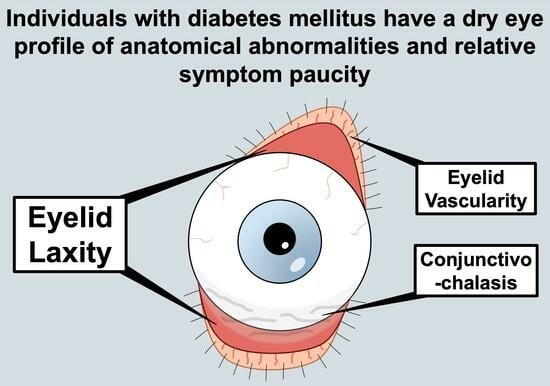
Individuals with Diabetes Mellitus Have a Dry Eye Phenotype Driven by Low Symptom Burden and Anatomic Abnormalities
Abstract
:1. Introduction
2. Materials and Methods
- (1)
- Tear film osmolarity (TearLAB, San Diego, CA, USA) [23];
- (2)
- Assessment of upper or lower eyelid laxity as determined based on rotation (0 = 0–25%; 1 = 25–50%; 2 = 50–100%) and the snapback test (0 = prompt snapback; 1 = slow return; 2 = does not return fully until blinking) [24], respectively;
- (3)
- Inferior meibomian gland plugging graded on a scale from 0 to 3 (0 = none; 1 = less than 1/3; 2 = between 1/3 and 2/3; 3 = greater than 2/3 lid involvement, graded without contact) [25];
- (4)
- Telangiectasias of the lower eyelids (0 = none; 1 = mild; 2 = moderate; 3 = severe) [25];
- (5)
- Assessment of conjunctivochalasis (0 = absent vs. 1 = present) in each area of the lower eyelid (nasally, medially, and temporally);
- (6)
- Non-invasive tear film stability based on TBUT (5 µL of fluorescein placed, 3 measurements taken in each eye and averaged) [26];
- (7)
- Fluorescein corneal staining graded according to the National Eye Institute (NEI) scale [26], with 5 areas of the cornea being assessed, including the inferior, nasal, superior, temporal, and central areas, and scored from 0 to 3 in each (max. total = 15);
- (8)
- Tear production graded based on mm wetting of anesthetized Schirmer’s test placed in the inferior fornix for 5 min (300 s) [26];
- (9)
- Meibum quality graded based on a scale from 0 to 4 (0 = clear; 1 = cloudy; 2 = granular; 3 = toothpaste; 4 = no meibum extracted) [25];
- (10)
- Inferior eyelid meibomian gland dropout graded according to the Meiboscale (0 = no dropout; 1 ≤ 25% dropout; 3 = 25% to 75% dropout; 3 ≥ 75% dropout) [27].
3. Results
3.1. Study Sample
3.2. DED Symptoms
3.3. DED Signs
3.4. Multivariable Analyses
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, Y.; Kim, M.; Galor, A. Beyond dry eye: How co-morbidities influence disease phenotype in dry eye disease. Clin. Exp. Optom. 2022, 105, 177–185. [Google Scholar] [CrossRef]
- Craig, J.P.; Nelson, J.D.; Azar, D.T.; Belmonte, C.; Bron, A.J.; Chauhan, S.K.; de Paiva, C.S.; Gomes, J.A.P.; Hammitt, K.M.; Jones, L.; et al. TFOS DEWS II Report Executive Summary. Ocul. Surf. 2017, 15, 802–812. [Google Scholar] [CrossRef]
- Kim, M.; Lee, Y.; Mehra, D.; Sabater, A.L.; Galor, A. Dry eye: Why artificial tears are not always the answer. BMJ Open Ophthalmol. 2021, 6, e000697. [Google Scholar] [CrossRef]
- Shtein, R.M.; Harper, D.E.; Pallazola, V.; Harte, S.E.; Hussain, M.; Sugar, A.; Williams, D.A.; Clauw, D.J. Discordant Dry Eye Disease (An American Ophthalmological Society Thesis). Trans. Am. Ophthalmol. Soc. 2016, 114, T4. [Google Scholar]
- Pouyeh, B.; Viteri, E.; Feuer, W.; Lee, D.J.; Florez, H.; Fabian, J.A.; Perez, V.L.; Galor, A. Impact of ocular surface symptoms on quality of life in a United States veterans affairs population. Am. J. Ophthalmol. 2012, 153, 1061–1066.e3. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, M. Systemic Health and Dry Eye. Inv. Ophthalmol. Vis. Sci. 2018, 59, DES138–DES142. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.S.; Schaumberg, D.; Uchino, M.; Vehof, J.; et al. TFOS DEWS II Epidemiology Report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, L.; Deng, S.; Sun, X.; Wang, N. Dry Eye Syndrome in Patients with Diabetes Mellitus: Prevalence, Etiology, and Clinical Characteristics. J. Ophthalmol. 2016, 2016, 8201053. [Google Scholar] [CrossRef]
- Chen, L.; Magliano, D.J.; Zimmet, P.Z. The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nat. Rev. Endocrinol. 2011, 8, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Najafi, L.; Malek, M.; Valojerdi, A.E.; Aghili, R.; Khamseh, M.E.; Fallah, A.E.; Tokhmehchi, M.R.; Behrouz, M.J. Dry eye and its correlation to diabetes microvascular complications in people with type 2 diabetes mellitus. J. Diabetes Complicat. 2013, 27, 459–462. [Google Scholar] [CrossRef]
- Ozdemir, M.; Buyukbese, M.A.; Cetinkaya, A.; Ozdemir, G. Risk factors for ocular surface disorders in patients with diabetes mellitus. Diabetes Res. Clin. Pract. 2003, 59, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Dogru, M.; Katakami, C.; Inoue, M. Tear function and ocular surface changes in noninsulin-dependent diabetes mellitus. Ophthalmology 2001, 108, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Yazdani-Ibn-Taz, M.K.; Han, M.M.; Jonuscheit, S.; Collier, A.; Nally, J.E.; Hagan, S. Patient-reported severity of dry eye and quality of life in diabetes. Clin. Ophthalmol. 2019, 13, 217–224. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, G.R.; Ferraz, G.A.M.; Gehlen, M.; Skare, T.L. Dry eyes in patients with diabetes mellitus. Prim. Care Diabetes 2021, 15, 184–186. [Google Scholar] [CrossRef]
- An, Q.; Zou, H. Ocular surface microbiota dysbiosis contributes to the high prevalence of dry eye disease in diabetic patients. Crit. Rev. Microbiol. 2022, 1–10. [Google Scholar] [CrossRef]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef]
- Lin, X.; Xu, B.; Zheng, Y.; Coursey, T.G.; Zhao, Y.; Li, J.; Fu, Y.; Chen, X.; Zhao, Y.E. Meibomian Gland Dysfunction in Type 2 Diabetic Patients. J. Ophthalmol. 2017, 2017, 3047867. [Google Scholar] [CrossRef]
- Zhmud, T.; Malachkova, N.; Redjak, R.; Costagliola, C.; Concilio, M.; Drozhzhyna, G.; Toro Mario, D.; Veretelnyk, S. Dry eye disease severity and impact on quality of life in type II diabetes mellitus. Front. Med. 2023, 10, 1103400. [Google Scholar] [CrossRef]
- Chalmers, R.L.; Begley, C.G.; Caffery, B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Contact Lens Anterior Eye 2010, 33, 55–60. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Farhangi, M.; Feuer, W.; Galor, A.; Bouhassira, D.; Levitt, R.C.; Sarantopoulos, C.D.; Felix, E.R. Modification of the Neuropathic Pain Symptom Inventory for use in eye pain (NPSI-Eye). Pain 2019, 160, 1541–1550. [Google Scholar] [CrossRef]
- Spierer, O.; Felix, E.R.; McClellan, A.L.; Parel, J.M.; Gonzalez, A.; Feuer, W.J.; Sarantopoulos, C.D.; Levitt, R.C.; Ehrmann, K.; Galor, A. Corneal Mechanical Thresholds Negatively Associate With Dry Eye and Ocular Pain Symptoms. Inv. Ophthalmol. Vis. Sci. 2016, 57, 617–625. [Google Scholar] [CrossRef]
- Gokhale, M.; Stahl, U.; Jalbert, I. In situ osmometry: Validation and effect of sample collection technique. Optom. Vis. Sci. 2013, 90, 359–365. [Google Scholar] [CrossRef]
- Ansari, Z.; Singh, R.; Alabiad, C.; Galor, A. Prevalence, risk factors, and morbidity of eye lid laxity in a veteran population. Cornea 2015, 34, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Foulks, G.N.; Bron, A.J. Meibomian gland dysfunction: A clinical scheme for description, diagnosis, classification, and grading. Ocul. Surf. 2003, 1, 107–126. [Google Scholar] [CrossRef]
- Methodologies to diagnose and monitor dry eye disease: Report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop (2007). Ocul. Surf. 2007, 5, 108–152. [CrossRef]
- Pult, H.; Riede-Pult, B. An Assement of Subjective and Objective Grading of Meibography Images. Investig. Ophthalmol. Vis. Sci. 2012, 53, 588. [Google Scholar]
- Viso, E.; Rodriguez-Ares, M.T.; Abelenda, D.; Oubina, B.; Gude, F. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Inv. Ophthalmol. Vis. Sci. 2012, 53, 2601–2606. [Google Scholar] [CrossRef] [PubMed]
- Vehof, J.; Wang, B.; Kozareva, D.; Hysi, P.G.; Snieder, H.; Hammond, C.J. The heritability of dry eye disease in a female twin cohort. Inv. Ophthalmol. Vis. Sci. 2014, 55, 7278–7283. [Google Scholar] [CrossRef]
- Liu, H.; Sheng, M.; Liu, Y.; Wang, P.; Chen, Y.; Chen, L.; Wang, W.; Li, B. Expression of SIRT1 and oxidative stress in diabetic dry eye. Int. J. Clin. Exp. Pathol. 2015, 8, 7644–7653. [Google Scholar] [PubMed]
- Zhou, Q.; Yang, L.; Wang, Q.; Li, Y.; Wei, C.; Xie, L. Mechanistic investigations of diabetic ocular surface diseases. Front. Endocrinol. 2022, 13, 1079541. [Google Scholar] [CrossRef]
- Modulo, C.M.; Jorge, A.G.; Dias, A.C.; Braz, A.M.; Bertazolli-Filho, R.; Jordao, A.A., Jr.; Sergio Marchini, J.; Rocha, E.M. Influence of insulin treatment on the lacrimal gland and ocular surface of diabetic rats. Endocrine 2009, 36, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Yu, C.; Dong, H.; Mu, Y.; Zhang, R.; Zhang, Q.; Liang, W.; Li, W.; Wang, X.; Zhang, L. Recent Developments About the Pathogenesis of Dry Eye Disease: Based on Immune Inflammatory Mechanisms. Front. Pharmacol. 2021, 12, 732887. [Google Scholar] [CrossRef] [PubMed]
- Goldin, A.; Beckman, J.A.; Schmidt, A.M.; Creager, M.A. Advanced glycation end products: Sparking the development of diabetic vascular injury. Circulation 2006, 114, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Whiddett, R.O.; Buckle, I.; Chen, C.; Forbes, J.M.; Fotheringham, A.K. Advanced Glycation End Products and Inflammation in Type 1 Diabetes Development. Cells 2022, 11, 3503. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Liu, J.; Shi, B.; He, S.; Yao, X.; Willcox, M.D. Advanced glycation end product (AGE) modified proteins in tears of diabetic patients. Mol. Vis. 2010, 16, 1576–1584. [Google Scholar] [PubMed]
- Qu, M.; Qi, X.; Wang, Q.; Wan, L.; Li, J.; Li, W.; Li, Y.; Zhou, Q. Therapeutic Effects of STAT3 Inhibition on Experimental Murine Dry Eye. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3776–3785. [Google Scholar] [CrossRef]
- Byun, Y.S.; Kang, B.; Yoo, Y.S.; Joo, C.K. Poly(ADP-Ribose) Polymerase Inhibition Improves Corneal Epithelial Innervation and Wound Healing in Diabetic Rats. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1948–1955. [Google Scholar] [CrossRef]
- Batawi, H.; Shalabi, N.; Joag, M.; Koru-Sengul, T.; Rodriguez, J.; Green, P.T.; Campigotto, M.; Karp, C.L.; Galor, A. Sub-basal Corneal Nerve Plexus Analysis Using a New Software Technology. Eye Contact Lens 2018, 44 (Suppl. S1), S199–S205. [Google Scholar] [CrossRef]
- Yoon, K.C.; Im, S.K.; Seo, M.S. Changes of tear film and ocular surface in diabetes mellitus. Korean J. Ophthalmol. 2004, 18, 168–174. [Google Scholar] [CrossRef]
- Chhadva, P.; McClellan, A.L.; Alabiad, C.R.; Feuer, W.J.; Batawi, H.; Galor, A. Impact of Eyelid Laxity on Symptoms and Signs of Dry Eye Disease. Cornea 2016, 35, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Leibovitch, I.; Selva, D. Floppy eyelid syndrome: Clinical features and the association with obstructive sleep apnea. Sleep. Med. 2006, 7, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Chen, S.; Fu, S.; Li, Y.; Li, Z.; Li, S.; Liang, X.; Wang, Z.; Wang, Z.; Chen, Y.; et al. A Survey on How Ocular Surface Demodex Infestation Interactively Associates with Diabetes Mellitus and Dry Eye Disease. Acta Parasitol. 2021, 66, 1039–1047. [Google Scholar] [CrossRef] [PubMed]
- Rynerson, J.M.; Perry, H.D. DEBS-a unification theory for dry eye and blepharitis. Clin. Ophthalmol. 2016, 10, 2455–2467. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, H.; Qin, G.; Wu, Y.; Song, Y.; Yang, L.; Yu, S.; He, X.; Moore, J.E.; Moutari, S.; et al. Impact of Diquafosol Ophthalmic Solution on Tear Film and Dry Eye Symptom in Type 2 Diabetic Dry Eye: A Pilot Study. J. Ocul. Pharmacol. Ther. 2022, 38, 133–140. [Google Scholar] [CrossRef]
- Zagon, I.S.; Klocek, M.S.; Sassani, J.W.; McLaughlin, P.J. Dry eye reversal and corneal sensation restoration with topical naltrexone in diabetes mellitus. Arch. Ophthalmol. 2009, 127, 1468–1473. [Google Scholar] [CrossRef]
- Su, Y.C.; Hung, J.H.; Chang, K.C.; Sun, C.C.; Huang, Y.H.; Lee, C.N.; Hung, M.J.; Lai, C.C.; Shao, S.C.; Lai, E.C. Comparison of Sodium-Glucose Cotransporter 2 Inhibitors vs. Glucagonlike Peptide-1 Receptor Agonists and Incidence of Dry Eye Disease in Patients With Type 2 Diabetes in Taiwan. JAMA Netw. Open 2022, 5, e2232584. [Google Scholar] [CrossRef]
| Controls (n = 272) | DM − C (n = 53) | DM + C (n = 41) | p-Value | |
|---|---|---|---|---|
| Demographics, % (n) | ||||
| Age, years, mean ± SD | 59.0 ± 6.5 | 58.2 ± 6.4 | 61.7 ± 5.2 b | 0.02 |
| Sex, male | 88% (238) | 91% (48) | 100% (41)a | 0.05 |
| Race, White | 40% (109) | 30% (16) | 41% (17) | 0.20 |
| Ethnicity, Hispanic | 23% (62) | 26% (14) | 34% (14) | 0.27 |
| Clinical data, mean ± SD (n) | ||||
| HbA1C, % | 6.1 ± 1.7 (19) | 7.0 ± 1.3 (52) a | 8.0 ± 1.9 (40) b | <0.001 |
| Weight, pounds | 194.3 ± 41.9 (270) | 221.5 ± 45.7 (52) a | 226.9 ± 34.2 (41) a | <0.001 |
| BMI (kg/m2) | 28.6 ± 5.8 (270) | 32.7 ± 5.9 (52) a | 32.8 ± 3.6 (41) a | <0.001 |
| Comorbidities, % (n) | ||||
| Smoking (current) | 44% (119) | 40% (21) | 37% (15) | 0.62 |
| Hypertension | 61% (166) | 92% (49) a | 85% (35) a | <0.001 |
| Hypercholesterolemia | 47% (128) | 83% (44) a | 85% (35) a | <0.001 |
| PTSD | 22% (60) | 25% (13) | 29% (12) | 0.58 |
| Depression | 70% (190) | 62% (33) | 61% (25) | 0.34 |
| Arthritis | 51% (139) | 49% (26) | 56% (23) | 0.78 |
| Sleep apnea | 23% (62) | 36% (19) | 24% (10) | 0.13 |
| BPH | 11% (31) | 21% (11) | 24% (10) a | 0.03 |
| Rosacea | 3% (7) | 0% (0) | 0% (0) | 0.29 |
| Hepatitis C | 15% (40) | 11% (6) | 7% (3) | 0.39 |
| Devices and medications, % (n) | ||||
| CPAP | 5% (13) | 6% (3) | 10% (4) | 0.43 |
| NSAIDs | 40% (108) | 47% (25) | 20% (8) b | 0.02 |
| ASA | 33% (91) | 66% (35) a | 59% (24) a | <0.001 |
| Fish oil | 7% (19) | 15% (8) | 7% (3) | 0.14 |
| Multivitamins | 48% (130) | 53% (28) | 63% (26) | 0.16 |
| Beta blockers | 17% (46) | 25% (13) | 32% (13) | 0.05 |
| Statins | 35% (96) | 79% (42) a | 83% (34) a | <0.001 |
| Antidepressants | 60% (162) | 47% (25) | 46% (19) | 0.09 |
| Anxiolytics | 57% (154) | 49% (26) | 49% (20) | 0.44 |
| Analgesics | 69% (187) | 74% (39) | 61% (25) | 0.42 |
| Antihistamines | 23% (63) | 25% (13) | 20% (8) | 0.84 |
| Alpha-2-delta ligands | 31% (85) | 36% (19) | 34% (14) | 0.78 |
| Venlafaxine | 1% (3) | 0% (0) | 0% (0) | 0.59 |
| Sildenafil | 33% (90) | 38% (20) | 34% (14) | 0.81 |
| DE Metric [Range] (n) | Controls (n = 272) | DM − C (n = 53) | DM + C (n = 41) | p-Value |
|---|---|---|---|---|
| DED and ocular pain symptoms quantified based on questionnaires [range] (n), mean ± SD | ||||
| DEQ-5 [0–22] (366) | 12.21 ± 4.55 | 11.83 ± 5.09 | 11.56 ± 4.75 | 0.65 |
| OSDI [0–100] (366) | 42.08 ± 24.46 | 38.88 ± 25.13 | 23.63 ± 16.20 b | <0.001 |
| NRS [0–10] (366) | 4.89 ± 3.17 | 4.34 ± 2.72 | 3.54 ± 2.68 a | 0.02 |
| NPSI-Eye [0–40] (366) | 13.22 ± 10.73 | 11.06 ± 10.51 | 7.59 ± 7.97 a | 0.004 |
| Corneal sensation assessed using Belmonte aesthesiometer (right eye) [range] (n), mean ± SD | ||||
| Detection threshold, ml/min [12.5–240] (360) | 79.60 ± 38.44 | 85.29 ± 38.42 | 87.32 ± 33.17 | 0.34 |
| Pain threshold, ml/min [25–410] (346) | 233.75 ± 118.30 | 225.30 ± 116.20 | 248.51 ± 120.06 | 0.66 |
| Tear film osmolarity (value from more severely affected eye) [range] (n), mean ± SD | ||||
| Osmolarity, mOsmol/L [277–380] (342) | 305.43 ± 15.58 | 308.53 ± 19.00 | 304.38 ± 12.77 | 0.38 |
| Osmolarity difference between eyes, mOsmol/L [0–86] (330) | 9.97 ± 12.12 | 11.98 ± 15.68 | 8.94 ± 6.14 | 0.48 |
| Ocular surface evaluation (value from more severely affected eye) [range] (n), mean ± SD | ||||
| Floppy eyelids, upper and lower [0–2] (355) | 0.69 ± 0.64 | 0.73 ± 0.72 | 1.08 ± 0.77 b | 0.004 |
| MG plugging [0–3] (365) | 1.71 ± 0.91 | 1.75 ± 0.83 | 1.78 ± 0.91 | 0.87 |
| Eyelid vascularity [0–3] (365) | 0.52 ± 0.71 | 0.26 ± 0.56 a | 0.59 ± 0.67 c | 0.03 |
| Conjunctivochalasis sum [0–3] (351) | 1.51 ± 0.98 | 1.20 ± 1.03 a | 1.81 ± 1.00 c | 0.02 |
| TBUT, seconds [0–15] (362) | 9.63 ± 4.91 | 8.98 ± 4.95 | 9.84 ± 4.85 | 0.63 |
| CFS [0–15] (364) | 1.85 ± 2.42 | 2.15 ± 2.23 | 2.29 ± 2.09 | 0.43 |
| Schirmer’s test, mm wetting [0–35] (362) | 12.97 ± 7.53 | 13.72 ± 7.60 | 11.73 ± 5.76 | 0.43 |
| Meibum quality [0–4] (358) | 1.85 ± 1.21 | 1.79 ± 1.31 | 2.05 ± 1.28 | 0.57 |
| MG dropout [0–4] (365) | 1.41 ± 0.95 | 1.43 ± 1.02 | 1.76 ± 1.04 | 0.10 |
| Unstandardized Coefficients | Standardized Coefficients | Coefficient of Determination | |||||
|---|---|---|---|---|---|---|---|
| Dependent Variable | Model | Predictor | B | SE | β | p-Value | R2 |
| OSDI | 1 | DM 0–2 | −7.95 | 1.84 | −0.22 | <0.001 | 0.05 |
| 2 | DM 0–2 | −6.19 | 1.97 | −0.17 | 0.002 | 0.06 | |
| Statins | −6.33 | 2.67 | −0.13 | 0.018 | |||
| 3 | DM 0–2 | −5.89 | 1.97 | −0.16 | 0.003 | 0.07 | |
| Statins | −6.14 | 1.97 | −0.13 | 0.022 | |||
| Age | −0.391 | 2.66 | −0.10 | 0.043 | |||
| Floppy eyelids, upper and lower | 1 | Age | 0.03 | 0.01 | 0.24 | <0.001 | 0.06 |
| 2 | Age | 0.03 | 0.01 | 0.24 | <0.001 | 0.08 | |
| DM 0–2 | 0.14 | 0.05 | 0.14 | 0.01 | |||
| 3 | Age | 0.03 | 0.01 | 0.24 | <0.001 | 0.09 | |
| DM 0–2 | 0.12 | 0.05 | 0.11 | 0.031 | |||
| BMI | 0.01 | <0.01 | 0.11 | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Locatelli, E.V.T.; Huang, J.J.; Mangwani-Mordani, S.; Tovar Vetencourt, A.A.; Galor, A. Individuals with Diabetes Mellitus Have a Dry Eye Phenotype Driven by Low Symptom Burden and Anatomic Abnormalities. J. Clin. Med. 2023, 12, 6535. https://doi.org/10.3390/jcm12206535
Locatelli EVT, Huang JJ, Mangwani-Mordani S, Tovar Vetencourt AA, Galor A. Individuals with Diabetes Mellitus Have a Dry Eye Phenotype Driven by Low Symptom Burden and Anatomic Abnormalities. Journal of Clinical Medicine. 2023; 12(20):6535. https://doi.org/10.3390/jcm12206535
Chicago/Turabian StyleLocatelli, Elyana V. T., Jaxon J. Huang, Simran Mangwani-Mordani, Arianna A. Tovar Vetencourt, and Anat Galor. 2023. "Individuals with Diabetes Mellitus Have a Dry Eye Phenotype Driven by Low Symptom Burden and Anatomic Abnormalities" Journal of Clinical Medicine 12, no. 20: 6535. https://doi.org/10.3390/jcm12206535