Angiographic Characteristics of the Vein of Marshall in Patients with and without Atrial Fibrillation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Electrophysiology Study and Catheter Ablation
2.3. VOM Angiography and Ethanol Infusion
2.4. Measurements and Definitions
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Characteristics of the VOM and Difference between Patients with and without AF
4.2. The Morphology Characteristics of the VOM
4.3. Correlation between the VOM and LAV
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Calkins, H.; Hindricks, G.; Cappato, R.; Kim, Y.H.; Saad, E.B.; Aguinaga, L.; Akar, J.G.; Badhwar, V.; Brugada, J.; Camm, J.; et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm 2017, 14, e275–e444. [Google Scholar] [CrossRef]
- Poole, J.E.; Bahnson, T.D.; Monahan, K.H.; Johnson, G.; Rostami, H.; Silverstein, A.P.; Al-Khalidi, H.R.; Rosenberg, Y.; Mark, D.B.; Lee, K.L.; et al. Recurrence of Atrial Fibrillation After Catheter Ablation or Antiarrhythmic Drug Therapy in the CABANA trial. J. Am. Coll. Cardiol. 2020, 75, 3105–3118. [Google Scholar] [CrossRef] [PubMed]
- Morillo, C.A.; Verma, A.; Connolly, S.J.; Kuck, K.H.; Nair, G.M.; Champagne, J.; Sterns, L.D.; Beresh, H.; Healey, J.S.; Natale, A.; et al. Radiofrequency ablation vs antiarrhythmic drugs as fisrt-line treatment of paroxysmal atrial fibrillation (RAAFT-2): 2 randomized trial. JAMA 2014, 311, 692–699. [Google Scholar] [CrossRef]
- Lee, S.H.; Tai, C.T.; Hsieh, M.H.; Tsao, H.M.; Lin, Y.J.; Chang, S.L.; Huang, J.L.; Lee, K.T.; Chen, Y.J.; Cheng, J.J.; et al. Predictors of non-pulmonary vein ectopic beats initiating paroxysmal atrial fibrillation: Implication for catheter ablation. J. Am. Coll. Cardiol. 2005, 46, 1054–1059. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.I.; Pak, H.N.; Park, J.H.; Choi, E.J.; Kim, S.K.; Kwak, J.J.; Jang, J.K.; Hwang, C.; Kim, Y. Clincal significance of complete conduction block of the left lateral isthmus and its relationship with anatomical variation of the vein of Marshall in patients with nonparoxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol. 2009, 20, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Ulphani, J.S.; Arora, R.; Cain, J.H.; Villuendas, R.; Shen, S.; Gordon, D.; Inderyas, F.; Harvey, L.A.; Morris, A.; Goldberger, J.J.; et al. The ligament of Marshall as a parasympathetic conduit. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H1629–H1635. [Google Scholar] [CrossRef] [PubMed]
- Valderrábano, M.; Peterson, L.E.; Swarup, V.; Schurmann, P.A.; Makkar, A.; Doshi, R.N.; DeLurgio, D.; Athill, C.A.; Ellenbogen, K.A.; Natale, A.; et al. Effect of Catheter Ablation With Vein of Marshall Ethanol Infusion vs Catheter Ablation Alone on Persistent Atrial Fibrillation: The VENUS Randomized Clinical Trial. JAMA 2020, 324, 1620–1628. [Google Scholar] [CrossRef]
- Kamakura, T.; Derval, N.; Duchateau, J.; Denis, A.; Nakashima, T.; Takagi, T.; Ramirez, F.D.; André, C.; Krisai, P.; Nakatani, Y.; et al. Vein of Marshall Ethanol Infusion: Feasibility, Pitfalls, and Complications in Over 700 Patients. Circ. Arrhythm. Electrophysiol. 2021, 14, e010001. [Google Scholar] [CrossRef]
- Derval, N.; Duchateau, J.; Denis, A.; Ramirez, F.D.; Mahida, S.; André, C.; Krisai, P.; Nakatani, Y.; Kitamura, T.; Takigawa, M.; et al. Marhshall bundle elimination, Pulmonary vein isolation, and Line completion for ANtomical ablation of persistent atrial fibrillation (Marhall-PLAN): Prospective, single-center study. Heart Rhythm 2021, 18, 529–537. [Google Scholar] [CrossRef]
- Gillis, K.; O’Neill, L.; Wielandts, J.Y.; Hilfiker, G.; Almorad, A.; Lycke, M.; El Haddad, M.; de Waroux, J.B.; Tavernier, R.; Duytschaever, M.; et al. Vein of Marshall Ethanol Infusion as First Step for Mitral Ishthmus Linear Ablation. JACC Clin. Electrophysiol. 2022, 8, 367–376. [Google Scholar] [CrossRef]
- Baez-Escudero, J.L.; Morales, P.F.; Dave, A.S.; Sasaridis, C.M.; Kim, Y.H.; Okishige, K.; Valderrabano, M. Ethanol infusion in the vein of Marshall facilitates mitral isthmus ablation. Heart Rhythm 2012, 9, 1207–1215. [Google Scholar] [CrossRef] [PubMed]
- Dave, A.S.; Baez-Escudero, J.L.; Sasaridis, C.; Hong, T.E.; Rami, T.; Valderrabano, M. Role of the vein of Marshall in atrial fibrillation recurrences after catheter ablation: Therapeutic effect of ethanol infusion. J. Cardiovasc. Electrophysiol. 2012, 23, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Knight, B.P.; Ebinger, M.; Oral, H.; Kim, M.H.; Sticherling, C.; Pelosi, F.; Michaud, G.F.; Strickberger, S.A.; Morady, F. Diagnostic value of tachycardia features and pacing maneuvers during paroxysmal supraventricular tachycardia. J. Am. Coll. Cardiol. 2000, 36, 574–582. [Google Scholar] [CrossRef]
- Saremi, F.; Muresian, H.; SánchezQuintana, D. Coronary veins: Comprehensive CT-anatomic classification and review of variantsand clinical implications. Radiographics 2012, 32, E1–E32. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, T.; Vlachos, K.; Denis, A.; Andre, C.; Martin, R.; Pambrun, T.; Duchateau, J.; Frontera, A.; Takigawa, M.; Thompson, N.; et al. Ethanol infusion for Marshall bundle epicardial connections in Marshall bundle-related atrial tachycardias following atrial fibrillation ablation: The accessibility and success rate of ethanol infusion by using a femoral approach. J. Cardiovasc. Electrophysiol. 2019, 30, 1443–1451. [Google Scholar] [CrossRef]
- Lfjllinghausen, M.V.; Ohmachi, N.; Besch, S.; Mettenleiter, A. Atrial Veins of the Human Heart. Clin. Anat. 1995, 8, 169–189. [Google Scholar]
- Ludinghausen, M. The venous drainage of the human myocardium. Anat. Embryol. Cell Biol. 2003, 168, 1–104. [Google Scholar]
- Takagi, T.; Derval, N.; Pambrun, T.; Nakatani, Y.; André, C.; Ramirez, F.D.; Nakashima, T.; Krisai, P.; Kamakura, T.; Pineau, X.; et al. Optimized Computed Tomography Acquisition Protocol for Ethanol Infusion Into the Vein of Marshall. JACC Clin. Electrophysiol. 2022, 8, 168–178. [Google Scholar] [CrossRef]
- Kurotobi, T.; Ito, H.; Inoue, K.; Iwakura, K.; Kawano, S.; Okamura, A.; Date, M.; Fujii, K. Marshall vein as arrhythmogenic source in patients with atrial fibrillation: Correlation between its anatomy and electrophysiological findings. J. Cardiovasc. Electrophysiol. 2006, 17, 1062–1067. [Google Scholar] [CrossRef]
- Habib, A.; Lachman, N.; Christensen, K.N.; Asirvatham, S.J. The anatomy of the coronary sinus venous system for the cardiac electrophysiologist. Europace 2009, 11 (Suppl. 5), v15–v21. [Google Scholar] [CrossRef]
- Hummel, J.D.; Strickberger, S.A.; Man, K.C.; Daoud, E.; Nibeauer, M.; Morady, F. A quantitative fluoroscopic comparison of the coronary sinus ostium in patients with and without AV nodal reentrant tachycardia. J. Cardiovasc. Electrophysiol. 1995, 6, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Ortale, J.R.; Gabriel, E.A.; Iost, C.; Márquez, C.Q. The anatomy of the coronary sinus and its tributaries. Surg. Radiol. Anat. 2001, 23, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, M.; Morales, P.F.; Rodriguez-Manero, M.; Lloves, C.; Schurmann, P.A.; Dave, A.S. The Human Left Atrial Venous Circulation as a Vascular Route for Atrial Pharmacological Therapies: Effects of Ethanol Infusion. JACC Clin. Electrophysiol. 2017, 3, 1020–1032. [Google Scholar] [CrossRef] [PubMed]
- Abhayaratna, W.P.; Fatema, K.; Barnes, M.E.; Seward, J.B.; Gersh, B.J.; Bailey, K.R.; Casaclang-Verzosa, G.; Tsang, T.S. Left atrial reservoir function as a potent marker for first atrial fibrillation or flutter in persons > or = 65 years of age. Am. J. Cardiol. 2008, 101, 1626–1629. [Google Scholar] [CrossRef]
- Tan, B.Y.; Ho, J.S.; Sia, C.H.; Boi, Y.; Foo, A.S.; Dalakoti, M.; Chan, M.Y.; Ho, A.F.; Leow, A.S.; Chan, B.P.; et al. Left Atrial Volume Index Predicts New-Onset Atrial Fibrillation and Stroke Recurrence in Patients with Embolic Stroke of Undetermined Source. Cerebrovasc. Dis. 2020, 49, 285–291. [Google Scholar] [CrossRef]
- Njoku, A.; Kannabhiran, M.; Arora, R.; Reddy, P.; Gopinathannair, R.; Lakkireddy, D.; Dominic, P. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: A meta-analysis. Europace 2018, 20, 33–42. [Google Scholar] [CrossRef]
- Flaker, G.C.; Fletcher, K.A.; Rothbart, R.M.; Halperin, J.L.; Hart, R.G. Clinical and echocardiographic features of intermittent atrial fibrillation that predict recurrent atrial fibrillation. Stroke Prevention in Atrial Fibrillation (SPAF) investigators. Am. J. Cardiol. 1995, 76, 355–358. [Google Scholar] [CrossRef]
- Tsang, T.S.; Barnes, M.E.; Bailey, K.R.; Leibson, C.L.; Montgomery, S.C.; Takemoto, Y.; Diamond, P.M.; Marra, M.A.; Gersh, B.J.; Wiebers, D.O.; et al. Left atrial volume: Important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin. Proc. 2001, 76, 467–475. [Google Scholar] [CrossRef]





| AF (n = 183) | Non-AF (n = 107) | p Value | |
|---|---|---|---|
| Age onset, y | 53.9 ± 11.6 | 45.4 ± 16.5 | <0.001 * |
| Age at admission, y | 58.5 ± 11.0 | 50.5 ± 15.1 | <0.001 * |
| Female, n (%) | 57 (31.1) | 57 (53.3) | 0.001 * |
| BMI, kg/m2 | 25.8 ± 3.6 | 25.0 ± 3.5 | 0.059 |
| Comorbidities, n (%) | |||
| Hypertension | 95 (51.9) | 35 (32.7) | 0.002 * |
| Diabetes mellitus | 36 (19.7) | 18 (16.8) | 0.547 |
| Coronary heart disease | 31 (16.9) | 13 (12.1) | 0.273 |
| Heart failure | 25 (13.7) | 4 (3.7) | 0.007 * |
| Stroke | 24 (13.1) | 7 (6.5) | 0.080 |
| Vascular disease | 19 (10.4) | 5 (4.7) | 0.089 |
| CHA2DS2-VASc score | 2.0 ± 1.5 | - | - |
| HAS-BLED score | 0.6 ± 0.7 | - | - |
| Open heart surgery, n (%) | 7 (3.8) | 2 (1.9) | 0.354 |
| NYHA-FC, n (%) | |||
| I/II | 177 (96.7) | 107 (100.0) | 0.058 |
| III/IV | 6 (3.3) | 0 | 0.058 |
| LAV, mL | 68.2 ± 25.8 | 49.7 ± 18.1 | <0.001 * |
| LVEF, % | 62.3 ± 7.0 | 64.0 ± 5.3 | 0.023 * |
| AF (n = 183) | Non-AF (n = 107) | p Value | |
|---|---|---|---|
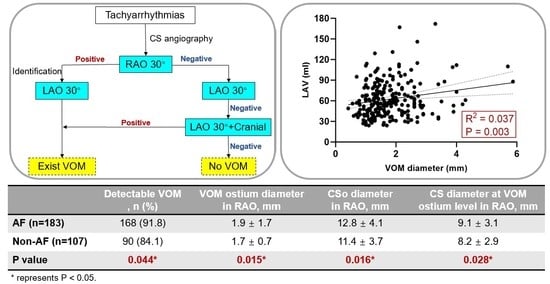
| Undetectable VOM on venography in all views, n (%) | 15 (8.2) | 17 (15.9) | 0.044 * |
| Detectable PLSVA, n (%) | 2 (1.1) | 2 (1.9) | 0.584 |
| Number of branches at VOM ostium | |||
| Type I | 143 (78.1) | 79 (73.8) | 0.477 |
| Type II | 25 (13.7) | 11 (10.3) | 0.477 |
| RAO | |||
| Undetectable VOM on venography in RAO | 20 (10.9) | 23 (21.5) | 0.015 * |
| VOM-CS angle, ° | 45.3 ± 20.5 | 41.4 ± 18.5 | 0.237 |
| VOM ostium diameter, mm | 1.9 ± 0.9 | 1.7 ± 0.7 | 0.015 * |
| CSo diameter, mm | 12.8 ± 4.1 | 11.4 ± 3.7 | 0.016 * |
| CS diameter at VOM level, mm | 9.1 ± 3.1 | 8.2 ± 2.9 | 0.028 * |
| LAO | |||
| Undetectable VOM on venography in LAO | 53 (29.0) | 45 (42.1) | 0.023 * |
| VOM-CS angle, ° | 144.2 ± 36.8 | 156.0 ± 12.6 | 0.036 * |
| VOM-to-CSo distance, mm | 37.8 ± 15.6 | 36.8 ± 13.1 | 0.684 |
| VOM ostium diameter, mm | 1.7 ± 1.0 | 1.7 ± 0.7 | 0.664 |
| CSo diameter, mm | 11.7 ± 5.8 | 10.1 ± 5.4 | 0.022 * |
| CS diameter at VOM level, mm | 7.2 ± 2.9 | 6.5 ± 2.0 | 0.047 * |
| LAO cranial | |||
| Undetectable VOM on venography in LAO + Cranial | 39 (21.3) | 27 (25.2) | 0.442 |
| VOM-CS angle, ° | 127.9 ± 57.5 | 109.2 ± 70.7 | 0.087 |
| VOM-to-CSo distance, mm | 39.6 ± 16.6 | 37.8 ± 13.8 | 0.419 |
| VOM ostium diameter, mm | 1.9 ± 1.1 | 1.6 ± 0.8 | 0.069 |
| CSo diameter, mm | 13.1 ± 5.0 | 12.4 ± 4.8 | 0.263 |
| CS diameter at VOM level, mm | 8.1 ± 3.2 | 7.4 ± 2.4 | 0.141 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ding, L.; Zhang, H.; Yu, F.; Mi, L.; Hua, W.; Zhang, S.; Yao, Y.; Tang, M. Angiographic Characteristics of the Vein of Marshall in Patients with and without Atrial Fibrillation. J. Clin. Med. 2022, 11, 5384. https://doi.org/10.3390/jcm11185384
Ding L, Zhang H, Yu F, Mi L, Hua W, Zhang S, Yao Y, Tang M. Angiographic Characteristics of the Vein of Marshall in Patients with and without Atrial Fibrillation. Journal of Clinical Medicine. 2022; 11(18):5384. https://doi.org/10.3390/jcm11185384
Chicago/Turabian StyleDing, Lei, Hongda Zhang, Fengyuan Yu, Lijie Mi, Wei Hua, Shu Zhang, Yan Yao, and Min Tang. 2022. "Angiographic Characteristics of the Vein of Marshall in Patients with and without Atrial Fibrillation" Journal of Clinical Medicine 11, no. 18: 5384. https://doi.org/10.3390/jcm11185384