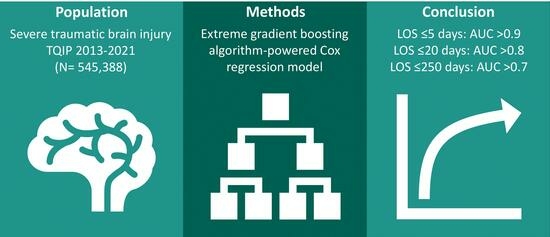
Development and Validation of an XGBoost-Algorithm-Powered Survival Model for Predicting In-Hospital Mortality Based on 545,388 Isolated Severe Traumatic Brain Injury Patients from the TQIP Database
Abstract
:1. Introduction
2. Materials and Methods
2.1. Source of the Data
2.2. Participants
2.3. Outcome
2.4. Predictors
2.5. Sample Size
2.6. Missing Data
2.7. Statistical Analysis
3. Results
3.1. Participants
3.2. Model Development
3.3. Predictive Model Specification
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Capizzi, A.; Woo, J.; Verduzco-Gutierrez, M. Traumatic Brain Injury: An Overview of Epidemiology, Pathophysiology, and Medical Management. Med. Clin. N. Am. 2020, 104, 213–238. [Google Scholar] [CrossRef]
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, Regional, and National Burden of Traumatic Brain Injury and Spinal Cord Injury, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 56–87. [Google Scholar] [CrossRef]
- Faul, M.; Coronado, V. Epidemiology of Traumatic Brain Injury. Handb. Clin. Neurol. 2015, 127, 3–13. [Google Scholar] [CrossRef]
- Majdan, M.; Plancikova, D.; Brazinova, A.; Rusnak, M.; Nieboer, D.; Feigin, V.; Maas, A. Epidemiology of Traumatic Brain Injuries in Europe: A Cross-Sectional Analysis. Lancet Public Health 2016, 1, e76–e83. [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the Global Incidence of Traumatic Brain Injury. J. Neurosurg. 2018, 130, 1080–1097. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Surveillance Report of Traumatic Brain Injury-Related Hospitalizations and Deaths by Age Group, Sex, and Mechanism of Injury; Centers for Disease Control and Prevention, U.S. Department of Health and Human Services: Washington, DC, USA, 2021. [Google Scholar]
- Stocchetti, N.; Zanier, E.R. Chronic Impact of Traumatic Brain Injury on Outcome and Quality of Life: A Narrative Review. Crit. Care 2016, 20, 148. [Google Scholar] [CrossRef]
- Matney, C.; Bowman, K.; Berwick, D.; National Academies of Sciences, Engineering, and Medicine. Understanding Patients with Traumatic Brain Injury. In Traumatic Brain Injury: A Roadmap for Accelerating Progress; National Academies Press: Washington, DC, USA, 2022. [Google Scholar]
- Matney, C.; Bowman, K.; Berwick, D.; National Academies of Sciences, Engineering, and Medicine. Rehabilitation and Long-Term Care Needs after Traumatic Brain Injury. In Traumatic Brain Injury: A Roadmap for Accelerating Progress; National Academies Press: Washington, DC, USA, 2022. [Google Scholar]
- Whiffin, C.J.; Gracey, F.; Ellis-Hill, C. The Experience of Families Following Traumatic Brain Injury in Adult Populations: A Meta-Synthesis of Narrative Structures. Int. J. Nurs. Stud. 2021, 123, 104043. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.I.R.; Menon, D.K.; Manley, G.T.; Abrams, M.; Åkerlund, C.; Andelic, N.; Aries, M.; Bashford, T.; Bell, M.J.; Bodien, Y.G.; et al. Traumatic Brain Injury: Progress and Challenges in Prevention, Clinical Care, and Research. Lancet Neurol. 2022, 21, 1004–1060. [Google Scholar] [CrossRef] [PubMed]
- Matney, C.; Bowman, K.; Berwick, D.; National Academies of Sciences, Engineering, and Medicine. Gaps, Challenges, and Opportunities. In Traumatic Brain Injury: A Roadmap for Accelerating Progress; National Academies Press: Washington, DC, USA, 2022. [Google Scholar]
- Timmons, S.D.; Bee, T.; Webb, S.; Diaz-Arrastia, R.R.; Hesdorffer, D. Using the Abbreviated Injury Severity and Glasgow Coma Scale Scores to Predict 2-Week Mortality after Traumatic Brain Injury. J. Trauma 2011, 71, 1172–1178. [Google Scholar] [CrossRef]
- Foreman, B.P.; Caesar, R.R.; Parks, J.; Madden, C.; Gentilello, L.M.; Shafi, S.; Carlile, M.C.; Harper, C.R.; Diaz-Arrastia, R.R. Usefulness of the Abbreviated Injury Score and the Injury Severity Score in Comparison to the Glasgow Coma Scale in Predicting Outcome after Traumatic Brain Injury. J. Trauma 2007, 62, 946–950. [Google Scholar] [CrossRef]
- Tenovuo, O.; Diaz-Arrastia, R.; Goldstein, L.E.; Sharp, D.J.; van der Naalt, J.; Zasler, N.D. Assessing the Severity of Traumatic Brain Injury—Time for a Change? J. Clin. Med. 2021, 10, 148. [Google Scholar] [CrossRef]
- Demetriades, D.; Kuncir, E.; Murray, J.; Velmahos, G.C.; Rhee, P.; Chan, L. Mortality Prediction of Head Abbreviated Injury Score and Glasgow Coma Scale: Analysis of 7764 Head Injuries. J. Am. Coll. Surg. 2004, 199, 216–222. [Google Scholar] [CrossRef]
- Wang, R.; Zeng, X.; Long, Y.; Zhang, J.; Bo, H.; He, M.; Xu, J. Prediction of Mortality in Geriatric Traumatic Brain Injury Patients Using Machine Learning Algorithms. Brain Sci. 2023, 13, 94. [Google Scholar] [CrossRef]
- Wu, X.; Sun, Y.; Xu, X.; Steyerberg, E.W.; Helmrich, I.R.A.R.; Lecky, F.; Guo, J.; Li, X.; Feng, J.; Mao, Q.; et al. Mortality Prediction in Severe Traumatic Brain Injury Using Traditional and Machine Learning Algorithms. J. Neurotrauma 2023, 40, 1366–1375. [Google Scholar] [CrossRef]
- Lang, L.; Wang, T.; Xie, L.; Yang, C.; Skudder-Hill, L.; Jiang, J.; Gao, G.; Feng, J. An Independently Validated Nomogram for Individualised Estimation of Short-Term Mortality Risk among Patients with Severe Traumatic Brain Injury: A Modelling Analysis of the CENTER-TBI China Registry Study. eClinicalMedicine 2023, 59, 101975. [Google Scholar] [CrossRef] [PubMed]
- Abujaber, A.; Fadlalla, A.; Gammoh, D.; Abdelrahman, H.; Mollazehi, M.; El-Menyar, A. Prediction of In-Hospital Mortality in Patients on Mechanical Ventilation Post Traumatic Brain Injury: Machine Learning Approach. BMC Med. Inform. Decis. Mak. 2020, 20, 336. [Google Scholar] [CrossRef]
- Amorim, R.L.; Oliveira, L.M.; Malbouisson, L.M.; Nagumo, M.M.; Simoes, M.; Miranda, L.; Bor-Seng-Shu, E.; Beer-Furlan, A.; De Andrade, A.F.; Rubiano, A.M.; et al. Prediction of Early TBI Mortality Using a Machine Learning Approach in a LMIC Population. Front. Neurol. 2020, 10, 1366. [Google Scholar] [CrossRef] [PubMed]
- Utomo, W.K.; Gabbe, B.J.; Simpson, P.M.; Cameron, P.A. Predictors of In-Hospital Mortality and 6-Month Functional Outcomes in Older Adults after Moderate to Severe Traumatic Brain Injury. Injury 2009, 40, 973–977. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A.; Pratap Singh, R.; Suman, R.; Rab, S. Significance of Machine Learning in Healthcare: Features, Pillars and Applications. Int. J. Intell. Netw. 2022, 3, 58–73. [Google Scholar] [CrossRef]
- Pettit, R.W.; Fullem, R.; Cheng, C.; Amos, C.I. Artificial Intelligence, Machine Learning, and Deep Learning for Clinical Outcome Prediction. Emerg. Top. Life Sci. 2021, 5, 729–745. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; Association for Computing Machinery: New York, NY, USA, 2016; pp. 785–794. [Google Scholar]
- Brownlee, J. XGBoost with Python: Gradient Boosted Trees with XGBoost and Scikit-Learn; Machine Learning Mastery: Vermont, VIC, Australia, 2016. [Google Scholar]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD): The TRIPOD Statement. BMC Med. 2015, 13, 1. [Google Scholar] [CrossRef]
- WMA—The World Medical Association-WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 13 May 2020).
- Allgöwer, M.; Burri, C. Schockindex. DMW—Dtsch. Med. Wochenschr. 1967, 92, 1947–1950. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; ISBN 978-0-470-58247-3. [Google Scholar]
- Kamarudin, A.N.; Cox, T.; Kolamunnage-Dona, R. Time-Dependent ROC Curve Analysis in Medical Research: Current Methods and Applications. BMC Med. Res. Methodol. 2017, 17, 53. [Google Scholar] [CrossRef]
- Nohara, Y.; Matsumoto, K.; Soejima, H.; Nakashima, N. Explanation of Machine Learning Models Using Shapley Additive Explanation and Application for Real Data in Hospital. Comput. Methods Programs Biomed. 2022, 214, 106584. [Google Scholar] [CrossRef] [PubMed]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Development Core Team: Vienna, Austria, 2008. [Google Scholar]
- Rossum, G.V.; Drake, F.L. Python 3 Reference Manual: (Python Documentation Manual Part 2); CreateSpace Independent Publishing Platform: Scotts Valley, CA, USA, 2009; ISBN 978-1-4414-1269-0. [Google Scholar]
- Matney, C.; Bowman, K.; Berwick, D.; National Academies of Sciences, Engineering, and Medicine. Traumatic Brain Injury Prevention and Awareness. In Traumatic Brain Injury: A Roadmap for Accelerating Progress; National Academies Press: Washington, DC, USA, 2022. [Google Scholar]
- Fatuki, T.A.; Zvonarev, V.; Rodas, A.W. Prevention of Traumatic Brain Injury in the United States: Significance, New Findings, and Practical Applications. Cureus 2020, 12, e11225. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control Brain Injury Safety Tips and Prevention. Available online: https://www.cdc.gov/headsup/basics/concussion_prevention.html (accessed on 5 June 2023).
- Krishnamoorthy, V.; Distelhorst, J.T.; Vavilala, M.S.; Thompson, H. Traumatic Brain Injury in the Elderly: Burden, Risk Factors, and Prevention. J. Trauma Nurs. JTN 2015, 22, 204. [Google Scholar] [CrossRef]
- Yee, G.; Jain, A. Geriatric Head Injury. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Bramlett, H.M.; Dietrich, W.D. Long-Term Consequences of Traumatic Brain Injury: Current Status of Potential Mechanisms of Injury and Neurological Outcomes. J. Neurotrauma 2015, 32, 1834–1848. [Google Scholar] [CrossRef]
- Ng, S.Y.; Lee, A.Y.W. Traumatic Brain Injuries: Pathophysiology and Potential Therapeutic Targets. Front. Cell. Neurosci. 2019, 13, 528. [Google Scholar] [CrossRef]
- Dash, H.H.; Chavali, S. Management of Traumatic Brain Injury Patients. Korean J. Anesthesiol. 2018, 71, 12–21. [Google Scholar] [CrossRef]
- Khalili, H.; Ahl, R.; Paydar, S.; Sjolin, G.; Cao, Y.; Abdolrahimzadeh Fard, H.; Niakan, A.; Hanna, K.; Joseph, B.; Mohseni, S. Beta-Blocker Therapy in Severe Traumatic Brain Injury: A Prospective Randomized Controlled Trial. World J. Surg. 2020, 44, 1844–1853. [Google Scholar] [CrossRef]






| Survived (N = 498,599) | Died (N = 46,789) | p-Value | |
|---|---|---|---|
| Length of hospital stay, median [IQR] | 4.0 [2.0–7.0] | 3.0 [2.0–8.0] | <0.001 |
| Missing, n (%) | 3919 (0.8) | 2302 (4.9) | |
| Age, median [IQR] | 67 [49–79] | 74 [60–82] | <0.001 |
| Sex, n (%) | <0.001 | ||
| Female | 190,692 (38.2) | 16,661 (35.6) | |
| Male | 307,239 (61.6) | 30,061 (64.2) | |
| Missing | 668 (0.1) | 67 (0.1) | |
| Race, n (%) | <0.001 | ||
| White | 383,863 (77.0) | 36,761 (78.6) | |
| Black | 47,635 (9.6) | 3514 (7.5) | |
| Asian | 14,670 (2.9) | 1750 (3.7) | |
| American Indian | 4693 (0.9) | 356 (0.8) | |
| Pacific islander | 1403 (0.3) | 151 (0.3) | |
| Other | 35,796 (7.2) | 2941 (6.3) | |
| Missing | 6480 (1.3) | 644 (1.4) | |
| History of myocardial infarction, n (%) | 8110 (1.6) | 1122 (2.4) | <0.001 |
| Congestive heart failure, n (%) | 28,071 (5.6) | 4749 (10.1) | <0.001 |
| Cerebrovascular disease, n (%) | 27,543 (5.5) | 3365 (7.2) | <0.001 |
| History of peripheral vascular disease, n (%) | 5540 (1.1) | 833 (1.8) | <0.001 |
| Diabetes mellitus, n (%) | 100,978 (20.3) | 11,426 (24.4) | <0.001 |
| Chronic renal failure, n (%) | 11,768 (2.4) | 2279 (4.9) | <0.001 |
| Dementia, n (%) | 44,075 (8.8) | 4215 (9.0) | 0.222 |
| Coagulopathy, n (%) | 32,520 (6.5) | 5801 (12.4) | <0.001 |
| Anticoagulant therapy, n (%) | 2870 (0.6) | 90 (0.2) | <0.001 |
| Missing | 100,926 (20.2) | 9556 (20.4) | |
| Currently receiving chemotherapy for cancer, n (%) | 3924 (0.8) | 800 (1.7) | <0.001 |
| Disseminated cancer, n (%) | 5765 (1.2) | 1320 (2.8) | <0.001 |
| Current smoker, n (%) | 79,330 (15.9) | 4177 (8.9) | <0.001 |
| COPD, n (%) | 37,049 (7.4) | 4496 (9.6) | <0.001 |
| Cirrhosis, n (%) | 7658 (1.5) | 1790 (3.8) | <0.001 |
| Alcohol use disorder, n (%) | 54,543 (10.9) | 4868 (10.4) | <0.001 |
| Drug use disorder, n (%) | 24,727 (5.0) | 1471 (3.1) | <0.001 |
| Major psychiatric illness, n (%) | 55,874 (11.2) | 3885 (8.3) | <0.001 |
| Advanced directive limiting care, n (%) | 22,674 (4.5) | 6037 (12.9) | <0.001 |
| Head AIS, n (%) | <0.001 | ||
| 3 | 283,581 (56.9) | 9253 (19.8) | |
| 4 | 136,610 (27.4) | 7405 (15.8) | |
| 5 | 78,408 (15.7) | 30,131 (64.4) | |
| Face AIS, n (%) | |||
| Injury present | 139,844 (28.0) | 10,921 (23.3) | <0.001 |
| Neck AIS, n (%) | |||
| Injury present | 3099 (0.6) | 351 (0.8) | <0.001 |
| Spine AIS, n (%) | |||
| Injury present | 5953 (1.2) | 158 (0.3) | <0.001 |
| Thorax AIS, n (%) | |||
| Injury present | 18,423 (3.7) | 2577 (5.5) | <0.001 |
| Abdomen AIS, n (%) | |||
| Injury present | 11,363 (2.3) | 1574 (3.4) | <0.001 |
| Upper extremity AIS, n (%) | |||
| Injury present | 65,262 (13.1) | 6416 (13.7) | <0.001 |
| Lower extremity AIS, n (%) | |||
| Injury present | 50,267 (10.1) | 5309 (11.3) | <0.001 |
| External/Other AIS, n (%) | |||
| Injury present | 20,205 (4.1) | 2387 (5.1) | <0.001 |
| GCS at admission, n (%) | <0.001 | ||
| Mild (GCS 14–15) | 392,770 (78.8) | 11,104 (23.7) | |
| Moderate (GCS 9–13) | 43,050 (8.6) | 5986 (12.8) | |
| Severe (GCS 3–8) | 36,331 (7.3) | 27,567 (58.9) | |
| Missing | 26,448 (5.3) | 2132 (4.6) | |
| Hypotension at admission, n (%) | 3498 (0.7) | 3169 (6.8) | <0.001 |
| Missing | 12,064 (2.4) | 1438 (3.1) | |
| Tachycardia, n (%) | 80,891 (16.2) | 11,252 (24.0) | <0.001 |
| Missing | 11,639 (2.3) | 1195 (2.6) | |
| Shock index, median [IQR] | 0.57 [0.48–0.69] | 0.57 [0.45–0.72] | <0.001 |
| Missing, n (%) | 13,967 (2.8) | 3133 (6.7) | |
| Oxygen saturation, median [IQR] | 98 [96–99] | 98 [96–100] | <0.001 |
| Missing, n (%) | 25,842 (5.2) | 3374 (7.2) | |
| Respiratory rate, mean (SD) | 18.0 (±4.1) | 17.3 (±6.9) | <0.001 |
| Missing, n (%) | 16,193 (3.2) | 3039 (6.5) | |
| Temperature, mean (SD) | 36.6 (±0.9) | 36.2 (±1.9) | <0.001 |
| Missing, n (%) | 46,866 (9.4) | 10,022 (21.4) | |
| Intracranial injury, n (%) | |||
| Cerebral contusion | 125,674 (25.2) | 17,584 (37.6) | <0.001 |
| Epidural hematoma | 22,534 (4.5) | 1855 (4.0) | <0.001 |
| Traumatic subdural hematoma | 353,638 (70.9) | 36,099 (77.2) | <0.001 |
| Traumatic subarachnoid hemorrhage | 155,472 (31.2) | 20,948 (44.8) | <0.001 |
| Diffuse axonal injury | 5044 (1.0) | 1545 (3.3) | <0.001 |
| Other intracranial injury | 14,434 (2.9) | 3408 (7.3) | <0.001 |
| Neurosurgical intervention, n (%) | <0.001 | ||
| None | 454,615 (91.2) | 37,421 (80.0) | |
| Within 24 h | 32,392 (6.5) | 8075 (17.3) | |
| After 24 h | 11,324 (2.3) | 1218 (2.6) | |
| Missing | 268 (0.1) | 75 (0.2) | |
| Volume PRBC transfused within 4 h, median [IQR] | 0.00 [0.00–0.00] | 0.00 [0.00–0.00] | <0.001 |
| Missing, n (%) | 0 (0.0) | 2 (0.0) | |
| Hospital teaching status, n (%) | <0.001 | ||
| Community | 196,758 (39.5) | 17,856 (38.2) | |
| Non-teaching | 87,816 (17.6) | 7201 (15.4) | |
| University | 212,138 (42.5) | 21,533 (46.0) | |
| Missing | 1887 (0.4) | 199 (0.4) | |
| Payment method, n (%) | <0.001 | ||
| Private/commercial insurance | 128,167 (25.7) | 8773 (18.8) | |
| Medicaid | 53,869 (10.8) | 3594 (7.7) | |
| Medicare | 237,888 (47.7) | 27,564 (58.9) | |
| Other government insurance | 11,854 (2.4) | 843 (1.8) | |
| Self-pay | 39,499 (7.9) | 3588 (7.7) | |
| Not billed (for any reason) | 1736 (0.3) | 125 (0.3) | |
| Other | 11,219 (2.3) | 873 (1.9) | |
| Missing | 14,367 (2.9) | 1429 (3.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, Y.; Forssten, M.P.; Sarani, B.; Montgomery, S.; Mohseni, S. Development and Validation of an XGBoost-Algorithm-Powered Survival Model for Predicting In-Hospital Mortality Based on 545,388 Isolated Severe Traumatic Brain Injury Patients from the TQIP Database. J. Pers. Med. 2023, 13, 1401. https://doi.org/10.3390/jpm13091401
Cao Y, Forssten MP, Sarani B, Montgomery S, Mohseni S. Development and Validation of an XGBoost-Algorithm-Powered Survival Model for Predicting In-Hospital Mortality Based on 545,388 Isolated Severe Traumatic Brain Injury Patients from the TQIP Database. Journal of Personalized Medicine. 2023; 13(9):1401. https://doi.org/10.3390/jpm13091401
Chicago/Turabian StyleCao, Yang, Maximilian Peter Forssten, Babak Sarani, Scott Montgomery, and Shahin Mohseni. 2023. "Development and Validation of an XGBoost-Algorithm-Powered Survival Model for Predicting In-Hospital Mortality Based on 545,388 Isolated Severe Traumatic Brain Injury Patients from the TQIP Database" Journal of Personalized Medicine 13, no. 9: 1401. https://doi.org/10.3390/jpm13091401