1. Introduction
Human epidermal growth factor receptor 2 (HER2) is a tyrosine kinase receptor involved in the pathogenesis of several cancers, including advanced gastric and gastroesophageal junction cancer [
1]. HER2 protein binds to an extracellular ligand binding domain that initiates a signal transduction cascade that affects tumor cell biology through several mechanisms, including cell proliferation, apoptosis, adhesion, migration, and differentiation [
2]. Trastuzumab (TZB) (Roche, Boston, MA, USA) is the first humanized monoclonal antibody (mAb) approved for immunotherapy and the first oncogene-targeted treatment with a proven survival benefit in HER2-positive cancer [
3]. Several studies have examined the efficacy of anti-HER2 therapies in both in vitro and in vivo models of gastric cancer using TZB and have shown that TZB leads to decreased HER2 signaling and inhibits cell growth [
4]. Although the clinical benefit of TZB was well described, it may be associated with cardio toxicity, which can lead to left ventricular dysfunction and congestive heart failure [
5]. Until now, there was no report regarding chemo-brain after TZB therapy.
Statins, which are well-known inhibitors of HMG-CoA reductase in cholesterol synthesis, are widely used to lower cholesterol for the treatment of hypercholesterolemia [
6,
7]. Recently, they have been reported to exhibit anti-tumor activities in various cancer cells mediated by anti-proliferative, proapoptotic, and anti-invasive properties [
8,
9,
10]. Atorvastatin (ATV) was reported to promote cell death and radio-sensitivity in prostate cancer cells [
11]. The effect of attenuating cognitive impairment after ATV therapy was also reported in a cellular level and mouse mode [
12,
13]. In addition, Taylor BA et al. reported that neural activity and cognition function improved after administration of ATV by f-MRI study in humans [
14].
Chemotherapy-associated cognitive impairment was referred to as chemo-brain. Although several candidate mechanisms explain chemo-brain, the accurate biological pathway remains obscure [
15,
16]. However, studies from humans and animal models have been published that focus on the relation between inflammatory markers, as a proxy for neuroinflammation, and cognitive performance. And many studies suggest that cognitive dysfunction may involve the actions of cytokines including IL-6, IL-1β, and TNF-α and microglia activation [
17,
18,
19]. Previously, oneauthor in this study reported donepezil, which is a reversible acetylcholinesterase inhibitor, improves cognitive impairment during doxorubicin or cyclophosphamide therapy [
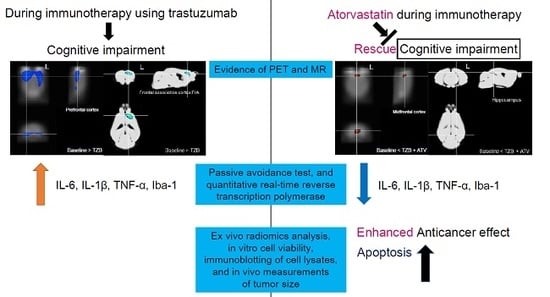
20]. In this study, we investigated cognitive impairment after administration of TZB, which has not yet been explored. We also showed that administration of ATV (Pfizer, New York, NY, USA) could compensate for cognitive impairment resulting from TZB therapy. Cognitive impairment was assessed by measuring cerebral glucose metabolism using statistical parametric mapping (SPM) analysis, regional gray matter concentration using voxel-based morphometry (VBM) analysis, the passive avoidance test, and quantitative real-time reverse transcription polymerase chain reaction. Alongside the enhanced anti-cancer effect of TZB, administration of ATV was confirmed by an ex vivo radiomics analysis, in vitro cell viability, immunoblotting of cell lysates, and in vivo measurements of tumor size. We also investigated that there was no hair loss side effect due to ATV therapy although ATV has anti-tumor activities for the NCI-N87 HER2 positive tumor mouse model.
2. Materials and Methods
2.1. Animals
In this study, five-week-old female BALB/C nude mice and C57BL/6 mice were obtained from Shizuoka Laboratory Center (Japan). Mice were maintained in temperature-controlled clean racks with a 12-h light/dark cycle. The mice were allowed to acclimatize for one week before the start of the experiment. All experiments were performed in accordance with the institutional guidelines of the Korea Institute of Radiological & Medical Sciences. BALB/nude mice were used for cognitive impairment and anti-tumor studies. C57BL/6 mice were used for alopecia studies.
2.2. Assessment of Chemobrain Using PET SPM and MR VBM
2.2.1. Cognitive Deficit Model
A cognitive deficit was evaluated after administration of 150 μg of TZB (
n = 7 per group, female). A total of 20 mg/kg of ATV was administered for 5 days to determine any effects on recovery of the cognitive deficit. Similarly, 70 mg/kg (equivalent to a dose of 215 mg/m
2 in humans, which is within the range of doses typically used for treatment of women with metastatic breast cancer (100–250 mg/m
2)) of cyclophosphamide (CTX) was administered. The experimental design, including the drug doses, dose schedule, and PET imaging schedule used, is described in
Figure 1A, and the MR imaging schedule is described in
Figure 2A.
2.2.2. PET Data Acquisition
Siemens Inveon PET was used in this study [
21]. Regional cerebral glucose metabolism was measured using
18F-fluorodeoxyglucose (FDG) PET. Before PET scanning, mice (
n = 10 per group, female) fasted for at least 8 h, after which they were anesthetized with 2% isoflurane in 100% oxygen (Forane solution, Choongwae Pharma, Seoul, Korea). During PET scanning, the body temperature was maintained at 36 °C with heating pads. Then, 200 μCi of
18F-FDG was injected through a tail vein. After 30 min of uptake, 30-min emission PET data were acquired with an energy window of 350–650 keV. Emission list-mode data were sorted into three-dimensional (3D) sinograms and reconstructed using 3D reprojection algorithms. No filter was applied. The image matrix measured 256 × 256 × 159, the pixel size was 0.155 × 0.155 mm
2, and the slice thickness was 0.796 mm.
2.2.3. Voxel-Based Statistical Analysis of PET Data
Voxel-wise statistical analysis was performed to identify regional differences between groups using SPM 8 (
http://www.fil.ion.ucl.ac.uk/spm). SPM analysis for small animals was described in our previous study [
22]. For SPM analysis, the brain was extracted and a study-specific mouse brain template was constructed. Individual PET data were spatially normalized onto the mouse brain template. Spatial normalization for individual PET was performed using affine and nonlinear transformations. The voxel size of spatially normalized images was 0.3 × 0.3 × 0.3 mm
3. Additionally, a 3-mm Gaussian smoothing kernel was applied to enhance the signal-to-noise ratio. Count normalization was performed. Paired
t-tests were used to identify regional differences in cerebral glucose metabolism between groups (
p < 0.005, uncorrected).
2.2.4. MR Data Acquisition
T2w 3D MR images were acquired using an Agilent 9.4 T MR scanner (USA). An AD quad 70 RF coil was used, and the matrix size was 192 × 192 × 192. The repetition time (RT) was 2500 ms. The effective echo time (TE) was 7.00 ms, and the image acquisition time was 3 h 36 min.
2.2.5. VBM Analysis of MR Data
Modulated Voxel-based morphometry (VBM) was performed to compare the regional gray matter concentration between groups in particular brain regions [
23]. Skull stripping was performed using BrainSuite (version 16) software [
24]. Parameters including brain surface extractor diffusion iterations, diffusion constant, edge constant, and erosion size were adjusted for skull stripping using individual T2w 3D MR data. Skull-stripped MR data were set to dimensions of 512 × 512 × 512 with a voxel size of 0.04 × 0.04 × 0.04 mm
3. A predefined gray matter template created by the Delora research team was used for spatial normalization [
25]. Individual skull-stripped MR data were spatially normalized onto the template and smoothed with a 2-mm Gaussian kernel. SPM 8 was used for VBM analysis. Paired
t-tests were used to identify regional differences in gray matter concentrations between groups (
p < 0.005, uncorrected).
2.3. Behavioral Analysis and Biomarker of Cognitive Deficit Model
2.3.1. Passive Avoidance Test
The passive avoidance test was used to assess the response to an aversive stimulus and long-term memory. The apparatus consisted of two divided rooms and a grilled floor for electric stimulation. A steel board separated the two rooms and could automatically be moved up and down. In the adaptation session, mice traveled freely between the two rooms for 5 min. The next day, the rooms were divided, and each mouse was placed in one room. The room was kept dark for 60 s to allow the mouse to adjust to darkness, and then the light was turned on as the steel panel was moved simultaneously. As the mouse traveled across to the other room to avoid the bright light, the mouse’s movement caused the steel panel to shut, and an electrical shock impulse (0.15 mA, 2 s) was transmitted to the grill. After 24 h, the mice were subjected to the same trial without electrical shock, and the latency time to cross over to the other room was automatically recorded (
Figure 3A).
2.3.2. Quantitative Real-Time Reverse Transcription PCR (qPCR)
Total RNA was extracted from the mouse frontal cortex using QIAzol Lysis Reagent (QIGEN, Hilden, Germany). cDNA was synthesized by amfiRivert cDNA synthesis platinum master mix (GenDEPOT, Katy, TX, USA). Real-time quantitative PCR analysis was performed using a qPCR Green 2X Master Mix kit (m.biotech, Gyeonggi-do, Korea) and a LightCycler® 96 Instrument (Roche Molecular Systems, Basel, Switzerland). The PCR protocol was as follows: initial denaturation for 10 min at 95 °C, 42 cycles of 95 °C for 15 s, 58 °C for 20 s, and 72 °C for 30 s. The comparative Ct method was used to determine the normalized changes in the target gene relative to a calibrator reference (Gapdh). The sequence-specific primers were as follows: mouse IL6 forward 5′-CCTTCCCTACTTCACAAGTC-3′, reverse 5′-TTTTCTGCAAGTGCATCATC-3′, and mouse Il-1β forward 5′-ACCTTTTGACAGTGATGAGAA-3′, reverse 5′-GCTGCTGCGAGATTTGA-3′, TNF-α forward 5′-TGGGTTGTACCTTGTCTACT-3′, reverse 5′-TGGTATGAGATAGCAAATCGG-3′, mouse Iba1 forward 5′-CCTTCCCTACTTCACAAGTC-3′, 5′-TTTTCTGCAAGTGCATCATC-3′, Gapdh forward 5′-CAAGAAGGTGGTGAAGCAGG-3′, and reverse 5′-AGGTGGAAGAGTGGGAGTTG-3′.
2.3.3. Assessment of Abnormal Hair Regrowth Using the Alopecia Model
To investigate whether ATV induced abnormal hair regrowth in mice, hair was shaved from the dorsal surface of the back in C57BL/6 mice (
n = 7 per group) by shaving and waxing using wax strips (Veet, Slough, UK), and the skin was washed using PBS. Mice were administered PBS, CTX, and ATV (all I.P.). After 23 days from depilation of hair, hair growth and hair color were observed. The doses and dose schedule was described in detail in
Figure 4A.
2.4. Enhanced Anti-Cancer Effect of Trastuzumab after Administration of Atorvastatin
2.4.1. Cell Culture and Tumor Xenograft in Mice
NCI-N87 HER2-positive cancer cell lines obtained from the American Type Culture Collection were maintained in RPMI containing 10% fetal bovine serum with antibiotics (Sigma, Darmstadt, Germany) at 37 °C in a humidified 5% CO2 incubator. Cells were seeded at a density of 20,000 cells per well in 96-well plate in four replicates. After 24 h, the medium was replaced with a new medium containing ATV and/or TZB. Following 48 h of incubation, alamarBlue reagent (Bio Rad, Hercules, CA, USA) was added directly to cells and incubated for 2 hours at 37 °C. NCI-N87 cells (5 × 106) were subcutaneously injected into female BALB/nude mice (n = 5 per group). Tumor size was measured using a digital caliper and tumor volume was determined using the formula width2 × length × 0.4.
2.4.2. Labelling and Purification of Alexa-488-TZB
A solution of Alexa-Fluor-488 NHS Ester (Invitrogen, Waltham, MA, USA) was prepared in dimethyl sulfoxide with 1% acetic acid. This solution was immediately dissolved in 500 μL (10 mg/mL) of 1 M sodium bicarbonate solution, which had a pH of 8.4. The solution was mixed thoroughly and allowed to stand for 1 h at room temperature. This reaction solution was purified with a size exclusion PD-10 column (GE Healthcare Bio-Sciences AB, Uppsala, Sweden) with PBS as the elution buffer. An aliquot (100 μg/100 μL PBS, pH 7.2) of the purified Alexa-488-TZB and unconjugated purified solution were measured using a NanoDrop spectrophotometer (ThermoFisher Scientific, Waltham, MA, USA). The number of Alexa-488 molecules conjugated per unit TZB was estimated by the Alexa-488 peak intensity distributed between the mAb-Alexa-488 conjugate and free Alexa-488 eluted from size-exclusion high-performance liquid chromatography. This reaction resulted in Alexa-488-TZB with 2.6 Alexa-Fluor-488 molecules per TZB. The concentration of Alexa-488-TZB was 1.5 mg/mL.
2.4.3. Immunofluorescence Staining of Tumor Tissues
When the tumor size reached 200 ± 20 mm
3, Alexa-488-TZB was I.V. injected as a single dose (150 μg) in the control group (
n = 7). In the ATV-treated group (
n = 7), 20 mg/kg of ATV in a 0.2 mL volume was I.P. injected for 5 days [
26]. To compare the therapeutic effect of ATV, CTX (70 mg/kg) was I.P. injected in another group of animals (
n = 7) [
27]. Five days later, the mice received a lateral tail vein injection of rhodamine-lectin (Rhodamine Ricinus communis Agglutinin I, 1 mg in 0.2 mL of PBS) to delineate blood vessels, and, 5 min after the lectin injection, the mice were euthanized by CO
2 inhalation and exsanguinated by cardiac puncture before dissection. The doses and dose schedule are described in detail in
Figure 5A.
Tumors were harvested and flash-frozen with the skin intact. Tumors were fixed with 4% paraformaldehyde overnight at 4 °C and were then cryopreserved with 30% sucrose in PBS until the tissue sank to the bottom of the tube at 4 °C. Tumors were embedded in an optimal cutting temperature compound for 1 h at −20 °C prior to sectioning and stored at −70 °C until use. Tumors were sectioned using a Leica CM 1850 cryostat (Leica Microsystems, Buffalo Grove, IL, USA) to a thickness of 8 µm to cover the entire tumor tissue. The 8-µm-thick cryostat sections were mounted on SuperFrost Plus slides. Before staining, slides were warmed at room temperature for 10 min. Slides were rehydrated with 200 µL of PBS for 10 min and then fixed in 4% paraformaldehyde for 10 min. Lastly, the DAPI stain was applied, and slides were cover-slipped.
2.4.4. Acquisition and Analysis of Fluorescent Images
Fluorescent images were acquired with a 10× objective using a fluorescence microscope (In cell analyzer 2200, GE Healthcare, Milwaukee, NY, USA) equipped with mosaic stitching software (In cell developer toolbox, GE Healthcare, Milwaukee, NY, USA). Three independent channels were obtained as follows: DAPI for nuclei (shown in blue, Ex/Em = 358/461 nm), rhodamine for blood vessels (shown in red, Ex/Em = 558/581 nm), and FITC for Alexa 488-TZB (shown in green, Ex/Em = 488/525 nm). Values were grouped together from 12 regions in each tumor. Four regions were measured 25% of the distance from the tumor apex, four regions were measured from the central region of the tumor, and four regions were measured 75% of the distance from the tumor apex. Each tumor was treated as an independent sample (n = 5).
2.4.5. Measurement of Alexa-488-TZB Accumulation in Tumor Tissues
Image analysis was performed using an in-house program written in MATLAB (MathWorks, Natick, MA, USA). Individual image channels were exported as TIFF images for analysis. For the measurement of Alexa-488-TZB penetration from the vessel and tumor surface, a region of interest (ROI) was drawn to calculate the intensity of Alexa-488-TZB. The penetration of Alexa-488-TZB up to a depth of ~80 µm depth from the vessel and tumor surface was calculated by area under the curve analysis. The total accumulation of Alexa-488-TZB was calculated by total Alexa-488-TZB intensity in the tumor divided by the total tumor area.
2.4.6. Microvascular Analysis in Tumor Tissues
Overall micro-distribution of functional vessels was assessed by measuring vascular density. To calculate vascular density, an individual blood vessel image was segmented using the fuzzy c-means clustering method. A value of 1 was regarded as the vessel area and 0 was regarded as the non-vessel area on a segmented binary image. The fraction of vessel area over the entire tumor area (vessel area/non-vessel area) was represented as vascular density. Microvascular analysis was performed using the in-house MATLAB code and the MIPAV program (National Institutes of Health, Bethesda, MD, USA).
2.4.7. Radiomics Analysis of the Cell Nuclei in Tumor Tissues
Radiomics analyses such as circularity and fractal dimension (FD) analyses for cell nuclei were performed to identify morphological changes after treatment in each group. Measurements of circularity or FD for cell nuclei demonstrate the therapeutic effect of a drug [
28]. Circularity and FD analyses for cell nuclei in tumor tissues were performed near the vessel (~80 µm from the vessel). The edge contour information of DAPI cell nuclei was extracted using a Laplacian edge-finding algorithm. Circularity and FD analysis were then performed. Image analysis was performed using the in-house MATLAB code and the MIPAV program (National Institutes of Health, Bethesda, MD, USA).
2.5. Measurement of Tumor Growth after Co-Administration of ATV
Cell Viability Assay, Cell Lysate Analysis, and Tumor Growth Delay
Cell viability was measured at an emission wavelength of 590 nm using a microplate reader. We examined whether ATV and/or TZB affects NCI-N87 cell proliferation following treatment by counting cells. Various concentrations (0, 1, 5, 10, 50, 100, 200, 300, 400, and 500 μM) of ATV and (0, 1, and 5 μg/mL) of TZB were used. Next, cytotoxicity resulting from the poly (ADP-ribose) polymerase 1 and Bcl-2, which are a unique characteristic of apoptotic cell death, was proven by immunoblotting cell lysates using Anti-Bcl-2 antibody (cat No. ab59348) (Abcam, Rockville, MD, USA) and Anti-PARP1 antibody (cat No. ab32138) (Abcam, Rockville, MD, USA).
When the tumor volume in NCI-N87-bearing mice was 200 ± 20 mm2, the mice were randomly divided into five groups (n = 3–5 per group). Each group was treated with TZB (150 μg) or TZB (150 μg) plus ATV (20 mg/kg for 5 days). The tumor size was measured using a digital caliper, and the tumor volume was calculated three times a week, according to the following formula: width2 × length × 0.4.
2.6. Statistics
Data are expressed as means ± standard deviation. The differences between groups were analyzed using a one-way analysis of variance. PRISM 5 (GraphPad software, San Diego, CA, USA) was used for statistical analysis.
2.7. Study Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. The animal study was approved by the Institutional Animal Care and Use Committee (IACUC) and Institutional review board in Korea Institute of Radiological and Medical Sciences (#KIRAMS 2018-0016).
4. Discussion
4.1. Atorvastatin Rescued Cognitive Impairment during Trastuzumab Therapy without Chemo-Brain and Hair-Loss Side Effect
The present study shows that TZB induces cognitive impairment, which is a side effect that occurs in addition to its anti-tumor effects, in a HER2-positive gastric cancer model. The study shows that co-administration of ATV with TZB can rescue the resulting cognitive impairment. In addition, co-administration of ATV with TZB can increase the anti-cancer effect of TZB with no side effect of hair loss.
4.2. Why Atorvastatin Therapy Could Rescue the Chemo-Brain Effect during Trastuzumab Therapy
We found that cerebral glucose metabolism and regional gray matter concentration in the region of the prefrontal cortex or frontal association cortex was decreased when TZB was administered. Because TZB cannot penetrate the brain-blood barrier, it cannot act on the brain directly. It has been previously reported that IL-6 is increased after administration of TZB [
29]. Therefore, cognitive impairment during TZB therapy may be explained by increased IL-6 levels [
30]. In our present study, the degree of cognitive impairment following TZB therapy and the compensatory effects of ATV were confirmed using a passive avoidance test and measuring the levels of IL-6, IL-1β, and TNF-α. According to the VBM results, only the frontal association cortex and left hippocampus were altered. The left hippocampus was highly correlated with an associative spatial long-term memory [
31]. Decreased grey matter concentration in the left hippocampus might represent a decrease in associative spatial long-term memory.
The issue of chemo-brain with breast cancer patients was described in our previous study in detail [
15]. According to the report, large number of drugs such as rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone, vincristine and rituximab, or vincristine and bendamustine were discussed [
15]. However, there was no report on chemo-brain after treatment of TZB. In our present study, we first showed the effect of chemo-brain after treatment of TZB. Additionally, we also showed ATV can rescue the symptom of chemo-brain after treatment of TZB. Recovery of cognitive deficit after use of ATV was also found in the previous study [
14] and well matched the result, which was performed from our groups. In our present study, we extensively analyzed the effect of rescue of chemo-brain after ATV treatment using an imaging marker such as FDG PET and Voxel based morphometry, and behavioral study. Cytokine analysis also supported the image analysis.
However, we used nude mice in this study and a nude mouse has a genetic mutant that has a deteriorated or removed thymus, which results in an inhibited immune system due to a greatly reduced number of T cells [
32]. In chemotherapy-induced dyscognition, cytokines are presented as an important pathway or as a marker for the prediction. Therefore, these nude mice may have limitations in studying chemo-brain.
4.3. Advantage As an Anticancer Drug of Atorvastatint during Trastuzumab Therapy
An advantage of ATV as a combinatorial drug with TZB is the enhanced therapeutic efficacy of TZB in tumors. ATV enhanced accumulation and penetration of TZB in solid tumor tissue in a gastric cancer xenograft model. Increased tumor accumulation and penetration of TZB in tumor improved the anti-tumor effect of TZB. Accumulation of TZB in the tumor increased by 100% after co-administration of ATV compared with that observed for TZB alone. Anti-tumor activity was measured by circularity and FD analyses to determine the fragmentation of nuclear DNA during co-administration of ATV and TZB. At distances of 0 to 80 μm from the vessel, the circularity significantly decreased by 43% during co-administration of TZB and ATV compared with that observed with the administration of TZB alone. Taken together, these results suggest that ATV may expand the interstitial space, which, thereby, promotes the delivery of Alexa-488-TZB and enhances the therapeutic efficacy of TZB.
Although the enhancement in the accumulation of TZB after administration of CTX was greater than that observed with co-administration of ATV, CTX induced hair loss and cognitive impairment (
Figure 1). Abnormal hair growth and alopecia are common side effects of systemic cancer treatment using CTX [
33]. However, we showed that ATV did not induce abnormal hair regrowth in mice.
A further advantage of co-administration of ATV could be a decrease in radio-resistance during radio-immunotherapy, which can be induced by IL6 during TZB therapy [
34,
35]. Co-administration of ATV during radio-immunotherapy using α-particles such as
211At and
225Ac offers another advantage [
36]. α-particles show much higher linear energy transfer (50–230 keV/μm) within a short range in tissues (28–50 μm) than do β-particles emitted by radionuclides such as
131I,
90Y, or
177Lu (LET = 0.1–1.0 keV/μm) whose range is 2 to 10 mm in the tissue [
37]. Deep penetration of TZB into a tumor is important to avoid off-target normal tissue toxicity. We found that the depth at which the highest amount of Alexa-488-TZB occurred was shifted from 15 μm to 27 μm when ATV was co-administered (
Figure 4E). Therefore, co-administration of ATV may offer an advantage during radioimmunotherapy using α-particles.
Collectively, our results demonstrate that the co-administration of ATV and TZB blocked the development of cognitive impairment. To the best of our knowledge, our study is the first to demonstrate this effect on cognitive impairment during TZB therapy. We also showed that ATV could rescue cognitive impairment during TZB therapy. In addition, we showed that ATV enhanced the therapeutic efficacy of TZB in tumors. This approach represents a promising therapeutic strategy for enhancing TZB treatment without the side effects of cognitive impairment or hair loss.