleft Lip and Palate. Part 1: Craniofacial Morphology. J. Cranio-Maxillofac. Surg. 2016, 44, 1767–1776. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Pascadopoli, M.; Gallo, S.; Ricaldone, F.; Kramp, D.D.; Valla, M.; Gandini, P.; Scribante, A. Effect of Enamel Pretreatment with Pastes Presenting Different Relative Dentin Abrasivity (RDA) Values on Orthodontic Bracket Bonding Efficacy of Microfilled Composite Resin: In Vitro Investigation and Randomized Clinical Trial. Materials 2022, 15, 531. [Google Scholar] [CrossRef]
- Miletić, I.; Baraba, A.; Basso, M.; Pulcini, M.G.; Marković, D.; Perić, T.; Ozkaya, C.A.; Turkun, L.S. Clinical Performance of a Glass-Hybrid System Compared with a Resin Composite in the Posterior Region: Results of a 2-Year Multicenter Study. J. Adhes. Dent. 2020, 22, 235–247. [Google Scholar] [CrossRef]
- Alifui-Segbaya, F.; Varma, S.; Lieschke, G.J.; George, R. Biocompatibility of Photopolymers in 3D Printing. 3D Print. Addit. Manuf. 2017, 4, 185–191. [Google Scholar] [CrossRef] [Green Version]
- Schuster, M.; Turecek, C.; Kaiser, B.; Stampfl, J.; Liska, R.; Varga, F. Evaluation of Biocompatible Photopolymers I: Photoreactivity and Mechanical Properties of Reactive Diluents. J. Macromol. Sci. Part A 2007, 44, 547–557. [Google Scholar] [CrossRef]



















| Mechanical Properties | Post-Cured Post-Cured Dental LT Clear Resin (V2) | Method |
|---|---|---|
| Ultimate Tensile strength | 52 MPa | ASTM D638-10 (type IV) |
| Young’s modulus | 2080 MPa | ASTM D638-10 (type IV) |
| Elongation | 12% | ASTM D638-10 (Type IV) |
| Flexural Strength at 5% Strain | 84 MPa | ASTM D790-15 (Method B) |
| Flexural Modulus | 2300 MPa | ASTM D790-15 (Method B) |
| Hardness Shore D | 78 D | ASTM D2240-15 (Type D |
| Water Absorption | 0.54% | ASTM D570-98 (2018) |
| Properties | Post-Cured Denture Teeth Resin (Shade A2) |
|---|---|
| Density of the material 1 | 1.15 g/cm3 |
| Flexural Strength 2 | 90 Mpa |
| Relative worn volume % of ΔV 3 | 70% |
| Post-Cured Dental LT Clear Resin (V2) | (% w/w) | Post-Cured Denture Teeth Resin (Shade A2) | (% w/w) |
|---|---|---|---|
| 7,7,9-trimethyl-4,13-dioxo-3,14-dioxa-5,12- diazahexadecane-1,16-diyl bismethacrylate | 50–75 | Proprietary methacrylate monomer | 40–60 |
| 2-hydroxyethyl methacrylate | 10–20 | Diurethane dimethacrylate | 30–50 |
| Reaction mass of Bis(1,2,2,6,6-pentamethyl-4-piperidyl) sebacate and Methyl 1,2,2,6,6-pentamethyl-4-piperidyl sebacate | <10 | Trimethylolpropane trimethacrylate | 3–10 |
| Diphenyl (2,4,6- trimethylbenzoyl) phosphine oxide | 1–5 | Initiator | <3 |
| Acrylic acid, monoester with propane-1,2-diol | 0.1–1 | Stabilizer | <1 |
| ethylene dimethacrylate | <10 | Pigment | <0.7 |
| ID | Sex | Age | Distalization Target | Time in Weeks until Target Achieved | Total Failiures 1 | Material Patient Had | What Material a Patient Would Prefer Next Time |
|---|---|---|---|---|---|---|---|
| # | [M/F] | [years] | [mm] | [weeks] | # | [CLEAR/WHITE] | [CLEAR/WHITE] |
| 1 | F | 25 | 2.50 | 19 | 2 | CLEAR | CLEAR |
| 2 | F | 26 | 3.00 | 22 | 2 | WHITE | WHITE |
| 3 | F | 31 | 3.50 | 20 | 0 | WHITE | CLEAR |
| 4 | M | 23 | 3.00 | 24 | 0 | CLEAR | WHITE |
| 5 | M | 29 | 4.50 | 33 | 1 | CLEAR | CLEAR |
| 6 | F | 30 | 4.00 | 32 | 0 | CLEAR | CLEAR |
| 7 | F | 31 | 2.50 | 21 | 0 | WHITE | CLEAR |
| 8 | F | 37 | 3.00 | 25 | 0 | CLEAR | CLEAR |
| 9 | M | 28 | 3.50 | 26 | 0 | WHITE | CLEAR |
| 10 | F | 20 | 5.00 | 30 | 1 | WHITE | CLEAR |
| 11 | F | 21 | 5.50 | 36 | 1 | CLEAR | CLEAR |
| 12 | F | 26 | 3.00 | 20 | 0 | WHITE | CLEAR |
| Variable | Statistics or Category | Group | p-Value | Statistical Test | |
|---|---|---|---|---|---|
| WHITE | CLEAR | ||||
| n | 6 | 6 | n.a. | ||
| Age [years] | mean ± SD | 27.0 ± 4.10 | 27.5 ± 5.79 | 0.866 * | t-test |
| median (range) | 27 (20–31) | 27 (21–37) | |||
| Sex | male | 1 | 2 | 0.591 * | Fisher exact test |
| female | 5 | 4 | |||
| Side of oral cavity | left | 3 | 3 | 0.999 * | Fisher exact test |
| right | 3 | 3 | |||
| Distance to distalization target [mm] | mean ± SD | 3.42 ± 0.861 | 3.75 ± 1.129 | 0.578 | t-test |
| median (range) | 3.25 (2.5–5.0) | 3.5 (2.5–5.5) | |||
| Time until target achieved [weeks] | mean ± SD | 23.2 ± 4.01 | 28.2 ± 6.49 | 0.223 | Mann–Whitney test |
| median (range) | 21.5 (20–30) | 28.5 (19–36) | |||
| Total failures a | Mean b (Poisson CI) | 0.5 (0.10–1.46) | 0.67 (0.18–1.71) | 0.706 | Poisson regression |
| Material preference | white | 1 | 1 | 0.999 | Fisher exact test |
| clear | 6 | 6 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thurzo, A.; Urbanová, W.; Novák, B.; Waczulíková, I.; Varga, I. Utilization of a 3D Printed Orthodontic Distalizer for Tooth-Borne Hybrid Treatment in Class II Unilateral Malocclusions. Materials 2022, 15, 1740. https://doi.org/10.3390/ma15051740
Thurzo A, Urbanová W, Novák B, Waczulíková I, Varga I. Utilization of a 3D Printed Orthodontic Distalizer for Tooth-Borne Hybrid Treatment in Class II Unilateral Malocclusions. Materials. 2022; 15(5):1740. https://doi.org/10.3390/ma15051740
Chicago/Turabian StyleThurzo, Andrej, Wanda Urbanová, Bohuslav Novák, Iveta Waczulíková, and Ivan Varga. 2022. "Utilization of a 3D Printed Orthodontic Distalizer for Tooth-Borne Hybrid Treatment in Class II Unilateral Malocclusions" Materials 15, no. 5: 1740. https://doi.org/10.3390/ma15051740